Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Syrup, Oral:
Clarinex: 0.5 mg/mL (473 mL [DSC]) [contains edetate disodium, fd&c yellow #6 (sunset yellow), propylene glycol, sodium benzoate; bubble-gum flavor]
Tablet, Oral:
Clarinex: 5 mg [contains fd&c blue #2 aluminum lake]
Generic: 5 mg
Tablet Disintegrating, Oral:
Generic: 2.5 mg, 5 mg
Pharmacology
Mechanism of Action
Desloratadine, a major active metabolite of loratadine, is a long-acting tricyclic antihistamine with selective peripheral histamine H1 receptor antagonistic activity.
Pharmacokinetics/Pharmacodynamics
Metabolism
Hepatic to active metabolite, 3-hydroxydesloratadine (specific enzymes not identified); subsequently undergoes glucuronidation. Decreased in slow metabolizers of desloratadine. Not expected to affect or be affected by medications metabolized by CYP with normal doses.
Excretion
Urine (87%) and feces (as metabolites)
Onset of Action
Within 1 hour
Time to Peak
Children 2 to 5 years: Mean: 3.17 hours (range: 1.5 to 8 hours) (Gupta 2007).
Children 6 to 11 years: Mean: 3.57 hours (range: 4 to 12 hours) (Gupta 2007).
Adults: 3 hours.
Duration of Action
24 hours
Half-Life Elimination
Children 2 to 5 years: Mean: 16.4 hours (Gupta 2007).
Children 6 to 11 years: Mean: 19.4 hours (Gupta 2007).
Adults: 27 hours.
Protein Binding
Desloratadine: 82% to 87%; 3-hydroxydesloratadine (active metabolite): 85% to 89%
Use in Specific Populations
Special Populations: Renal Function Impairment
AUC and Cmax are increased.
Special Populations: Hepatic Function Impairment
AUC and half-life are increased.
Special Populations: Elderly
Cmax and AUC are 20% higher. The half-life is 33.7 hours.
Special Populations: Children
Systemic exposure in children (based on AUC and Cmax) is similar to adults (Gupta 2007).
Use: Labeled Indications
Allergic rhinitis: Relief of nasal and non-nasal symptoms of seasonal (SAR) and perennial (PAR) allergic rhinitis
Urticaria: Symptomatic relief of pruritus, reduction in number of hives, and reduction in size of hives associated with chronic idiopathic urticaria (CIU)
Use: Off Label
NSAID-associated urticaria (prophylaxis)c
Data from a retrospective study with a limited number of patients suggest that desloratadine may be beneficial for prophylactic therapy in patients with NSAID-associated urticaria prior to receiving a strong COX-1 inhibitor. Additional trials may be needed to further define the role of desloratadine in this setting Trautmann 2016.
Contraindications
Hypersensitivity to desloratadine, loratadine, or any component of the formulation
Dosage and Administration
Dosing: Adult
Chronic idiopathic urticaria: Oral: 5 mg once daily. In one clinical trial, the titrated use of higher doses (up to 10 mg twice daily) in adults demonstrated clinical improvement (Staevska 2010).
Seasonal or perennial allergic rhinitis: Oral: 5 mg once daily
NSAID-associated urticaria, prophylaxis (off-label use): Oral: 5 mg 30 minutes before intake of a strong COX-1 inhibitor (Trautmann 2016).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Perennial allergic rhinitis: Oral:
Infants 6 to ≤11 months: 1 mg once daily.
Children ≤5 years: 1.25 mg once daily.
Children 6 to ≤11 years: 2.5 mg once daily.
Children ≥12 years and Adolescents: 5 mg once daily.
Seasonal allergic rhinitis: Oral:
Children 2 to ≤5 years: 1.25 mg once daily.
Children 6 to ≤11 years: 2.5 mg once daily.
Children ≥12 years and Adolescents: 5 mg once daily.
Urticaria, chronic idiopathic: Oral:
Infants 6 to ≤11 months: 1 mg once daily.
Children ≤5 years: 1.25 mg once daily.
Children 6 to ≤11 years: 2.5 mg once daily.
Children ≥12 years and Adolescents: 5 mg once daily.
Administration
May be taken with or without food.
RediTabs should be placed on the tongue; tablet will disintegrate immediately. Take immediately after removing from blister package. Allow tablet to dissolve completely before swallowing. May be taken with or without water.
Dietary Considerations
Some products may contain phenylalanine.
Storage
Syrup, tablet, orally-disintegrating tablet: Store at 25°C (77°F); excursions permitted between 15°C to 30°C (59°F to 85°F). Protect from moisture and excessive heat. Use orally-disintegrating tablet immediately after opening blister package. Syrup should be protected from light.
