Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Soma: 250 mg, 350 mg
Generic: 250 mg, 350 mg
Pharmacology
Mechanism of Action
Precise mechanism is not yet clear, but many effects have been ascribed to its central depressant actions. In animals, carisoprodol blocks interneuronal activity and depresses polysynaptic neuron transmission in the spinal cord and reticular formation of the brain. It is also metabolized to meprobamate, which has anxiolytic and sedative effects.
Pharmacokinetics/Pharmacodynamics
Metabolism
Hepatic, via CYP2C19 to active metabolite (meprobamate)
Excretion
Urine, as metabolite
Onset of Action
Rapid
Time to Peak
Plasma: 1.5 to 2 hours
Duration of Action
4 to 6 hours
Half-Life Elimination
Carisoprodol: ~2 hours; Meprobamate: ~10 hours
Protein Binding
Carisoprodol: (<70%); Meprobamate: (<25%) (Olsen, 1994)
Use in Specific Populations
Special Populations: Gender
Carisoprodol exposure is 30% to 50% higher in women than men; however, meprobamate exposure is not affected by gender.
Special Populations Note
Individuals with reduced CYP2C19 activity have a fourfold increase in carisoprodol exposure and a 50% reduced exposure to meprobamate compared with normal CYP2C19 metabolizers. Prevalence of poor metabolizers in white and black patients is ~3% to 5% and in Asian patients ~15% to 20%.
Use: Labeled Indications
Musculoskeletal conditions: Short-term (2 to 3 weeks) treatment of discomfort associated with acute painful musculoskeletal conditions.
Limitations of use: Carisoprodol should only be used for short periods (up to 2 or 3 weeks); adequate evidence of effectiveness for more prolonged use has not been established and acute, painful musculoskeletal conditions are generally of short duration.
Contraindications
Hypersensitivity to carbamates (eg, meprobamate), or any component of the formulation; history of acute intermittent porphyria
Dosage and Administration
Dosing: Adult
Musculoskeletal conditions: Oral: 250 to 350 mg 3 times daily and at bedtime for a maximum recommended duration of 2 to 3 weeks.
Discontinuation in patients on long-term therapy: Although carisoprodol should only be used for short periods (2 to 3 weeks), in patients with a history of long term use or high doses, carisoprodol should be tapered off slowly (eg, over 14 days) to avoid withdrawal symptoms such as anxiety, insomnia, or irritability (Eleid 2010).
Dosing: Geriatric
Avoid use (Beers Criteria [AGS 2019]).
Dosing: Pediatric
Musculoskeletal conditions: Adolescents ≥16 years: Oral: 250 to 350 mg 3 times daily and at bedtime (ie, 4 daily doses); maximum daily dose: 1,400 mg/day; maximum duration of therapy: 3 weeks
Discontinuation in patients on long-term therapy: Although carisoprodol should only be used for short periods (2 to 3 weeks), experience in adult patients with a history of long-term use or high doses suggests carisoprodol should be tapered off slowly (eg, over 14 days) to avoid withdrawal symptoms such as anxiety, insomnia, or irritability (Eleid 2010)
Administration
May be administered with or without food.
Storage
Store at 20°C to 25°C (68°F to 77°F).
