Boxed Warning
Serious cardiovascular thrombotic events:
Nonsteroidal anti-inflammatory drugs (NSAIDs) cause an increased risk of serious cardiovascular thrombotic events, including myocardial infarction (MI) and stroke, which can be fatal. This risk may occur early in treatment and may increase with duration of use.
Diclofenac is contraindicated in the setting of coronary artery bypass graft (CABG) surgery.
Serious gastrointestinal bleeding, ulceration, and perforation:
NSAIDs cause an increased risk of serious gastrointestinal (GI) adverse events, including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients and patients with a prior history of peptic ulcer disease and/or GI bleeding are at greater risk for serious GI events.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule, Oral, as base:
Zorvolex: 18 mg, 35 mg [contains brilliant blue fcf (fd&c blue #1), fd&c blue #2 (indigotine)]
Capsule, Oral, as potassium:
Zipsor: 25 mg [contains gelatin (bovine)]
Packet, Oral, as potassium:
Cambia: 50 mg (1 ea, 9 ea) [anise-mint flavor]
Cambia: 50 mg (1 ea [DSC], 9 ea [DSC]) [contains aspartame, saccharin sodium]
Solution, Intravenous, as sodium:
Dyloject: 37.5 mg/mL (1 mL [DSC])
Tablet, Oral, as potassium:
Generic: 50 mg
Tablet Delayed Release, Oral, as sodium:
Generic: 25 mg, 50 mg, 75 mg
Tablet Extended Release 24 Hour, Oral, as sodium:
Generic: 100 mg
Pharmacology
Mechanism of Action
Reversibly inhibits cyclooxygenase-1 and 2 (COX-1 and 2) enzymes, which results in decreased formation of prostaglandin precursors; has antipyretic, analgesic, and anti-inflammatory properties
Other proposed mechanisms not fully elucidated (and possibly contributing to the anti-inflammatory effect to varying degrees), include inhibiting chemotaxis, altering lymphocyte activity, inhibiting neutrophil aggregation/activation, and decreasing proinflammatory cytokine levels.
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: ~50% (systemically available)
Distribution
Oral: ~1.3 to 1.4 L/kg
Metabolism
Hepatic; undergoes first-pass metabolism; forms several metabolites (1 with weak activity)
Excretion
Urine (~65%); bile (~35%)
Time to Peak
Serum: Note: Fasted values reported for oral products; may be delayed with food.
Cambia: ~0.25 hours
Cataflam, Zorvolex: ~1 hour
Zipsor: ~0.47 ± 0.17 hour
Injection: ~5 minutes
Tablet, delayed release (diclofenac sodium): 2.3 hours
Tablet, extended release (diclofenac sodium): 5.3 hours
Half-Life Elimination
Oral: ~2 hours, ~1 hour (liquid filled capsule [Zipsor]); Injection: ~1.4 hours
Protein Binding
>99%, primarily to albumin
Use in Specific Populations
Special Populations Note
Body weight: Injection: Increased volume of distribution and clearance with increased body weight (>95 kg).
Use: Labeled Indications
Ankylosing spondylitis (delayed-release tablets only): Acute or long-term use in the relief of signs and symptoms of ankylosing spondylitis.
Dysmenorrhea (immediate-release tablets only): Treatment of primary dysmenorrhea.
Migraine (powder for oral solution only): Acute treatment of migraine attacks with or without aura in adults.
Osteoarthritis (immediate-release, extended-release, and delayed-release tablets; capsules [Zorvolex]; and suppositories [Canadian product] only): Relief of signs and symptoms of osteoarthritis.
Pain
Capsules/immediate-release tablets only: Relief of mild to moderate acute pain.
Injection only: Management of mild to moderate pain and moderate to severe pain (alone or in combination with opioid analgesics) in adults.
Rheumatoid arthritis (immediate-release, extended-release, and delayed-release tablets; and suppositories [Canadian product] only): Relief of signs and symptoms of rheumatoid arthritis.
Use: Off Label
Gout, treatment (acute flares)byes
Data from a limited number of trials support the efficacy of diclofenac in the treatment of acute gout flares Cheng 2004, Zhang 2014. Clinical experience also suggests the utility of diclofenac as an alternative agent for acute gout flares, particularly in younger adults (<60 years of age) without renal or cardiovascular comorbidities and active GI disease Becker 2019.
Based on the 2012 American College of Rheumatology guidelines for management of gout, nonsteroidal anti-inflammatory drugs are effective and recommended agents in the treatment of acute gout flares.
Contraindications
Hypersensitivity to diclofenac (eg, anaphylactoid reactions, serious skin reactions) or bovine protein (Zipsor only) or any component of the formulation; history of asthma, urticaria, or other allergic-type reactions after taking aspirin or other NSAIDs; use in the setting of CABG surgery; patients with moderate to severe renal impairment in the perioperative period and who are at risk for volume depletion (injection only).
Canadian labeling: Additional contraindications (not in US labeling): Severe uncontrolled heart failure; active gastric/duodenal/peptic ulcer; active GI bleed or perforation, regional ulcer or enteritis, gastritis, ulcerative colitis, or recurrent ulceration; cerebrovascular bleeding or other bleeding disorders; inflammatory bowel disease; severe hepatic impairment; active hepatic disease; severe renal impairment (CrCl <30 mL/minute) or deteriorating renal disease; known hyperkalemia; patients <16 years of age (suppository, tablet) or <18 years of age (packet only); breastfeeding; pregnancy (third trimester); recent history of bleeding or inflammatory lesions of rectum/anus (suppository only)
Dosage and Administration
Dosing: Adult
Note: Use the lowest effective dose for the shortest duration of time, consistent with individual patient treatment goals. Due to an increased risk of cardiovascular events, use should generally be avoided in patients with established cardiovascular disease or risk factors for cardiovascular disease. Use should also be avoided in those with heart failure (Chan 2018; Schmidt 2016). Of note, Dyloject (diclofenac injection) has been discontinued in the United States for >1 year.
