Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Injection, powder for reconstitution [preservative free]:
Avonex: 30 mcg [contains albumin (human), mouse (murine) and/or hamster protein; supplied with diluent] [DSC]
Injection, solution:
Avonex: 30 mcg/0.5 mL (0.5 mL) [albumin free; contains mouse (murine) and/or hamster protein; prefilled syringe]
Avonex Pen: 30 mcg/0.5 mL (0.5 mL) [albumin free; contains mouse (murine) and/or hamster protein]
Injection, solution [preservative free]:
Rebif: 22 mcg/0.5 mL (0.5 mL), 44 mcg/0.5 mL (0.5 mL) [contains albumin (human), mouse (murine) and/or hamster protein; prefilled syringe]
Rebif Rebidose: 22 mcg/0.5 mL (0.5 mL), 44 mcg/0.5 mL (0.5 mL) [contains albumin (human), mouse (murine) and/or hamster protein; autoinjector]
Injection, solution [preservative free, combination package]:
Rebif Titration Pack: 8.8 mcg/0.2 mL (6s) and 22 mcg/0.5 mL (6s) [contains albumin (human), mouse (murine) and/or hamster protein; prefilled syringe]
Rebif Rebidose Titration Pack: 8.8 mcg/0.2 mL (6s) and 22 mcg/0.5 mL (6s) [contains albumin (human), mouse (murine) and/or hamster protein; autoinjector]
Pharmacology
Mechanism of Action
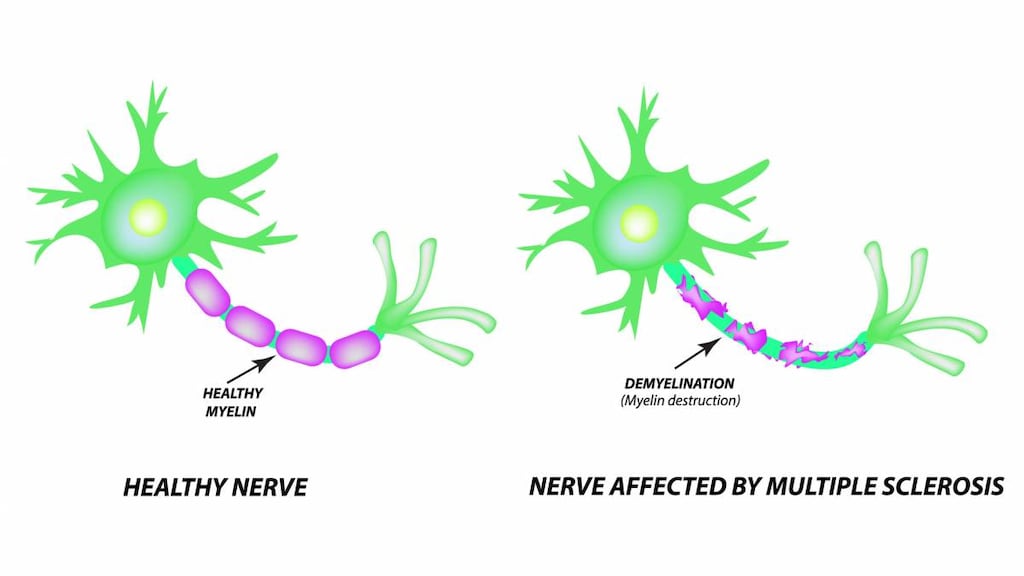
Interferon beta differs from naturally occurring human protein by a single amino acid substitution and the lack of carbohydrate side chains; alters the expression and response to surface antigens and can enhance immune cell activities. Properties of interferon beta that modify biologic responses are mediated by cell surface receptor interactions; mechanism in the treatment of MS is unknown.
