Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Solution, Intravenous:
Generic: 20 mg (50 mL); 40 mg/4 mL (4 mL); 200 mg/20 mL (20 mL)
Solution, Intravenous [preservative free]:
Generic: 20 mg/2 mL (2 mL)
Suspension Reconstituted, Oral:
Pepcid: 40 mg/5 mL (50 mL [DSC]) [contains methylparaben sodium, propylparaben sodium, sodium benzoate; cherry banana mint flavor]
Generic: 40 mg/5 mL (50 mL)
Tablet, Oral:
Acid Controller Max St: 20 mg
Acid Controller Original Str: 10 mg
Acid Reducer: 10 mg
Acid Reducer Maximum Strength: 20 mg
Heartburn Relief: 10 mg
Heartburn Relief Max St: 20 mg
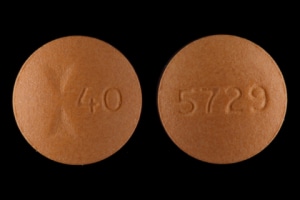
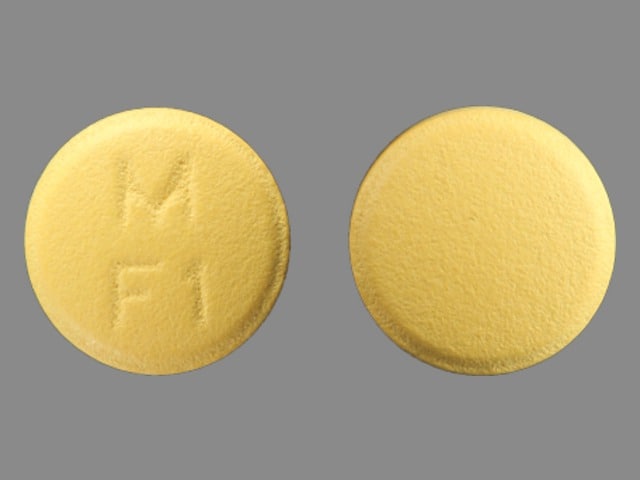
Pepcid: 20 mg, 40 mg [contains corn starch]
Pepcid AC Maximum Strength: 20 mg
Generic: 10 mg, 20 mg, 40 mg
Pharmacology
Mechanism of Action
Competitive inhibition of histamine at H2 receptors of the gastric parietal cells, which inhibits gastric acid secretion
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Incompletely absorbed
Distribution
Vd: IV:
Infants: ≤3 months: 1.4 ± 0.4 L/kg to 1.8 ± 0.3 L/kg; >3 to 12 months: 2.3 ± 0.7 L/kg
Children <11 years: 2.07 ± 1.49 L/kg
Children ≥11 years and Adolescents ≤15 years: 1.5 ± 0.4 L/kg
Adults: 1.3 ± 0.2 L/kg
Metabolism
30% to 35%; minimal first-pass metabolism; forms one metabolite (S-oxide)
Excretion
Urine (25% to 30% [oral], 65% to 70% [IV] as unchanged drug)
Clearance: IV:
Infants: ≤3 months: 0.13 ± 0.06 to 0.21 ± 0.06 L/hour/kg; >3 to 12 months: 0.49 ± 0.17 L/hour/kg
Children <11 years: 0.54 ± 0.34 L/hour/kg
Children ≥11 years and Adolescents ≤15 years: 0.48 ± 0.14 L/hour/kg
Adults: 0.39 ± 0.14 L/hour/kg
Onset of Action
Antisecretory effect: Oral: Within 1 hour; Peak effect: Antisecretory effect: Oral: Within 1 to 3 hours (dose-dependent); IV: Within 30 minutes
Time to Peak
Serum: Oral: ~1 to 3 hours
Duration of Action
Antisecretory effect: IV, Oral: 10 to 12 hours
Half-Life Elimination
IV:
Infants: ≤3 months: 8.1 ± 3.5 hours to 10.5 ± 5.4 hours; >3 to 12 months: 4.5 ± 1.1 hours
Children <11 years: 3.38 ± 2.6 hours
Children ≥11 years and Adolescents ≤15 years: 2.3 ± 0.4 hours
Adults: 2.5 to 3.5 hours; prolonged with renal impairment; Oliguria: >20 hours; Anuria: 24 hours
Protein Binding
15% to 20%
Use in Specific Populations
Special Populations: Renal Function Impairment
AUC increased at least 5-fold and at least 2-fold in adults with CrCl <30 mL/minute and CrCl 30 to 60 mL/minute, respectively.