Note: For all indications, it has been recommended to not exceed 100 mg/day based on increased risk of vascular events (eg, stroke, nonfatal myocardial infarction) (Bhala 2013; Health Canada communication 2014).
Ankylosing spondylitis: Oral: Delayed-release tablet: 25 mg 4 times daily and 25 mg at bedtime as needed.
Gout, treatment (acute flares) (alternative agent) (off-label use): Oral: IR tablets or delayed-release tablets: 50 mg twice daily (Becker 2019); initiate within 24 to 48 hours of flare onset preferably; discontinue 2 to 3 days after resolution of clinical signs; usual duration: 5 to 7 days (ACR [Khanna 2012]; Becker 2019).
Migraine: Oral: Powder for oral solution: 50 mg (one packet) as a single dose; safety and efficacy of a second dose have not been established.
Osteoarthritis:
Oral:
Immediate-release tablet: 50 mg 2 to 3 times daily; Delayed-release tablet: 50 mg 2 to 3 times daily or 75 mg twice daily; Extended-release tablet: 100 mg once daily.
Immediate-release capsule: Zorvolex (diclofenac acid): 35 mg 3 times daily.
Rectal suppository [Canadian product]: Insert 50 mg or 100 mg rectally as single dose to substitute for final oral daily dose (maximum combined dose [rectal and oral]: 100 mg/day).
Pain:
Oral:
Immediate-release tablet: 50 mg 3 times daily; may administer 100 mg as an initial dose, followed by 50 mg 3 times daily.
Immediate-release capsule:
Zipsor (diclofenac potassium): 25 mg 4 times daily.
Zorvolex (diclofenac acid): 18 mg or 35 mg 3 times daily.
IV: 37.5 mg every 6 hours as needed; adjust frequency according to patient response (maximum: 150 mg/day).
Primary dysmenorrhea: Oral: Immediate-release tablet: 50 mg 3 times daily; may administer 100 mg as an initial dose, followed by 50 mg 3 times daily.
Rheumatoid arthritis:
Oral: Immediate-release tablet: 50 mg 3 to 4 times daily; Delayed-release tablet: 50 mg 3 to 4 times daily or 75 mg twice daily; Extended-release tablet: 100 mg once daily; may increase to 100 mg twice daily.
Rectal suppository [Canadian product]: Insert 50 mg or 100 mg rectally as single dose to substitute for final oral daily dose (maximum combined dose [rectal and oral]: 100 mg/day.
Dosing: Geriatric
Refer to adult dosing. Use with caution; initiate using lowest recommended dose and frequency.
Dosing: Pediatric
Note: Different oral formulations are not bioequivalent; do not interchange products.
Juvenile idiopathic arthritis: Limited data available: Children and Adolescents: Oral: Immediate release tablet: 2 to 3 mg/kg/day in divided doses 2 to 4 times/day; maximum daily dose: 150 mg/day (Haapasaari 1983; Hashkes 2005; Leak 1996; Petty 2016)
Migraine: Adolescents ≥18 years: Oral: Oral solution: 50 mg (one packet) as a single dose at the time of migraine onset; safety and efficacy of a second dose have not been established
Reconstitution
Powder for oral solution: Empty contents of one packet into 30 to 60 mL of water (do not use other liquids); mix well and administer immediately.
Administration
Injection: Administer as an IV bolus over 15 seconds.
Oral: Do not crush delayed- or extended-release tablets. May administer immediate-release formulations with food or milk to avoid gastric distress.
Cambia, Zorvolex: Administering with food may cause a reduction in effectiveness.
Dietary Considerations
Oral immediate-release formulations may be taken with food to decrease GI distress. However, food may reduce effectiveness of oral solution and diclofenac acid (capsule). Some products may contain phenylalanine.
Storage
Capsule, tablet: Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from moisture.
Injection: Store at 20°C to 25°C (68°F to 77°F). Do not freeze. Protect from light.
Powder for oral solution: Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
Suppository [Canadian product]: Store at 15°C to 30°C (59°F to 86°F); protect from heat.
