Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Capsule Delayed Release, Oral:
Tecfidera: 120 mg, 240 mg [contains brilliant blue fcf (fd&c blue #1)]
Miscellaneous, Oral:
Tecfidera: Capsule, delayed release: 120 mg (14s) and Capsule, delayed release: 240 mg (46s) (60 ea) [contains brilliant blue fcf (fd&c blue #1)]
Pharmacology
Mechanism of Action
DMF and its active metabolite, monomethyl fumarate (MMF), have been shown to activate the nuclear factor (erythroid-derived 2)-like 2 (Nrf2) pathway, which is involved in cellular response to oxidative stress. The mechanism by which dimethyl fumarate (DMF) exerts a therapeutic effect in MS is unknown, although it is believed to result from its anti-inflammatory and cytoprotective properties via activation of the Nrf2 pathway (Fox, 2012; Gold, 2012).
Pharmacokinetics/Pharmacodynamics
Distribution
Vd: MMF: 53 to 73 L
Metabolism
Undergoes rapid and extensive presystemic hydrolysis by esterases to its active metabolite, monomethyl fumarate (MMF); MMF is further metabolized via the tricarboxylic acid (TCA) cycle. Major serum metabolites include: MMF, fumaric acid, citric acid, and glucose.
Excretion
CO2 via exhalation (~60%); urine (16%; trace amounts as unchanged MMF), feces (1%)
Time to Peak
2 to 2.5 hours; delayed to 5.5 hours with food
Half-Life Elimination
MMF: ~1 hour
Protein Binding
MMF: 27% to 45%
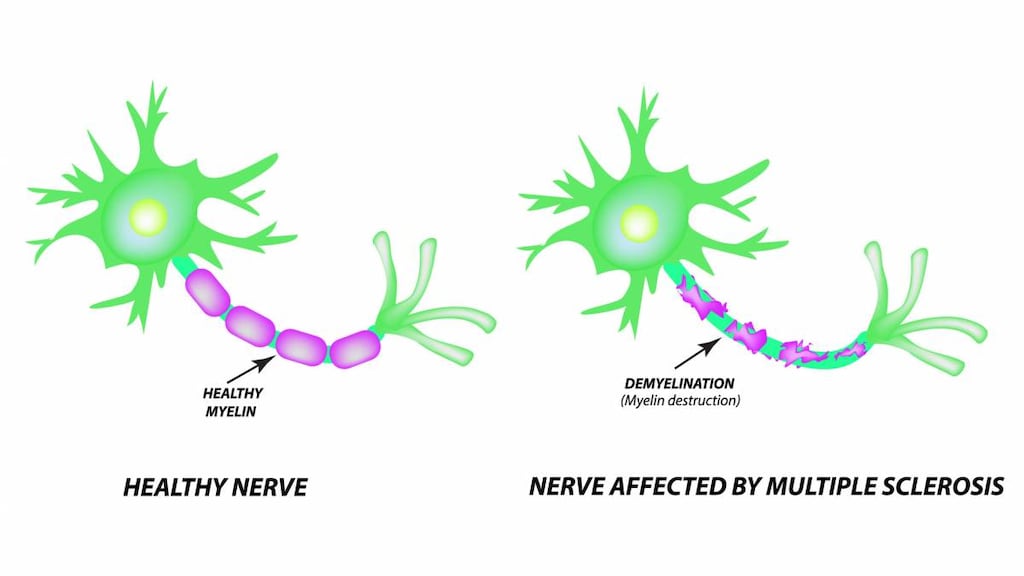
Use: Labeled Indications
Multiple sclerosis, relapsing: Treatment of patients with relapsing forms of multiple sclerosis, including clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease.
Contraindications
Known hypersensitivity (eg, anaphylaxis, angioedema) to dimethyl fumarate or any component of the formulation
Dosage and Administration
Dosing: Adult
Multiple sclerosis, relapsing: Oral: Initial: 120 mg twice daily; after 7 days, increase to the maintenance dose: 240 mg twice daily
Dosing: Geriatric
Refer to adult dosing.
Dosing: Adjustment for Toxicity
Flushing, GI intolerance, or intolerance to maintenance dose: Consider temporary dose reduction to 120 mg twice daily (resume recommended maintenance dose of 240 mg twice daily within 4 weeks). Consider discontinuation in patients who cannot tolerate return to the maintenance dose.
Hepatic injury (suspected drug-induced), clinically significant: Discontinue treatment.
Lymphocyte count <500/mm3 persisting for >6 months: Consider treatment interruption.
Serious infection: Consider withholding treatment until infection resolves.
Administration
Oral: Swallow capsules whole and intact; do not crush, chew, open the capsule, or sprinkle contents on food. Administer with or without food; administering with high-fat, high-protein food (eg, yogurt or peanut butter) may decrease the incidence of flushing and gastrointestinal effects (Mayer 2017). Administration of aspirin (nonenteric coated up to a dose of 325 mg) 30 minutes prior to dimethyl fumarate may also reduce the incidence of flushing.