Pharmacokinetics/Pharmacodynamics
Onset of Action
Avonex: 12 hours (based on biological response markers)
Time to Peak
Serum: Avonex (IM): ~15 hours (range: 6-36 hours); Rebif (SubQ): 16 hours
Duration of Action
Avonex: 4 days (based on biological response markers)
Half-Life Elimination
Avonex: ~19 hours (range: 8-54 hours); Rebif: 69 hours
Use: Labeled Indications
US labeling:
Multiple sclerosis, relapsing: Treatment of relapsing forms of multiple sclerosis (MS), including clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease
Canadian labeling:
Treatment of relapsing forms of MS to decrease the frequency of clinical exacerbations, delay the accumulation of physical disability, reduce the requirement for steroids, reduce the number of hospitalizations, and reduce disease burden
To decrease the number and volume of active brain lesions, decrease overall disease burden, and delay onset of clinically definite MS in patients who have experienced a single demyelinating event
Contraindications
Hypersensitivity to natural or recombinant interferon beta, human albumin (albumin-containing formulations only), or any other component of the formulation
Documentation of allergenic cross-reactivity for interferons is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Canadian labeling: Additional contraindications (not in US labeling): Rebif: Pregnancy; decompensated liver disease
Dosage and Administration
Dosing: Adult
Multiple sclerosis, relapsing: Note: Analgesics and/or antipyretics may help decrease flu-like symptoms on treatment days:
IM (Avonex):
US labeling: 30 mcg once weekly; to decrease flu-like symptoms, may initiate once-weekly dosing with 7.5 mcg (week 1) then increase dose in increments of 7.5 mcg once weekly (weeks 2 to 4) up to recommended dose (30 mcg once weekly).
Canadian labeling: 30 mcg once weekly; to decrease flu-like symptoms, may initiate once-weekly dosing with 7.5 mcg (week 1) then increase dose in increments of 7.5 mcg once weekly (weeks 2 to 4) or once every 2 weeks (to week 7) up to recommended dose (30 mcg once weekly). In progressive relapsing MS or secondary progressive MS with recurrent neurologic dysfunction may consider increasing to 60 mcg once weekly.
SubQ (Rebif): Target dose is either 22 or 44 mcg 3 times weekly; doses should be separated by at least 48 hours:
Target dose 44 mcg 3 times weekly:
Initial: 8.8 mcg (20% of target dose) 3 times weekly for 2 weeks.
Titration: 22 mcg (50% of target dose) 3 times weekly for 2 weeks.
Target dose: 44 mcg 3 times weekly.
Target dose 22 mcg 3 times weekly:
Initial: 4.4 mcg (20% of target dose) 3 times weekly for 2 weeks.
Titration: 11 mcg (50% of target dose) 3 times weekly for 2 weeks.
Target dose: 22 mcg 3 times weekly.
Single demyelinating event (Canadian labeling [Rebif]; not in US labeling): SubQ:
Target dose 44 mcg 3 times weekly: Note: Analgesics and/or antipyretics prior to and for 24 hours after dosing may help decrease flu-like symptoms:
Initial: 8.8 mcg (20% of target dose) 3 times weekly for 2 weeks.
Titration: 22 mcg (50% of target dose) 3 times weekly for 2 weeks.
Target dose: 44 mcg 3 times weekly.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Adjustment for Toxicity
Autoimmune disorder development: Consider discontinuing treatment.
Depression or other severe psychiatric symptoms: Consider discontinuing treatment.
Hepatotoxicity:
ALT >5 x ULN: Temporarily discontinue therapy or consider dose reduction until ALT normalizes, then may consider retitration of dose.
Symptomatic (eg, jaundice): Discontinue immediately.
Leukopenia: May require temporary discontinuation or dose reduction until resolution.
Reconstitution
Avonex: Reconstitute with 1.1 mL of diluent (SWFI) and swirl gently to dissolve. Do not shake. The reconstituted product contains no preservative and is for single-use only; discard unused portion.
Administration
The first injection should be administered under the supervision of a health care professional.
Avonex: Administer IM; rotate injection site; do not inject into area where skin is irritated, red, bruised, scarred, or infected. Two hours after injection, examine site for redness, swelling, or tenderness. Discard any unused portion.
Rebif: Administer SubQ at the same time of day on the same 3 days each week (eg, Mon, Wed, Fri), preferably in the late afternoon or evening; doses should be at least 48 hours apart; rotate injection site; do not inject into area where skin is irritated, red, bruised, or scarred. Discard any unused portion.
Storage
Avonex:
Prefilled syringe or pen: Store at 2°C to 8°C (36°F to 46°F); do not freeze. Protect from light. Allow to warm to room temperature prior to use (do not use external heat source). If refrigeration is not available, product may be stored at ≤25°C (77°F) for up to 7 days.
Vial: Store unreconstituted vial at 2°C to 8°C (36°F to 46°F). If refrigeration is not available, may be stored at 25°C (77°F) for up to 30 days; do not freeze. Protect from light. Following reconstitution, use immediately, but may be stored up to 6 hours at 2°C to 8°C (36°F to 46°F); do not freeze.