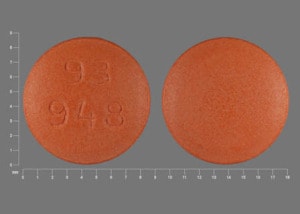
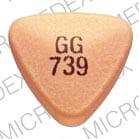
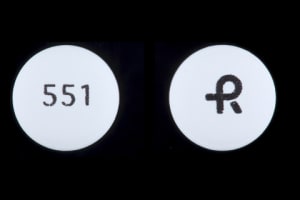
Diclofenac (Systemic) Images
Drug Interactions
5-Aminosalicylic Acid Derivatives: Nonsteroidal Anti-Inflammatory Agents may enhance the nephrotoxic effect of 5-Aminosalicylic Acid Derivatives. Monitor therapy
Acalabrutinib: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Acemetacin: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Agents with Antiplatelet Properties (e.g., P2Y12 inhibitors, NSAIDs, SSRIs, etc.): May enhance the antiplatelet effect of other Agents with Antiplatelet Properties. Monitor therapy
Alcohol (Ethyl): May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Specifically, the risk of GI bleeding may be increased with this combination. Monitor therapy
Aliskiren: Nonsteroidal Anti-Inflammatory Agents may diminish the antihypertensive effect of Aliskiren. Nonsteroidal Anti-Inflammatory Agents may enhance the nephrotoxic effect of Aliskiren. Management: Monitor renal function periodically in patients receiving aliskiren and any nonsteroidal anti-inflammatory agent. Patients at elevated risk of renal dysfunction include those who are elderly, are volume depleted, or have pre-existing renal dysfunction. Monitor therapy
Aminoglycosides: Nonsteroidal Anti-Inflammatory Agents may decrease the excretion of Aminoglycosides. Data only in premature infants. Monitor therapy
Aminolevulinic Acid (Systemic): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Systemic). Avoid combination
Aminolevulinic Acid (Topical): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Topical). Monitor therapy
Angiotensin II Receptor Blockers: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Specifically, the combination may result in a significant decrease in renal function. Nonsteroidal Anti-Inflammatory Agents may diminish the therapeutic effect of Angiotensin II Receptor Blockers. The combination of these two agents may also significantly decrease glomerular filtration and renal function. Monitor therapy
Angiotensin-Converting Enzyme Inhibitors: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Specifically, the combination may result in a significant decrease in renal function. Nonsteroidal Anti-Inflammatory Agents may diminish the antihypertensive effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Anticoagulants: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Anticoagulants. Exceptions: Bemiparin; Enoxaparin; Heparin. Monitor therapy
Apixaban: Nonsteroidal Anti-Inflammatory Agents (Nonselective) may enhance the adverse/toxic effect of Apixaban. Specifically, the risk of bleeding may be increased. Management: A comprehensive risk to benefit assessment should be done for all patients before any concurrent use of apixaban and nonsteroidal anti-inflammatory drugs (NSAIDs). If combined, monitor patients extra closely for signs and symptoms of bleeding. Consider therapy modification
Bemiparin: Nonsteroidal Anti-Inflammatory Agents may enhance the anticoagulant effect of Bemiparin. Management: Avoid concomitant use of bemiparin and nonsteroidal anti-inflammatory agents (NSAIDs) due to the increased risk of bleeding. If concomitant use is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Bemiparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Bemiparin. Management: Avoid concomitant use of bemiparin with antiplatelet agents. If concomitant use is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Beta-Blockers: Nonsteroidal Anti-Inflammatory Agents may diminish the antihypertensive effect of Beta-Blockers. Exceptions: Levobunolol; Metipranolol. Monitor therapy
Bile Acid Sequestrants: May decrease the absorption of Nonsteroidal Anti-Inflammatory Agents. Consider therapy modification
Bisphosphonate Derivatives: Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Bisphosphonate Derivatives. Both an increased risk of gastrointestinal ulceration and an increased risk of nephrotoxicity are of concern. Monitor therapy
Cephalothin: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Cephalothin. Specifically, the risk for bleeding may be increased. Monitor therapy
Collagenase (Systemic): Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Collagenase (Systemic). Specifically, the risk of injection site bruising and/or bleeding may be increased. Monitor therapy
Corticosteroids (Systemic): May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents (Nonselective). Monitor therapy
CycloSPORINE (Systemic): Nonsteroidal Anti-Inflammatory Agents may enhance the nephrotoxic effect of CycloSPORINE (Systemic). Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of CycloSPORINE (Systemic). CycloSPORINE (Systemic) may increase the serum concentration of Nonsteroidal Anti-Inflammatory Agents. Management: Consider alternatives to nonsteroidal anti-inflammatory agents (NSAIDs). Monitor for evidence of nephrotoxicity, as well as increased serum cyclosporine concentrations and systemic effects (eg, hypertension) during concomitant therapy with NSAIDs. Consider therapy modification
CYP2C9 Inducers (Moderate): May decrease the serum concentration of Diclofenac (Systemic). Monitor therapy
CYP2C9 Inhibitors (Moderate): May increase the serum concentration of Diclofenac (Systemic). Management: Consider using a reduced dose of diclofenac when used together with moderate CYP2C9 inhibitors. Arthrotec (diclofenac and misoprostol) prescribing information recommends a maximum dose of 50 mg twice daily. Consider therapy modification
Dabigatran Etexilate: Nonsteroidal Anti-Inflammatory Agents (Nonselective) may enhance the adverse/toxic effect of Dabigatran Etexilate. Specifically, the risk of bleeding may be increased. Management: A comprehensive risk to benefit assessment should be done for all patients before any concurrent use of dabigatran and nonsteroidal anti-inflammatory drugs (NSAIDs). If combined, monitor patients extra closely for signs and symptoms of bleeding. Consider therapy modification
Dasatinib: May enhance the anticoagulant effect of Agents with Antiplatelet Properties. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Deferasirox: Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Deferasirox. Specifically, the risk for GI ulceration/irritation or GI bleeding may be increased. Monitor therapy
Deferiprone: UGT1A6 Inhibitors may increase the serum concentration of Deferiprone. Avoid combination
Deoxycholic Acid: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Deoxycholic Acid. Specifically, the risk for bleeding or bruising in the treatment area may be increased. Monitor therapy
Desmopressin: Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Desmopressin. Monitor therapy
Dexibuprofen: Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Dexibuprofen. Avoid combination
