Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Capsule, Oral:
Gilenya: 0.5 mg
Pharmacology
Mechanism of Action
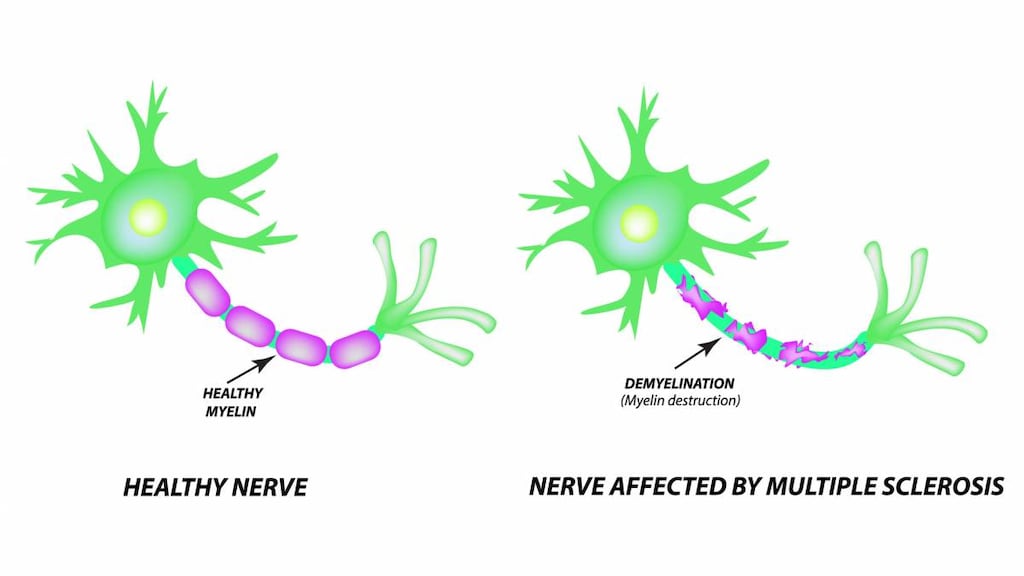
Fingolimod-phosphate, active metabolite of fingolimod, binds to sphingosine 1-phosphate receptors 1, 3, 4, and 5. Fingolimod-phosphate blocks the lymphocytes' ability to emerge from lymph nodes; therefore, the amount of lymphocytes available to the central nervous system is decreased, which reduces central inflammation.
Pharmacokinetics/Pharmacodynamics
Distribution
Vd: ~1,200 L: distributes into red blood cells (86%)
Metabolism
Hepatic via CYP4F2 to fingolimod-phosphate (active) and other metabolites (inactive); CYP2D6, 2E1, 3A4, and 4F12 also contribute to metabolism
Excretion
Urine (~81% as inactive metabolites); feces (fingolimod and fingolimod phosphate: <2.5% of dose)
Time to Peak
Plasma: 12 to 16 hours
Half-Life Elimination
6 to 9 days; prolonged by approximately 50% in patients with moderate or severe hepatic impairment
Protein Binding
>99.7% (fingolimod and fingolimod-phosphate)
Use in Specific Populations
Special Populations: Renal Function Impairment
Fingolimod Cmax and AUC are increased by 32% and 43%, respectively, and by 25% and 14%, respectively, for fingolimod-phosphate in patients with severe renal impairment.
Special Populations: Hepatic Function Impairment
Fingolimod area under the curve (AUC) increased by 12%, 44%, and 103% in patients with mild, moderate, or severe hepatic impairment, respectively. Fingolimod-phosphate maximal drug concentration (Cmax) was decreased by 22% in patients with severe hepatic impairment.
Use: Labeled Indications
Multiple sclerosis, relapsing: Treatment of relapsing forms of multiple sclerosis (MS), including clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease, in patients ≥10 years.
Contraindications
Hypersensitivity to fingolimod (including rash, urticaria, and angioedema) or any component of the formulation; myocardial infarction, unstable angina, stroke, transient ischemic attack, decompensated heart failure requiring hospitalization, or New York Heart Association class III/IV heart failure in the past 6 months; Mobitz Type II second- or third-degree atrioventricular block or sick sinus syndrome (unless patient has a functioning pacemaker); baseline QTc interval ≥500 msec; concurrent use of a class Ia or III antiarrhythmic.