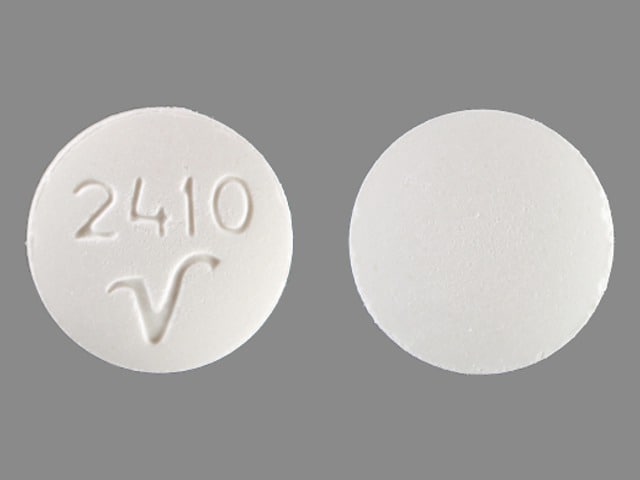
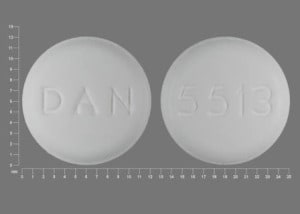
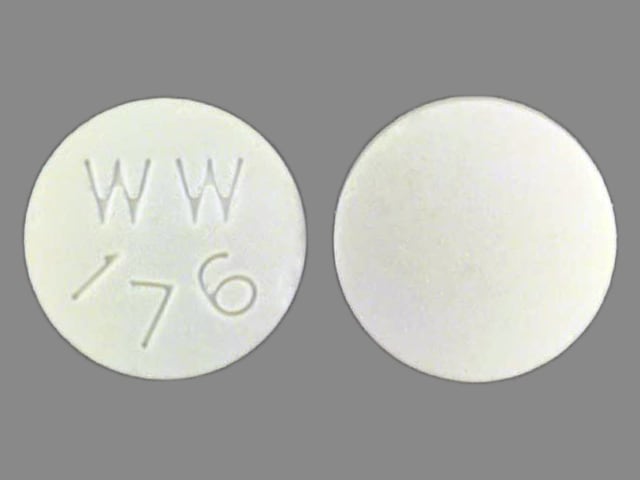
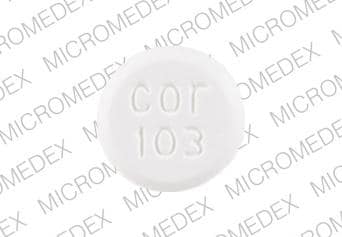
Carisoprodol Images
Drug Interactions
Alcohol (Ethyl): CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Aspirin: May increase serum concentrations of the active metabolite(s) of Carisoprodol. Specifically, Meprobamate concentrations may be increased. Aspirin may decrease the serum concentration of Carisoprodol. Monitor therapy
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Botulinum Toxin-Containing Products: Muscle Relaxants (Centrally Acting) may enhance the adverse/toxic effect of Botulinum Toxin-Containing Products. Specifically, the risk for increased muscle weakness may be enhanced. Monitor therapy
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
CYP2C19 Inducers (Moderate): May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Monitor therapy
CYP2C19 Inducers (Strong): May increase the metabolism of CYP2C19 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP2C19 Inhibitors (Moderate): May decrease the metabolism of CYP2C19 Substrates (High risk with Inhibitors). Monitor therapy
CYP2C19 Inhibitors (Strong): May decrease the metabolism of CYP2C19 Substrates (High risk with Inhibitors). Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP2C19 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Enzalutamide: May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Conversely, concentrations of active metabolites may be increased for those drugs activated by CYP2C19. Management: Concurrent use of enzalutamide with CYP2C19 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP2C19 substrate should be performed with caution and close monitoring. Consider therapy modification
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Lumacaftor and Ivacaftor: May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Monitor therapy
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Ombitasvir, Paritaprevir, and Ritonavir: May decrease the serum concentration of Carisoprodol. Monitor therapy
Ombitasvir, Paritaprevir, Ritonavir, and Dasabuvir: May decrease the serum concentration of Carisoprodol. Monitor therapy
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
St John's Wort: May increase serum concentrations of the active metabolite(s) of Carisoprodol. Specifically, Meprobamate concentrations may be increased. St John's Wort may decrease the serum concentration of Carisoprodol. Monitor therapy
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Tolperisone: May enhance the adverse/toxic effect of Muscle Relaxants (Centrally Acting). Management: Monitor for increased sedation or CNS effects if tolperisone is combined with other centrally acting muscle relaxants. Consider decreasing the tolperisone dose if these agents are combined. Consider therapy modification
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Adverse Reactions
>10%: Central nervous system: Drowsiness (13% to 17%)
1% to 10%: Central nervous system: Dizziness (7% to 8%), headache (3% to 5%)
Postmarketing and/or case reports: Abdominal cramps, agitation, allergic dermatitis, anaphylaxis, angioedema, ataxia, burning sensation of eyes, depression, drug dependence, dyspnea, epigastric pain, eosinophilia, erythema multiforme, exacerbation of asthma, fixed drug eruption, hallucination, headache, hiccups, hypersensitivity reaction, idiosyncratic reaction (symptoms may include agitation, ataxia, confusion, diplopia, disorientation, dysarthria, euphoria, extreme weakness, muscle twitching, mydriasis, temporary vision loss, and/or transient quadriplegia); insomnia, irritability, leukopenia, nausea, orthostatic hypotension, pancytopenia, paradoxical central nervous system stimulation, pruritus, psychosis, seizure, skin rash, syncope, tachycardia, transient flushing of face, tremor, urticaria, vertigo, vomiting, weakness, withdrawal syndrome (abdominal cramps, headache, insomnia, nausea, seizure)