Use: Labeled Indications
Oral:
Gastroesophageal reflux disease: Treatment of gastroesophageal reflux disease (GERD) and esophagitis due to GERD.
Heartburn (OTC only): Relief of heartburn, acid indigestion, and sour stomach.
Peptic ulcer disease: Treatment of active duodenal or gastric ulcers. Note: Although a labeled indication, proton pump inhibitors (PPIs) are considered the standard of care for treatment of peptic ulcer disease (PUD) rather than H2-receptor antagonists (eg, famotidine) (Lanas 2017; Vakil 2019).
Injection:
Patients not able to take oral medication: As an alternative to the oral dosage form for short-term use in patients who are unable to take oral medication.
Use: Off Label
Aspiration prophylaxis in patients undergoing anesthesiabyes
Data from multiple studies of varying methodologies support the use of H2-receptor antagonists for the prevention of aspiration in patients undergoing anesthesia Manchikanti 1984, Olsson 1982, O'Reardon 2011, Stuart 1996. Studies have encompassed a wide variety of patient populations and surgical and procedural settings, including (but not limited to) elective and emergency surgeries, rapid sequence intubation, and scheduled or emergent cesarean deliveries. Clinical experience and case reports also suggest use may be especially beneficial in patients at high risk for aspiration (eg, patients with a full stomach, severe GERD, gastroparesis, and/or pregnant patients undergoing anesthesia for electroconvulsive therapy [ECT]) Berkow 2019, Hagberg 2019, Kellner 2019, Nixon 2019.
Based on the American Society of Anesthesiologists (ASA) practice guidelines for obstetric anesthesia, famotidine is an effective and recommended prophylactic agent for the prevention of aspiration during surgical procedures (eg, cesarean delivery, postpartum tubal ligation) in pregnant patients.
Chronic spontaneous urticariayes
Based on a joint guideline published by the American Academy of Allergy, Asthma, and Immunology (AAAAI), American College of Allergy, Asthma, and Immunology (ACAAI), and the Joint Council of Allergy, Asthma, & Immunology, the addition of an H2-receptor antagonist (eg, famotidine) may be considered as adjunctive therapy to an H1 antihistamine in patients with insufficient response to a full-dose H1 antihistamine alone.
Infusion reaction, premedicationc
Clinical experience suggests the utility of H2-receptor antagonists (eg, famotidine) as adjunctive therapy for premedication prior to the infusion of certain chemotherapy agents (eg, certain taxanes) or biologics to prevent infusion reactions Castells 2019b.
Mastocytosisc
Clinical experience suggests the utility of H2-receptor antagonists (eg, famotidine) as adjunctive therapy for cutaneous or systemic mastocytosis Akin 2019, Castells 2019a.
Stress ulcer prophylaxis in select critically ill patientsbyes
A meta-analysis found no difference between PPIs and H2-receptor antagonists in terms of stress-related upper GI bleeding prophylaxis, pneumonia, and mortality in intensive care units Barbateskovic 2019, Reynolds 2018.
Based on the American Society of Health-System Pharmacists (ASHP) therapeutic guidelines on stress ulcer prophylaxis, H2-receptor antagonists are recommended for stress ulcer prophylaxis in critically ill patients, although there was limited data on the use of PPIs for stress ulcer prophylaxis at the time of publication.
Based on the Surviving Sepsis Campaign international guidelines for the management of sepsis and septic shock, stress ulcer prophylaxis using an H2-receptor antagonist or a PPI is recommended in sepsis or septic shock patients who have GI bleeding risk factors.
Contraindications
Serious hypersensitivity (eg, anaphylaxis) to famotidine, other H2 antagonists, or any component of the formulation
OTC labeling: When used for self-medication (OTC), do not use if trouble or pain when swallowing food, vomiting with blood, or bloody or black stools; allergic to other acid reducers; renal impairment; coadministration with other acid reducers.
Dosage and Administration
Dosing: Adult
Aspiration prophylaxis in patients undergoing anesthesia (off-label use): Note: May be considered in patients at high risk for aspiration (ASA 2016; Berkow 2019; Hagberg 2019; O'Reardon 2011; Rabheru 2001):
IV: 20 mg as a single dose ~40 to 90 minutes prior to induction of anesthesia; may be given with a rapid-acting nonparticulate antacid (eg, oral sodium citrate and citric acid) and/or metoclopramide (Abir 2019; ASA 2016; ASA 2017; Berkow 2019; McCammon 1986).