Canadian labeling: Additional contraindications (not in US labeling): Patients at increased risk for opportunistic infections, including those who are immunocompromised due to treatment (eg, antineoplastic, immunosuppressive or immunomodulating therapies, total lymphoid irradiation, bone marrow transplantation) or disease (eg, immunodeficiency syndrome); severe active infections including active chronic bacterial, fungal, or viral infections (eg, hepatitis, tuberculosis); known active malignancy (excluding basal cell carcinoma); severe hepatic impairment (Child-Pugh class C); pregnancy and women in childbearing years not using effective contraception.
Dosage and Administration
Dosing: Adult
Multiple sclerosis, relapsing: Oral: 0.5 mg once daily; doses >0.5 mg daily are associated with increased adverse events and no additional benefit. Note: Administer the first dose and doses following therapy interruption (longer than 14 days) in a setting in which resources to appropriately manage symptomatic bradycardia are available.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Multiple sclerosis: Note: Doses >0.5 mg daily are associated with increased adverse events and no additional benefit. The first dose and doses following therapy interruption (see Monitoring Parameters) as well as dose increases should be administered in a setting in which resources to appropriately manage symptomatic bradycardia are available.
Children ≥10 years and Adolescents:
≤40 kg: Oral: 0.25 mg once daily
>40 kg: Oral: 0.5 mg once daily
Administration
Oral: Administer with or without food.
Storage
Store at 25°C (77°F); excursions are permitted between 15°C and 30°C (59°F and 86°F). Protect from moisture.
Drug Interactions
Amiodarone: Fingolimod may enhance the QTc-prolonging effect of Amiodarone. Avoid combination
Baricitinib: Immunosuppressants may enhance the immunosuppressive effect of Baricitinib. Management: Use of baricitinib in combination with potent immunosuppressants such as azathioprine or cyclosporine is not recommended. Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted. Consider therapy modification
BCG (Intravesical): Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Beta-Blockers: May enhance the bradycardic effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and beta-blockers if possible. If coadministration is necessary, patients should have overnight continuous ECG monitoring conducted after the first dose of fingolimod. Monitor patients for bradycardia. Consider therapy modification
Bradycardia-Causing Agents: May enhance the bradycardic effect of other Bradycardia-Causing Agents. Monitor therapy
CarBAMazepine: May decrease the serum concentration of Fingolimod. Monitor therapy
Ceritinib: Bradycardia-Causing Agents may enhance the bradycardic effect of Ceritinib. Management: If this combination cannot be avoided, monitor patients for evidence of symptomatic bradycardia, and closely monitor blood pressure and heart rate during therapy. Exceptions are discussed in separate monographs. Consider therapy modification
Cladribine: May enhance the immunosuppressive effect of Immunosuppressants. Avoid combination
Coccidioides immitis Skin Test: Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. Monitor therapy
Denosumab: May enhance the adverse/toxic effect of Immunosuppressants. Specifically, the risk for serious infections may be increased. Monitor therapy
DilTIAZem: May enhance the bradycardic effect of Fingolimod. Monitor therapy
Echinacea: May diminish the therapeutic effect of Immunosuppressants. Consider therapy modification
Esmolol: May enhance the bradycardic effect of Fingolimod. Avoid combination
Fexinidazole [INT]: Bradycardia-Causing Agents may enhance the arrhythmogenic effect of Fexinidazole [INT]. Avoid combination
Immunosuppressants: May enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). Consider therapy modification
Ivabradine: Bradycardia-Causing Agents may enhance the bradycardic effect of Ivabradine. Monitor therapy
Ketoconazole (Systemic): May increase serum concentrations of the active metabolite(s) of Fingolimod. Ketoconazole (Systemic) may increase the serum concentration of Fingolimod. Monitor therapy