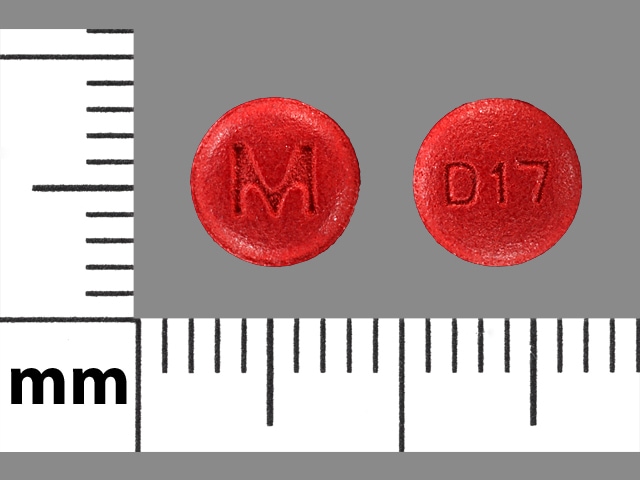
Desloratadine Images
Drug Interactions
Alcohol (Ethyl): CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Amezinium: Antihistamines may enhance the stimulatory effect of Amezinium. Monitor therapy
Amphetamines: May diminish the sedative effect of Antihistamines. Monitor therapy
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Benzylpenicilloyl Polylysine: Antihistamines may diminish the diagnostic effect of Benzylpenicilloyl Polylysine. Management: Suspend systemic H1 antagonists for benzylpenicilloyl-polylysine skin testing and delay testing until systemic antihistaminic effects have dissipated. A histamine skin test may be used to assess persistent antihistaminic effects. Consider therapy modification
Betahistine: Antihistamines may diminish the therapeutic effect of Betahistine. Monitor therapy
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
CYP2C8 Inhibitors (Moderate): May increase the serum concentration of Desloratadine. Monitor therapy
CYP2C8 Inhibitors (Strong): May increase the serum concentration of Desloratadine. Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Erdafitinib: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
Hyaluronidase: Antihistamines may diminish the therapeutic effect of Hyaluronidase. Management: Patients receiving antihistamines (particularly at larger doses) may not experience the desired clinical response to standard doses of hyaluronidase. Larger doses of hyaluronidase may be required. Consider therapy modification
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Lasmiditan: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Avoid combination
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Lumacaftor and Ivacaftor: May decrease the serum concentration of CYP2C8 Substrates (High Risk with Inhibitors or Inducers). Lumacaftor and Ivacaftor may increase the serum concentration of CYP2C8 Substrates (High Risk with Inhibitors or Inducers). Monitor therapy
Lumacaftor and Ivacaftor: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. Lumacaftor and Ivacaftor may increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
P-glycoprotein/ABCB1 Inducers: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inducers may also further limit the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
P-glycoprotein/ABCB1 Inhibitors: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inhibitors may also enhance the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pitolisant: Antihistamines may diminish the therapeutic effect of Pitolisant. Avoid combination
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
Ranolazine: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Test Interactions
May suppress the wheal and flare reactions to skin test antigens
Adverse Reactions
>10%:
Central nervous system: Headache (14%), irritability (infants: 12%)
Gastrointestinal: Diarrhea (infants: 15% to 20%)
Respiratory: Upper respiratory tract infection (infants: 11% to 21%), cough (infants: 11%)
Miscellaneous: Fever (infants: 12% to 17%)
1% to 10%:
Central nervous system: Drowsiness (infants: 9%), insomnia (infants: 5%), fatigue (2% to 5%), dizziness (4%), emotional lability (infants: 3%)
Dermatologic: Erythema of skin (infants: 3%), maculopapular rash (infants: 3%)
Gastrointestinal: Vomiting (infants: 6%), anorexia (infants: 5%), nausea (infants and children: 3% to 5%), dyspepsia (3%), increased appetite (infants: 3%), xerostomia (adults: 3%)
Genitourinary: Urinary tract infection (children: 4%)
Infection: Varicella zoster infection (4%), parasitic infection (infants: 3%)
Neuromuscular & skeletal: Myalgia (3%)
Otic: Otitis media (infants: 6%)
Respiratory: Bronchitis (infants: 6%), rhinorrhea (infants: 5%), pharyngitis (3% to 5%), epistaxis (infants: 3%)
Postmarketing and/or case reports: Dyspnea, hepatitis, hyperbilirubinemia, hypersensitivity reaction, increased liver enzymes, movement disorder, palpitations, pruritus, psychomotor agitation, seizure, skin rash, tachycardia
Warnings/Precautions
Concerns related to adverse effects:
- Hypersensitivity: Hypersensitivity reactions (including anaphylaxis) have been reported with use; discontinue therapy immediately with signs/symptoms of hypersensitivity.
Disease-related concerns:
- Hepatic impairment: Use with caution in patients with severe hepatic impairment.
- Renal impairment: Use with caution in patients with severe renal impairment.
Concurrent drug therapy issues:
- Sedatives: Effects may be potentiated when used with other sedative drugs or ethanol.
Special populations:
- Slow metabolizers: Use with caution in patients known to be slow metabolizers of desloratadine (incidence of side effects may be increased).
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggest that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol derivative with caution in neonates. See manufacturer's labeling.
- Phenylalanine: Some products may contain phenylalanine.
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Guidelines for the use of antihistamines in the treatment of allergic rhinitis or urticaria in pregnancy are generally the same as in nonpregnant females. Second generation antihistamines may be used for the treatment of allergic rhinitis and urticaria during pregnancy; however, information related to the use of desloratadine in pregnancy is limited and other medications may be preferred (Wallace 2008; Zuberbier 2018).
Patient Education
What is this drug used for?
- It is used to ease allergy signs.
- It is used to treat hives.
Frequently reported side effects of this drug
- Headache
- Dry mouth
- Sore throat
- Muscle pain
- Fatigue
- Menstrual pain
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Shortness of breath
- Irritability
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.