Rebif: Store at 2°C to 8°C (36°F to 46°F); do not freeze. Protect from heat and light. Allow to warm to room temperature prior to use (do not use external heat source). Refrigeration is preferred; however, if needed, may be stored at 2°C to 25°C (36°F to 77°F) for up to 30 days.
Drug Interactions
Cladribine: May enhance the adverse/toxic effect of Interferons (Beta). Specifically, the risk for lymphopenia may be increased. Avoid combination
Zidovudine: Interferons may enhance the adverse/toxic effect of Zidovudine. Interferons may decrease the metabolism of Zidovudine. Monitor therapy
Adverse Reactions
Adverse reactions reported as a composite of both commercially-available products. Spectrum and incidence of reactions is generally similar between products, but consult individual product labels for specific incidence.
>10%:
Central nervous system: Headache (58% to 70%), fatigue (33% to 41%), depression (18% to 25%), pain (23%), chills (19%), dizziness (14%)
Gastrointestinal: Nausea (23%), abdominal pain (8% to 22%)
Genitourinary: Urinary tract infection (17%)
Hematologic & oncologic: Leukopenia (28% to 36%), lymphadenopathy (11% to 12%)
Hepatic: Increased serum ALT (20% to 27%), increased serum AST (10% to 17%)
Immunologic: Antibody development (neutralizing; significance not known; Rebif: 24% to 31%; Avonex: 5%)
Local: Injection site reaction (3% to 92%)
Neuromuscular & skeletal: Myalgia (25% to 29%), back pain (23% to 25%), weakness (24%), skeletal pain (10% to 15%), rigors (6% to 13%)
Ophthalmic: Visual disturbance (7% to 13%)
Respiratory: Flu-like symptoms (49% to 59%), sinusitis (14%), upper respiratory tract infection (14%)
Miscellaneous: Fever (20% to 28%)
1% to 10%:
Cardiovascular: Chest pain (5% to 8%), vasodilation (2%)
Central nervous system: Hypertonia (6% to 7%), migraine (5%), ataxia (4% to 5%), drowsiness (4% to 5%), malaise (4% to 5%), seizure (1% to 5%), suicidal tendencies (4%)
Dermatologic: Erythematous rash (5% to 7%), maculopapular rash (4% to 5%), alopecia (4%), hyperhidrosis (4%), urticaria
Endocrine & metabolic: Thyroid disease (4% to 6%)
Gastrointestinal: Xerostomia (1% to 5%), toothache (3%)
Genitourinary: Urinary frequency (2% to 7%), urinary incontinence (2% to 4%), urine abnormality (3%)
Hematologic & oncologic: Thrombocytopenia (2% to 8%), anemia (3% to 5%)
Hepatic: Hyperbilirubinemia (2% to 3%)
Infection: Infection (7%)
Local: Pain at injection site (8%), bruising at injection site (6%), inflammation at injection site (6%), tissue necrosis at injection site (1% to 3%)
Neuromuscular & skeletal: Arthralgia (9%)
Ophthalmic: Eye disease (4%), xerophthalmia (1% to 3%)
Respiratory: Bronchitis (8%)
<1%, postmarketing, and/or case reports: Abnormal gait, abnormal healing, abnormal hepatic function tests, abscess, abscess at injection site, amnesia, anaphylaxis, angioedema, anxiety, arteritis, arthritis, ascites, autoimmune hepatitis, basal cell carcinoma, Bell's palsy, bloody stools, breast fibroadenosis, cardiac arrhythmia, cardiac failure, cardiomyopathy, cellulitis, cellulitis at injection site, clumsiness, cold and clammy skin, colitis, confusion, conjunctivitis, constipation, contact dermatitis, dehydration, depersonalization, dermal ulcer, diaphoresis, diverticulitis, drug dependence, dyspnea, dysuria, ecchymoses, emotional lability, emphysema, epididymitis, erythema, erythema multiforme, eye pain, facial edema, facial paralysis, fibrocystic breast changes, fibrosis at injection site, furunculosis, gallbladder disease, gastritis, gastrointestinal hemorrhage, genital pruritus, gingival hemorrhage, gingivitis, gynecomastia, hematuria, hemolytic-uremic syndrome, hemoptysis, hemorrhage, hepatic failure, hepatic injury, hepatic neoplasm, hepatitis, hepatomegaly, hepatotoxicity (idiosyncratic) (Chalasani 2014), hernia, hiccups, hyperesthesia, hypermenorrhea, hypersensitivity reaction at injection site, hyperthyroidism, hyperventilation, hypoglycemia, hypokalemia, hypomagnesemia, hypotension, hypothyroidism, immune thrombocytopenia, increased appetite, increased coagulation time, increased libido, increased thirst, intestinal obstruction, intestinal perforation, labyrinthitis, laryngitis, leukorrhea, lipoma, lump in breast, lupus erythematosus, menopause, myasthenia, neoplasm, nephrolithiasis, neurological