Lacosamide: Bradycardia-Causing Agents may enhance the AV-blocking effect of Lacosamide. Monitor therapy
Leflunomide: Immunosuppressants may enhance the adverse/toxic effect of Leflunomide. Specifically, the risk for hematologic toxicity such as pancytopenia, agranulocytosis, and/or thrombocytopenia may be increased. Management: Consider not using a leflunomide loading dose in patients receiving other immunosuppressants. Patients receiving both leflunomide and another immunosuppressant should be monitored for bone marrow suppression at least monthly. Consider therapy modification
Midodrine: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Natalizumab: Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. Avoid combination
Nivolumab: Immunosuppressants may diminish the therapeutic effect of Nivolumab. Consider therapy modification
Pidotimod: Immunosuppressants may diminish the therapeutic effect of Pidotimod. Monitor therapy
Pimecrolimus: May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
QT-prolonging Agents (Highest Risk): Fingolimod may enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias (including TdP) with a continuous overnight ECG when fingolimod is combined with QT prolonging drugs. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Ajmaline; Amiodarone; Disopyramide; Dofetilide; Dronedarone; Ibutilide; Procainamide; QuiNIDine; Sotalol; Vernakalant. Monitor therapy
QT-prolonging Class IA Antiarrhythmics (Highest Risk): Fingolimod may enhance the QTc-prolonging effect of QT-prolonging Class IA Antiarrhythmics (Highest Risk). Avoid combination
QT-prolonging Class III Antiarrhythmics (Highest Risk): Fingolimod may enhance the QTc-prolonging effect of QT-prolonging Class III Antiarrhythmics (Highest Risk). Avoid combination
Roflumilast: May enhance the immunosuppressive effect of Immunosuppressants. Consider therapy modification
Siponimod: Bradycardia-Causing Agents may enhance the bradycardic effect of Siponimod. Management: Avoid coadministration of siponimod with drugs that may cause bradycardia. Consider therapy modification
Sipuleucel-T: Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. Consider therapy modification
Tacrolimus (Topical): May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Terlipressin: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Tertomotide: Immunosuppressants may diminish the therapeutic effect of Tertomotide. Monitor therapy
Tofacitinib: Immunosuppressants may enhance the immunosuppressive effect of Tofacitinib. Management: Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted, and this warning seems particularly focused on more potent immunosuppressants. Consider therapy modification
Trastuzumab: May enhance the neutropenic effect of Immunosuppressants. Monitor therapy
Upadacitinib: Immunosuppressants may enhance the immunosuppressive effect of Upadacitinib. Avoid combination
Vaccines (Inactivated): Fingolimod may diminish the therapeutic effect of Vaccines (Inactivated). Management: Vaccine efficacy may be reduced. Complete all age-appropriate vaccinations at least 2 weeks prior to starting fingolimod. If vaccinated during fingolimod therapy, revaccinate 2 to 3 months after fingolimod discontinuation. Consider therapy modification
Vaccines (Live): Fingolimod may enhance the adverse/toxic effect of Vaccines (Live). Vaccinal infections may develop. Fingolimod may diminish the therapeutic effect of Vaccines (Live). Avoid combination
Verapamil: May enhance the bradycardic effect of Fingolimod. Monitor therapy
Zoster Vaccine (Live/Attenuated): Fingolimod may enhance the adverse/toxic effect of Zoster Vaccine (Live/Attenuated). The risk of herpes zoster infection may be increased. Fingolimod may diminish the therapeutic effect of Zoster Vaccine (Live/Attenuated). Management: Wait 1 month after zoster vaccine administration to initiate fingolimod therapy. Avoid the use of the zoster vaccine during fingolimod treatment, and for 2 months following treatment discontinuation. Consider therapy modification
Adverse Reactions
As reported in adults, unless otherwise noted.
