Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Packet, Oral, as hydrochloride:
Welchol: 3.75 g (30 ea) [sugar free; contains aspartame]
Generic: 3.75 g (30 ea)
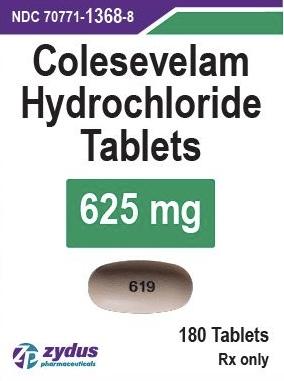
Tablet, Oral, as hydrochloride:
Welchol: 625 mg
Generic: 625 mg
Pharmacology
Mechanism of Action
Cholesterol is the major precursor of bile acid. Colesevelam binds with bile acids in the intestine to form an insoluble complex that is eliminated in feces. This increased excretion of bile acids results in an increased oxidation of cholesterol to bile acid and a lowering of the serum cholesterol.
Pharmacokinetics/Pharmacodynamics
Absorption
None
Excretion
Urine (0.05%)
Onset of Action
Lipid lowering: Therapeutic: ~2 weeks
Reduction of hemoglobin A1C (Type II diabetes): 4-6 weeks initial onset; 12-18 weeks maximal effect
Use: Labeled Indications
Diabetes mellitus, type 2: Improve glycemic control in adults with type 2 diabetes mellitus in conjunction with diet and exercise
Guideline recommendations: Colesevelam is not generally used in patients with type 2 diabetes but may be tried in specific situations (ADA 2019).
Hyperlipidemia (primary):
Management of elevated LDL-C in adults with primary hyperlipidemia in conjunction with diet and exercise.
Management of heterozygous familial hypercholesterolemia (heFH) in adolescent patients (males and postmenarcheal females 10 to 17 years of age) who are unable to reach LDL-C target levels despite an adequate trial of dietary therapy and lifestyle modification.
Use: Off Label
Diarrhea associated with bile acid malabsorptionc
Data from a systematic review and a small randomized, double-blind, placebo-controlled trial in patients with Crohn disease suggest colesevelam may be beneficial as alternative treatment of diarrhea associated with bile acid malabsorption in patients who are intolerant or unresponsive to other bile acid sequestrants Beigel 2014, Wilcox 2014.
Contraindications
History of bowel obstruction; serum TG concentrations of more than 500 mg/dL; history of hypertriglyceridemia-induced pancreatitis.
Canadian labeling: Additional contraindications (not in US labeling): Hypersensitivity to colesevelam or any component of the formulation; biliary obstruction
Dosage and Administration
Dosing: Adult
Diarrhea associated with bile acid malabsorption (off-label use): Oral: 3.75 g/day in 1 or 2 divided doses (Beigel 2014; Wilcox 2014)
Hyperlipidemia (primary), diabetes mellitus (type 2): Oral: 3.75 g/day in 1 or 2 divided doses
Note: Use may be considered in patients with fasting triglyceride level ≤300 mg/dL who do not meet cholesterol treatment goals with dietary modification and other lipid lowering therapies (eg, maximally tolerated statin and ezetimibe) (AHA/ACC [Grundy 2018]).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Due to large tablet size, the manufacturer recommends packets of oral suspension or chewable bars for pediatric patients. Overall with dyslipidemia management, lifestyle changes are recommended to be implemented for at least 6 to 12 months before beginning pharmacotherapy (AACE [Jellinger 2017]). Bile acid sequestrant therapy may be considered for LDL/apo B reduction and mild HDL increases but should not be used in pediatric patients with hypertriglyceridemia. Multivitamin supplementation recommended due to potential folic acid and cholecalciferol malabsorption (AACE [Jellinger 2017]).
Heterozygous familial hypercholesterolemia: Children ≥10 years and Adolescents: Oral: 3.75 g once daily or in divided doses twice daily.
Reconstitution
Granules for oral suspension: Empty 1 packet into a glass or cup; add 1 cup (8 ounces) of water, fruit juice, or a diet soft drink and mix well.
Administration
Chewable bars: Administer with meal(s).
Granules for oral suspension: Administer with meal(s). Powder is not to be taken in dry form (to avoid esophageal distress).
Tablets: Administer with meal(s) and a liquid. Due to tablet size, it is recommended that any patient who has trouble swallowing tablets should use the oral suspension form.
Dietary Considerations
Some products may contain phenylalanine. Each chewable bar contains ~80 calories.
Storage
Store at 25°C (77°F). Excursions permitted to 15°C to 30°C (59°F to 86°F); brief excursions permitted to 40°C (104°F) (tablets only). Protect from moisture.
