Boxed Warning
Diminished antiplatelet effect in patients with two loss-of-function alleles of the CYP2C19 gene:
The effectiveness of clopidogrel results from its antiplatelet activity, which is dependent on its conversion to an active metabolite by the cytochrome P450 (CYP-450) system, principally CYP2C19. Clopidogrel at recommended doses forms less of the active metabolite and has a reduced effect on platelet activity in patients who are homozygous for nonfunctional alleles of the CYP2C19 genes (termed “CYP2C19 poor metabolizers”). Tests are available to identify patients who are CYP2C19 poor metabolizers. Consider use of another platelet P2Y12 inhibitor in patients identified as CYP2C19 poor metabolizers.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Tablet, Oral:
Plavix: 75 mg, 300 mg [DSC]
Generic: 75 mg, 300 mg
Pharmacology
Mechanism of Action
Clopidogrel requires in vivo biotransformation to an active thiol metabolite. The active metabolite irreversibly blocks the P2Y12 component of ADP receptors on the platelet surface, which prevents activation of the GPIIb/IIIa receptor complex, thereby reducing platelet aggregation. Platelets blocked by clopidogrel are affected for the remainder of their lifespan (~7 to 10 days).
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid, well absorbed
Metabolism
Extensively hepatic via esterase-mediated hydrolysis to a carboxylic acid derivative (inactive) and via CYP450-mediated (CYP2C19 primarily) oxidation to a thiol metabolite (active)
Excretion
Following administration of a single 14C-labeled clopidogrel oral dose; radioactivity measured over 5 days: Urine (50%); feces (46%)
Onset of Action
Onset of action: Inhibition of platelet aggregation (IPA): Dose-dependent:
300 to 600 mg loading dose: Detected within 2 hours
50 to 100 mg/day: Detected by the second day of treatment
Peak effect: Time to maximal IPA: Dose-dependent: Note: Degree of IPA based on adenosine diphosphate (ADP) concentration used during light aggregometry:
300 to 600 mg loading dose:
ADP 5 micromole/L: 20% to 30% IPA at 6 hours post administration (Montelescot 2006)
ADP 20 micromole/L: 30% to 37% IPA at 6 hours post administration (Montelescot 2006)
50 to 100 mg/day: ADP 5 micromole/L: 50% to 60% IPA at 5 to 7 days (Herbert 1993)
Time to Peak
Serum: ~0.75 hours
Duration of Action
Platelet aggregation and bleeding time gradually return to baseline after ~5 days after discontinuation.
Half-Life Elimination
Parent drug: ~6 hours; Thiol derivative (active metabolite) ~30 minutes; carboxylic acid derivative (inactive; main circulating metabolite): ~8 hours; Note: A clopidogrel radiolabeled study has shown that covalent binding to platelets accounts for 2% of radiolabel and has a half-life of 11 days.
Protein Binding
Parent drug: 98%; Inactive metabolite (carboxylic acid derivative): 94%
Use in Specific Populations
Special Populations: Renal Function Impairment
After repeated doses of clopidogrel 75 mg/day, patients with severe (CrCl 5 to 15 mL/minute) and moderate (CrCl 30 to 60 mL/minute) renal impairment showed low (25%) inhibition of ADP-induced platelet aggregation.
Special Populations: Gender
Less inhibition of ADP-induced platelet aggregation was observed in women.
Use: Labeled Indications
Acute coronary syndrome:
ST-segment elevation myocardial infarction: To reduce the rate of myocardial infarction (MI) and stroke in conjunction with aspirin in patients with acute ST-elevation MI who are to be managed medically.
Non-ST-segment elevation acute coronary syndromes: To decrease the rate of MI and stroke in conjunction with aspirin in patients with non-ST-segment elevation acute coronary syndromes (unstable angina/non-ST-elevation MI), including patients who are to be managed medically and those who are to be managed with coronary revascularization.
Myocardial infarction, ischemic stroke, or peripheral atherosclerotic disease: To reduce the rate of MI and stroke in patients with a history of recent MI, recent stroke, or established peripheral atherosclerotic disease.
Use: Off Label
Carotid artery atherosclerosis, symptomaticyes
Based on the American College of Chest Physicians guidelines for antithrombotic therapy in peripheral artery disease, clopidogrel is effective and recommended for patients with symptomatic carotid artery atherosclerosis.
Carotid artery stentingc
A randomized, controlled trial with blinded end point adjudication evaluated carotid artery stenting versus carotid endarterectomy in patients with carotid artery stenosis. In this trial, aspirin in combination with clopidogrel was used for patients who underwent carotid artery stenting, which suggests that this antiplatelet combination is effective Brott 2010. Clinical experience also suggests the utility of this antiplatelet regimen around the time of carotid artery stenting Fairman 2019.
Coronary artery bypass graft surgeryyes
Based on the 2015 American Heart Association (AHA) scientific statement on secondary prevention after coronary artery bypass graft surgery (CABG), clopidogrel is a reasonable alternative to aspirin for patients who are intolerant or allergic to aspirin. Additionally, in patients following off-pump CABG, clopidogrel in combination with aspirin should be administered for 1 year to reduce graft occlusion. In patients following on-pump CABG (without recent acute coronary syndrome), clopidogrel in combination with aspirin may be considered but benefits are not well established.
Percutaneous coronary intervention for stable ischemic heart diseaseayes
Data from prospective, randomized, double-blind, placebo-controlled trials support the use of clopidogrel as part of the antiplatelet regimen for percutaneous coronary intervention (PCI) Mehta 2001, Patti 2011, Sabatine 2005b, Steinhubl 2002.