>10%:
Endocrine & metabolic: Increased gamma-glutamyl transfer (≤15%)
Gastrointestinal: Diarrhea (13%), nausea (13%), abdominal pain (11%)
Hepatic: Increased serum alanine aminotransferase (≤15%), increased serum aspartate transaminase (≤15%)
Infection: Influenza (11%)
Nervous system: Headache (25%)
Respiratory: Cough (12%), sinusitis (11%)
1% to 10%:
Cardiovascular: Hypertension (8%), first degree atrioventricular block (5%), second degree atrioventricular block (4%), bradycardia (3%)
Dermatologic: Alopecia (3%), actinic keratosis (2%), pityriasis versicolor (2%)
Endocrine & metabolic: Increased serum triglycerides (3%)
Hematologic & oncologic: Lymphocytopenia (7%), cutaneous papilloma (3%), leukopenia (2%), basal cell carcinoma of skin (2%)
Infection: Herpes virus infection (9%), herpes zoster infection (2%)
Nervous system: Seizure (children and adolescents: 6%), migraine (6%)
Neuromuscular & skeletal: Back pain (10%), limb pain (10%), asthenia (2%)
Ophthalmic: Blurred vision (4%)
Respiratory: Dyspnea (9%), bronchitis (8%), decreased lung function (3%; diffusion lung capacity for carbon monoxide), reduced forced expiratory volume (3%)
<1%, postmarketing, and/or case reports: Acute exacerbations of multiple sclerosis (tumefactive), angioedema, arthralgia, asystole, bacterial infection, cerebrovascular accident, complete atrioventricular block, cryptococcosis, fungal infection, hemolytic anemia, hepatic injury, herpes simplex encephalitis, human papilloma virus infection (including related cancer), hypersensitivity reaction, increased serum bilirubin, JC virus infection, Kaposi sarcoma, macular edema, malignant lymphoma (including B-cell), malignant melanoma, Merkel cell carcinoma, multiorgan failure, myalgia, neoplasm, non-Hodgkin lymphoma, peripheral arterial disease, pneumonia, progressive multifocal leukoencephalopathy, prolonged QT interval on ECG, reversible posterior leukoencephalopathy syndrome, skin rash, squamous cell carcinoma, status epilepticus, syncope, T-cell lymphoma (including cutaneous T-cell lymphoma and mycosis fungoides), thrombocytopenia, urticaria
Warnings/Precautions
Concerns related to adverse reactions:
- Atrioventricular (AV) block: May result in transient and asymptomatic AV conduction delays, which typically resolve within 24 hours of treatment initiation; recurrence may be observed following discontinuation and subsequent reinitiation of therapy. Third-degree AV block and AV block with junctional escape occurred within the first 6 hours of the initial dose, and transient asystole and unexplained death have occurred within the first 24 hours; syncope has also occurred.
- Bacterial infections: Serious opportunistic bacterial infections (eg, atypical mycobacteria) have been reported with use. Promptly evaluate and treat patients with symptoms and signs of an infection.
- Bradycardia: Initiation must occur in a setting with resources and personnel capable of appropriately managing symptomatic bradycardia. Following the first dose, heart rate may decrease as soon as 1 hour postdose, with the maximal decrease usually occurring ~6 hours postdose with recovery (but not to baseline levels) 8 to 10 hours postdose. A second heart rate decrease occurs within 24 hours after the first dose and may be more pronounced than the first 6-hour rate decrease. Most patients are asymptomatic; however, hypotension, dizziness, fatigue, palpitations, and/or chest pain may occur; symptoms usually resolve within 24 hours. With the second dose, heart rate may also decrease, but to a lesser magnitude than observed with the first dose. Heart rate typically returns to baseline after 1 month of chronic therapy.
- Cryptococcal infections: Cases of cryptococcal meningitis and disseminated cryptococcal infections (including fatalities) have been reported. Cryptococcal infections have generally occurred after ~2 years of treatment, although may occur earlier (relationship between risk and duration of treatment is unknown). Patients with signs and symptoms of cryptococcal infections should undergo prompt diagnostic evaluation and treatment.
- Herpes infection: Serious, life-threatening herpes infections, including fatalities (eg, disseminated primary herpes zoster and herpes simplex encephalitis) have occurred. Consider disseminated herpes infections as an etiology if an atypical MS relapse or multiorgan failure occurs. Cases of Kaposi sarcoma (associated with human herpes virus-8) have been reported; if suspected, prompt diagnostic evaluation and management is required.
- Hypersensitivity reaction: Hypersensitivity reactions, including rash, urticaria, and angioedema upon treatment initiation, have been reported.
- Hypertension: Increased blood pressure may occur ~1 month after initiation of therapy; monitor blood pressure throughout treatment.
