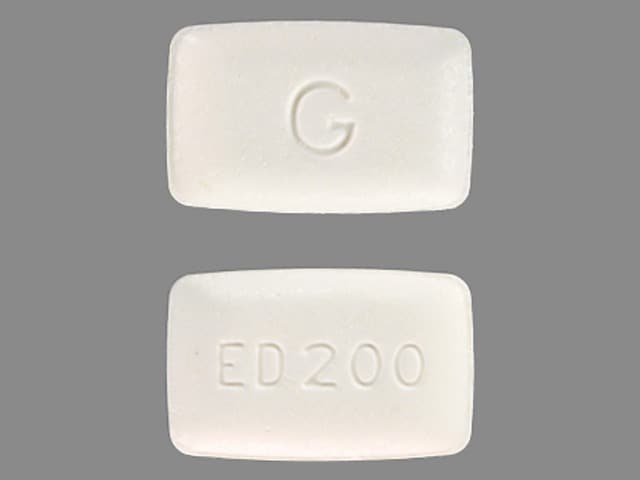
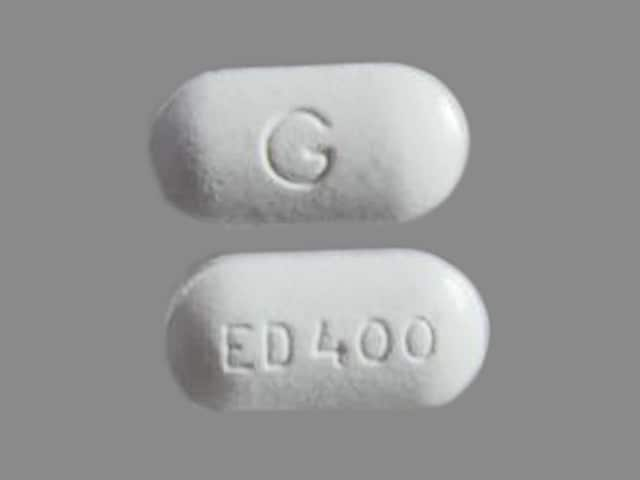
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Tablet, Oral, as disodium:
Generic: 200 mg [DSC], 400 mg [DSC]
Pharmacology
Mechanism of Action
Decreases bone resorption by inhibiting osteocytic osteolysis; decreases mineral release and matrix or collagen breakdown in bone
Pharmacokinetics/Pharmacodynamics
Absorption
~3%
Metabolism
None
Excretion
Primarily urine (50% as unchanged drug); feces (as unabsorbed drug)
Onset of Action
1 to 3 months
Duration of Action
Can persist for 12 months without continuous therapy
Half-Life Elimination
1 to 6 hours
Use: Labeled Indications
Heterotopic ossification: Prevention and treatment of heterotopic ossification due to spinal cord injury or after total hip replacement
Paget disease: Symptomatic treatment of Paget disease of bone
Note: Not generally a recommended treatment option; guidelines recommend the use of more potent bisphosphonate therapy (eg, zoledronic acid) (Endocrine Society [Singer 2014]; Ralston 2019).
Contraindications
Hypersensitivity to bisphosphonates or any component of the formulation; overt osteomalacia; patients with abnormalities of the esophagus (eg, stricture, achalasia) which delay esophageal emptying
Dosage and Administration
Dosing: Adult
Patients should receive supplemental calcium and vitamin D if dietary intake is inadequate.
Paget disease: Oral:
Initial: 5 mg/kg/day (not to exceed 6 months) is recommended as initial therapy; if higher doses are needed, may give 5 to 10 mg/kg/day (not to exceed 6 months) or 11 to 20 mg/kg/day (not to exceed 3 months). Doses >10 mg/kg/day should be used only when lower doses are ineffective or there is a need to suppress rapid bone turnover (ie, potential for irreversible neurologic damage) or reduce elevated cardiac output. Doses >20 mg/kg/day are not recommended.
Re-treatment: Initiate only after etidronate-free period ≥90 days. Monitor patients every 3 to 6 months. Re-treatment regimens are the same as for initial treatment. In cases where the original dose is not adequate, consider increasing the dose within the recommended guidelines.
Heterotopic ossification: Oral:
Caused by spinal cord injury: 20 mg/kg/day for 2 weeks, then 10 mg/kg/day for 10 weeks; total treatment period: 12 weeks
Complicating total hip replacement: 20 mg/kg/day for 1 month preoperatively then 20 mg/kg/day for 3 months postoperatively; total treatment period is 4 months
Re-treatment: Has not been studied.
Dosing: Geriatric
Refer to adult dosing. Use with caution and monitor closely.