Based on the 2011 American College of Cardiology Foundation/American Heart Association/Society for Cardiovascular Angiography and Interventions (ACCF/AHA/SCAI) PCI guidelines, clopidogrel is an effective and recommended adjunctive oral antithrombotic agent for patients with stable ischemic heart disease undergoing PCI.
Stable ischemic heart diseaseayes
Data from a prospective, randomized, double-blind, placebo-controlled trial in patients with a history of atherosclerotic cardiovascular disease support the long-term use of clopidogrel for secondary prevention of cardiovascular events (eg, ischemic stroke, myocardial infarction, vascular death) CAPRIE 1996.
Based on the 2012 ACCF/AHA guideline for the diagnosis and management of patients with stable ischemic heart disease, clopidogrel is effective and recommended for secondary prevention of cardiovascular disease in patients with a documented aspirin allergy.
Transcatheter aortic valve replacement (thromboprophylaxis)byes
Data from multiple clinical trials support the use of clopidogrel in combination with aspirin as an antithrombotic strategy for transcatheter aortic valve replacement (TAVR) Adams 2014, Leon 2010, Leon 2016, Reardon 2017, Smith 2011b.
Based on the 2017 American Heart Association/American College of Cardiology (AHA/ACC) focused update of the 2014 guideline for the management of patients with valvular heart disease, clopidogrel may be reasonable for up to 6 months after TAVR in addition to life-long aspirin. The optimal postprocedure antithrombotic strategy for TAVR is unknown, especially for patients who require concomitant anticoagulation. Various antithrombotic regimens are still under investigation. Clinicians should consider patient-specific risks for bleeding and thrombosis when making pharmacotherapy plans ACC [Otto 2017], Kalich 2018.
Contraindications
Hypersensitivity (eg, anaphylaxis) to clopidogrel or any component of the formulation; active pathological bleeding (eg, peptic ulcer, intracranial hemorrhage).
Canadian labeling: Additional contraindications (not in US labeling): Significant liver impairment or cholestatic jaundice; concomitant use of repaglinide.
Dosage and Administration
Dosing: Adult
Acute coronary syndrome:
Note: Routine platelet-function testing or genetic testing for CYP2C19 polymorphisms is not recommended (ACC/AHA [Levine 2016]; Scott 2013; Sibbing 2019).
ST-segment elevation myocardial infarction: Note: Regardless of the reperfusion strategy, administer clopidogrel in combination with a parenteral anticoagulant and aspirin (ACCF/AHA [O'Gara 2013]).
If using fibrinolytic therapy for reperfusion:
Age ≤75 years: Oral: Initial loading dose: 300 mg once at the time of diagnosis; followed by 75 mg once daily (ACCF/AHA [O'Gara 2013]; Sabatine 2005a).
Age >75 years: Oral: 75 mg once daily (ACCF/AHA [O'Gara 2013]).
Patient requires percutaneous coronary intervention following fibrinolytic therapy:
Fibrinolytic administered with a loading dose of clopidogrel: Oral: Continue 75 mg once daily (do not administer an additional loading dose) (ACCF/AHA [O'Gara 2013]).
Fibrinolytic administered ≤24 hours ago without a loading dose of clopidogrel: Oral: Initial: 300 mg once prior to percutaneous coronary intervention (PCI); followed by 75 mg once daily after PCI (ACCF/AHA [O'Gara 2013]).
Fibrinolytic administered >24 hours ago without a loading dose of clopidogrel: Oral: Initial: 600 mg once prior to PCI; followed by 75 mg once daily after PCI (ACCF/AHA [O'Gara 2013]).
If using percutaneous coronary intervention for reperfusion (alternative agent) (off-label use): Note: Some experts prefer ticagrelor or prasugrel over clopidogrel unless there is high risk for bleeding (Lincoff 2019; Wallentin 2009; Wiviott 2007).
Oral: Initial: 600 mg once as early as possible before PCI; followed by 75 mg once daily after PCI (ACCF/AHA [O'Gara 2013]; Dangas 2009; Mehta 2010).
If no planned reperfusion strategy (alternative agent): Note: Some experts prefer ticagrelor over clopidogrel (Lincoff 2019).
Oral: Initial: 300 mg once at the time of diagnosis; followed by 75 mg once daily (Lincoff 2019).
Duration of therapy: Clopidogrel plus aspirin (dual antiplatelet therapy [DAPT]) should be continued for ≥12 months unless bleeding is a concern. If there have been no major bleeding complications after 12 months, continuation of DAPT may be considered. Reevaluate the need for DAPT at regular intervals based on bleeding and thrombotic risks. When DAPT is complete, discontinue clopidogrel and continue aspirin indefinitely (ACC/AHA [Levine 2016]; ACCF/AHA [O'Gara 2013]; Lincoff 2019; Mauri 2014).
Non-ST-segment elevation acute coronary syndromes: Note: Regardless of the management strategy, administer clopidogrel in combination with a parenteral anticoagulant and aspirin (ACC/AHA [Amsterdam 2014]).
If using an ischemia-guided approach (medical management) (alternative agent): Note: Some experts prefer ticagrelor over clopidogrel (Cutlip 2019a).
Oral: Initial: 300 or 600 mg once at the time of diagnosis; followed by 75 mg once daily (ACC/AHA [Amsterdam 2014]). Some experts prefer an initial dose of 600 mg unless there is high risk for bleeding, in which case, an initial dose of 300 mg is also appropriate (Cutlip 2019a).
