Boxed Warning
Torsades de pointes and sudden death
Cases of torsades de pointes, cardiac arrest, and death have been reported with the use of a higher than recommended dosage of loperamide.
Loperamide is contraindicated in pediatric patients <2 years of age.
Avoid dosages higher than recommended in adults and pediatric patients ≥2 years due to the risk of serious cardiac adverse reactions.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
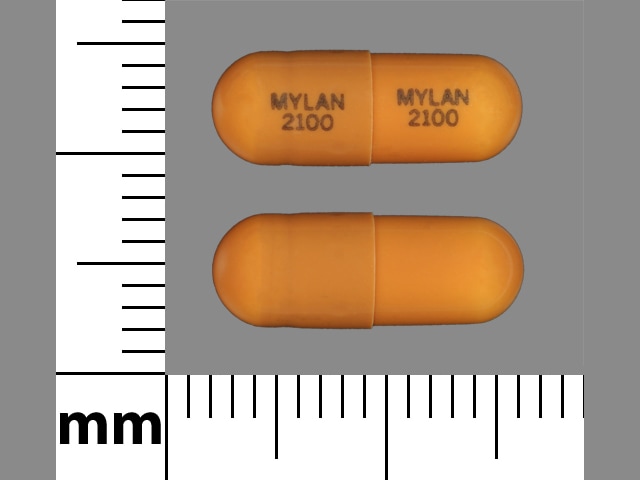
Capsule, Oral, as hydrochloride:
Imodium A-D: 2 mg [contains brilliant blue fcf (fd&c blue #1), peg-40 hydrogenated castor oil]
Generic: 2 mg
Liquid, Oral, as hydrochloride:
Imodium A-D: 1 mg/7.5 mL (120 mL, 240 mL) [contains brilliant blue fcf (fd&c blue #1), fd&c yellow #10 (quinoline yellow), propylene glycol, sodium benzoate]
Imodium A-D: 1 mg/7.5 mL (120 mL, 240 mL) [contains brilliant blue fcf (fd&c blue #1), fd&c yellow #10 (quinoline yellow), propylene glycol, sodium benzoate; mint flavor]
Generic: 1 mg/5 mL (5 mL [DSC], 10 mL [DSC], 118 mL [DSC]); 1 mg/7.5 mL (120 mL)
Suspension, Oral, as hydrochloride:
Generic: 1 mg/7.5 mL (120 mL)
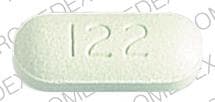
Tablet, Oral, as hydrochloride:
Anti-Diarrheal: 2 mg [scored]
Anti-Diarrheal: 2 mg [scored; contains brilliant blue fcf (fd&c blue #1), corn starch, fd&c yellow #10 (quinoline yellow)]
Anti-Diarrheal: 2 mg [DSC] [contains brilliant blue fcf (fd&c blue #1), fd&c yellow #10 (quinoline yellow)]
Anti-Diarrheal: 2 mg [scored; contains brilliant blue fcf (fd&c blue #1), fd&c yellow #10 (quinoline yellow)]
Anti-Diarrheal: 2 mg [contains fd&c blue #1 aluminum lake, fd&c yellow #10 (quinoline yellow)]
Diamode: 2 mg [scored]
Imodium A-D: 2 mg [scored; contains fd&c blue #1 aluminum lake, fd&c yellow #10 aluminum lake]
Loperamide A-D: 2 mg [DSC]
Pharmacology
Mechanism of Action
Acts directly on circular and longitudinal intestinal muscles, through the opioid receptor, to inhibit peristalsis and prolong transit time; reduces fecal volume, increases viscosity, and diminishes fluid and electrolyte loss; demonstrates antisecretory activity. Loperamide increases tone on the anal sphincter
Pharmacokinetics/Pharmacodynamics
Absorption
Poor
Distribution
Poor penetration into brain
Metabolism
Hepatic via oxidative N-demethylation; CYP2C8 and CYP3A4 (major) and CYP2B6 and CYP2D6 (minor) role in N-demethylation.
Excretion
Feces
Time to Peak
Liquid: 2.5 hours; Capsule: ~5 hours
Half-Life Elimination
9.4 to 14.4 hours
Use: Labeled Indications
Diarrhea:
Rx labeling: Control and symptomatic relief of chronic diarrhea associated with inflammatory bowel disease in adults; acute nonspecific diarrhea in patients ≥2 years; to reduce volume of ileostomy discharge
OTC labeling: Control of symptoms of diarrhea, including Traveler's diarrhea
Use: Off Label
Cancer treatment-induced diarrheabyes
Data from clinical trials, clinical practice guidelines, and reviews support the use of loperamide in the management of cancer treatment-induced diarrhea, including irinotecan-induced diarrhea Andreyev 2014, Benson 2004, Morturano 2012, Park 2016, Rothenberg 1996, Sharma 2005, Swain 2017.
