Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Capsule, Oral:
Generic: 2.5 mg, 5 mg
Pharmacology
Mechanism of Action
Inhibits calcium ion from entering the “slow channels” or select voltage-sensitive areas of vascular smooth muscle and myocardium during depolarization, producing relaxation of vascular smooth muscle, resulting in coronary vasodilation and reduced blood pressure; increases myocardial oxygen delivery in patients with vasospastic angina
Pharmacokinetics/Pharmacodynamics
Absorption
90% to 95%, but large first-pass effect
Distribution
Vd: 3 L/kg
Metabolism
Extensive first-pass effect; hepatically metabolized via cytochrome P450 isoenzyme CYP3A4; major metabolic pathways include oxidation and ester cleavage; six inactive metabolites have been identified
Excretion
Urine (60% to 65% as metabolites); feces (25% to 30%)
Onset of Action
2 to 3 hours; Note: Full hypotensive effect may not occur for 2 to 4 weeks
Time to Peak
Serum: 1 to 1.5 hours
Duration of Action
>12 hours
Half-Life Elimination
Alpha half-life: 1.5 to 2 hours; Terminal half-life: 8 hours
Protein Binding
95%
Use in Specific Populations
Special Populations: Hepatic Function Impairment
The Cmax increases by 32%
Special Populations: Elderly
The AUC and Cmax increases.
Use: Labeled Indications
Hypertension: Management of hypertension.
Guideline recommendations: The 2017 Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults recommends if monotherapy is warranted, in the absence of comorbidities (eg, cerebrovascular disease, chronic kidney disease, diabetes, heart failure, ischemic heart disease), that thiazide-like diuretics or dihydropyridine calcium channel blockers may be preferred options due to improved cardiovascular end points (eg, prevention of heart failure and stroke). ACE inhibitors and ARBs are also acceptable for monotherapy. Combination therapy may be required to achieve blood pressure goals and is initially preferred in patients at high risk (stage 2 hypertension or atherosclerotic cardiovascular disease [ASCVD] risk ≥10%) (ACC/AHA [Whelton 2017]).
Contraindications
Hypersensitivity to isradipine or any component of the formulation
Dosage and Administration
Dosing: Adult
Hypertension: Oral: Initial: 2.5 mg twice daily; titrate at 2- to 4-week intervals as needed based on patient response in 5 mg increments; usual dose range: 5 to 10 mg/day in 2 divided doses (ACC/AHA [Whelton 2017]). Note: Most patients show no improvement with doses >10 mg daily except adverse reaction rate increases; therefore, maximal dose in older adults should be 10 mg daily.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Hypertension: Limited data available: Children and Adolescents: Oral: Immediate release: Initial: 0.05 to 0.1 mg/kg/dose 2 to 3 times daily; titrate upwards at 2- to 4-week intervals; maximum daily dose: 0.6 mg/kg/day or 10 mg/day (whichever is lower) (AAP [Flynn 2017]). Based on retrospective observations, initial doses of 0.05 to 0.15 mg/kg/dose administered 3 to 4 times daily have been suggested in patients with secondary hypertension and acute severe hypertension; usual daily dose: 0.3 to 0.4 mg/kg/day in divided doses (eg, every 8 hours); reported range: 0.04 to 1.2 mg/kg/day (Flynn 2002; Flynn 2009; Johnson 1997; Miyashita 2010; Strauser 2000). Note: Most adult patients show no improvement with doses >10 mg daily and adverse reaction rate increases.
Extemporaneously Prepared
A 1 mg/mL oral suspension may be made from isradipine capsules; glycerin, USP; and Simple Syrup, N.F. Empty the contents of ten 5 mg isradipine capsules into a glass mortar. Add a small portion of glycerin, USP and mix to a fine paste; mix while adding 15 mL of simple syrup and transfer contents to a 60 mL amber glass prescription bottle. Rinse mortar with 10 mL simple syrup, NF and transfer to the prescription bottle; repeat, and add quantity of vehicle sufficient to make 50 mL. Label "protect from light", "refrigerate", and "shake well". Stable for 35 days when stored in amber glass prescription bottles in the dark and refrigerated.