If using an invasive approach (reperfusion using percutaneous coronary intervention) (alternative agent): Note: Some experts prefer ticagrelor or prasugrel over clopidogrel unless there is high risk for bleeding (Cutlip 2019a; Wallentin 2009; Wiviott 2007).
Oral: Initial: 600 mg once as early as possible before PCI; followed by 75 mg once daily after PCI (ACC/AHA [Amsterdam 2014]).
Duration of therapy: Clopidogrel plus aspirin (DAPT) should be continued for ≥12 months unless bleeding is a concern. If there have been no major bleeding complications after 12 months, continuation of DAPT may be considered. Reevaluate the need for DAPT at regular intervals based on bleeding and thrombotic risks. When DAPT is complete, discontinue clopidogrel and continue aspirin indefinitely (ACC/AHA [Amsterdam 2014]; ACC/AHA [Levine 2016]; Cutlip 2019a; Mauri 2014; Mehta 2001; Yusuf 2001).
Percutaneous coronary intervention for stable ischemic heart disease (off-label use): Note: Administer clopidogrel in combination with a parenteral anticoagulant and aspirin for patients who undergo PCI with stenting (ACCF/AHA/SCAI [Levine 2011]).
Oral: Initial: 600 mg once, administered ≥2 hours before PCI, ideally ≥24 hours before PCI; followed by 75 mg once daily (ACCF/AHA/SCAI [Levine 2011]; Cutlip 2020).
Duration of therapy: Upon completion of the recommended duration of DAPT (clopidogrel plus aspirin), discontinue clopidogrel and continue aspirin indefinitely (ACC/AHA [Levine 2016]; Cutlip 2019c):
- Bare metal stent implantation: DAPT for a minimum of 1 month (ACC/AHA [Levine 2016]). Some experts recommend at least 6 months and up to 12 months; in patients at high bleeding risk, shorter duration may be considered. After 6 to 12 months, assess bleeding and ischemic risks to determine if patient should receive longer therapy (eg, for an additional 18 to 24 months) (Cutlip 2019c).
- Drug eluting stent implantation: DAPT for at least 6 months and up to 12 months; if bleeding occurs or patient is at high risk of bleeding, may stop after 3 months (ACC/AHA [Levine 2016]). After 6 to 12 months, assess bleeding and ischemic risks to determine if patient should receive longer therapy (eg, for an additional 18 to 24 months) (Cutlip 2019c).
Carotid artery atherosclerosis, symptomatic (alternative agent) (off-label use): Note: For patients who are intolerant of aspirin.
Oral: 75 mg once daily (ACCP [Alonso-Coello 2012]; Cucchiara 2019).
Carotid artery stenting (off-label use):
Initial:
Initiation ≥48 hours before procedure: Oral: 75 mg twice daily in combination with aspirin (Brott 2010; Fairman 2019).
Initiation <48 hours of procedure: Oral: 450 mg once ≥4 hours before procedure in combination with aspirin (Brott 2010; Fairman 2019).
Maintenance: Oral: 75 mg once daily in combination with aspirin for ≥6 weeks; after 6 weeks of DAPT with clopidogrel and aspirin, assess bleeding and ischemic risks to determine total duration of therapy; upon completion of DAPT, discontinue clopidogrel and continue aspirin indefinitely. In patients with history of neck irradiation, some experts recommend continuing clopidogrel plus aspirin indefinitely (Brott 2010; Fairman 2019).
Coronary artery bypass graft surgery (off-label use):
Aspirin-allergic or aspirin-intolerant patients: Oral: 75 mg once daily; continue indefinitely (AHA [Kulik 2015]).
Following off-pump coronary artery bypass graft surgery: Oral: 75 mg once daily in combination with aspirin for 1 year, then discontinue clopidogrel and continue aspirin indefinitely (AHA [Kulik 2015]; Deo 2013; Mannacio 2012).
Patients with acute coronary syndrome followed by coronary artery bypass graft surgery: Oral: 75 mg once daily in combination with aspirin for 1 year, then discontinue clopidogrel and continue aspirin indefinitely (AHA [Kulik 2015]). Some experts do not use clopidogrel postoperatively in these patients (Aranki 2019).
Peripheral atherosclerotic disease (upper or lower extremity; with or without revascularization): Oral: 75 mg once daily (ACCP [Alonso-Coello 2012]; AHA/ACC [Gerhard-Herman 2017]; CAPRIE 1996).
Stable ischemic heart disease (alternative agent) (off-label use): Note: Aspirin is preferred; clopidogrel is an alternative for patients who have a history of GI bleeding or are allergic to aspirin (ACCF/AHA [Fihn 2012]).
Oral: 75 mg once daily (ACCF/AHA [Fihn 2012]; ACCP [Vandvik 2012]; CAPRIE 1996).
Stroke/Transient ischemic attack:
Intracranial atherosclerosis (50% to 99% stenosis of a major intracranial artery), secondary prevention: Note: Aspirin is recommended for all patients; may consider clopidogrel (in combination with aspirin) for short-term use in patients with recent stroke or transient ischemic attack (within 30 days) (AHA/ASA [Kernan 2014]; Ehtisham 2019). For long-term stroke prevention, indefinite use of clopidogrel monotherapy is an alternative to aspirin (AHA/ASA [Kernan 2014]).
Oral: 75 mg once daily in combination with aspirin; duration of clopidogrel depends on degree of stenosis.
Stenosis of 50% to 69%: Clopidogrel may be added to aspirin for 21 days; after 21 days, discontinue clopidogrel and continue aspirin indefinitely (Ehtisham 2019).