signs and symptoms (transient; may mimic multiple sclerosis exacerbations), nevus, nocturia, orolingual edema, orthostatic hypotension, osteonecrosis, otalgia, palpitations, pancytopenia, paresthesia, pelvic inflammatory disease, penile disease, pericarditis, periodontal abscess, periodontitis, peripheral ischemia, peripheral vascular disease, petechia, Peyronie disease, pharyngeal edema, pneumonia, polyuria, postmenopausal bleeding, proctitis, prostatic disease, pruritus, psychiatric disturbance (new or worsening; including suicidal ideation), psychoneurosis, pulmonary embolism, pulmonary hypertension (Govern 2015; Health Canada Nov. 2, 2016), pyelonephritis, renal pain, retinal vascular disease, seborrhea, sepsis, severe weakness (transient), skin blister, skin discoloration, skin photosensitivity, skin rash, spider telangiectasia, Stevens-Johnson syndrome, synovitis, tachycardia, telangiectasia, testicular disease, thromboembolism, thrombotic thrombocytopenic purpura, tongue disease, urethral pain, urinary retention, urinary urgency, uterine fibroids, uterine hemorrhage, vaginal hemorrhage, vascular disease, vesicular eruption, vitreous opacity, vomiting
Warnings/Precautions
Concerns related to adverse effects:
- Anaphylaxis/hypersensitivity reactions: Allergic reactions, including anaphylaxis, have been reported. Some reactions may occur after prolonged use. Discontinue therapy if anaphylaxis or other allergic reactions occur.
- Autoimmune disorders: Autoimmune disorders including idiopathic thrombocytopenia, hyper- and hypothyroidism and rarely autoimmune hepatitis have been reported. Consider discontinuation of treatment if patient develops a new autoimmune disorder.
- Bone marrow suppression: Pancytopenia (rare), leukopenia, and thrombocytopenia have been reported. Monitor blood counts at 1, 3, and 6 months post therapy initiation and periodically thereafter. Events may recur with rechallenge.
- Flu-like symptoms: Associated with a high incidence of flu-like adverse effects; use of analgesics and/or antipyretics on treatment days may be helpful.
- Hepatic effects: Rare cases of severe hepatic injury, including cases of hepatic failure requiring transplantation, have been reported in patients receiving interferon beta-1a; risk may be increased by ethanol use or concurrent therapy with hepatotoxic drugs. Some reports indicate symptoms began after 1 to 6 months of treatment. Transaminase elevations may be asymptomatic. Use with caution in patients with active or a history of liver disease, alcohol abuse, or increased serum ALT (>2.5 times ULN) at baseline. Obtain liver function tests at 1, 3, and 6 months post therapy initiation and periodically thereafter. Treatment should be suspended immediately if jaundice or symptoms of hepatic dysfunction occur. Consider dose reductions or temporary discontinuation if ALT >5 times ULN.
- Injection site reactions: Severe injection site reactions have occurred, including pain, erythema, edema, cellulitis, abscess, and necrosis. Necrosis may occur at single and multiple sites. Some reactions have occurred ≥2 years after initiation; reactions typically resolve with conservative treatment (antibiotics or surgical intervention may be required). Patient and/or caregiver competency in injection technique should be confirmed and periodically re-evaluated.
- Neuropsychiatric disorders: Interferons have been associated with psychiatric adverse events (psychosis, depression, suicidal behavior/ideation) in patients with and without previous psychiatric symptoms; use with caution in patients with depression. Patients exhibiting symptoms of depression or other severe psychiatric symptoms should be closely monitored and discontinuation of therapy should be considered.
- Thrombotic microangiopathy: Cases of thrombotic microangiopathy manifesting as thrombotic thrombocytopenic purpura (TTP) or hemolytic uremic syndrome (HUS) (some fatal) have been reported (Hunt 2014; Mahe 2013; Rebif Canadian product labeling 2016). Some cases may occur after several years of therapy. Monitor for new onset hypertension, thrombocytopenia, or impaired renal function; discontinuation of therapy and prompt treatment may be necessary if TTP/HUS are confirmed.