Traveler’s diarrheayes
The American College of Gastroenterology recommends adjunctive loperamide therapy in patients receiving antibiotics for Traveler’s diarrhea to decrease duration of diarrhea and increase chance for a cure Riddle 2016.
Contraindications
Hypersensitivity to loperamide or any component of the formulation; abdominal pain without diarrhea; children <2 years; acute dysentery; acute ulcerative colitis; bacterial enterocolitis (caused by Salmonella, Shigella, and Campylobacter); pseudomembranous colitis associated with broad-spectrum antibiotic use.
Canadian labeling: Additional contraindications (not in the US labeling): When constipation should be avoided; when the inhibition of peristalsis should be avoided
OTC labeling: When used for self-medication, do not use if stool is bloody or black.
Documentation of allergenic cross-reactivity for antidiarrheals is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Dosage and Administration
Dosing: Adult
Acute diarrhea: Oral: Initial: 4 mg, followed by 2 mg after each loose stool (maximum: 16 mg/day)
Chronic diarrhea: Oral: Initial: 4 mg, followed by 2 mg after each loose stool (maximum: 16 mg/day); maintenance dose should be slowly titrated downward to minimum required to control symptoms (usual: 4 to 8 mg/day as a single dose or in divided doses; maximum: 16 mg/day). If clinical improvement is not observed after at least 10 days of treatment with 16 mg/day, symptoms are unlikely to be controlled by further administration; treatment may be continued if diarrhea cannot be adequately controlled with diet or other therapy.
Traveler's diarrhea: Oral: Initial: 4 mg after first loose stool, followed by 2 mg after each subsequent stool (maximum dose: 16 mg/day [OTC: 8 mg/day]); (duration of therapy: ≤48 hours); in patients with moderate-to-severe illness receiving an antibiotic, loperamide is recommended as adjunctive therapy to decrease duration of diarrhea (ACG [Riddle 2016]; however, acquisition of extended-spectrum-beta-lactamase-producing pathogens may be more common when loperamide and antibiotics are coadministered (CDC 2018). Do not use loperamide in cases of dysentery (IDSA [Hill 2006]).
Cancer treatment-induced diarrhea (off-label use): Oral: 4 mg, followed by 2 mg every 2 to 4 hours or after each loose stool (more persistent diarrhea will require the higher frequency); doses >16 mg/day may not provide benefit (Andreyev 2014) or 4 mg, followed by 2 mg every 4 hours or after each loose stool; Maximum: 16 mg/day (Benson 2004; Morturano 2012) or 4 mg followed by 2 mg every 2 hours (may utilize 4 mg every 4 hours at night) until 12 hours have passed without a loose bowel movement (Sharma 2005).
Neratinib-induced diarrhea, prophylaxis (off-label use): Oral: 4 mg 3 times daily (days 1 to 14 of neratinib therapy), followed by 4 mg twice daily (days 15 to 56 of neratinib therapy), followed by 4 mg as needed up to a maximum of 16 mg/day (days 57 to 365 of neratinib therapy) (Nerlynx product labeling 2018). Note: Antidiarrheal prophylaxis is recommended during the first 2 cycles of neratinib therapy; initiate with the first neratinib dose. Titrate to 1 to 2 bowel movements/day. Additional antidiarrheal medication may be required for loperamide-refractory diarrhea.
Irinotecan-induced delayed diarrhea (off-label use): Oral: 4 mg after first loose or frequent bowel movement, then 2 mg every 2 hours (4 mg every 4 hours at night) until 12 hours have passed without a bowel movement (Rothenberg 1996).
Dosing: Geriatric
Refer to adult dosing; use with caution.
Dosing: Pediatric
Acute diarrhea: Note: Loperamide is not recommended for management of infectious diarrhea in pediatric patients (IDSA [Shane 2017]). For patients who are small for chronological age, consider dosing according to weight range and not by age group. Use lowest effective dose for shortest duration.