- Liver injury: Liver injury has occurred (including acute liver failure requiring liver transplant); elevated serum liver enzymes and total bilirubin have been reported as early as 10 days after the first dose and with prolonged use (most elevations occurred within 6 to 9 months). Recurrence of liver transaminase elevations may occur with rechallenge. Obtain baseline liver enzymes and bilirubin in all patients prior to therapy initiation (within 6 months) and periodically during therapy and until 2 months after discontinuation of therapy. Monitor liver enzymes and bilirubin in patients who develop symptoms of hepatic injury (eg, right abdominal pain, fatigue, anorexia, jaundice, dark urine). Interrupt treatment if ALT and bilirubin are >3 times and >2 times the ULN, respectively; transaminases tend to return to normal within 2 months of discontinuation. Do not resume treatment if etiology of liver injury cannot be established.
- Lymphopenia: A dose-dependent decrease in lymphocyte counts may occur. Obtain a CBC, including lymphocyte count, prior to initiation of therapy, then every 3 months thereafter or as clinically indicated (AAN [Rae-Grant 2018]). Patients with lower lymphocyte counts at baseline or BMI <18.5 kg/m2, females, and those with previous exposure to natalizumab may be at increased risk (Baharnoori 2018; Warnke 2014). In patients who develop lymphopenia during fingolimod treatment, using an alternate dosing schedule (eg, every other day dosing ordosing 5 days out of 7 days) may raise circulating lymphocyte counts without increasing disease activity (Longbrake 2018). Interrupt therapy with fingolimod in patients who develop serious infections. Due to a potential for delayed lymphocyte recovery following treatment interruption or discontinuation, monitor lymphocyte counts for at least 2 months after stopping therapy. Do not initiate or restart fingolimod in patients with acute or chronic infections.
- Macular edema: Macular edema may occur, typically within the first 6 months of treatment. Patients may present with blurred vision, decreased visual acuity, or without symptoms. Signs and symptoms generally improve or resolve with discontinuation of treatment; however, residual decreased visual acuity has occurred in some patients. Patients with a history of diabetes mellitus or uveitis are at increased risk; use with caution. Ophthalmologic exams (including the fundus and macula) should be performed prior to therapy, 3 to 4 months after treatment initiation, and anytime visual disturbances are reported; more frequent examination is warranted in patients with diabetes or a history of uveitis.
- Malignancy: Cases of lymphoma (eg, non-Hodgkin, CNS, mycosis fungoides) and skin cancers have been reported. Basal cell carcinoma and melanoma risk is increased with fingolimod use; monitor for suspicious skin lesions periodically (especially in patients with risk factors for skin cancer) and promptly evaluate. Patients should minimize exposure to sunlight and ultraviolet light by wearing protective clothing and sunscreen with high protection factor.
- Neurotoxicity: Posterior reversible encephalopathy syndrome (PRES) has been observed. Monitor for signs/symptoms of PRES (eg, sudden onset of severe headache, altered mental status, visual disturbances, seizure); symptoms are usually reversible, but may evolve into ischemic stroke or cerebral hemorrhage. Delayed diagnosis and treatment may result in permanent neurological sequelae. Discontinue use if PRES is suspected.
- Progressive multifocal leukoencephalopathy: Cases of progressive multifocal leukoencephalopathy (PML) due to the John Cunningham (JC) virus have been reported. With the exception of prior immunosuppressant use (eg, natalizumab), risk factors for PML with fingolimod have not been identified (Berger 2018). Cases have been reported in patients who were not immunocompromised and had no prior exposure to immunosuppressant drugs. The majority of PML cases occurred in patients treated with fingolimod for at least 2 years (relationship between risk and duration of treatment is unknown). At the first sign or symptom suggestive of PML, perform a diagnostic evaluation and withhold therapy; symptoms progress over days to weeks and may include progressive weakness on one side of the body or clumsiness of limbs, vision disturbances, and mental status changes. Cases of PML have been diagnosed based on MRI findings and the detection of JC virus DNA in the CSF without specific PML signs/symptoms. Monitoring with brain MRI for signs that may be consistent with PML may be beneficial and allow for an early diagnosis of PML.