Chronic spontaneous urticaria (alternative agent) (adjunct) (off-label use): Note: Use as additional therapy if insufficient response to full-dose H1 antihistamine.
Oral: 20 mg twice daily given in combination with H1 antihistamine; a trial of 2 to 4 weeks is suggested to assess response (Bernstein 2014; Kahn 2019; Kulthanan 2016).
Gastroesophageal reflux disease, treatment:
Initial therapy:
Mild and intermittent symptoms (<2 episodes/week), and no evidence of erosive esophagitis: Note: For more severe or frequent initial symptoms, with or without evidence of erosive esophagitis, a proton pump inhibitor (PPI) as initial therapy is recommended.
Oral: 10 mg twice daily as needed; if symptoms persist after 2 to 4 weeks, increase to 20 mg twice daily for 2 weeks; if symptoms improve, may continue therapy as needed (Kahrilas 2019).
Note: If symptoms persist after 2 weeks of 20 mg twice daily, discontinue and consider PPI therapy (Kahrilas 2019).
Residual acid reflux symptoms despite maximal PPI therapy (adjunct): Oral: 20 mg once daily given at bedtime in addition to PPI therapy (ACG [Katz 2013]; Wang 2009); may also administer famotidine intermittently or on demand with scheduled PPI (Fass 2019).
OTC labeling (patient-guided therapy): Heartburn, mild intermittent symptoms: Oral: 10 to 20 mg up to twice daily when needed (maximum: 40 mg/day); may also be taken 10 to 60 minutes before meals or beverages that cause heartburn (maximum: 40 mg/day).
Infusion reaction, premedication (adjunct) (off-label use): IV, Oral: 20 mg typically administered 30 to 60 minutes prior to infusion of certain chemotherapy agents or biologics; usually given in conjunction with an H1 antihistamine (eg, diphenhydramine) and glucocorticoid (refer to institutional protocols) (Castells 2019b).
Mastocytosis (adjunct) (off-label use): Oral: 10 to 20 mg every 12 hours adjusted to achieve GI symptom relief. Typically used in combination with other appropriate agent(s) (eg, H1 antihistamine and/or leukotriene inhibitor) (Akin 2019; Castells 2019a).
Stress ulcer prophylaxis in select critically ill patients (off-label use): Note: For ICU patients with associated risk factors for GI bleeding (including coagulopathy, mechanical ventilation for >48 hours, traumatic brain injury, history of GI ulceration or bleeding within past year, extensive burns); discontinue prophylaxis once risk factors have resolved (Rhodes 2017; Weinhouse 2019).
Oral or via nasogastric (NG) tube (alternative to enteral PPI): 20 mg twice daily (ASHP 1999; Weinhouse 2019)
IV: 20 mg twice daily (ASHP 1999; Weinhouse 2019)
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
GERD:
Oral:
Suspension:
Infants <3 months: 0.5 mg/kg/dose once daily for up to 8 weeks; if not effective after 2 weeks, increasing to 1 mg/kg/dose once daily has been suggested (Orenstein 2003)
Infants ≥3 months, Children, and Adolescents ≤16 years: Initial: 0.5 mg/kg/dose twice daily; maximum dose: 40 mg/dose; doses up to 1 mg/kg/dose twice daily have been reported (Orenstein 2003)
Tablets: Children and Adolescents ≥40 kg: 20 mg twice daily for up to 6 weeks; for esophagitis and accompanying symptoms due to GERD, may use 20 to 40 mg twice daily for up to 12 weeks
IV:
Infants <3 months: Limited data available: 0.25 mg/kg/dose once daily; dosing based on a pharmacokinetic study which included 7 patients <3 months who received IV famotidine (Wenning 2005)
Infants ≥3 months: Limited data available: Initial: 0.25 mg/kg/dose every 12 hours; maximum dose: 20 mg/dose; dosing based on a pharmacokinetic study which included 11 patients >3 to 12 months who received IV famotidine (Wenning 2005)