Stenosis of 70% to 99%: Clopidogrel may be added to aspirin for 90 days; after 90 days, discontinue clopidogrel and continue aspirin indefinitely (AHA/ASA [Kernan 2014]; Derdeyn 2014; Ehtisham 2019).
Ischemic stroke or transient ischemic attack, noncardioembolic, secondary prevention: Oral: 75 mg once daily.
Minor ischemic stroke (NIHSS score ≤3) or high-risk transient ischemic attack (ABCD2 score ≥4): Note: Short-term use of clopidogrel in combination with aspirin may be considered for initiation as soon as possible and within 24 hours of stroke onset. If an IV thrombolytic was administered, delay starting antiplatelet therapy for ≥24 hours but administer as soon as possible thereafter (AHA/ASA [Kernan 2014]; AHA/ASA [Powers 2018]; Johnston 2018; Wang 2013).
Oral: Initial: 300 to 600 mg in combination with aspirin; followed by 75 mg once daily for 21 days; after 21 days, discontinue clopidogrel and continue aspirin indefinitely (AHA/ASA [Kernan 2014]; AHA/ASA [Powers 2018]; Johnston 2018; Wang 2013).
Transcatheter aortic valve replacement (thromboprophylaxis) (off-label use): Oral: 300 mg once prior to valve implantation in combination with aspirin; followed by 75 mg once daily for 3 to 6 months depending on the type of valve implanted; after completion of clopidogrel, continue aspirin indefinitely (ACC [Otto 2017]; AHA/ACC [Nishimura 2014], AHA/ACC [Nishimura 2017]; Kalich 2018).
Transitioning between P2Y12 inhibitors: Note: This provides general guidance on transitioning between P2Y12 inhibitors.
Transitioning from another P2Y12 inhibitor to clopidogrel:
Transitioning from prasugrel:
Patient received prasugrel for ≤5 days: Give a clopidogrel 300 mg loading dose 24 hours after the last dose of prasugrel, followed by 75 mg once daily; some experts do not administer a loading dose (Lincoff 2019).
Patient received prasugrel for >5 days: Give clopidogrel 75 mg once daily, starting 24 hours after the last dose of prasugrel (Lincoff 2019).
Transitioning from ticagrelor: Give a clopidogrel 600 mg loading dose 12 hours after the last dose of ticagrelor, followed by 75 mg once daily (Franchi 2018).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Antiplatelet effect: Limited data available:
Infants and Children ≤24 months: In the PICOLO trial, a dose of 0.2 mg/kg/dose once daily was found to achieve a mean inhibition of platelet aggregation similar to adults receiving the recommended dose; Note: This study included pediatric patients with a systemic-to-pulmonary artery shunt, intracardiac or intravascular stent, Kawasaki disease, or arterial graft; 79% of patients received concomitant aspirin (Li 2008).
Children >2 years and Adolescents: Initial dose: 1 mg/kg once daily; titrate to response; in general, do not exceed adult dose (Finkelstein 2005; Soman 2006).
CYP2C19 poor metabolizers (ie, CYP2C19*2 or *3 carriers): Specific pediatric recommendations are lacking; based on experience in adult patients, routine genetic testing is not recommended in patients treated with clopidogrel undergoing PCI, testing may be considered to identify poor metabolizers who would be at risk for poor outcomes while receiving clopidogrel; if identified, these patients may be considered for an alternative P2Y12 inhibitor (Levine 2011).
Extemporaneously Prepared
A 5 mg/mL oral suspension may be made using tablets. Crush four 75 mg tablets and reduce to a fine powder. Add a small amount of a 1:1 mixture of Ora-Sweet® and Ora-Plus® and mix to a uniform paste; mix while adding the vehicle in geometric proportions to almost 60 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 60 mL. Label "shake well". Stable 60 days at room temperature or under refrigeration.
Skillman KL, Caruthers RL, and Johnson CE, "Stability of an Extemporaneously Prepared Clopidogrel Oral Suspension," Am J Health Syst Pharm, 2010, 67(7):559-61.20237383
Administration
Administer without regard to meals.
Dietary Considerations
Avoid or minimize the consumption of grapefruit juice (Holmberg 2013).