- Respiratory effects: Reductions of forced expiratory volume in the first second of expiration (FEV1) and diffusion lung capacity for carbon monoxide (DLCO) are dose dependent and may occur within the first month of therapy. FEV1 changes may be reversible with drug discontinuation. Use in multiple sclerosis (MS) patients with compromised respiratory function has not been evaluated. If clinically necessary, spirometric evaluation of respiratory function and evaluation of DLCO should be performed during therapy.
- QT prolongation: May cause QT prolongation; patients with a prolonged QT interval at baseline (adult and pediatric males: >450 msec; adult females: >470 msec; pediatric females: >460 msec) or during the first 6 hours of treatment initiation, or who are at an increased risk of QT prolongation (eg, hypokalemia, hypomagnesemia, concomitant QT-prolonging drugs [eg, citalopram, chlorpromazine, haloperidol, methadone, erythromycin], congenital long-QT syndrome) require continuous overnight electrocardiogram (ECG) monitoring in a medical facility after the initial dose.
- Varicella zoster infections: Serious, life-threatening events of disseminated varicella infections have occurred with fingolimod use. Varicella zoster virus vaccination is recommended prior to initiation of treatment in patients without a health care professional-confirmed history of chickenpox, without a documented full course of varicella zoster vaccination, and patients who are VZV antibody negative; postpone fingolimod treatment for 1 month after varicella zoster vaccination.
Disease-related concerns:
- Cardiovascular: Due to the risk of bradycardia and AV conduction delays, an ECG is required prior to initiation of therapy and after the initial observation period (6 hours) in all patients. Patients receiving concomitant therapy with drugs that slow heart rate or AV conduction (eg, beta-blockers, heart rate-lowering calcium channel blockers, digoxin) or with other cardiac risk factors (eg, AV block, sick sinus syndrome, prolonged QT interval, ischemic cardiac disease, history of myocardial infarction [MI], symptomatic bradycardia and/or cardiac arrest, heart failure, cerebrovascular disease, uncontrolled hypertension, recurrent syncope, severe sleep apnea [untreated]) require continuous overnight ECG monitoring in a medical facility after the first dose.
- Hepatic impairment: Use caution in patients with preexisting liver disease; may be at increased risk of increased liver enzymes.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings and precautions:
- Discontinuation of therapy: Cases of rebound syndrome (clinical and radiological signs of severe exacerbation beyond what was expected) have been reported; may occur within the first 24 weeks after stopping fingolimod treatment in patients with multiple sclerosis of varying severity and duration. In some cases, relapses have occurred despite the initiation of other disease-modifying therapies. Rebound symptoms have included back and extremity pain, confusion, constipation, diplopia, facial muscle spasms, fatigue, increased leg weakness, nausea paraparesis and paresthesias (Hatcher 2016; Willis 2017). Patients who experience rebound symptoms may not return to the functional status attained during treatment with fingolimod. Monitor for development of severe increase in disability, especially during the first 12 weeks following discontinuation and begin appropriate treatment as needed.
- Immunizations: Pediatric patients should complete all immunizations according to current immunization guidelines, if possible, prior to initiating fingolimod therapy.
Monitoring Parameters
CBC including lymphocyte counts (baseline, then every 3 months thereafter and as clinically necessary) (AAN [Rae-Grant 2018]).
Hepatic monitoring: Baseline bilirubin and transaminase levels in all patients prior to therapy initiation (within 6 months) and periodically thereafter (including for 2 months after therapy discontinued); monitor transaminases in patients who develop symptoms of hepatic dysfunction.