Children and Adolescents: Initial: 0.25 mg/kg/dose every 12 hours; maximum dose: 20 mg/dose; doses up to 0.5 mg/kg/dose every 12 hours have been reported
Heartburn, acid indigestion, or sour stomach (OTC labeling): Children ≥12 years and Adolescents: Oral: 10 to 20 mg every 12 hours; dose may be taken 15 to 60 minutes before eating foods known to cause heartburn; maximum daily dose: 2 tablets/day (20 to 40 mg dependent upon OTC product)
Pathological hypersecretory conditions (eg, Zollinger-Ellison): Adolescents ≥17 years:
Oral: Initial: 20 mg every 6 hours, may increase up to 160 mg every 6 hours
IV: 20 mg every 12 hours
Peptic ulcer disease:
Oral:
Suspension: Children and Adolescents ≤16 years: 0.5 mg/kg/day at bedtime or divided twice daily; maximum daily dose: 40 mg/day; doses up to 1 mg/kg/day at bedtime or divided twice daily have been used
Tablets: Children and Adolescents >40 kg:
Duodenal ulcer: Acute therapy: 40 mg once daily at bedtime or 20 mg twice daily for 4 to 8 weeks
Gastric ulcer: Acute therapy: 40 mg once daily at bedtime for up to 8 weeks
IV: Children and Adolescents: Initial: 0.25 mg/kg/dose every 12 hours; maximum dose: 20 mg/dose; doses up to 0.5 mg/kg/dose every 12 hours have been reported
Stress ulcer prophylaxis, gastric acid suppression: Limited data available: Infants, Children, and Adolescents: IV: 1 to 2 mg/kg/day in divided doses every 8 to 12 hours; maximum daily dose: 40 mg/day (Aanpreung 1998; ASHP 1999; Behrens 1994; Kraus 1990; Treem 1991)
Reconstitution
Solution for injection:
IV push: Dilute 2 mL (20 mg) with NS (or another compatible solution) to a total of 5 to 10 mL. May also administer undiluted (Lipsy 1995).
Infusion: Dilute 2 mL (20 mg) with 100 mL of D5W or another compatible solution.
Extemporaneously Prepared
Note: A famotidine suspension (8 mg/mL) is commercially available.
8 mg/mL Oral Suspension
An 8 mg/mL oral suspension may be made with tablets. Crush seventy 40 mg tablets in a mortar and reduce to a fine powder. Add small portions of sterile water and mix to a uniform paste. Mix while adding a 1:1 mixture of Ora-Plus and Ora-Sweet in incremental proportions to almost 350 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 350 mL. Label "shake well." Stable for 95 days at room temperature.
Dentinger PJ, Swenson CF, Anaizi NH. Stability of famotidine in an extemporaneously compounded oral liquid. Am J Health Syst Pharm. 2000;57(14):1340-1342.10918924
Administration
IV push: Administer over at least 2 minutes.
Solution for infusion: Administer over 15 to 30 minutes.
Oral: Administer without regard to meals. May administer with antacids.
Suspension: Shake vigorously before use.
Tablet (OTC): Do not chew. To prevent symptoms, administer 10 to 60 minutes before eating food or drinking beverages known to cause heartburn.
Storage
Oral:
Powder for oral suspension: Prior to reconstitution, store at 25°C (77°F). Reconstituted oral suspension is stable for 30 days at room temperature; do not freeze.
Tablet: Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from light.
IV:
Solution for injection: Prior to use, store at 2°C to 8°C (36°F to 46°F). If solution freezes, allow to solubilize at room temperature. Protect from light.
IV push: Following preparation, solutions for IV push should be used immediately, or may be stored in refrigerator and used within 48 hours.
Infusion: Following dilution in D5W, D10W, NS or LR, may be stored for up to 48 hours under refrigeration; however, solutions for infusion have been found to be physically and chemically stable for 7 days at room temperature (maintains at least 90% of initial potency).
Solution for injection, premixed bags: Store at 25°C (77°F); avoid excessive heat.