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
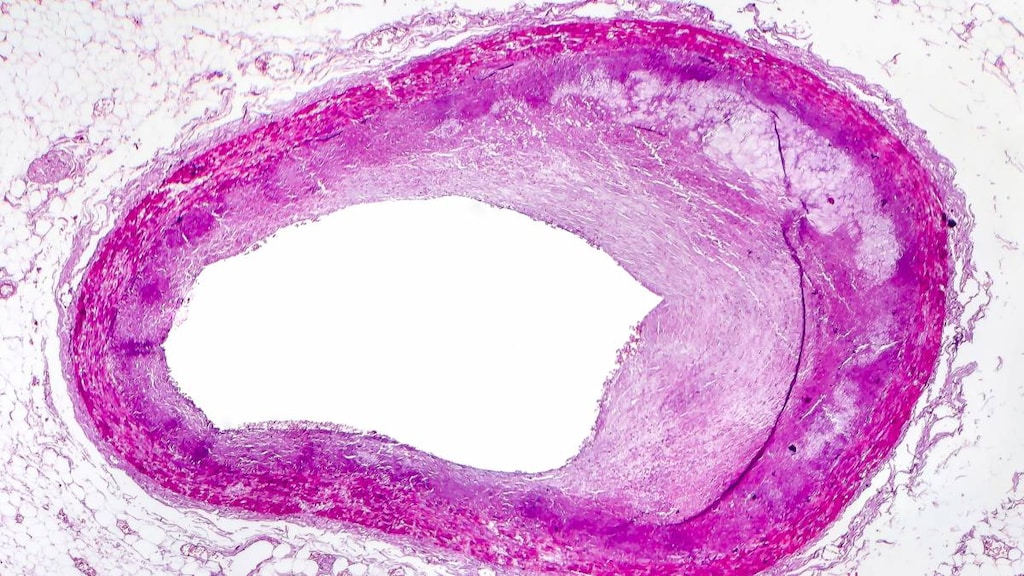
Clopidogrel Images
Drug Interactions
Acalabrutinib: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Agents with Antiplatelet Properties (e.g., P2Y12 inhibitors, NSAIDs, SSRIs, etc.): May enhance the antiplatelet effect of other Agents with Antiplatelet Properties. Monitor therapy
Alpelisib: BCRP/ABCG2 Inhibitors may increase the serum concentration of Alpelisib. Management: Avoid coadministration of BCRP/ABCG2 inhibitors and alpelisib due to the potential for increased alpelisib concentrations and toxicities. If coadministration cannot be avoided, closely monitor for increased alpelisib adverse reactions. Consider therapy modification
Amiodarone: May decrease serum concentrations of the active metabolite(s) of Clopidogrel. Monitor therapy
Amodiaquine: CYP2C8 Inhibitors (Moderate) may increase the serum concentration of Amodiaquine. Avoid combination
Anticoagulants: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Anticoagulants. Exceptions: Bemiparin; Enoxaparin; Heparin. Monitor therapy
Apixaban: Antiplatelet Agents (P2Y12 Inhibitors) may enhance the adverse/toxic effect of Apixaban. Specifically, the risk for bleeding may be increased. Management: Carefully consider risks and benefits of this combination and monitor closely; Canadian labeling recommends avoiding prasugrel or ticagrelor. Consider therapy modification
Bemiparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Bemiparin. Management: Avoid concomitant use of bemiparin with antiplatelet agents. If concomitant use is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
BuPROPion: CYP2B6 Inhibitors (Weak) may increase the serum concentration of BuPROPion. Monitor therapy
Calcium Channel Blockers: May diminish the therapeutic effect of Clopidogrel. Exceptions: Clevidipine. Monitor therapy
Cangrelor: May diminish the antiplatelet effect of Clopidogrel. More specifically, while the use of Cangrelor is expected to increase total platelet inhibition in patients who have previously received Clopidogrel, Cangrelor is expected to decrease binding of Clopidogrel metabolites to P2Y12 receptors and thus reduce the extent of irreversible platelet inhibition. Management: Avoid administration of clopidogrel until cangrelor infusion is discontinued. Consider therapy modification
Cephalothin: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Cephalothin. Specifically, the risk for bleeding may be increased. Monitor therapy
Cladribine: BCRP/ABCG2 Inhibitors may increase the serum concentration of Cladribine. Management: Avoid concomitant use of BCRP inhibitors during the 4 to 5 day oral cladribine treatment cycles whenever possible. If combined, consider dose reduction of the BCRP inhibitor and separation in the timing of administration. Consider therapy modification
Collagenase (Systemic): Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Collagenase (Systemic). Specifically, the risk of injection site bruising and/or bleeding may be increased. Monitor therapy
CYP2C19 Inducers (Strong): May increase serum concentrations of the active metabolite(s) of Clopidogrel. Monitor therapy
CYP2C19 Inhibitors (Moderate): May decrease serum concentrations of the active metabolite(s) of Clopidogrel. Management: Due to a risk for impaired clopidogrel effectiveness with such a combination, carefully consider the need for a moderate CYP2C19 inhibitor in patients receiving clopidogrel. Monitor patients closely for evidence of a diminished response to clopidogrel. Consider therapy modification
CYP2C19 Inhibitors (Strong): May decrease serum concentrations of the active metabolite(s) of Clopidogrel. Management: Due to a risk for impaired clopidogrel effectiveness with such a combination, carefully consider the need for a strong CYP2C19 inhibitor in patients receiving clopidogrel. Monitor patients closely for evidence of a diminished response to clopidogrel. Consider therapy modification
Dabigatran Etexilate: Antiplatelet Agents (P2Y12 Inhibitors) may enhance the adverse/toxic effect of Dabigatran Etexilate. Specifically, the risk of bleeding may be increased. Antiplatelet Agents (P2Y12 Inhibitors) may increase the serum concentration of Dabigatran Etexilate. Specifically, clopidogrel may increase dabigatran serum concentrations. Management: Carefully consider risks and benefits of this combination and monitor closely; Canadian labeling recommends avoiding prasugrel or ticagrelor. Consider therapy modification
Dabrafenib: CYP2C8 Inhibitors (Moderate) may increase the serum concentration of Dabrafenib. Monitor therapy
Dasabuvir: CYP2C8 Inhibitors (Moderate) may increase the serum concentration of Dasabuvir. Monitor therapy
Dasatinib: May enhance the anticoagulant effect of Agents with Antiplatelet Properties. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Deoxycholic Acid: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Deoxycholic Acid. Specifically, the risk for bleeding or bruising in the treatment area may be increased. Monitor therapy
Desloratadine: CYP2C8 Inhibitors (Moderate) may increase the serum concentration of Desloratadine. Monitor therapy
Edoxaban: Antiplatelet Agents (P2Y12 Inhibitors) may enhance the adverse/toxic effect of Edoxaban. Specifically, the risk of bleeding may be increased. Management: Carefully consider the anticipated risks and benefits of this combination. If combined, increased monitoring for bleeding is recommended. Consider therapy modification
Enoxaparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Enoxaparin. Management: Discontinue antiplatelet agents prior to initiating enoxaparin whenever possible. If concomitant administration is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Enzalutamide: CYP2C8 Inhibitors (Moderate) may increase the serum concentration of Enzalutamide. Monitor therapy
