Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Generic: Colchicine 0.5 mg and probenecid 0.5 g
Use: Labeled Indications
Treatment of chronic gouty arthritis when complicated by frequent, recurrent acute attacks of gout
Contraindications
Hypersensitivity to colchicine, probenecid, or any component of the formulation; children <2 years of age; small- or large-dose aspirin therapy; blood dyscrasias; uric acid kidney stones; initiation during an acute gout attack; concomitant use of a P-glycoprotein (P-gp) or strong CYP3A4 inhibitor in presence of renal or hepatic impairment
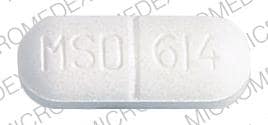
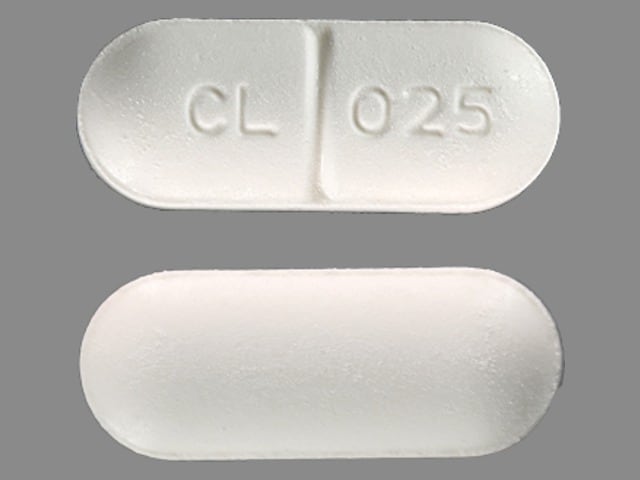
Colchicine and Probenecid Images
Dosage and Administration
Dosing: Adult
Gout: Oral: Colchicine 0.5 mg and probenecid 0.5 g: One tablet once daily for 1 week, then 1 tablet twice daily thereafter
Note: Current prescribing information states a maximum dose of 4 tablets per day; however this exceeds the usual maximum dose of colchicine for gout prophylaxis (1.2 mg per day).
Dosing: Geriatric
Refer to adult dosing.
Administration
Do not initiate therapy until acute attack has subsided.
Drug Interactions
Acetaminophen: Probenecid may increase the serum concentration of Acetaminophen. Probenecid may also limit the formation of at least one major non-toxic metabolite, possibly increasing the potential for formation of the toxic NAPQI metabolite. Consider therapy modification
Anagliptin: Probenecid may increase the serum concentration of Anagliptin. Monitor therapy
Antihepaciviral Combination Products: May increase the serum concentration of Colchicine. Avoid combination
Avibactam: Probenecid may increase the serum concentration of Avibactam. Avoid combination
Baricitinib: Probenecid may increase the serum concentration of Baricitinib. Management: Decrease the dose of baricitinib to 1 mg daily when combined with probenecid. Consider therapy modification
Betalactamase Inhibitors: Probenecid may increase the serum concentration of Betalactamase Inhibitors. Management: Coadministration of probenecid with amoxicillin/clavulanate is not recommended per official package labeling. Exceptions: Avibactam; Sulbactam. Consider therapy modification
Cabozantinib: MRP2 Inhibitors may increase the serum concentration of Cabozantinib. Monitor therapy
Cefotaxime: Probenecid may increase the serum concentration of Cefotaxime. Management: Avoid cefotaxime doses greater than 6 g/day with concurrent probenecid. Any patients receiving this combination should be monitored closely for evidence of cefotaxime toxicity. Consider therapy modification
Cephalosporins: Probenecid may increase the serum concentration of Cephalosporins. Monitor therapy
Choline C 11: Colchicine may diminish the therapeutic effect of Choline C 11. Monitor therapy
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Cyanocobalamin: Colchicine may decrease the serum concentration of Cyanocobalamin. Monitor therapy
CYP3A4 Inhibitors (Moderate): May increase the serum concentration of Colchicine. Management: Reduce colchicine dose as directed when using with a moderate CYP3A4 inhibitor, and increase monitoring for colchicine-related toxicity. See full monograph for details. Use extra caution in patients with impaired renal and/or hepatic function. Consider therapy modification
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Colchicine. Management: Colchicine is contraindicated in patients with impaired renal or hepatic function who are also receiving a strong CYP3A4 inhibitor. In those with normal renal and hepatic function, reduce colchicine dose as directed. See full monograph for details. Consider therapy modification
Dapsone (Systemic): Probenecid may increase the serum concentration of Dapsone (Systemic). Monitor therapy
Deferiprone: UGT1A6 Inhibitors may increase the serum concentration of Deferiprone. Avoid combination
Dexketoprofen: Probenecid may increase the serum concentration of Dexketoprofen. Monitor therapy
Dichlorphenamide: OAT1/3 Inhibitors may increase the serum concentration of Dichlorphenamide. Monitor therapy
Digoxin: May increase the serum concentration of Colchicine. Monitor therapy
Doripenem: Probenecid may increase the serum concentration of Doripenem. This effect is due to probenecid's ability to decrease the active tubular secretion of doripenem. Avoid combination
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Erdafitinib: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Ertapenem: Probenecid may increase the serum concentration of Ertapenem. Monitor therapy