Famotidine Images
Drug Interactions
Acalabrutinib: Histamine H2 Receptor Antagonists may decrease the serum concentration of Acalabrutinib. Management: To minimize the potential for a significant interaction, separate administration of these agents by giving acalabrutinib 2 hours before ingestion of a histamine-2 receptor antagonist. Consider therapy modification
Atazanavir: Histamine H2 Receptor Antagonists may decrease the serum concentration of Atazanavir. Management: Specific dose limitations and administration guidelines exist; consult full interaction monograph or atazanavir prescribing information. Consider therapy modification
Bosutinib: Histamine H2 Receptor Antagonists may decrease the serum concentration of Bosutinib. Management: Administer histamine H2 receptor antagonists more than 2 hours before or after bosutinib. Consider therapy modification
Cefditoren: Histamine H2 Receptor Antagonists may decrease the serum concentration of Cefditoren. Management: Concomitant use of cefditoren with H2-antagonists and antacids is not recommended. Consider alternative methods to control acid reflux (eg, diet modification) or alternative antimicrobial therapy if use of H2-antagonists can not be avoided. Consider therapy modification
Cefpodoxime: Histamine H2 Receptor Antagonists may decrease the absorption of Cefpodoxime. Separate oral doses by at least 2 hours. Monitor therapy
Cefuroxime: Histamine H2 Receptor Antagonists may decrease the absorption of Cefuroxime. Separate oral doses by at least 2 hours. Avoid combination
Cysteamine (Systemic): Histamine H2 Receptor Antagonists may diminish the therapeutic effect of Cysteamine (Systemic). Monitor therapy
Dacomitinib: Histamine H2 Receptor Antagonists may decrease the serum concentration of Dacomitinib. Management: Administer dacomitinib at least 6 hours before or 10 hours after an histamine H2-receptor antagonist (H2RA). Consider therapy modification
Dasatinib: Histamine H2 Receptor Antagonists may decrease the absorption of Dasatinib. Management: Antacids (taken 2 hours before or after dasatinib administration) can be used in place of H2-antagonists if some acid-reducing therapy is needed. Avoid combination
Delavirdine: Histamine H2 Receptor Antagonists may decrease the serum concentration of Delavirdine. Management: Chronic therapy with H2-antagonists should be avoided in patients who are being treated with delavirdine. The clinical significance of short-term H2-antagonist therapy with delavirdine is uncertain, but such therapy should be undertaken with caution. Avoid combination
Dexmethylphenidate: Histamine H2 Receptor Antagonists may increase the absorption of Dexmethylphenidate. Specifically, H2-antagonists may interfere with the normal release of drug from the extended-release capsules (Focalin XR brand), which could result in both increased absorption (early) and decreased delayed absorption. Monitor therapy
Dichlorphenamide: May increase the serum concentration of Famotidine. Avoid combination
Erdafitinib: May increase the serum concentration of OCT2 Substrates. Monitor therapy
Erlotinib: Histamine H2 Receptor Antagonists may decrease the serum concentration of Erlotinib. Management: Avoid H2-antagonists in patients receiving erlotinib when possible. If concomitant treatment cannot be avoided, erlotinib should be dosed once daily, 10 hours after and at least 2 hours before H2-antagonist dosing. Consider therapy modification
Fosamprenavir: Histamine H2 Receptor Antagonists may decrease the serum concentration of Fosamprenavir. Cimetidine may also inhibit the metabolism of the active metabolite amprenavir, making its effects on fosamprenavir/amprenavir concentrations difficult to predict. Monitor therapy
Gefitinib: Histamine H2 Receptor Antagonists may decrease the serum concentration of Gefitinib. Management: Administer gefitinib at least 6 hours before or after administration of a histamine H2-antagonist, and closely monitor clinical response to gefitinib. Consider therapy modification
Indinavir: Histamine H2 Receptor Antagonists may decrease the serum concentration of Indinavir. Monitor therapy
Iron Preparations: Histamine H2 Receptor Antagonists may decrease the absorption of Iron Preparations. Exceptions: Ferric Carboxymaltose; Ferric Citrate; Ferric Derisomaltose; Ferric Gluconate; Ferric Hydroxide Polymaltose Complex; Ferric Pyrophosphate Citrate; Ferumoxytol; Iron Dextran Complex; Iron Sucrose. Monitor therapy
Itraconazole: Histamine H2 Receptor Antagonists may increase the serum concentration of Itraconazole. Histamine H2 Receptor Antagonists may decrease the serum concentration of Itraconazole. Management: Administer Sporanox brand itraconazole at least 2 hours before or 2 hours after administration of any histamine H2 receptor antagonists (H2RAs). Exposure to Tolsura brand itraconazole may be increased by H2RAs; consider itraconazole dose reduction. Consider therapy modification