Dosing: Pediatric
Heterotopic ossification, traumatic brain injury: Limited data available: Children and Adolescents: Oral: Initial: 20 mg/kg/dose once daily for 2 to 4 weeks, then decrease to 10 mg/kg/dose once daily for 12 weeks to 1 year (Hurvitz 1992).
Administration
Administer tablet on an empty stomach with a full glass of plain water (6 to 8 oz) 2 hours before food. Patients should be instructed to stay upright (not to lie down) after taking the medication. If gastrointestinal discomfort occurs, the dose may be divided.
Dietary Considerations
Ensure adequate calcium and vitamin D intake; women and men >50 years of age should consume 1,200 to 1,500 mg/day of elemental calcium and 800 to 1,000 units/day of vitamin D. Tablet should be taken with water or fruit juice on an empty stomach; avoid administering foods/supplements with calcium, iron, or magnesium within 2 hours of drug. Do not take with mineral water or with other beverages.
Storage
Store at controlled room temperature of 25°C (77°F).
Etidronate Images
Drug Interactions
Aminoglycosides: May enhance the hypocalcemic effect of Bisphosphonate Derivatives. Monitor therapy
Angiogenesis Inhibitors (Systemic): May enhance the adverse/toxic effect of Bisphosphonate Derivatives. Specifically, the risk for osteonecrosis of the jaw may be increased. Monitor therapy
Deferasirox: Bisphosphonate Derivatives may enhance the adverse/toxic effect of Deferasirox. Specifically, the risk for GI ulceration/irritation or GI bleeding may be increased. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents: May enhance the adverse/toxic effect of Bisphosphonate Derivatives. Both an increased risk of gastrointestinal ulceration and an increased risk of nephrotoxicity are of concern. Monitor therapy
Polyvalent Cation Containing Products: May decrease the serum concentration of Bisphosphonate Derivatives. Management: Avoid administration of oral medications containing polyvalent cations within: 2 hours before or after tiludronate/clodronate/etidronate; 60 minutes after oral ibandronate; or 30 minutes after alendronate/risedronate. Consider therapy modification
Proton Pump Inhibitors: May diminish the therapeutic effect of Bisphosphonate Derivatives. Monitor therapy
Test Interactions
Bisphosphonates may interfere with diagnostic imaging agents such as technetium-99m-diphosphonate in bone scans.
Adverse Reactions
Gastrointestinal: Diarrhea (≤30%; dose dependent), nausea (≤30%; dose dependent)
Neuromuscular & skeletal: Ostealgia (10% to 20%; dose dependent)
Postmarketing and/or case reports: Agranulocytosis, alopecia, amnesia, angioedema, arthralgia, arthritis, bone fracture, confusion, depression, erythema multiforme, esophagitis, exacerbation of asthma, exacerbation of peptic ulcer, folliculitis, gastritis, glossitis, glossopyrosis, hallucination, headache, hypersensitivity reaction, leg cramps, leukemia, leukopenia, maculopapular rash, osteomalacia, osteonecrosis of the jaw, pancytopenia, paresthesia, pruritus, skin rash (macular), Stevens-Johnson syndrome, toxic epidermal necrolysis, urticaria
Warnings/Precautions
Concerns related to adverse effects:
- Bone/joint/muscle pain: Infrequently, severe (and occasionally debilitating) bone, joint, and/or muscle pain have been reported during bisphosphonate treatment. The onset of pain ranged from a single day to several months. Consider discontinuing therapy in patients who experience severe symptoms; symptoms usually resolve upon discontinuation. Some patients experienced recurrence when rechallenged with same drug or another bisphosphonate; avoid use in patients with a history of these symptoms in association with bisphosphonate therapy.
- Fracture risk: Do not exceed recommended dose or use continuously for >6 months in patients with Paget's disease; risk of osteomalacia or fractures may be increased. Long bones with predominantly lytic lesions may be prone to fracture, particularly in patients unresponsive to treatment.
- GI mucosa irritation: May cause irritation to upper GI mucosa. Esophagitis, dysphagia, esophageal ulcers, esophageal erosions, and esophageal stricture (rare) have been reported with oral bisphosphonates; risk increases in patients unable to comply with dosing instructions. Use with caution in patients with dysphagia, esophageal disease, gastritis, duodenitis, or ulcers (may worsen underlying condition). Discontinue use if new or worsening symptoms develop.