Children 2 to <12 years: Oral:
2 to 5 years weighing 13 to <21 kg: Initial: 1 mg with first loose stool followed by 1 mg/dose after each subsequent loose stool; maximum daily dose: 3 mg/day
6 to 8 years weighing 21 to 27 kg: Initial: 2 mg with first loose stool followed by 1 mg/dose after each subsequent loose stool; maximum daily dose: 4 mg/day
9 to 11 years weighing 27.1 to 43 kg: Initial: 2 mg with first loose stool followed by 1 mg/dose after each subsequent loose stool; maximum daily dose: 6 mg/day
Children ≥12 years and Adolescents: Oral: Initial: 4 mg with first loose stool followed by 2 mg/dose after each subsequent loose stool; maximum daily dose: 8 mg/day
Chronic diarrhea; secondary to intestinal failure, short-bowel syndrome, or other noninfectious causes: Limited data available; dosing regimens variable: Infants ≥2 months and Children: Oral: 0.08 to 0.24 mg/kg/day divided 2 to 3 times/day was reported in a case series of 10 pediatric patients (age range: 2 to 52 months) (Buts 1975). In a case series of six infants and young children, higher dosing was described: Initial: 1 to 1.5 mg/kg/day in 4 divided doses with subsequent dose decreased as stool output and diet tolerance improved and patient weight increased. Reported final dose range of 0.25 to 0.5 mg/kg/day in 2 divided doses was used long-term until patient achieved target weight and dietary goals; reported duration of therapy: 6 months to ~2 years (Sandhu 1983); maximum single dose: 2 mg
Irinotecan-induced (delayed) diarrhea: Limited data available; consult individual protocols; some organizations have used the following:
Fixed dosing (Children's Oncology Group 2009):
Children ≥2 to 12 years:
<13 kg: Initial: 0.5 mg after the first loose bowel movement, followed by 0.5 mg every 3 hours while awake; during the night, may administer every 4 hours; maximum daily dose: 4 mg/day
13 kg to <20 kg: Initial: 1 mg after the first loose bowel movement, followed by 1 mg every 4 hours; maximum daily dose: 6 mg/day
20 kg to <30 kg: Initial: 2 mg after the first loose bowel movement, followed by 1 mg every 3 hours while awake; during the night, may administer every 4 hours; maximum daily dose: 8 mg/day
30 kg to <43 kg: Initial: 2 mg after the first loose bowel movement, followed by 1 mg every 2 hours while awake; during the night, may administer every 4 hours; maximum daily dose: 12 mg/day
Adolescents weighing ≥43 kg: Initial: 4 mg after the first loose bowel movement, followed by 2 mg after each loose stool; maximum daily dose: 16 mg/day
Weight-directed dosing (Vassal 2007): Children and Adolescents 2 to <15 years:
Grade 1 or 2: 0.03 mg/kg/dose every 4 hours
Grade 3 or 4: 0.06 mg/kg/dose every 4 hours
Maximum single dose dependent upon weight:
<13 kg: 0.5 mg
13 to <20 kg: 1 mg
20 to <43 kg: Initial: 2 mg; subsequent doses: 1 mg
≥43 kg: Initial: 4 mg; subsequent doses: 2 mg
Administration
Oral: Administer with plenty of clear fluids to prevent dehydration.
Oral solution: Shake well before administering dose.
Cancer treatment-induced diarrhea: Consider administering 30 minutes prior to eating 4 times daily to slow gastrocolic reflex (Andreyev 2014).
Dietary Considerations
Some products may contain sodium.
Storage
Store between 20°C and 25°C (68°F and 77°F).