Ketoconazole (Systemic): Histamine H2 Receptor Antagonists may decrease the serum concentration of Ketoconazole (Systemic). Management: Administer oral ketoconazole at least 2 hours prior to use of any H2-receptor antagonist. Monitor patients closely for signs of inadequate clinical response to ketoconazole. Consider therapy modification
Ledipasvir: Histamine H2 Receptor Antagonists may decrease the serum concentration of Ledipasvir. Consider therapy modification
Mesalamine: Histamine H2 Receptor Antagonists may diminish the therapeutic effect of Mesalamine. Histamine H2-Antagonist-mediated increases in gastrointestinal pH may cause the premature release of mesalamine from specific sustained-release mesalamine products. Management: Consider avoiding concurrent administration of high-dose histamine H2-receptor antagonists with sustained-release mesalamine products. Consider therapy modification
Methylphenidate: Histamine H2 Receptor Antagonists may increase the absorption of Methylphenidate. Specifically, H2-antagonists may interfere with the normal release of drug from the extended-release capsules (Ritalin LA brand), which could result in both increased absorption (early) and decreased delayed absorption. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): Histamine H2 Receptor Antagonists may decrease the serum concentration of Multivitamins/Minerals (with ADEK, Folate, Iron). Specifically, the absorption of iron may be impaired by H2-antagonists. Monitor therapy
Nelfinavir: Histamine H2 Receptor Antagonists may decrease the serum concentration of Nelfinavir. Concentrations of the active M8 metabolite may also be reduced. Monitor therapy
Neratinib: Histamine H2 Receptor Antagonists may decrease the serum concentration of Neratinib. Specifically, histamine H2 receptor antagonists may reduce neratinib absorption. Management: Administer neratinib at least 2 hours before or 10 hours after administration of a histamine H2 receptor antagonist to minimize the impact of this interaction. Avoid combination
Nilotinib: Histamine H2 Receptor Antagonists may decrease the serum concentration of Nilotinib. Management: The nilotinib dose should be given 10 hours after or 2 hours before the H2 receptor antagonist in order to minimize the risk of a significant interaction. Consider therapy modification
PAZOPanib: Histamine H2 Receptor Antagonists may decrease the serum concentration of PAZOPanib. Management: Avoid the use of histamine H2-antagonists in combination with pazopanib. Strategies to minimize the expected interaction between these agents (eg, dose separation) have not been investigated. Avoid combination
Pexidartinib: Histamine H2 Receptor Antagonists may decrease the serum concentration of Pexidartinib. Management: Administer pexidartinib 2 hours before or 10 hours after histamine H2 receptor antagonists. Consider therapy modification
Posaconazole: Histamine H2 Receptor Antagonists may decrease the serum concentration of Posaconazole. Management: Avoid concurrent use of oral suspension with H2-antagonists whenever possible. Monitor patients closely for decreased antifungal effects if this combination is used. Delayed-release posaconazole tablets may be less likely to interact. Consider therapy modification
Rilpivirine: Histamine H2 Receptor Antagonists may decrease the serum concentration of Rilpivirine. Management: Administer histamine H2 receptor antagonists at least 12 hours before or 4 hours after rilpivirine. Consider therapy modification
Risedronate: Histamine H2 Receptor Antagonists may increase the serum concentration of Risedronate. This applies specifically to delayed-release risedronate. Avoid combination
Saquinavir: Histamine H2 Receptor Antagonists may increase the serum concentration of Saquinavir. Monitor therapy
Secretin: Histamine H2 Receptor Antagonists may diminish the diagnostic effect of Secretin. Specifically, use of H2-Antagonists may cause a hyperresponse in gastrin secretion in response to secretin stimulation testing, falsely suggesting gastrinoma. Management: Avoid concomitant use of histamine H2-antagonists (H2RAs) and secretin. Discontinue H2RAs at least 2 days prior to secretin administration. Consider therapy modification
Tafenoquine: May increase the serum concentration of OCT2 Substrates. Management: Avoid use of OCT2 substrates with tafenoquine, and if the combination cannot be avoided, monitor closely for evidence of toxicity of the OCT2 substrate and consider a reduced dose of the OCT2 substrate according to that substrate's labeling. Consider therapy modification
Varenicline: Histamine H2 Receptor Antagonists may increase the serum concentration of Varenicline. Management: Monitor for increased varenicline adverse effects with concomitant use of cimetidine or other H2-antagonists, particularly in patients with severe renal impairment. International product labeling recommendations vary. Consult appropriate labeling. Monitor therapy
Velpatasvir: Histamine H2 Receptor Antagonists may decrease the serum concentration of Velpatasvir. Monitor therapy
Adverse Reactions
All reported ADRs are for the oral formulations unless otherwise noted.