Erythromycin (Systemic): May diminish the antiplatelet effect of Clopidogrel. Monitor therapy
Esomeprazole: May diminish the antiplatelet effect of Clopidogrel. Esomeprazole may decrease serum concentrations of the active metabolite(s) of Clopidogrel. Management: Clopidogrel prescribing information recommends avoiding concurrent use with esomeprazole. Rabeprazole or pantoprazole may be lower-risk alternatives to esomeprazole. Consider therapy modification
Etravirine: May decrease serum concentrations of the active metabolite(s) of Clopidogrel. Management: Consider alternatives to clopidogrel in patients treated with etravirine. If combined, monitor for reduced clopidogrel effectiveness. Consider therapy modification
Fat Emulsion (Fish Oil Based): May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Monitor therapy
FentaNYL: May diminish the antiplatelet effect of Antiplatelet Agents (P2Y12 Inhibitors). FentaNYL may decrease the serum concentration of Antiplatelet Agents (P2Y12 Inhibitors). Monitor therapy
FluvoxaMINE: May enhance the adverse/toxic effect of Clopidogrel. Specifically, the risk for bleeding may be increased. FluvoxaMINE may decrease serum concentrations of the active metabolite(s) of Clopidogrel. Monitor therapy
Glucosamine: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Grapefruit Juice: May decrease serum concentrations of the active metabolite(s) of Clopidogrel. Management: Advise patients receiving clopidogrel to minimize consumption of grapefruit and grapefruit juice. Consumption of three 200 mL glasses of grapefruit juice a day may substantially reduce clopidogrel antiplatelet effects. Consider therapy modification
Heparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Heparin. Management: Decrease the dose of heparin or agents with antiplatelet properties if coadministration is required. Consider therapy modification
Herbs (Anticoagulant/Antiplatelet Properties) (eg, Alfalfa, Anise, Bilberry): May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Bleeding may occur. Management: Avoid combination when possible. If used, monitor more closely for evidence of bleeding. Discontinue herbal products with anticoagulant or antiplatelet actions 2 weeks prior to surgical, dental, or invasive procedures. Consider therapy modification
Ibritumomab Tiuxetan: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Ibritumomab Tiuxetan. Both agents may contribute to impaired platelet function and an increased risk of bleeding. Monitor therapy
Ibrutinib: May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Monitor therapy
Inotersen: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Lansoprazole: May decrease serum concentrations of the active metabolite(s) of Clopidogrel. Monitor therapy
Limaprost: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Morphine (Systemic): May diminish the antiplatelet effect of Antiplatelet Agents (P2Y12 Inhibitors). Morphine (Systemic) may decrease the serum concentration of Antiplatelet Agents (P2Y12 Inhibitors). Management: Consider alternative anti-ischemic/analgesic therapies (eg, beta-blockers, nitroglycerin) in patients with acute coronary syndromes treated with a P2Y12 inhibitor when possible. The risks associated with other opioids are unknown. Consider therapy modification
Multivitamins/Fluoride (with ADE): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Multivitamins/Minerals (with AE, No Iron): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Obinutuzumab: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Obinutuzumab. Specifically, the risk of serious bleeding-related events may be increased. Monitor therapy
Ombitasvir, Paritaprevir, Ritonavir, and Dasabuvir: CYP2C8 Inhibitors (Moderate) may increase the serum concentration of Ombitasvir, Paritaprevir, Ritonavir, and Dasabuvir. Specifically, the concentrations of the dasabuvir component may be increased. Monitor therapy
Omega-3 Fatty Acids: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Omeprazole: May diminish the antiplatelet effect of Clopidogrel. Omeprazole may decrease serum concentrations of the active metabolite(s) of Clopidogrel. Management: Clopidogrel labeling recommends avoiding concurrent omeprazole due to a possible decrease in clopidogrel effectiveness. Rabeprazole or pantoprazole may be lower-risk alternatives to omeprazole. Consider therapy modification
PACLitaxel (Conventional): CYP2C8 Inhibitors (Moderate) may increase the serum concentration of PACLitaxel (Conventional). Monitor therapy
PACLitaxel (Protein Bound): CYP2C8 Inhibitors (Moderate) may increase the serum concentration of PACLitaxel (Protein Bound). Monitor therapy
Pantoprazole: May decrease serum concentrations of the active metabolite(s) of Clopidogrel. Management: Due to the possible risk for impaired clopidogrel effectiveness, clinicians should carefully consider the need for proton pump inhibitor therapy in patients receiving clopidogrel. Other acid-lowering therapies do not appear to share this interaction. Monitor therapy
PAZOPanib: BCRP/ABCG2 Inhibitors may increase the serum concentration of PAZOPanib. Avoid combination
Pentosan Polysulfate Sodium: May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Specifically, the risk of bleeding may be increased by concurrent use of these agents. Monitor therapy
Pentoxifylline: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Pioglitazone: CYP2C8 Inhibitors (Moderate) may increase the serum concentration of Pioglitazone. Monitor therapy
Prostacyclin Analogues: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Repaglinide: Clopidogrel may increase the serum concentration of Repaglinide. Management: Avoid use of clopidogrel and repaglinide if possible; if the combination must be used, limit total repaglinide daily dose to no more than 4 mg. This is contraindicated in some non-US labeling. Consider therapy modification