Dexketoprofen: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Digoxin: Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of Digoxin. Monitor therapy
Drospirenone: Nonsteroidal Anti-Inflammatory Agents may enhance the hyperkalemic effect of Drospirenone. Monitor therapy
Edoxaban: Nonsteroidal Anti-Inflammatory Agents (Nonselective) may enhance the adverse/toxic effect of Edoxaban. Specifically, the risk of bleeding may be increased. Management: A comprehensive risk to benefit assessment should be done for all patients before any concurrent use of edoxaban and nonsteroidal anti-inflammatory drugs (NSAIDs). If combined, monitor patients extra closely for signs and symptoms of bleeding. Consider therapy modification
Enoxaparin: Nonsteroidal Anti-Inflammatory Agents may enhance the anticoagulant effect of Enoxaparin. Management: Discontinue nonsteroidal anti-inflammatory agents (NSAIDs) prior to initiating enoxaparin whenever possible. If concomitant administration is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Enoxaparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Enoxaparin. Management: Discontinue antiplatelet agents prior to initiating enoxaparin whenever possible. If concomitant administration is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Eplerenone: Nonsteroidal Anti-Inflammatory Agents may diminish the antihypertensive effect of Eplerenone. Nonsteroidal Anti-Inflammatory Agents may enhance the hyperkalemic effect of Eplerenone. Monitor therapy
Fat Emulsion (Fish Oil Based): May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Monitor therapy
Felbinac: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Monitor therapy
Floctafenine: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Glucosamine: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Haloperidol: Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Haloperidol. Specifically including drowsiness and confusion. Monitor therapy
Heparin: Nonsteroidal Anti-Inflammatory Agents may enhance the anticoagulant effect of Heparin. Management: Decrease the dose of heparin or nonsteroidal anti-inflammatory agents (NSAIDs) if coadministration is required. Consider therapy modification
Heparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Heparin. Management: Decrease the dose of heparin or agents with antiplatelet properties if coadministration is required. Consider therapy modification
Herbs (Anticoagulant/Antiplatelet Properties) (eg, Alfalfa, Anise, Bilberry): May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Bleeding may occur. Management: Avoid combination when possible. If used, monitor more closely for evidence of bleeding. Discontinue herbal products with anticoagulant or antiplatelet actions 2 weeks prior to surgical, dental, or invasive procedures. Consider therapy modification
Herbs (Anticoagulant/Antiplatelet Properties) (eg, Alfalfa, Anise, Bilberry): May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Bleeding may occur. Management: Concomitant treatment with these agents should generally be avoided. If used concomitantly, increased diligence in monitoring for adverse effects (eg, bleeding, bruising, altered mental status due to CNS bleeds) must be employed. Consider therapy modification
HydrALAZINE: Nonsteroidal Anti-Inflammatory Agents may diminish the antihypertensive effect of HydrALAZINE. Monitor therapy
Ibritumomab Tiuxetan: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Ibritumomab Tiuxetan. Both agents may contribute to impaired platelet function and an increased risk of bleeding. Monitor therapy
Ibrutinib: May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Monitor therapy
Inotersen: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Ketorolac (Nasal): May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Ketorolac (Systemic): May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Limaprost: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Lithium: Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of Lithium. Consider therapy modification
Loop Diuretics: Nonsteroidal Anti-Inflammatory Agents may diminish the diuretic effect of Loop Diuretics. Loop Diuretics may enhance the nephrotoxic effect of Nonsteroidal Anti-Inflammatory Agents. Management: Monitor for evidence of kidney injury or decreased therapeutic effects of loop diuretics with concurrent use of an NSAID. Consider avoiding concurrent use in CHF or cirrhosis. Concomitant use of bumetanide with indomethacin is not recommended. Consider therapy modification
Macimorelin: Nonsteroidal Anti-Inflammatory Agents may diminish the diagnostic effect of Macimorelin. Avoid combination
MetFORMIN: Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of MetFORMIN. Monitor therapy
Methotrexate: Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of Methotrexate. Management: Alternative anti-inflammatory therapy should be considered whenever possible, especially if the patient is receiving higher, antineoplastic doses of methotrexate. Consider therapy modification
Mifamurtide: Nonsteroidal Anti-Inflammatory Agents may diminish the therapeutic effect of Mifamurtide. Avoid combination
Morniflumate: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Multivitamins/Fluoride (with ADE): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Multivitamins/Minerals (with AE, No Iron): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Naftazone: May enhance the antiplatelet effect of Nonsteroidal Anti-Inflammatory Agents. Monitor therapy
Nalmefene: Diclofenac (Systemic) may increase the serum concentration of Nalmefene. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents: Diclofenac (Systemic) may enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Management: Seek alternatives to the combined use of diclofenac with other nonsteroidal anti-inflammatory agents (NSAIDs). Avoid the use of diclofenac/misoprostol with other NSAIDs. Consider therapy modification
Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective): Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective). Avoid combination
Obinutuzumab: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Obinutuzumab. Specifically, the risk of serious bleeding-related events may be increased. Monitor therapy
Omacetaxine: Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Omacetaxine. Specifically, the risk for bleeding-related events may be increased. Management: Avoid concurrent use of nonsteroidal antiinflammatory drugs (NSAIDs) with omacetaxine in patients with a platelet count of less than 50,000/uL. Avoid combination
Omega-3 Fatty Acids: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Pelubiprofen: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Pentosan Polysulfate Sodium: May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Specifically, the risk of bleeding may be increased by concurrent use of these agents. Monitor therapy