MacDonald JL, Johnson CE, and Jacobson P, “Stability of Isradipine in Extemporaneously Compounded Oral Liquids,” Am J Hosp Pharm, 1994, 51(19):2409-11.7847406
Administration
Oral: May be administered without regard to meals.
Storage
Store at 20°C to 25°C (68°F to 77°F) in a tight container, protected from moisture, humidity, and light.
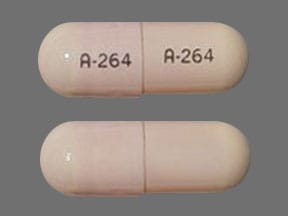
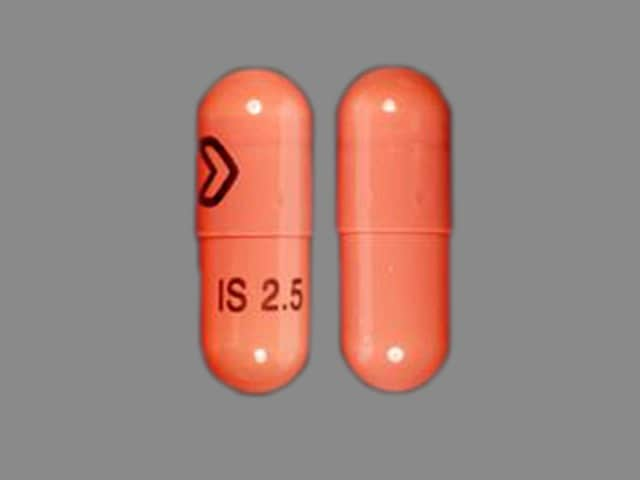
Isradipine Images
Drug Interactions
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Alpha1-Blockers: May enhance the hypotensive effect of Calcium Channel Blockers. Monitor therapy
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Amphetamines: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Antifungal Agents (Azole Derivatives, Systemic): May enhance the adverse/toxic effect of Calcium Channel Blockers. Specifically, itraconazole may enhance the negative inotropic effects of verapamil or diltiazem. Antifungal Agents (Azole Derivatives, Systemic) may decrease the metabolism of Calcium Channel Blockers. Fluconazole and isavuconazonium likely exert weaker effects than other azoles and are addressed in separate monographs. Management: Concurrent use of felodipine or nisoldipine with itraconazole is specifically contraindicated. Frequent monitoring is warranted with any such combination; calcium channel blocker dose reductions may be required. Exceptions: Fluconazole; Isavuconazonium Sulfate. Consider therapy modification
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Atosiban: Calcium Channel Blockers may enhance the adverse/toxic effect of Atosiban. Specifically, there may be an increased risk for pulmonary edema and/or dyspnea. Monitor therapy
Barbiturates: May increase the metabolism of Calcium Channel Blockers. Management: Monitor for decreased therapeutic effects of calcium channel blockers with concomitant barbiturate therapy. Calcium channel blocker dose adjustments may be necessary. Nimodipine Canadian labeling contraindicates concomitant use with phenobarbital. Monitor therapy
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Brigatinib: May diminish the antihypertensive effect of Antihypertensive Agents. Brigatinib may enhance the bradycardic effect of Antihypertensive Agents. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Calcium Channel Blockers (Nondihydropyridine): Calcium Channel Blockers (Dihydropyridine) may enhance the hypotensive effect of Calcium Channel Blockers (Nondihydropyridine). Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of Calcium Channel Blockers (Dihydropyridine). Monitor therapy
Calcium Salts: May diminish the therapeutic effect of Calcium Channel Blockers. Monitor therapy
CarBAMazepine: May increase the metabolism of Calcium Channel Blockers (Dihydropyridine). Management: Consider calcium channel blocker (CCB) dose adjustments or alternative therapy in patients receiving concomitant carbamazepine. Nimodipine Canadian labeling contraindicates concurrent use with carbamazepine. Consider therapy modification
Cimetidine: May increase the serum concentration of Calcium Channel Blockers. Management: Consider alternatives to cimetidine. If no suitable alternative exists, monitor for increased effects of calcium channel blockers following cimetidine initiation/dose increase, and decreased effects following cimetidine discontinuation/dose decrease. Consider therapy modification
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Clopidogrel: Calcium Channel Blockers may diminish the therapeutic effect of Clopidogrel. Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CycloSPORINE (Systemic): Calcium Channel Blockers (Dihydropyridine) may increase the serum concentration of CycloSPORINE (Systemic). CycloSPORINE (Systemic) may increase the serum concentration of Calcium Channel Blockers (Dihydropyridine). Monitor therapy
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dapoxetine: May enhance the orthostatic hypotensive effect of Calcium Channel Blockers. Monitor therapy
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Dexmethylphenidate: May diminish the therapeutic effect of Antihypertensive Agents. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Efavirenz: May decrease the serum concentration of Calcium Channel Blockers. Monitor therapy
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fluconazole: May increase the serum concentration of Calcium Channel Blockers. Monitor therapy