Ritonavir: May diminish the antiplatelet effect of Clopidogrel. Ritonavir may decrease serum concentrations of the active metabolite(s) of Clopidogrel. Monitor therapy
Rivaroxaban: Antiplatelet Agents (P2Y12 Inhibitors) may enhance the adverse/toxic effect of Rivaroxaban. Specifically, the risk of bleeding may be increased. Management: Carefully consider risks and benefits of this combination and monitor closely; Canadian labeling recommends avoiding prasugrel or ticagrelor. Consider therapy modification
Rosuvastatin: Clopidogrel may increase the serum concentration of Rosuvastatin. Monitor therapy
Salicylates: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Salicylates. Increased risk of bleeding may result. Monitor therapy
Selexipag: CYP2C8 Inhibitors (Moderate) may increase serum concentrations of the active metabolite(s) of Selexipag. Management: Reduce the selexipag dose to once daily when combined with moderate CYP2C8 inhibitors. Revert back to twice daily selexipag dosing upon stopping the moderate CYP2C8 inhibitor. Consider therapy modification
Sibutramine: CYP2B6 Inhibitors (Weak) may increase serum concentrations of the active metabolite(s) of Sibutramine. CYP2B6 Inhibitors (Weak) may increase the serum concentration of Sibutramine. Monitor therapy
Sodium Zirconium Cyclosilicate: May decrease serum concentrations of the active metabolite(s) of Clopidogrel. Management: Separate the administration of sodium zirconium cyclosilicate and clopidogrel by at least 2 hours. Consider therapy modification
Talazoparib: BCRP/ABCG2 Inhibitors may increase the serum concentration of Talazoparib. Monitor therapy
Thrombolytic Agents: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Thrombolytic Agents. Monitor therapy
Tipranavir: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Topotecan: BCRP/ABCG2 Inhibitors may increase the serum concentration of Topotecan. Avoid combination
Treprostinil: CYP2C8 Inhibitors (Moderate) may increase the serum concentration of Treprostinil. Monitor therapy
Ubrogepant: BCRP/ABCG2 Inhibitors may increase the serum concentration of Ubrogepant. Management: Use an initial ubrogepant dose of 50 mg and second dose (if needed) of 50 mg when used with a BCRP inhibitor. Consider therapy modification
Urokinase: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Urokinase. Avoid combination
Vitamin E (Systemic): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Warfarin: Clopidogrel may enhance the anticoagulant effect of Warfarin. Consider therapy modification
Zanubrutinib: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Adverse Reactions
As with all drugs that may affect hemostasis, bleeding is associated with clopidogrel. Hemorrhage may occur at virtually any site. Risk is dependent on multiple variables, including the concurrent use of multiple agents that alter hemostasis and patient susceptibility.
1% to 10%:
Hematologic & oncologic: Minor hemorrhage (4% to 5%), major hemorrhage (4%)
Frequency not defined:
Hematologic & oncologic: Bruise, hematoma
Respiratory: Epistaxis
<1%, postmarketing, and/or case reports: Abnormal hepatic function tests, acute generalized exanthematous pustulosis, acute hepatic failure, ageusia, agranulocytosis, angioedema, aplastic anemia, arthralgia, arthritis, bronchospasm, bullous rash, colitis (including ulcerative or lymphocytic), confusion, diarrhea, drug-induced hypersensitivity reaction, drug reaction with eosinophilia and systemic symptoms, duodenal ulcer, eczema, eosinophilic pneumonitis, erythema multiforme, erythematous rash, exfoliative dermatitis, fever, gastric ulcer, hallucination, headache, hemophilia A (acquired), hepatitis (noninfectious), hypersensitivity reaction, hypotension, increased serum creatinine, insulin autoimmune syndrome, interstitial pneumonitis, intracranial hemorrhage, lichen planus, maculopapular rash, myalgia, nonimmune anaphylaxis, pancreatitis, pancytopenia, pruritus, serum sickness, Stevens-Johnson syndrome, stomatitis, taste disorder, thrombotic thrombocytopenic purpura, toxic epidermal necrolysis, urticaria, vasculitis
Warnings/Precautions
Concerns related to adverse effects:
- Bleeding: Clopidogrel increases the risk of bleeding. Use is contraindicated in patients with active pathological bleeding (eg, peptic ulcer, intracranial hemorrhage). Additional risk factors for bleeding include age ≥75 years, propensity to bleed (eg, recent trauma or surgery, recent or recurrent GI bleeding, active peptic ulcer disease, severe hepatic impairment), body weight <60 kg, coronary artery bypass graft (CABG) or other surgical procedure, concomitant use of medications that increase risk of bleeding (eg, warfarin, nonsteroidal anti-inflammatory drugs). Use with caution in patients with platelet disorders, bleeding disorders, and/or at increased risk for bleeding. Bleeding should be suspected if patient becomes hypotensive, even if overt signs of bleeding do not exist. It may be possible to restore hemostasis by administering exogenous platelets; however, platelet transfusions within 4 hours of the clopidogrel loading dose or 2 hours of the maintenance dose may be less effective.
- Thienopyridine hypersensitivity: Because of structural similarities, cross-reactivity has been reported among the thienopyridines (clopidogrel, prasugrel, and ticlopidine); use with caution or avoid in patients with hypersensitivity or hematologic reactions to previous thienopyridine use. Use of clopidogrel is contraindicated in patients with hypersensitivity to clopidogrel. Although desensitization may be considered for mild to moderate hypersensitivity, do not desensitize patients with prior life-threatening allergic reactions to clopidogrel (eg, toxic epidermal necrolysis, exfoliative dermatitis, Stevens-Johnson syndrome, thrombotic thrombocytopenic purpura [TTP]) (Lokhandwala 2011).