>10%: Central nervous system: Agitation (infants: ≤14%; adults: <1%)
1% to 10%:
Central nervous system: Headache (5%), dizziness (1%)
Gastrointestinal: Diarrhea (2%), constipation (1%), necrotizing enterocolitis (very low birth weight neonates; Guillet 2006)
Frequency not defined: Local: Irritation at injection site (IV)
<1%, postmarketing, and/or case reports: Abdominal distress, acne vulgaris, agranulocytosis, alopecia, anaphylaxis, angioedema, anorexia, anxiety, arthralgia, asthenia, atrioventricular block, bronchospasm, cardiac arrhythmia, cholestatic jaundice, confusion, conjunctival injection, decreased libido, depression, drowsiness, facial edema, fatigue, fever, flushing, hallucination, hepatitis, hypersensitivity reaction, impotence, increased liver enzymes, insomnia, interstitial pneumonitis, leukopenia, muscle cramps, musculoskeletal pain, nausea, palpitations, pancytopenia, paresthesia, periorbital edema, prolonged Q-T interval on ECG, pruritus, psychiatric disturbance, rhabdomyolysis, seizure, skin rash, Stevens-Johnson syndrome, taste disorder, thrombocytopenia, tinnitus, toxic epidermal necrolysis, urticaria, vomiting, xeroderma, xerostomia
Warnings/Precautions
Concerns related to adverse effects.
- ECG changes: Prolonged QT interval has been reported in patients with moderate to severe renal impairment. The FDA has received reports of torsades de pointes occurring with famotidine (Poluzzi 2009).
- Vitamin B12 deficiency: Prolonged treatment (≥2 years) may lead to vitamin B12 malabsorption and subsequent vitamin B12 deficiency. The magnitude of the deficiency is dose-related and the association is stronger in females and those younger in age (<30 years); prevalence is decreased after discontinuation of therapy (Lam 2013).
Disease-related concerns:
- Gastric malignancy: Relief of symptoms does not preclude the presence of a gastric malignancy.
- Renal impairment: Use with caution; increased risk of CNS adverse reactions and QT prolongation; dosage adjustment recommended in moderate and severe renal impairment (CrCl ≤60 mL/minute).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Use with caution; CNS adverse reactions (eg, confusion, delirium, hallucinations, disorientation, agitation, seizures, lethargy) have been reported in elderly patients.
- Pediatric: Use of gastric acid inhibitors, including proton pump inhibitors and H2 blockers, has been associated with an increased risk for development of acute gastroenteritis and community-acquired pneumonia in pediatric patients (Canani 2006).
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain benzyl alcohol and/or sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol and/or benzyl alcohol derivative with caution in neonates. See manufacturer’s labeling.
Other warnings/precautions:
- OTC labeling: When used for self-medication (OTC), notify health care provider before use if any of the following are present: Frequent chest pain; frequent wheezing particularly with heartburn; nausea/vomiting; unexplained weight loss; stomach pain; heartburn >3 months; heartburn with light-headedness, sweating, or dizziness; chest pain or shoulder pain with shortness of breath; sweating; pain that spreads to arms, neck, or shoulders; light-headedness. Discontinue use and notify health care provider if heartburn continues or worsens, or if use is required >14 days.
Monitoring Parameters
CBC, gastric pH, occult blood with GI bleeding
Pregnancy
Pregnancy Considerations
Famotidine crosses the placenta (Wang 2013).
Due to pregnancy-induced physiologic changes, renal clearance of famotidine may be increased (Wang 2011).
Histamine H2 antagonists have been evaluated for the treatment of gastroesophageal reflux disease (GERD) during pregnancy. Agents other than famotidine may be preferred for initial therapy (Richter 2005; van der Woude 2014). Histamine H2 antagonists may be used for aspiration prophylaxis prior to cesarean delivery (ASA 2016).
Patient Education
What is this drug used for?
- It is used to treat or prevent GI (gastrointestinal) ulcers.
- It is used to treat gastroesophageal reflux disease (GERD; acid reflux).
- It is used to treat heartburn and sour stomach.
- It is used to treat syndromes caused by lots of stomach acid.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Headache
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Dizziness
- Passing out
- Fast heartbeat
- Abnormal heartbeat
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.