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosphenytoin: Calcium Channel Blockers may increase the serum concentration of Fosphenytoin. Management: Monitor for phenytoin toxicity with concomitant use of a calcium channel blocker (CCB) or decreased phenytoin effects with CCB discontinuation. Monitor for decreased CCB therapeutic effects. Nimodipine Canadian labeling contraindicates use with phenytoin. Consider therapy modification
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Herbs (Hypertensive Properties): May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Macrolide Antibiotics: May decrease the metabolism of Calcium Channel Blockers. Management: Consider using a noninteracting macrolide. Felodipine Canadian labeling specifically recommends avoiding its use in combination with clarithromycin. Exceptions: Azithromycin (Systemic); Fidaxomicin; Roxithromycin; Spiramycin. Consider therapy modification
Magnesium Salts: Calcium Channel Blockers may enhance the adverse/toxic effect of Magnesium Salts. Magnesium Salts may enhance the hypotensive effect of Calcium Channel Blockers. Monitor therapy
Melatonin: May diminish the antihypertensive effect of Calcium Channel Blockers (Dihydropyridine). Monitor therapy
Methylphenidate: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Neuromuscular-Blocking Agents (Nondepolarizing): Calcium Channel Blockers may enhance the neuromuscular-blocking effect of Neuromuscular-Blocking Agents (Nondepolarizing). Monitor therapy
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Phenytoin: Calcium Channel Blockers may increase the serum concentration of Phenytoin. Phenytoin may decrease the serum concentration of Calcium Channel Blockers. Management: Avoid use of nimodipine or nifedipine with phenytoin. Monitor for phenytoin toxicity and/or decreased calcium channel blocker effects with any concurrent use. Consider therapy modification
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
QuiNIDine: Calcium Channel Blockers (Dihydropyridine) may decrease the serum concentration of QuiNIDine. Calcium Channel Blockers (Dihydropyridine) may increase the serum concentration of QuiNIDine. QuiNIDine may increase the serum concentration of Calcium Channel Blockers (Dihydropyridine). Monitor therapy
Rifamycin Derivatives: May decrease the serum concentration of Calcium Channel Blockers. This primarily affects oral forms of calcium channel blockers. Management: The labeling for some US and Canadian calcium channel blockers contraindicate use with rifampin, however recommendations vary. Consult appropriate labeling. Consider therapy modification
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Sincalide: Drugs that Affect Gallbladder Function may diminish the therapeutic effect of Sincalide. Management: Consider discontinuing drugs that may affect gallbladder motility prior to the use of sincalide to stimulate gallbladder contraction. Consider therapy modification
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Tacrolimus (Systemic): Calcium Channel Blockers (Dihydropyridine) may increase the serum concentration of Tacrolimus (Systemic). Monitor therapy
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Yohimbine: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Test Interactions
May lead to false-negative aldosterone/renin ratio (ARR) (Funder 2016)
Adverse Reactions
>10%: Central nervous system: Headache (dose related 2% to 22%)
1% to 10%:
Cardiovascular: Edema (dose related 1% to 9%), flushing (dose related 1% to 5%), palpitations (dose related 1% to 5%), chest pain (3%), tachycardia (1% to 3%)
Central nervous system: Fatigue (dose related ≤9%), dizziness (2% to 8%)
Dermatologic: Skin rash (2%)
Gastrointestinal: Nausea (3% to 5%), abdominal distress (≤3%), diarrhea (≤3%), vomiting (≤1%)
Neuromuscular & skeletal: Weakness (≤1%)
Renal: Urinary frequency (1% to 3%)
Respiratory: Dyspnea (3%)
<1%, postmarketing, and/or case reports: Atrial fibrillation, cardiac failure, cerebrovascular accident, constipation, cough, decreased libido, depression, drowsiness, foot cramps, hyperhidrosis, hypotension, impotence, increased liver enzymes, insomnia, leg cramps, lethargy, leukopenia, myocardial infarction, nervousness, nocturia, numbness, paresthesia, pruritus, sore throat, syncope, transient ischemic attacks, urticaria, ventricular fibrillation, visual disturbance, xerostomia
Warnings/Precautions
Concerns related to adverse effects:
- Angina/MI: Increased angina and/or MI has occurred with initiation or dosage titration of dihydropyridine calcium channel blockers. Reflex tachycardia may occur resulting in angina and/or MI in patients with obstructive coronary disease, especially in the absence of concurrent beta-blockade.