Colesevelam Images
Drug Interactions
Amiodarone: Bile Acid Sequestrants may decrease the bioavailability of Amiodarone. Consider therapy modification
Chenodiol: Bile Acid Sequestrants may decrease the serum concentration of Chenodiol. Management: Administration of chenodiol 5 hours or more after bile acid sequestrants may reduce chenodiol adsorption in the gastrointestinal tract. Monitor for decreased therapeutic effects of chenodiol in patients receiving bile acid sequestrants. Consider therapy modification
Cholic Acid: Bile Acid Sequestrants may decrease the absorption of Cholic Acid. Management: Administer cholic acid at least 1 to 4 hours before or 4 to 6 hours after administration of any bile acid-binding products to minimize the potential for a significant interaction. Consider therapy modification
Corticosteroids (Oral): Bile Acid Sequestrants may decrease the absorption of Corticosteroids (Oral). Monitor therapy
CycloSPORINE (Systemic): Colesevelam may decrease the serum concentration of CycloSPORINE (Systemic). Management: Administer cyclosporine at least 4 hours prior to colesevelam. Monitor for decreased cyclosporine concentrations during concomitant colesevelam therapy. Consider therapy modification
Deferasirox: Bile Acid Sequestrants may decrease the serum concentration of Deferasirox. Management: Avoid combination when possible; if the combination must be used, consider a 50% increase in initial deferasirox dose, with monitoring of serum ferritin concentrations and clinical responses to guide further dosing. Consider therapy modification
Estrogen Derivatives (Contraceptive): Bile Acid Sequestrants may decrease the serum concentration of Estrogen Derivatives (Contraceptive). Management: Administer estrogen-based oral contraceptives at least 1 to 4 hours prior to or 4 to 6 hours after administration of a bile acid sequestrant. Consider therapy modification
Ethinyl Estradiol: Colesevelam may decrease the serum concentration of Ethinyl Estradiol. Management: Oral contraceptives containing ethinyl estradiol and norethindrone should be administered at least 4 hours before colesevelam. Consider therapy modification
Ezetimibe: Bile Acid Sequestrants may decrease the absorption of Ezetimibe. Management: Administer ezetimibe at least 2 hours before or 4 hours after any bile acid sequestrant. Consider therapy modification
Glimepiride: Colesevelam may decrease the serum concentration of Glimepiride. Management: Administer glimepiride at least 4 hours prior to colesevelam. Consider therapy modification
GlipiZIDE: Colesevelam may decrease the serum concentration of GlipiZIDE. Management: Administer glipizide at least 4 hours prior to colesevelam. Consider therapy modification
GlyBURIDE: Colesevelam may decrease the serum concentration of GlyBURIDE. Management: Administer glyburide at least 4 hours prior to colesevelam. Consider therapy modification
Leflunomide: Bile Acid Sequestrants may decrease serum concentrations of the active metabolite(s) of Leflunomide. Management: Unless using this combination to intentionally enhance leflunomide elimination, consider an alternative to the bile acid sequestrants when possible. Separating drug administration is not likely to be effective at avoiding this interaction. Consider therapy modification
Lomitapide: Bile Acid Sequestrants may decrease the absorption of Lomitapide. Management: Administer lomitapide at least 4 hours before or after administration of a bile acid sequestrant. Consider therapy modification
Loop Diuretics: Bile Acid Sequestrants may decrease the absorption of Loop Diuretics. Consider therapy modification
Methotrexate: Bile Acid Sequestrants may decrease the absorption of Methotrexate. Monitor therapy
Multivitamins/Fluoride (with ADE): Bile Acid Sequestrants may decrease the serum concentration of Multivitamins/Fluoride (with ADE). Management: Avoid concomitant administration of multivitamins and bile acid sequestrants (eg, cholestyramine). Separate administration of these agents by several hours to minimize the risk of an interaction. Consider therapy modification
Multivitamins/Minerals (with ADEK, Folate, Iron): Bile Acid Sequestrants may decrease the serum concentration of Multivitamins/Minerals (with ADEK, Folate, Iron). Specifically, bile acid sequestrants may impair the absorption of fat-soluble vitamins. Management: Avoid concomitant administration of multivitamins and bile acid sequestrants (eg, cholestyramine). Separate administration of these agents by several hours to minimize the risk of an interaction. Consider therapy modification
Multivitamins/Minerals (with AE, No Iron): Bile Acid Sequestrants may decrease the serum concentration of Multivitamins/Minerals (with AE, No Iron). Management: Avoid concomitant administration of multivitamins and bile acid sequestrants (e.g., cholestyramine). Separate administration of these agents by several hours to minimize the risk of an interaction. Consider therapy modification