- Osteonecrosis of the jaw: Osteonecrosis of the jaw (ONJ), also referred to as medication-related osteonecrosis of the jaw (MRONJ), has been reported in patients receiving bisphosphonates; this has been observed primarily following dental procedures such as tooth extractions and in cancer patients receiving IV bisphosphonates, but has also occurred in patients with postmenopausal osteoporosis and other diagnoses receiving oral bisphosphonates. Risk factors for MRONJ include invasive dental procedures (eg, tooth extraction, dental implants, boney surgery), cancer diagnosis, concomitant chemotherapy, radiotherapy, or corticosteroids; anemia, coagulopathy, infection, ill-fitting dentures, or preexisting dental disease. According to a position paper by the American Association of Maxillofacial Surgeons (AAOMS), MRONJ has been associated with bisphosphonate and other antiresorptive agents (denosumab), and antiangiogenic agents (eg, bevacizumab, sunitinib) used for the treatment of osteoporosis or malignancy. The manufacturer’s labeling states that discontinuing bisphosphonates in patients requiring invasive dental procedures may reduce the risk of ONJ and clinical judgment should guide the decision. However, the AAOMS suggests there is currently no evidence that interrupting oral bisphosphonate therapy alters the risk of ONJ following tooth extraction, and that in patients receiving oral bisphosphonates for <4 years who have no clinical risk factors, no alternations or delay in any procedure common to oral/maxillofacial surgeons, periodontists, and other dental providers is necessary (special considerations apply to patients receiving dental implants). Conversely, in patients receiving oral bisphosphonates for >4 years or in patients receiving oral bisphosphonates for <4 years who have also taken corticosteroids or antiangiogenic medications concomitantly, the AAOMS recommends considering a 2-month drug free period prior to invasive dental procedures (recommendation based on a theoretical benefit). Patients developing ONJ during therapy should receive care by an oral surgeon (AAOMS [Ruggiero 2014]). According to the manufacturer, discontinuation of the bisphosphonate therapy should be considered (based on risk/benefit evaluation) in patients who develop ONJ.
Disease-related concerns:
- Bariatric surgery: Altered absorption and ulceration risk: Avoid oral bisphosphates after bariatric surgery; inadequate oral absorption and potential anastomotic ulceration may occur. If therapy is indicated, IV administered bisphosphonates are recommended.
- Enterocolitis: Use with caution in patients with enterocolitis; diarrhea has been reported at high doses and therapy may need to be withheld.
- Renal impairment: Use with caution in patients with renal impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Bone mineralization: May retard mineralization of bone; treatment may need delayed or interrupted until callus is present.
- Calcium/vitamin D intake: Ensure adequate calcium and vitamin D intake.
Monitoring Parameters
Paget disease: Serum total alkaline phosphatase at 6 to 12 weeks for initial response to treatment (when bone turnover will have shown a substantial decline) and potentially at 6 months (maximal suppression of high bone turnover); following treatment completion, monitor at ~6- to 12-month intervals (Endocrine Society [Singer 2014]); monitoring more specific biochemical markers of bone turnover (eg, serum P1NP, NTX, serum beta-CTx) is generally only warranted in patients with Paget disease who have abnormal liver or biliary tract function or when early assessment of response to treatment is needed (eg, spinal compression, very active disease) (Endocrine Society [Singer 2014]); pain (posttreatment pain may not strictly correlate with increased biochemical markers [Ralston 2019]); serum calcium and 25(OH)D.
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
It is not known if bisphosphonates cross the placenta, but based on their lower molecular weight, fetal exposure is expected (Djokanovic 2008; Stathopoulos 2011).
Information related to the use of etidronate in pregnancy is available from case reports and small retrospective studies (Levy 2009; Sokal 2019; Vujasinovic-Stupar 2012).
Bisphosphonates are incorporated into the bone matrix and gradually released over time. The amount available in the systemic circulation varies by drug, dose, and duration of therapy. Theoretically, there may be a risk of fetal harm when pregnancy follows the completion of therapy (hypocalcemia, low birth weight, and decreased gestation have been observed in some case reports); however, available data have not shown that exposure to bisphosphonates during pregnancy significantly increases the risk of adverse fetal events (Djokanovic 2008; Green 2014; Levy 2009; Sokal 2019; Stathopoulos 2011). Exposed infants should be monitored for hypocalcemia after birth (Djokanovic 2008; Stathopoulos 2011).
Use of bisphosphonates in premenopausal females should be reserved for special circumstances when rapid bone loss is occurring (Bhalla 2010; Pereira 2012; Stathopoulos 2011).
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience nausea or diarrhea. Have patient report immediately to prescriber black, tarry, or bloody stools; chest pain; sore throat; vomiting blood; severe abdominal pain; heartburn; difficulty swallowing; pain with swallowing; severe bone pain; severe joint pain; severe muscle pain; groin, hip, or thigh pain; jaw pain; or jaw edema (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for health care professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience, and judgment in diagnosing, treating, and advising patients.