- Hypotension/syncope: Symptomatic hypotension with or without syncope can rarely occur; blood pressure must be lowered at a rate appropriate for the patient's clinical condition.
- Peripheral edema: A common side effect is peripheral edema (dose-dependent); may begin within 2 to 3 weeks of starting therapy.
Disease-related concerns:
- Aortic stenosis: Use with extreme caution in patients with severe aortic stenosis; may reduce coronary perfusion resulting in ischemia.
- Heart failure (HF): The ACC/AHA heart failure guidelines recommend to avoid use in patients with heart failure due to lack of benefit and/or worse outcomes with calcium channel blockers in general (ACC/AHA [Yancy 2013]).
- Hepatic impairment: Use with caution in patients with hepatic impairment; may require lower starting dose.
- Hypertrophic cardiomyopathy (HCM) with outflow tract obstruction: Use with caution in patients with HCM and outflow tract obstruction since reduction in afterload may worsen symptoms associated with this condition.
Monitoring Parameters
Blood pressure, heart rate
Hypertension: The 2017 Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults (ACC/AHA [Whelton 2017]):
Confirmed hypertension and known CVD or 10-year ASCVD risk ≥10%: Target blood pressure <130/80 mm Hg is recommended.
Confirmed hypertension without markers of increased ASCVD risk: Target blood pressure <130/80 mm Hg may be reasonable.
Diabetes and hypertension: The American Diabetes Association (ADA) guidelines (ADA 2019):
Patients 18 to 65 years of age, without ASCVD, and 10-year ASCVD risk <15%: Target blood pressure <140/90 mm Hg is recommended.
Patients 18 to 65 years of age and known ASCVD or 10-year ASCVD risk >15%: Target blood pressure <130/80 mm Hg may be appropriate if it can be safely attained.
Patients >65 years of age (healthy or complex/intermediate health): Target blood pressure <140/90 mm Hg is recommended.
Patients >65 years of age (very complex/poor health): Target blood pressure <150/90 mm Hg is recommended.
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Isradipine crosses the human placenta. In a study of 16 women, umbilical cord concentrations were less than maternal serum (Lunell 1993).
Chronic maternal hypertension may increase the risk of birth defects, low birth weight, preterm delivery, stillbirth, and neonatal death. Actual fetal/neonatal risks may be related to duration and severity of maternal hypertension. Untreated hypertension may also increase the risks of adverse maternal outcomes, including gestational diabetes, myocardial infarction, preeclampsia, stroke, and delivery complications (ACOG 203 2019).
Calcium channel blockers may be used to treat hypertension in pregnant women; however, agents other than isradipine are more commonly used (ACOG 203 2019; ESC [Regitz-Zagrosek 2018]). Females with preexisting hypertension may continue their medication during pregnancy unless contraindications exist (ESC [Regitz-Zagrosek 2018]).
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience flushing, loss of strength and energy, nausea, or headache. Have patient report immediately to prescriber abnormal heartbeat, fast heartbeat, severe dizziness, passing out, shortness of breath, excessive weight gain, or swelling of arms or legs (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for health care professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience, and judgment in diagnosing, treating, and advising patients.