Mycophenolate: Bile Acid Sequestrants may decrease the serum concentration of Mycophenolate. Avoid combination
Niacin: Bile Acid Sequestrants may decrease the absorption of Niacin. Consider therapy modification
Nonsteroidal Anti-Inflammatory Agents: Bile Acid Sequestrants may decrease the absorption of Nonsteroidal Anti-Inflammatory Agents. Consider therapy modification
Norethindrone: Colesevelam may decrease the serum concentration of Norethindrone. Management: Oral contraceptives containing ethinyl estradiol and norethindrone should be administered at least 4 hours before colesevelam. Consider therapy modification
Obeticholic Acid: Bile Acid Sequestrants may decrease the serum concentration of Obeticholic Acid. Management: Administer obeticholic acid at least 4 hours before or at least 4 hours after the administration of bile acid sequestrants. Consider therapy modification
Olmesartan: Colesevelam may decrease the serum concentration of Olmesartan. Management: Administer olmesartan at least 4 hours prior to colesevelam. Consider therapy modification
Phenytoin: Colesevelam may decrease the serum concentration of Phenytoin. Management: Administer phenytoin at least 4 hours prior to colesevelam. Consider therapy modification
Pravastatin: Bile Acid Sequestrants may decrease the serum concentration of Pravastatin. Management: Administer pravastatin at least 1 hour before or 4 hours after administration of bile-acid resins (eg, cholestyramine, colestipol, colesevelam) to minimize the risk for any significant interaction. Consider therapy modification
Progestins (Contraceptive): Bile Acid Sequestrants may decrease the serum concentration of Progestins (Contraceptive). Management: Administer oral progestin-containing contraceptives at least 1 to 4 hours prior to or 4 to 6 hours after administration of a bile acid sequestrant. Consider therapy modification
Propranolol: Bile Acid Sequestrants may decrease the serum concentration of Propranolol. Monitor therapy
Raloxifene: Bile Acid Sequestrants may decrease the absorption of Raloxifene. Consider therapy modification
Teriflunomide: Bile Acid Sequestrants may decrease the serum concentration of Teriflunomide. Management: Unless using this combination to intentionally enhance teriflunomide elimination, consider an alternative to the bile acid sequestrants when possible. Separating drug administration is unlikely to be effective at avoiding the interaction. Consider therapy modification
Tetracyclines: Bile Acid Sequestrants may decrease the absorption of Tetracyclines. Exceptions: Eravacycline. Consider therapy modification
Thiazide and Thiazide-Like Diuretics: Bile Acid Sequestrants may decrease the absorption of Thiazide and Thiazide-Like Diuretics. The diuretic response is likewise decreased. Consider therapy modification
Thyroid Products: Bile Acid Sequestrants may decrease the serum concentration of Thyroid Products. Management: Administer oral thyroid products at least 4 h prior to colesevelam, and at least 1 h before or 4-6 h after cholestyramine. Specific recommendations for colestipol are not available. Monitor for decreased concentrations/effects of the thyroid product. Consider therapy modification
Ursodiol: Bile Acid Sequestrants may decrease the serum concentration of Ursodiol. Management: Administer ursodiol 2 to 4 hours before or at least 2 to 5 hours after bile acid sequestrants to minimize the potential for any significant interaction. Monitor for decreased therapeutic effects of ursodiol in patients receiving bile acid sequestrants. Consider therapy modification
Vancomycin: Bile Acid Sequestrants may diminish the therapeutic effect of Vancomycin. Management: Avoid concurrent administration of oral vancomycin and bile acid sequestrants when possible. If use of both agents is necessary, consider separating doses by at least 2 hours to minimize the significance of the interaction. Consider therapy modification
Vitamin D Analogs: Bile Acid Sequestrants may decrease the serum concentration of Vitamin D Analogs. More specifically, bile acid sequestrants may impair absorption of Vitamin D Analogs. Management: Avoid concomitant administration of vitamin D analogs and bile acid sequestrants (eg, cholestyramine). Separate administration of these agents by several hours to minimize the potential risk of interaction. Monitor plasma calcium concentrations. Exceptions: Calcipotriene; Calcitriol (Topical); Tacalcitol. Consider therapy modification
Vitamin K Antagonists (eg, warfarin): Bile Acid Sequestrants may decrease the absorption of Vitamin K Antagonists. Monitor therapy
Test Interactions
Increased prothrombin time
Adverse Reactions
Actual frequency may be dependent upon indication. Unless otherwise noted, frequency of adverse effects is reported for adult patients.