Fibric Acid Derivatives: May enhance the myopathic (rhabdomyolysis) effect of Colchicine. Monitor therapy
Fosamprenavir: May increase the serum concentration of Colchicine. Management: Colchicine is contraindicated in patients with impaired renal or hepatic function who are receiving ritonavir-boosted fosamprenavir. In those with normal renal and hepatic function, reduce colchicine dose as directed. Consider therapy modification
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ganciclovir-Valganciclovir: Probenecid may increase the serum concentration of Ganciclovir-Valganciclovir. Monitor therapy
Gemifloxacin: Probenecid may increase the serum concentration of Gemifloxacin. Monitor therapy
Grapefruit Juice: May increase the serum concentration of Colchicine. Avoid combination
HMG-CoA Reductase Inhibitors (Statins): Colchicine may enhance the myopathic (rhabdomyolysis) effect of HMG-CoA Reductase Inhibitors (Statins). Colchicine may increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Consider therapy modification
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Imipenem: Probenecid may increase the serum concentration of Imipenem. Monitor therapy
Ketoprofen: Probenecid may increase the serum concentration of Ketoprofen. Monitor therapy
Ketorolac (Nasal): Probenecid may increase the serum concentration of Ketorolac (Nasal). Avoid combination
Ketorolac (Systemic): Probenecid may increase the serum concentration of Ketorolac (Systemic). Avoid combination
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Lasmiditan: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Avoid combination
Loop Diuretics: Probenecid may enhance the adverse/toxic effect of Loop Diuretics. Probenecid may diminish the diuretic effect of Loop Diuretics. Probenecid may increase the serum concentration of Loop Diuretics. Management: Monitor for decreased diuretic effects or increased adverse effects of loop diuretics with concomitant use of probenecid. Bumetanide prescribing information recommends against concomitant use of probenecid. Monitor therapy
LORazepam: Probenecid may increase the serum concentration of LORazepam. Consider therapy modification
Lumacaftor and Ivacaftor: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. Lumacaftor and Ivacaftor may increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Lumateperone: Probenecid may increase the serum concentration of Lumateperone. Avoid combination
Meropenem: Probenecid may increase the serum concentration of Meropenem. Avoid combination
Methotrexate: Probenecid may increase the serum concentration of Methotrexate. Management: Avoid concomitant use of probenecid and methotrexate if possible. If used together, consider lower methotrexate doses and monitor for evidence of methotrexate toxicity. Consider therapy modification
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Minoxidil (Systemic): Probenecid may increase the serum concentration of Minoxidil (Systemic). Monitor therapy
Multivitamins/Fluoride (with ADE): Colchicine may decrease the serum concentration of Multivitamins/Fluoride (with ADE). Specifically, colchicine may decrease absorption of cyanocobalamin (vitamin B12). Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): Colchicine may decrease the serum concentration of Multivitamins/Minerals (with ADEK, Folate, Iron). Specifically, colchicine may decrease the serum concentration of Cyanocobalamin. Monitor therapy
Multivitamins/Minerals (with AE, No Iron): Colchicine may decrease the serum concentration of Multivitamins/Minerals (with AE, No Iron). Specifically, colchicine may decrease absorption of cyanocobalamin (vitamin B12). Monitor therapy
Mycophenolate: Probenecid may increase the serum concentration of Mycophenolate. Monitor therapy
Nitrofurantoin: Probenecid may increase the serum concentration of Nitrofurantoin. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents: Probenecid may increase the serum concentration of Nonsteroidal Anti-Inflammatory Agents. Monitor therapy
Oseltamivir: Probenecid may increase serum concentrations of the active metabolite(s) of Oseltamivir. Management: Consider a change in therapy when using oseltamivir together with probenecid; reduced oseltamivir dose may be necessary. Increase monitoring for adverse events, such as thrombocytopenia. Consider therapy modification
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Pegloticase: Probenecid may enhance the adverse/toxic effect of Pegloticase. Specifically, Probenecid may blunt increases in serum urate that would signal an elevated risk of anaphylaxis and infusion reactions. Avoid combination