Storage
Store at 15°C to 30°C (50°F to 86°F). Protect capsules from light and store in the original container.
Dimethyl Fumarate Images
Drug Interactions
Diroximel Fumarate: Dimethyl Fumarate may enhance the adverse/toxic effect of Diroximel Fumarate. Avoid combination
Vaccines (Live): Dimethyl Fumarate may enhance the adverse/toxic effect of Vaccines (Live). Specifically, Dimethyl Fumarate may increase the risk of vaccinal infection. Dimethyl Fumarate may diminish the therapeutic effect of Vaccines (Live). Management: Canadian labeling for dimethyl fumarate states that live attenuated vaccine administration is not recommended during treatment. U.S. labeling does not mention this. Consider therapy modification
Adverse Reactions
>10%:
Cardiovascular: Flushing (40%)
Gastrointestinal: Abdominal pain (18%), diarrhea (14%), nausea (12%)
Infection: Infection (60%; similar to placebo)
1% to 10%:
Dermatologic: Pruritus (8%), skin rash (8%), erythema of skin (5%)
Endocrine & metabolic: Albuminuria (6%)
Gastrointestinal: Vomiting (9%), dyspepsia (5%)
Hematologic & oncologic: Lymphocytopenia (2% to 6%)
Hepatic: Increased serum aspartate aminotransferase (4%)
<1%, postmarketing, and/or case reports: Abnormal hepatic function tests, anaphylaxis, angioedema, eosinophilia (transient), progressive multifocal leukoencephalopathy
Warnings/Precautions
Concerns related to adverse effects:
- Dermatitis/irritation: May cause rash, pruritus, or erythema. There are case reports of contact dermatitis resulting from dimethyl fumarate exposure after use as a fungicide and desiccant in the shipping of furniture (Bruze 2011; Giménez-Arnau 2011; Ropper 2012).
- Flushing: Commonly causes mild to moderate flushing (eg, warmth, redness, itching, burning sensation); flushing generally appears soon after initiation, and improves or resolves with subsequent dosing. Administration with food may decrease flushing incidence. Administration of aspirin (nonenteric coated ≤325 mg) 30 minutes prior to dimethyl fumarate or a temporary dose reduction may also reduce the incidence and severity of flushing.
- Gastrointestinal events: GI events (eg, nausea, vomiting, diarrhea, abdominal pain, dyspepsia) commonly occur with use; GI events generally occur in the first month of use and decrease thereafter. To improve tolerability, administer with food or temporarily reduce the dosage.
- Hepatotoxicity: Clinically significant postmarketing cases of hepatic injury have been reported, with an onset ranging from a few days to several months after treatment initiation. Signs/symptoms of hepatic injury, including transaminase elevations >5 times the upper ULN and total bilirubin elevations >2 times ULN have been observed. Some cases have required hospitalization; however, none of the cases were fatal or resulted in liver failure or transplant. Liver function test abnormalities resolved upon discontinuation. Drug-induced hepatocellular injury resulting in new-onset transaminase elevations combined with increased bilirubin levels is an important predictor of serious hepatic injury that may lead to acute hepatic failure, liver transplant, or death in some patients. Transaminase elevations (usually <3 times ULN) were observed in clinical trials, generally occurring in the first 6 months of treatment. Transaminase elevations ≥3 times ULN occurred rarely. Monitor liver function tests prior to treatment initiation and during treatment. Discontinue treatment if dimethyl fumarate-induced hepatic injury is suspected.
- Hypersensitivity reactions: Anaphylaxis and angioedema may occur after the first dose or at any time during treatment. Discontinue therapy if signs and symptoms of anaphylaxis or angioedema occur.
- Infections: Serious cases of herpes zoster (eg, disseminated, ophthalmicus, meningoencephalitis, meningomyelitis) have been reported; may develop any time during treatment. Other serious opportunistic infections have occurred, including viral (eg, Cytomegalovirus, herpes simplex, West Nile), fungal (eg, Aspergillus, Candida), and bacterial (eg, Listeria monocytogenes, Mycobacterium tuberculosis, Nocardia), in patients with and without lymphopenia. Consider temporary interruption of therapy until infection has resolved.