Loperamide Images
Drug Interactions
Desmopressin: Loperamide-Loperamide Oxide may increase the serum concentration of Desmopressin. Monitor therapy
Eluxadoline: Loperamide-Loperamide Oxide may enhance the constipating effect of Eluxadoline. Monitor therapy
Erdafitinib: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Haloperidol: QT-prolonging Agents (Indeterminate Risk - Avoid) may enhance the QTc-prolonging effect of Haloperidol. Monitor therapy
Lasmiditan: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Avoid combination
Lumacaftor and Ivacaftor: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. Lumacaftor and Ivacaftor may increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
P-glycoprotein/ABCB1 Inducers: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inducers may also further limit the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
QT-prolonging Agents (Highest Risk): QT-prolonging Agents (Indeterminate Risk - Avoid) may enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QuiNIDine: May enhance the CNS depressant effect of Loperamide-Loperamide Oxide. Loperamide-Loperamide Oxide may enhance the QTc-prolonging effect of QuiNIDine. QuiNIDine may increase the serum concentration of Loperamide-Loperamide Oxide. Monitor therapy
Ramosetron: Loperamide-Loperamide Oxide may enhance the constipating effect of Ramosetron. Monitor therapy
Ranolazine: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Sincalide: Drugs that Affect Gallbladder Function may diminish the therapeutic effect of Sincalide. Management: Consider discontinuing drugs that may affect gallbladder motility prior to the use of sincalide to stimulate gallbladder contraction. Consider therapy modification
Adverse Reactions
1% to 10%:
Central nervous system: Dizziness (1%)
Gastrointestinal: Constipation (2% to 5%), abdominal cramps (≤3%), nausea (≤3%)
<1%, postmarketing, and/or case reports: Abdominal discomfort, abdominal distention, abdominal pain, anaphylactic shock, anaphylactoid reaction, angioedema, bullous rash (rare), drowsiness, dyspepsia, erythema multiforme (rare), fatigue, flatulence, hypersensitivity reaction, megacolon, paralytic ileus, pruritus, skin rash, Stevens-Johnson syndrome (rare), toxic epidermal necrolysis (rare), toxic megacolon, urinary retention, urticaria, vomiting, xerostomia
Warnings/Precautions
Concerns related to adverse effects:
- Allergic reactions: Rare cases of anaphylaxis and anaphylactic shock have been reported.
- CNS effects: May cause drowsiness or dizziness, which may impair physical or mental abilities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving).
- GI effects: Discontinue promptly if constipation, abdominal pain, abdominal distension, blood in stool, or ileus develop. Do not use when peristalsis inhibition should be avoided due to potential for ileus, megacolon and/or toxic megacolon.
- Torsades de pointes and sudden death: [US Boxed Warning]: Cases of torsades de pointes, cardiac arrest, and death have been reported with the use of a higher than recommended dosage. Contraindicated in pediatric patients <2 years. Avoid dosages higher than recommended in patients ≥2 years due to the risk of serious cardiac adverse reactions. Cases of syncope and ventricular tachycardia have been reported in adults receiving the recommended dose of loperamide. Cases of cardiac arrest, syncope, and respiratory depression have been reported in pediatric patients <2 years. Avoid use in patients with risk factors for QT prolongation (eg, congenital long QT syndrome, history of cardiac arrhythmias or other cardiac conditions, elderly, electrolyte abnormalities) and in combination with others drugs known to prolong the QT interval.
Disease-related concerns:
- AIDS patients: Stop therapy at the first sign of abdominal distention; cases of toxic megacolon have occurred in AIDS patients with infectious colitis (due to viral or bacterial pathogens).
- Hepatic impairment: Use with caution in patients with hepatic impairment due to reduced first-pass metabolism; monitor for signs of CNS toxicity.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Use with caution in the elderly; may be more susceptible to drug-associated effects on the QT interval.
- Pediatric: Use with caution in young children as response may be variable because of dehydration. Contraindicated in children <2 years.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol derivative with caution in neonates. See manufacturer's labeling.
Other warnings/precautions:
- Appropriate use: Loperamide is a symptom-directed treatment; if an underlying diagnosis is made, other disease-specific treatment may be indicated. Concurrent fluid and electrolyte replacement is often necessary in all age groups depending upon severity of diarrhea.
- Duration of use: If diarrhea lasts longer than 2 days, symptoms worsen, or abdominal swelling or bulging develops, discontinue use and consult healthcare provider.
- Self medication (OTC use): Consult health care provider prior to using, if taking antibiotics, if pregnant or breastfeeding, or in the presence of fever, mucus in stool, or a history of liver disease. Serious heart problems may occur if taken more than directed.
Monitoring Parameters
Signs of CNS toxicity in patients with hepatic impairment.
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Adverse effects have not been observed in animal reproduction studies. Information related to loperamide use in pregnancy is limited and data is conflicting (Einarson 2000; Källén 2008). For acute diarrhea in pregnant women, some clinicians recommend oral rehydration and dietary changes; loperamide in small amounts may be used only if symptoms are disabling (Wald 2003).
Patient Education
What is this drug used for?
- It is used to treat diarrhea.
- It is used to lower ostomy output.
Frequently reported side effects of this drug
- Fatigue
- Loss of strength and energy
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Severe dizziness
- Passing out
- Chest pain
- Fast heartbeat
- Abnormal heartbeat
- Severe nausea
- Severe vomiting
- Abdominal pain
- Constipation
- Abdominal edema
- Bloating
- Black, tarry, or bloody stools
- Unable to pass urine
- Change in amount of urine passed
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.