Penicillins: Probenecid may increase the serum concentration of Penicillins. Monitor therapy
Pexidartinib: UGT1A4 Inhibitors may increase the serum concentration of Pexidartinib. Management: Avoid use of UGT1A4 inhibitors and pexidartinib. If combined use is required, reduce the pexidartinib dose. If receving pexidartinib 800 mg or 600 mg daily, reduce to 200 mg twice daily. If receiving 400 mg/day, reduce to 200 mg/day. Consider therapy modification
P-glycoprotein/ABCB1 Inducers: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inducers may also further limit the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
P-glycoprotein/ABCB1 Inhibitors: May increase the serum concentration of Colchicine. Colchicine distribution into certain tissues (e.g., brain) may also be increased. Management: Colchicine is contraindicated in patients with impaired renal or hepatic function who are also receiving a p-glycoprotein inhibitor. In those with normal renal and hepatic function, reduce colchicine dose as directed. See full monograph for details. Consider therapy modification
PRALAtrexate: Probenecid may increase the serum concentration of PRALAtrexate. Monitor therapy
Propacetamol: Probenecid may increase serum concentrations of the active metabolite(s) of Propacetamol. Specifically, accetaminophen exposure may be increased. Probenecid may also limit the formation of at least one major non-toxic acetaminophen metabolite, possibly increasing the formation of the toxic NAPQI metabolite. Management: Consider limiting the use of propacetamide in patients who are also taking probenecid. Patients may be at an increased risk for toxicity, even if reduced propacetamide doses are used. Consider therapy modification
Quinolones: Probenecid may decrease the excretion of Quinolones. Specifically, probenecid may decreased the renal excretion of quinolone antibiotics. Probenecid may increase the serum concentration of Quinolones. Exceptions: Moxifloxacin (Systemic). Monitor therapy
Salicylates: May diminish the therapeutic effect of Probenecid. Monitor therapy
Sodium Benzoate: Probenecid may increase the serum concentration of Sodium Benzoate. Specifically, probenecid may inhibit the renal transport of the hippuric acid metabolite of sodium benzoate. Monitor therapy
Sodium Phenylacetate: Probenecid may increase the serum concentration of Sodium Phenylacetate. Specifically, probenecid may inhibit the renal transport of the phenylacetylglutamine metabolite of sodium phenylacetate. Monitor therapy
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Sulfonylureas: Probenecid may decrease the protein binding of Sulfonylureas. Probenecid may increase the serum concentration of Sulfonylureas. Monitor therapy
Tacrolimus (Systemic): May increase the serum concentration of Colchicine. Monitor therapy
Theophylline Derivatives: Probenecid may increase the serum concentration of Theophylline Derivatives. Exceptions: Aminophylline; Theophylline. Monitor therapy
Tipranavir: May increase the serum concentration of Colchicine. Management: Colchicine should not be used with tipranavir in patients with impaired renal or hepatic function. In those with normal renal and hepatic function, reduced colchicine doses (as directed) are required if used with tipranavir. Consider therapy modification
Urea Cycle Disorder Agents: Probenecid may increase serum concentrations of the active metabolite(s) of Urea Cycle Disorder Agents. Specifically, concentrations of phenylacetate and phenylacetylglutamine may be increased. Monitor therapy
Zidovudine: Probenecid may decrease the metabolism of Zidovudine. Monitor therapy
Adverse Reactions
See individual agents.
Warnings/Precautions
See individual agents.
Monitoring Parameters
CBC, renal function, serum uric acid, urinary uric acid, frequency of gout attacks (Khanna 2012).
Pregnancy
Pregnancy Considerations
See individual agents.
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience dizziness, headache, flushing, lack of appetite, or hair loss. Have patient report immediately to prescriber signs of infection, signs of liver problems (dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin), burning or numbness feeling, severe nausea, vomiting, severe diarrhea, signs of a kidney stone (back pain, abdominal pain, or blood in the urine), unable to pass urine, change in amount of urine passed, bruising, bleeding, severe loss of strength and energy, pale skin, muscle pain, or muscle weakness (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for health care professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience, and judgment in diagnosing, treating, and advising patients.