Pentoxifylline: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Phenylbutazone: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Porfimer: Photosensitizing Agents may enhance the photosensitizing effect of Porfimer. Monitor therapy
Potassium-Sparing Diuretics: Nonsteroidal Anti-Inflammatory Agents may diminish the antihypertensive effect of Potassium-Sparing Diuretics. Nonsteroidal Anti-Inflammatory Agents may enhance the hyperkalemic effect of Potassium-Sparing Diuretics. Monitor therapy
PRALAtrexate: Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of PRALAtrexate. More specifically, NSAIDS may decrease the renal excretion of pralatrexate. Management: Closely monitor for increased pralatrexate serum levels and/or toxicity if used concomitantly with an NSAID. Monitor for decreased pralatrexate serum levels with NSAID discontinuation. Monitor therapy
Probenecid: May increase the serum concentration of Nonsteroidal Anti-Inflammatory Agents. Monitor therapy
Prostacyclin Analogues: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Prostaglandins (Ophthalmic): Nonsteroidal Anti-Inflammatory Agents may diminish the therapeutic effect of Prostaglandins (Ophthalmic). Nonsteroidal Anti-Inflammatory Agents may also enhance the therapeutic effects of Prostaglandins (Ophthalmic). Monitor therapy
Quinolones: Nonsteroidal Anti-Inflammatory Agents may enhance the neuroexcitatory and/or seizure-potentiating effect of Quinolones. Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of Quinolones. Monitor therapy
Resveratrol: May increase the serum concentration of Diclofenac (Systemic). Monitor therapy
Rivaroxaban: Nonsteroidal Anti-Inflammatory Agents (Nonselective) may enhance the adverse/toxic effect of Rivaroxaban. Specifically, the risk of bleeding may be increased. Management: A comprehensive risk to benefit assessment should be done for all patients before any concurrent use of rivaroxaban and nonsteroidal anti-inflammatory drugs (NSAIDs). If combined, monitor patients extra closely for signs and symptoms of bleeding. Consider therapy modification
Salicylates: Nonsteroidal Anti-Inflammatory Agents (Nonselective) may enhance the adverse/toxic effect of Salicylates. An increased risk of bleeding may be associated with use of this combination. Nonsteroidal Anti-Inflammatory Agents (Nonselective) may diminish the cardioprotective effect of Salicylates. Salicylates may decrease the serum concentration of Nonsteroidal Anti-Inflammatory Agents (Nonselective). Exceptions: Choline Magnesium Trisalicylate. Consider therapy modification
Salicylates: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Salicylates. Increased risk of bleeding may result. Monitor therapy
Selective Serotonin Reuptake Inhibitors: May enhance the antiplatelet effect of Nonsteroidal Anti-Inflammatory Agents (Nonselective). Nonsteroidal Anti-Inflammatory Agents (Nonselective) may diminish the therapeutic effect of Selective Serotonin Reuptake Inhibitors. Management: Consider alternatives to NSAIDs. Monitor for evidence of bleeding and diminished antidepressant effects. It is unclear whether COX-2-selective NSAIDs reduce risk. Consider therapy modification
Serotonin/Norepinephrine Reuptake Inhibitors: May enhance the antiplatelet effect of Nonsteroidal Anti-Inflammatory Agents (Nonselective). Monitor therapy
Sincalide: Drugs that Affect Gallbladder Function may diminish the therapeutic effect of Sincalide. Management: Consider discontinuing drugs that may affect gallbladder motility prior to the use of sincalide to stimulate gallbladder contraction. Consider therapy modification
Sodium Phosphates: May enhance the nephrotoxic effect of Nonsteroidal Anti-Inflammatory Agents. Specifically, the risk of acute phosphate nephropathy may be enhanced. Management: Consider avoiding this combination by temporarily suspending treatment with NSAIDs, or seeking alternatives to oral sodium phosphate bowel preparation. If the combination cannot be avoided, maintain adequate hydration and monitor renal function closely. Consider therapy modification
Tacrolimus (Systemic): Nonsteroidal Anti-Inflammatory Agents may enhance the nephrotoxic effect of Tacrolimus (Systemic). Monitor therapy
Talniflumate: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Tenofovir Products: Diclofenac (Systemic) may enhance the nephrotoxic effect of Tenofovir Products. Management: Seek alternatives to this combination whenever possible. Avoid use of tenofovir with multiple NSAIDs or any NSAID given at a high dose. Consider therapy modification
Tenoxicam: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Thiazide and Thiazide-Like Diuretics: May enhance the nephrotoxic effect of Nonsteroidal Anti-Inflammatory Agents. Nonsteroidal Anti-Inflammatory Agents may diminish the therapeutic effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Thrombolytic Agents: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Thrombolytic Agents. Monitor therapy
Tipranavir: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Tolperisone: Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Tolperisone. Specifically, the risk of hypersensitivity reactions may be increased. Tolperisone may enhance the therapeutic effect of Nonsteroidal Anti-Inflammatory Agents. Monitor therapy
Tricyclic Antidepressants (Tertiary Amine): May enhance the antiplatelet effect of Nonsteroidal Anti-Inflammatory Agents (Nonselective). Monitor therapy
Urokinase: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Urokinase. Avoid combination
Vancomycin: Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of Vancomycin. Monitor therapy
Verteporfin: Photosensitizing Agents may enhance the photosensitizing effect of Verteporfin. Monitor therapy
Vitamin E (Systemic): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Nonsteroidal Anti-Inflammatory Agents (Nonselective) may enhance the anticoagulant effect of Vitamin K Antagonists. Management: Consider alternatives to this combination when possible. If the combination must be used, monitor coagulation status closely and advise patients to promptly report any evidence of bleeding or bruising. Consider therapy modification
Voriconazole: May increase the serum concentration of Diclofenac (Systemic). Management: Consider using a lower dose of diclofenac when used with voriconazole. Arthrotec (diclofenac and misoprostol) labeling recommends limiting the total daily dose to a maximum of 50 mg twice daily. Consider therapy modification
Zaltoprofen: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Zanubrutinib: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Test Interactions
May lead to false-positive aldosterone/renin ratio (ARR) (Funder 2016).