ECG (baseline; repeat after initial dose observation period); heart rate, blood pressure, and signs and symptoms of bradycardia (hourly for 6 hours following first dose; continued observation [until resolved] required if 6-hour postdose heart rate is <45 bpm in adults, <55 bpm in patients ≥12 years, and <60 bpm in patients 10 to 11 years, 6-hour postdose heart rate is lowest postbaseline measurement, or new-onset second-degree or higher AV block occurs on repeat ECG); continuous ECG monitoring (until symptoms resolved) if postdose symptomatic bradycardia occurs and no pharmacologic treatment is necessary (overnight continuous ECG in a medical facility and repeat observation period for second dose if pharmacologic intervention for bradycardia is necessary); overnight continuous ECG monitoring in a medical facility in patients with a prolonged QTc interval at baseline or 6-hours post dose (>450 msec: adult and pediatric males, >470 msec: adult females, or >460 msec: pediatric females) additional risks for QT prolongation (eg, hypokalemia, hypomagnesemia, congenital long-QT syndrome), concurrent therapy with QT prolonging agents with a known risk of torsades de pointes, or some preexisting heart and cerebrovascular conditions
Initial monitoring procedures (ECG, heart rate, blood pressure) must be repeated for
- treatment interruption of ≥1 day during the first 2 weeks after treatment initiation, or
- treatment interruption of >7 days during weeks 3 to 4 after treatment initiation, or
- treatment interruption of >14 days after ≥1 month of treatment initiation
Ophthalmologic exam at baseline and 3 to 4 months after initiation of treatment (continue periodic examinations for duration of therapy in patients with diabetes, history of uveitis, or visual complaints); respiratory function (FEV1, DLCO) if clinically indicated; VZV antibodies (prior to starting treatment; in patients with no health care professional-confirmed history of chickenpox or without documented previous full series VZV vaccination); signs and symptoms of infection (during treatment and at least 2 months after discontinuation), progressive multifocal leukoencephalopathy, and/or posterior reversible encephalopathy syndrome; monitor for suspicious skin lesions; severe increase in disability following discontinuation of therapy
Pregnancy
Pregnancy Considerations
Outcome information related to the use of fingolimod in pregnancy is limited (Geissbühler 2018; Karlsson 2014; Navardi 2018; Nguyen 2019).
In general, disease-modifying therapies for multiple sclerosis (MS) are stopped prior to a planned pregnancy, and not initiated during pregnancy, except in females at high risk of MS activity (AAN [Rae-Grant 2018]). Consider use of agents other than fingolimod in females at high risk of disease reactivation who are planning a pregnancy. Delaying pregnancy is recommended for females with persistent high disease activity; when disease-modifying therapy is needed in these patients, other agents are preferred (ECTRIMS/EAN [Montalban 2018]). Clinical rebound (new neurologic symptoms and increased lesions) has been reported when fingolimod treatment was discontinued during pregnancy (Meinl 2018; Novi 2017; Sempere 2013). Females who are considering stopping fingolimod because of pregnancy or when planning pregnancy should be counseled on the possibility of severe worsening of disability. Patients should seek immediate medical attention if they experience new or worsened symptoms of MS after fingolimod is stopped.
Evaluate pregnancy status prior to use in females of reproductive potential. Elimination of fingolimod takes ~2 months; to avoid potential fetal harm, females of childbearing potential should use effective contraception to avoid pregnancy during therapy and for 2 months after discontinuing treatment.
Data collection to monitor pregnancy and infant outcomes following exposure to fingolimod is ongoing. Health care providers are encouraged to enroll females exposed during pregnancy in the Gilenya Pregnancy Registry (1-877-598-7237 or https://www.gilenyapregnancyregistry.com). Pregnant females may also enroll themselves.
Patient Education
What is this drug used for?
- It is used to treat MS (multiple sclerosis).
Frequently reported side effects of this drug
- Flu-like symptoms
- Painful extremities
- Sinus pain
- Abdominal pain
- Diarrhea
- Back pain
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Meningitis like headache with fever, stiff neck, nausea, confusion, or sensitivity to light
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
- Severe headache
- Dizziness
- Slow heartbeat
- Abnormal heartbeat
- Fatigue
- Chest pain
- Mole changes
- Skin growth
- Excessive weight loss
- Night sweats
- Swollen glands
- Skin changes
- Passing out
- Shortness of breath
- Trouble breathing
- Vision changes
- Eye pain
- Severe eye irritation
- Posterior reversible encephalopathy syndrome like confusion, not alert, vision changes, seizures, or severe headache
- Progressive multifocal leukoencephalopathy like confusion, depression, trouble with memory, behavioral changes, change in strength on one side is greater than the other, trouble speaking, change in balance, or vision changes
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.