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with preexisting cardiovascular disease. Rare cases of new-onset cardiomyopathy and/or HF have been reported. In a scientific statement from the American Heart Association, interferon has been determined to be an agent that may either cause reversible direct myocardial toxicity or exacerbate underlying myocardial dysfunction (magnitude: moderate/major) (AHA [Page 2016]).
- Hepatic impairment: Use with caution in patients with hepatic impairment or in those who abuse alcohol.
- Seizure disorder: Use with caution in patients with a history of seizure disorder.
- Thyroid dysfunction: Thyroid abnormalities may develop with use; may worsen pre-existing thyroid conditions. Monitor thyroid function tests every 6 months or as clinically necessary.
Special populations:
- Chronic progressive MS: Safety and efficacy have not been established for this use.
Dosage form specific issues:
- Albumin: Some formulations contain albumin, which may carry a remote risk of transmitting Creutzfeldt-Jakob or other viral diseases. Interferon beta-1a formulations that contain albumin are contraindicated in albumin-sensitive patients.
- Latex: The packaging (prefilled syringe tip cap) may contain latex.
Monitoring Parameters
Thyroid function tests, CBC with differential, transaminase levels, blood chemistries, symptoms of autoimmune disorders, signs/symptoms of psychiatric disorder (including depression and/or suicidal ideation), signs/symptoms of new onset/worsening cardiovascular disease, signs/symptoms of thrombotic microangiopathy (new-onset hypertension, thrombocytopenia, renal impairment)
Avonex: Frequency of monitoring for patients receiving Avonex has not been specifically defined; in clinical trials, monitoring was at 6-month intervals.
Rebif: CBC and liver function testing at 1-, 3-, and 6 months, then periodically thereafter. Thyroid function every 6 months (in patients with pre-existing abnormalities and/or clinical indications).
Pregnancy
Pregnancy Considerations
Preliminary data from the Avonex pregnancy registry (published in abstract), as well as worldwide postmarketing data collected by the manufacturer of Rebif, do not show an increased risk of adverse fetal events when exposure occurs during pregnancy (Foulds 2010; Richman 2012; Sandberg-Wollheim 2011; Tomczyk 2013).
In general, disease-modifying therapies for multiple sclerosis (MS) are stopped prior to a planned pregnancy, and not initiated during pregnancy, except in females at high risk of MS activity (AAN [Rae-Grant 2018]). When disease-modifying therapy is needed in females planning a pregnancy (eg, high risk of disease reactivation), interferon beta-1a may be considered until pregnancy is confirmed, and in select cases (eg, female with active disease), use may be continued during pregnancy. Delaying pregnancy is recommended for females with persistent high disease activity (ECTRIMS/EAN [Montalban 2018]).
Patient Education
What is this drug used for?
- It is used to treat MS (multiple sclerosis).
Frequently reported side effects of this drug
- Flu-like symptoms
- Nausea
- Abdominal pain
- Muscle pain
- Joint pain
- Back pain
- Fatigue
- Dry mouth
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Thrombotic thrombocytopenic purpura/hemolytic uremic syndrome like bruising or bleeding; loss of strength and energy; dark urine or yellow skin; pale skin; change in amount of urine passed; vision changes; change in strength on one side is greater than the other, difficulty speaking or thinking, change in balance; or fever
- Heart problems like cough or shortness of breath that is new or worse, swelling of the ankles or legs, abnormal heartbeat, weight gain of more than five pounds in 24 hours, dizziness, or passing out
- Depression like thoughts of suicide, anxiety, emotional instability, agitation, irritability, panic attacks, mood changes, behavioral changes, or confusion
- Urinary tract infection like blood in your urine, burning or painful urination, passing a lot of urine, fever, lower abdominal pain, or pelvic pain
- Thyroid problems like change in weight without trying, anxiety, feeling restless, feeling very weak, hair thinning, depression, neck swelling, difficulty focusing, inability handling heat or cold, menstrual changes, tremors, or sweating
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
- Injection site discoloration, skin breakdown, swelling, or fluid drainage
- Chest pain
- Vision changes
- Swollen gland
- Seizures
- Severe dizziness
- Passing out
- Loss of strength or energy
- Bruising
- Bleeding
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.