Adverse Reactions
Injection: Frequency not always defined.
Cardiovascular: Edema (≤10%), cerebrovascular accident, hypertension, myocardial infarction, significant cardiovascular event
Central nervous system: Headache (≤10%), dizziness (8%)
Dermatologic: Pruritus (≤10%), skin rash (≤10%), exfoliative dermatitis, Stevens-Johnson syndrome, toxic epidermal necrolysis
Endocrine & metabolic: Fluid retention
Gastrointestinal: Constipation (13%), abdominal pain (≤10%), diarrhea (≤10%), dyspepsia (≤10%), esophageal perforation (≤10%), flatulence (≤10%), gastrointestinal ulcer (≤10%; including gastric/duodenal), heartburn (≤10%), intestinal perforation (≤10%), nausea (≤10%), vomiting (≤10%)
Hematologic & oncologic: Anemia (≤10%), hemorrhage (≤10%), prolonged bleeding time (≤10%)
Hepatic: Increased liver enzymes (≤10%), increased serum transaminases (15%), increased serum ALT (≤4%; >8X ULN: ≤1%), increased serum AST (2% to ≤4%; >8X ULN: ≤1%)
Hypersensitivity: Anaphylactoid reaction
Local: Infusion site reaction (10%), extravasation (3%)
Otic: Tinnitus (≤10%)
Renal: Renal insufficiency (≤10%)
Miscellaneous: Wound healing impairment (8%), gastrointestinal inflammation
<1%, postmarketing, and/or case reports : Abnormal Dreams, agranulocytosis, alopecia, anaphylaxis, angioedema, anxiety, aplastic anemia, asthma, auditory impairment, blurred vision, cardiac arrhythmia, cardiac failure, change in appetite, colitis, coma, confusion, conjunctivitis, convulsions, cystitis, depression, diaphoresis, drowsiness, dyspnea, dysuria, ecchymoses, eosinophilia, eructation, erythema multiforme, esophagitis, exfoliative dermatitis, fever, fulminant hepatitis, gastritis, gastrointestinal hemorrhage, glossitis, hallucination, hematemesis, hematuria, hemolytic anemia, hepatic failure, hepatic necrosis, hepatitis, hepatotoxicity, hyperglycemia, hypertension, hypotension, infection, insomnia, interstitial nephritis, jaundice, leukopenia, lymphadenopathy, malaise, melena, meningitis, nervousness, oliguria, palpitations, pancreatitis, pancytopenia, paresthesia, pneumonia, polyuria, proteinuria, purpura, rectal hemorrhage, renal failure, respiratory depression, sepsis, skin photosensitivity, stomatitis, syncope, tachycardia, thrombocytopenia, toxic epidermal necrolysis, tremor, urticaria, vasculitis, vertigo, weakness, weight changes
Oral: Frequency not always defined.
>10%:
Cardiovascular: Edema (33%)
Hepatic: Increased serum transaminases (≤3 x ULN; 15%)
1% to 10%:
Cardiovascular: Hypertension (2% to 3%)
Central nervous system: Headache (4% to 8%), procedural pain (3%), dizziness (2%), falling (2%)
Dermatologic: Pruritus (7%), skin rash
Gastrointestinal: Constipation (5% to 8%), nausea (6% to 7%), diarrhea (6%), GI adverse effects (gastric ulcer, hemorrhage, and perforation; ≤4%, risk increases with therapy duration), abdominal pain (2% to 3%), vomiting (3%), dyspepsia (2% to 3%), flatulence (2% to 3%), heartburn, abdominal discomfort (2%), duodenal ulcer
Genitourinary: Urinary tract infection (7%)
Hematologic & oncologic: Bruise (3%), anemia, prolonged bleeding time
Hepatic: Increased serum ALT (>3 x ULN: ≤4%; >8 x ULN: ≤1%), increased serum AST (>3 x ULN; ≤4%; >8 x ULN: ≤1%)
Infection: Influenza (3%)
Neuromuscular & skeletal: Osteoarthritis (5%), arthralgia (3%), back pain (3%), limb pain (3%)
Renal: Renal function abnormality
Otic: Tinnitus
Renal: Increased serum creatinine (2%), renal function abnormality
Respiratory: Upper respiratory tract infection (8%), nasopharyngitis (6%), sinusitis (3% to 5%), cough (4%), bronchitis (3%)
<1%, postmarketing, and/or case reports: Abnormal dreams, agranulocytosis, alopecia, anaphylactoid reaction, anaphylaxis, angioedema, anxiety, aplastic anemia, aseptic meningitis, asthma, auditory impairment, azotemia (Gurwitz, 1990), blurred vision, cardiac arrhythmia, cardiac failure, cerebrovascular accident, change in appetite, chest pain, colitis, coma, confusion, conjunctivitis, cystitis, decreased hemoglobin (Goldstein, 2011), depression, diaphoresis, diplopia, disorientation, drowsiness, dyspnea, dysuria, ecchymoses, eosinophilia, eructation, erythema multiforme, esophageal ulcer, esophagitis, exfoliative dermatitis, fever, fluid retention, fulminant hepatitis, gastritis, glossitis, hallucination, hearing loss, hematemesis, hematuria, hemolytic anemia, hepatic failure, hepatic necrosis, hepatitis, hepatotoxicity, hyperglycemia, hypotension, infection, insomnia, interstitial nephritis, intestinal perforation, jaundice, leukopenia, lymphadenopathy, malaise, melena, memory impairment, meningitis, myocardial infarction, nephrotic syndrome, nervousness, oliguria, palpitations, pancreatitis, pancytopenia, paresthesia, peptic ulcer, pneumonia, polyuria, proteinuria, psychotic reaction, purpura, rectal hemorrhage, renal failure, renal papillary necrosis, respiratory depression, seizure, sepsis, skin photosensitivity, Stevens-Johnson syndrome, stomatitis, syncope, tachycardia, taste disorder, thrombocytopenia, toxic epidermal necrolysis, tremor, urticaria, vasculitis, vertigo, weakness, weight changes, xerostomia
Rectal suppository [Canadian product]:
Also refer to adverse reactions associated with oral formulations.