>10%: Gastrointestinal: Constipation (3% to 11%)
1% to 10%:
Cardiovascular: Cardiovascular toxicity (2%, including myocardial infarction, aortic stenosis, bradycardia), hypertension (2% to 3%)
Central nervous system: Headache (children and adults 4% to 8%), fatigue (children 4%)
Endocrine & metabolic: Hypertriglyceridemia (4% to 5%; >500 mg/dL: <1%; >1,000 mg/dL: <1%), hyperglycemia (3%), hypoglycemia (3%)
Gastrointestinal: Dyspepsia (3% to 8%), diarrhea (4%), nausea (children and adults 3% to 4%), gastroesophageal reflux disease (2%), periodontal abscess (2%), vomiting (children 2%)
Hematologic & oncologic: C-reactive protein increased (3%)
Infection: Influenza (children and adolescents 4%)
Neuromuscular & skeletal: Weakness (4%), back pain (2%), increased creatine phosphokinase (children and adults 2%), myalgia (2%)
Respiratory: Nasopharyngitis (children 5% to 6%), upper respiratory tract infection (children and adults 3% to 5%), flu-like symptoms (children 4%), pharyngitis (3%), rhinitis (children 2%)
<1%, postmarketing, and/or case reports: Abdominal distension, dysphagia, esophageal obstruction, fecal impaction, flatulence, worsening of hemorrhoids, increased serum transaminases, infection, intestinal obstruction, pancreatitis, unstable angina pectoris
Warnings/Precautions
Disease-related concerns:
- Gastrointestinal disease: Use is not recommended in patients with gastroparesis, other severe GI motility disorders, a history of major GI tract surgery, or patients at risk for bowel obstruction. Use tablets with caution in patients with dysphagia or swallowing disorders; use the oral suspension form of colesevelam due to large tablet size and risk for esophageal obstruction. Discontinue if symptoms of bowel obstruction occur (eg, severe abdominal pain, severe constipation).
- Hypertriglyceridemia: Bile acid sequestrants can increase serum triglyceride concentrations; severely elevated triglycerides can cause acute pancreatitis. The manufacturer contraindicates use if triglycerides exceed 500 mg/dL and in patients with a history of hypertriglyceridemia-induced pancreatitis. The American College of Cardiology/American Heart Association recommends avoiding use in patients with baseline fasting triglyceride levels ≥300 mg/dL (ACC/AHA [Grundy 2018]). Use with caution in patients using insulin, thiazolidinediones, or sulfonylureas (may cause increased triglyceride concentrations). Discontinue if symptoms of acute pancreatitis occur (eg, severe abdominal pain with or without nausea and vomiting).
- Patients susceptible to fat-soluble vitamin deficiencies: Use with caution in patients susceptible to fat-soluble vitamin deficiencies. Absorption of fat soluble vitamins A, D, E, and K may be decreased; patients should take vitamins ≥4 hours before colesevelam.
- Phenylketonuria: Some products may contain phenylalanine; use with caution.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Phenylalanine: Some products may contain phenylalanine.
Other warnings/precautions:
- Appropriate use: Primary hyperlipidemia: Has not been studied in types I, III, IV, and V dyslipidemias. Diabetes: Not for use in patients with diabetic ketoacidosis (DKA) or patients with type 1 diabetes mellitus.
Monitoring Parameters
Lipid profile (fasting or nonfasting) should be rechecked 4 to 12 weeks after starting therapy and every 3 to 12 months thereafter (AHA/ACC [Grundy 2018])
Diabetes mellitus, type 2: Serum glucose and HbA1c (at least twice yearly in patients who have stable glycemic control and are meeting treatment goals; quarterly in patients not meeting treatment goals or with therapy change [ADA 2019])
Pregnancy
Pregnancy Considerations
Colesevelam is not absorbed systemically following oral administration and maternal use is not expected to result in fetal exposure to the drug.
Lipid concentrations increase during pregnancy as required for normal fetal development. When increases are greater than expected, supervised dietary intervention should be initiated. Bile acid sequestrants are recommended when treatment is needed, and therapy with colesevelam is preferred (Avis 2009; Jacobson 2015).
Colesevelam may interfere with maternal vitamin absorption; therefore, regular supplementation may not be adequate.
Colesevelam may reduce the efficacy of oral contraception; administer oral contraceptives at least 4 hours prior to colesevelam.
Patient Education
What is this drug used for?
- It is used to lower cholesterol.
- It is used to lower blood sugar in patients with high blood sugar (diabetes).
Frequently reported side effects of this drug
- Headache
- Heartburn
- Sore throat
- Stuffy nose
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Pancreatitis like severe abdominal pain, severe back pain, severe nausea, or vomiting
- Severe constipation
- Severe abdominal pain
- Difficulty swallowing
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.