Warnings/Precautions
Concerns related to adverse effects:
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; concomitant use of other CNS depressants may enhance these effects. Patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving); in postmarketing reports, motor vehicle accidents have been associated with use. Sedating effects may be potentiated when used with other CNS-depressant drugs or ethanol.
- Seizures: There have been postmarketing reports of seizures with carisoprodol; most cases occurred in the setting of multiple-drug overdoses (including drugs of abuse, illegal drugs, and alcohol).
Disease-related concerns:
- Drug abuse and dependence: Use with caution in patients with a history of drug abuse or acute alcoholism; potential for drug dependency exists. Tolerance, psychological and physical dependence to carisoprodol (and its metabolite, meprobamate) may occur with prolonged use. Limit use to 2 to 3 weeks.
- Hepatic impairment: Use with caution in patients with hepatic impairment; carisoprodol undergoes hepatic metabolism.
- Renal impairment: Use with caution in patients with renal impairment; carisoprodol undergoes renal excretion.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Poor CYP2C19 metabolizers: Use with caution in patients with reduced CYP2C19 activity; poor metabolizers have been shown to have a fourfold increase in carisoprodol exposure and a 50% reduced exposure to meprobamate (active metabolite) compared to normal metabolizers. Prevalence of poor metabolizers in the Asian population is ~15% to 20% while that of Caucasians and African-Americans is ~3% to 5%.
Other warnings/precautions:
- Withdrawal: May precipitate withdrawal after abrupt cessation of prolonged use. Reported withdrawal symptoms have included insomnia, vomiting, abdominal pain, headache, tremors/twitching, ataxia, hallucinations, and psychosis. Withdrawal symptoms may be due to accumulation of the active metabolite (meprobamate), although carisoprodol may also contribute to the symptoms (Reeves 2010). Although carisoprodol should only be used for short periods (2 to 3 weeks), in patients with a history of long term use or high doses, carisoprodol should be tapered off slowly (eg, over 14 days) to avoid withdrawal symptoms such as anxiety, insomnia, or irritability (Eleid 2010).
Monitoring Parameters
CNS effects (eg, mental status, excessive drowsiness); relief of pain and/or muscle spasm; signs of misuse, abuse, and addiction
Pregnancy
Pregnancy Considerations
Postmarketing data with meprobamate (the active metabolite) do not show a consistent association between maternal use and an increased risk or pattern of major congenital malformations. In one study, maternal use did not adversely affect mental or motor development, or IQ scores in children exposed in utero.
Patient Education
What is this drug used for?
- It is used to relax muscles.
Frequently reported side effects of this drug
- Headache
- Dizziness
- Fatigue
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Seizures
- Severe loss of strength and energy
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.