- Lymphopenia: Decreased lymphocyte counts may occur. The risk for lymphopenia is not reduced over time. A decline in absolute lymphocyte count (ALC) typically occurs in the first year of treatment and stabilizes, though an early ALC drop has been associated with later development of severe, prolonged lymphopenia. With a decline in ALC, an accompanying proportional decline occurs in lymphocyte subsets (eg, CD4+ and CD8+ central memory T-cells, memory B-cells) but is offset by a proportional increase in activated CD4+ and CD8+ T-cells, naive B-cells, and NK cells. Likely due to the shift in lymphocyte immunophenotypes, no increased risk of serious infections is seen in patients with a low T-cell subset count rendering monitoring of lymphocyte subsets of no clinical use (Mehta 2019). Obtain a CBC including lymphocyte count prior to initiation of therapy, then every 3 months thereafter, or as clinically indicated (AAN [Rae-Grant 2018]). Monitor for signs of infection in patients with lower lymphocyte counts at baseline and mild to moderate lymphopenia (Baharnoori 2018). Consider therapy interruption in patients with lymphocyte counts <500/mm3 persisting >6 months and in patients with serious infections. Progressive multifocal leukoencephalopathy (PML) may occur in patients with a lymphocyte count <500/mm3 for less than 6 months (Lehmann-Horn 2016). Due to a potential for delayed lymphocyte recovery following treatment interruption or discontinuation, monitor lymphocyte counts until lymphopenia is resolved. The decision to restart dimethyl fumarate should be individualized based on clinical circumstances. Dimethyl fumarate has not been studied in patients with preexisting low lymphocyte counts.
- Proteinuria: In clinical trials, proteinuria was reported at a slightly higher incidence than that observed with placebo; significance of these findings is unknown.
- Progressive multifocal leukoencephalopathy: Cases of progressive multifocal leukoencephalopathy (PML) due to the John Cunningham (JC) virus, including fatality, have been reported. The most common risk factors were persistent leukocytopenia, sarcoidosis, cancer history, and prior immunosuppressant use (Jamilloux 2014; Tan 2010). However, cases have been reported in patients who were not immunocompromised and had no prior exposure to immunosuppressive drugs, including natalizumab. Severe, long-standing lymphopenia was identified as a primary risk for PML, and the majority of PML cases occurred in patients with lymphocyte counts <800/mm3 (although the exact role of lymphopenia in PML is unknown). At the first sign or symptom suggestive of PML, withhold therapy immediately and perform a diagnostic evaluation; symptoms progress over days to weeks and may include progressive weakness on one side of the body or clumsiness of limbs, vision disturbances, and mental status changes. Cases of PML have been diagnosed based on MRI findings and the detection of JC virus DNA in the CSF without specific PML signs/symptoms. Monitoring with brain MRI for signs that may be consistent with PML may be beneficial and allow for an early diagnosis of PML (EMA 2015).
Concomitant drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Polysorbate 80: Some dosage forms may contain polysorbate 80 (also known as Tweens). Hypersensitivity reactions, usually a delayed reaction, have been reported following exposure to pharmaceutical products containing polysorbate 80 in certain individuals (Isaksson 2002; Lucente 2000; Shelley 1995). Thrombocytopenia, ascites, pulmonary deterioration, and renal and hepatic failure have been reported in premature neonates after receiving parenteral products containing polysorbate 80 (Alade 1986; CDC 1984). See manufacturer's labeling.
Monitoring Parameters
CBC including lymphocyte counts (obtained prior to initiation of therapy, then every 3 months thereafter and as clinically necessary; grade 3 lymphopenia should be monitored more frequently at intervals <3 months) (AAN [Rae-Grant 2018]); liver function tests (transaminases, alkaline phosphatase, total bilirubin) prior to treatment initiation and during treatment as clinically indicated; urinalysis (if proteinuria suspected and/or clinically indicated); MRI (baseline and as clinically indicated to monitor for early signs of progressive multifocal leukoencephalopathy [PML]). Monitor for signs/symptoms of hypersensitivity, infections, and/or PML.
Pregnancy
Pregnancy Considerations
Information related to the use of dimethyl fumarate in pregnancy is limited (Gold 2015; MacDonald 2019; Nguyen 2019).
In general, disease-modifying therapies for multiple sclerosis are stopped prior to a planned pregnancy, and not initiated during pregnancy, except in females at high risk of multiple sclerosis activity (AAN [Rae-Grant 2018]). Consider use of agents other than dimethyl fumarate for females at high risk of disease reactivation who are planning a pregnancy. Delaying pregnancy is recommended for females with persistent high disease activity; when disease-modifying therapy is needed in these patients, other agents are preferred (ECTRIMS/EAN [Montalban 2018]).
Females exposed to dimethyl fumarate during pregnancy are encouraged to enroll in the Pregnancy Registry by calling 866-810-1462 or visiting www.tecfiderapregnancyregistry.com.
Patient Education
What is this drug used for?
- It is used to treat MS (multiple sclerosis).
Frequently reported side effects of this drug
- Flushing
- Abdominal pain
- Diarrhea
- Vomiting
- Nausea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
- Progressive multifocal leukoencephalopathy like confusion, depression, trouble with memory, behavioral changes, change in strength on one side is greater than the other, difficulty speaking, change in balance, or vision changes
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.