<1%, postmarketing, and/or case reports: Hemorrhoids (exacerbation), local hemorrhage, proctitis, rectal irritation
Warnings/Precautions
Concerns related to adverse effects:
- Anaphylactoid reactions: Even in patients without prior exposure anaphylactoid reactions may occur; patients with "aspirin triad" (bronchial asthma, aspirin intolerance, rhinitis) may be at increased risk. Contraindicated in patients who experience bronchospasm, asthma, rhinitis, or urticaria with NSAID or aspirin therapy.
- Cardiovascular events: [US Boxed Warning]: NSAIDs cause an increased risk of serious (and potentially fatal) adverse cardiovascular thrombotic events, including MI and stroke. Risk may occur early during treatment and may increase with duration of use. Relative risk appears to be similar in those with and without known cardiovascular disease or risk factors for cardiovascular disease; however, absolute incidence of serious cardiovascular thrombotic events (which may occur early during treatment) was higher in patients with known cardiovascular disease or risk factors and in those receiving higher doses. New onset hypertension or exacerbation of hypertension may occur (NSAIDs may also impair response to ACE inhibitors, thiazide diuretics, or loop diuretics); may contribute to cardiovascular events; monitor blood pressure; use with caution in patients with hypertension. May cause sodium and fluid retention; use with caution in patients with edema. Avoid use in heart failure (ACCF/AHA [Yancy 2013]). Avoid use in patients with recent MI unless benefits outweigh risk of cardiovascular thrombotic events. Use the lowest effective dose for the shortest duration of time, consistent with individual patient goals, to reduce risk of cardiovascular events; alternate therapies should be considered for patients at high risk.
- CNS effects: May cause drowsiness, dizziness, blurred vision, and other neurologic effects which may impair physical or mental abilities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving). Discontinue use with blurred or diminished vision and perform ophthalmologic exam. Periodically evaluate vision in all patients receiving long term therapy.
- GI events: [US Boxed Warning]: NSAIDs cause an increased risk of serious gastrointestinal inflammation, ulceration, bleeding, and perforation (may be fata); elderly patients and patients with history of peptic ulcer disease and/or GI bleeding are at greater risk for serious GI events. These events may occur at any time during therapy and without warning. Avoid use in patients with active GI bleeding. In patients with a history of acute lower GI bleeding, avoid use of non-aspirin NSAIDs, especially if due to angioectasia or diverticulosis (Strate 2016). Use caution with a history of GI ulcers, concurrent therapy known to increase the risk of GI bleeding (eg, aspirin, anticoagulants and/or corticosteroids, selective serotonin reuptake inhibitors), advanced hepatic disease, coagulopathy, smoking, use of alcohol, or in elderly or debilitated patients. Use the lowest effective dose for the shortest duration of time, consistent with individual patient goals, to reduce risk of GI adverse events; alternate therapies should be considered for patients at high risk. When used concomitantly with aspirin, a substantial increase in the risk of gastrointestinal complications (eg, ulcer) occurs; concomitant gastroprotective therapy (eg, proton pump inhibitors) is recommended (Bhatt 2008).
- Hematologic effects: Platelet adhesion and aggregation may be decreased; may prolong bleeding time; patients with coagulation disorders or who are receiving anticoagulants should be monitored closely. Anemia may occur; patients on long-term NSAID therapy should be monitored for anemia. Rarely, NSAID use has been associated with potentially severe blood dyscrasias (eg, agranulocytosis, thrombocytopenia, aplastic anemia).
- Hepatic effects: Transaminase elevations have been reported with use; closely monitor patients with any abnormal LFT. Rare, sometimes fatal severe hepatic reactions (eg, fulminant hepatitis, hepatic necrosis, hepatic failure) have occurred with NSAID use; discontinue immediately if clinical signs or symptoms of liver disease develop or if systemic manifestations occur.
- Hyperkalemia: NSAID use may increase the risk of hyperkalemia, particularly in the elderly, diabetics, renal disease, and with concomitant use of other agents capable of inducing hyperkalemia (eg, ACE inhibitors). Monitor potassium closely.
- Renal effects: NSAID use may compromise existing renal function; dose-dependent decreases in prostaglandin synthesis may result from NSAID use, reducing renal blood flow which may cause renal decompensation (usually reversible). Patients with impaired renal function, dehydration, hypovolemia, heart failure, hepatic impairment, those taking diuretics and ACE inhibitors, and elderly patients are at greater risk of renal toxicity. Rehydrate patient before starting therapy; monitor renal function closely. Long-term NSAID use may result in renal papillary necrosis and other renal injury.