- Thrombotic thrombocytopenic purpura: Cases of TTP (usually occurring within the first 2 weeks of therapy), resulting in some fatalities, have been reported; urgent plasmapheresis is required.
Disease-related concerns:
- Lacunar stroke: In patients with recent lacunar stroke (within 180 days), the use of clopidogrel in addition to aspirin did not significantly reduce the incidence of the primary outcome of stroke recurrence (any ischemic stroke or intracranial hemorrhage) compared to aspirin alone; the use of clopidogrel in addition to aspirin did, however, increase the risk of major hemorrhage and the rate of all-cause mortality (SPS3 Investigators 2012).
- Renal impairment: Use with caution in patients with moderate to severe renal impairment (experience is limited).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- CYP2C19 poor metabolizers: [US Boxed Warning]: Effectiveness of clopidogrel results from its antiplatelet activity, which is dependent on its conversion to an active metabolite by the CYP-450 system, principally CYP2C19. In patients who are homozygous for nonfunctional alleles of the CYP2C19 genes (termed “CYP2C19 poor metabolizers”), clopidogrel at recommended doses forms less of the active metabolite and has a reduced effect on platelet activity. Tests are available to identify patients who are CYP2C19 poor metabolizers. Consider use of another platelet P2Y12 inhibitor in patients identified as CYP2C19 poor metabolizers. Routine platelet function testing or genetic testing for CYP2C19 polymorphisms is not recommended (ACC/AHA [Levine 2016]; Scott 2013; Sibbing 2019).
- Lower GI bleed patients: An individualized and multidisciplinary approach should be utilized to determine therapy discontinuation and management in patients with acute lower GI bleed (LGIB) who are on antiplatelet medications; risk of ongoing bleeding should be weighed with risk of thromboembolic events. If antiplatelet agents are discontinued, they should generally be resumed as soon as possible and at least within 7 days, taking into account control of bleeding and cardiovascular risk. Aspirin should generally not be discontinued. Dual antiplatelet therapy (DAPT) should generally not be discontinued in the 90 days post-acute coronary syndrome or 30 days post-coronary stenting (Strate 2016).
- Surgical patients: In patients undergoing elective surgery, consider discontinuing 5 days before surgery (except in patients with cardiac stents that have not completed their full course of DAPT); patient-specific situations need to be discussed with cardiologist; AHA/ACC/SCAI/ACS/ADA Science Advisory provides recommendations) (Grines 2007). Elective noncardiac surgery should not be performed in patients in whom DAPT will need to be discontinued perioperatively within 30 days following bare metal stent (BMS) placement or within 12 months after drug-eluting stent (DES) placement. In patients undergoing urgent non-cardiac surgery during the first 4 to 6 weeks after BMS or DES placement, DAPT may be continued. In patients with stents undergoing surgery that requires discontinuation of the P2Y12 inhibitor, continue aspirin and re-start the P2Y12 inhibitor as soon as possible after surgery (ACC/AHA [Fleisher 2014]). In patients undergoing elective CABG, discontinue clopidogrel at least 5 days before procedure; when urgent CABG is necessary, the ACC/AHA CABG guidelines recommend discontinuation for at least 24 hours prior to surgery (ACC/AHA [Hillis 2011]). The ACC/AHA STEMI guidelines recommend discontinuation for at least 24 hours prior to on-pump CABG if possible; off-pump CABG may be performed within 24 hours of clopidogrel administration if the benefits of prompt revascularization outweigh the risks of bleeding (ACCF/AHA [O'Gara 2013]).
Other warnings/precautions:
- Coronary artery stents: Premature interruption of therapy may result in stent thrombosis with subsequent fatal and nonfatal MI. Duration of therapy, in general, is determined by the type of stent placed (bare metal or drug eluting) and whether an acute coronary syndrome event was ongoing at the time of placement (ACC/AHA [Levine 2016]; AHA/ACC/SCAI/ACS/ADA [Grines 2007]).
Monitoring Parameters
Signs of bleeding; hemoglobin and hematocrit periodically.
Pregnancy
Pregnancy Considerations
Information related to use during pregnancy is limited (Bauer 2012; De Santis 2011; Myers 2011). Based on available data, an increased risk of major birth defects, miscarriage, or adverse fetal outcomes has not been associated with maternal use of clopidogrel. According to the manufacturer, use should not be withheld if needed for emergent treatment of stroke or myocardial infarction during pregnancy. Discontinue use 5 to 7 days prior to labor, delivery, or neuraxial blockade if possible due to increased risk of maternal bleeding and hemorrhage.
Available guidelines recommend using clopidogrel only when strictly needed and for the shortest duration possible until additional fetal safety data are available (ESC [Regitz-Zagrosek 2018]).
Patient Education
What is this drug used for?
- It is used to lower the chance of heart attack or stroke.
- It may be given to you for other reasons. Talk with the doctor.
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding.
- Low blood sugar like dizziness, headache, fatigue, feeling weak, shaking, fast heartbeat, confusion, increased hunger, or sweating.
- Thrombotic thrombocytopenic purpura like confusion, severe fatigue, severe weakness, weakness on one side of body, difficulty speaking, difficulty thinking, balance changes, drooping on one side of face, vision changes, fast heartbeat, fever, headache, pale skin, unable to pass urine, blood in the urine, purple spots on skin or mouth, seizures, severe diarrhea, abdominal pain, nausea, vomiting, dyspnea, or yellow skin.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.