- Skin reactions: NSAIDs may cause potentially fatal serious skin adverse events including exfoliative dermatitis, Stevens-Johnson syndrome (SJS), and toxic epidermal necrolysis (TEN); may occur without warning; discontinue use at first sign of skin rash (or any other hypersensitivity).
Disease-related concerns:
- Aseptic meningitis: May increase the risk of aseptic meningitis (rarely), especially in patients with systemic lupus erythematosus (SLE) and mixed connective tissue disorders.
- Asthma: Contraindicated in patients with aspirin-sensitive asthma; severe, potentially fatal bronchospasm may occur. Use caution in patients with other forms of asthma.
- Bariatric surgery: Gastric ulceration: Avoid chronic use of oral nonselective NSAIDs after bariatric surgery; development of anastomotic ulcerations/perforations may occur (Bhangu 2014; Mechanick 2013). Short-term use of celecoxib or IV ketorolac are recommended as part of a multimodal pain management strategy for postoperative pain (Chou 2016; Horsley 2019; Thorell 2016).
- Coronary artery bypass graft surgery: [US Boxed Warning]: Use is contraindicated in the setting of coronary artery bypass graft (CABG) surgery. Risk of MI and stroke may be increased with use following CABG surgery.
- Hepatic impairment: Use with caution in patients with hepatic impairment; reduced doses may be required due to extensive hepatic metabolism. Patients with advanced hepatic disease are at an increased risk of GI bleeding with NSAIDs.
- Renal impairment: Avoid use in patients with advanced renal disease unless benefits are expected to outweigh risk of worsening renal function; monitor closely if therapy must be initiated. Injection is not recommended in patients with moderate to severe renal impairment and is contraindicated in patients with moderate to severe renal impairment in the perioperative period and who are at risk for volume depletion.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Elderly patients are at greater risk for serious GI, cardiovascular, and/or renal adverse events.
Dosage form specific issues:
- Injection: Not indicated for long-term use.
- Oral solution: May contain phenylalanine.
- Zipsor: Contains gelatin; use is contraindicated in patients with history of hypersensitivity to bovine protein.
Other warnings/precautions:
- Appropriate use: Oral solution: Indicated only for the acute treatment of migraine (not indicated for migraine prophylaxis or cluster headache). Acute migraine agents (eg, NSAIDs, triptans, opioids, ergotamine, or a combination of the agents) used for 10 or more days per month may lead to worsening of headaches (medication overuse headache); withdrawal treatment may be necessary in the setting of overuse.
- Bioequivalence: Different formulations of oral diclofenac are not bioequivalent, even if the milligram strength is the same; do not interchange products.
- Surgical/dental procedures: Withhold for at least 4 to 6 half-lives prior to surgical or dental procedures.
Monitoring Parameters
Monitor CBC, chemistry profile, weight gain, edema, liver function tests (baseline and periodically during chronic therapy), renal function (serum BUN, serum creatinine, urine output); occult blood loss; blood pressure; observe for bleeding, bruising; GI effects (abdominal pain, bleeding, dyspepsia); mental confusion, disorientation
Pregnancy
Pregnancy Considerations
Diclofenac crosses the placenta. Birth defects have been observed following in utero NSAID exposure in some studies; however, data is conflicting (Bloor 2013). Nonteratogenic effects, including prenatal constriction of the ductus arteriosus, persistent pulmonary hypertension of the newborn, oligohydramnios, necrotizing enterocolitis, renal dysfunction or failure, and intracranial hemorrhage have been observed in the fetus/neonate following in utero NSAID exposure. In addition, nonclosure of the ductus arteriosus postnatally may occur and be resistant to medical management (Bermas 2014; Bloor 2013). Because they may cause premature closure of the ductus arteriosus, product labeling for diclofenac specifically states use should be avoided starting at 30-weeks gestation.
Use of NSAIDs can be considered for the treatment of mild rheumatoid arthritis flares in pregnant women; however, use should be minimized or avoided early and late in pregnancy (Bermas 2014; Saavedra Salinas 2015). If treatment of migraine is needed in pregnant women, agents other than diclofenac are preferred (Amundsen 2015).
The chronic use of NSAIDs, including diclofenac, in women of reproductive age may be associated with infertility that is reversible upon discontinuation of the medication. Consider discontinuing use in women having difficulty conceiving or those undergoing investigation of fertility. The use of NSAIDs close to conception may be associated with an increased risk of miscarriage (Bermas 2014; Bloor 2013).
Patient Education
What is this drug used for?
- It is used to ease pain.
- It is used to treat some types of arthritis.
- It is used to ease painful period (menstrual) cycles.
- It is used to treat migraine headaches.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Nausea
- Constipation
- Heartburn
- Abdominal pain
- Vomiting
- Diarrhea
- Passing gas
- Fatigue
- Common cold symptoms
- Injection site pain
- Sweating a lot
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Severe cerebrovascular disease like change in strength on one side is greater than the other, difficulty speaking or thinking, change in balance, or vision changes.
- Abdominal ulcers like severe abdominal or back pain; black, tarry, or bloody stools; vomiting blood or vomit that looks like coffee grounds; or weight gain or abnormal swelling.
- High potassium like abnormal heartbeat, confusion, dizziness, passing out, weakness, shortness of breath, or numbness or tingling feeling.
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding.
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain.
- Shortness of breath
- Severe dizziness
- Passing out
- Excessive weight gain
- Swelling of arm or leg
- Chest pain
- Fast heartbeat
- Severe headache
- Vision changes
- Severe loss of strength and energy
- Painful urination
- Blood in the urine
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.