Boxed Warning
Fetal toxicity:
Drugs that act directly on the renin-angiotensin system can cause injury and death to the developing fetus. When pregnancy is detected, discontinue therapy as soon as possible.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Hyzaar 50/12.5: Losartan potassium 50 mg and hydrochlorothiazide 12.5 mg [contains potassium 4.24 mg (0.108 mEq)]
Hyzaar 100/12.5: Losartan potassium 100 mg and hydrochlorothiazide 12.5 mg [contains potassium 8.48 mg (0.216 mEq)]
Hyzaar 100/25: Losartan potassium 100 mg and hydrochlorothiazide 25 mg [contains potassium 8.48 mg (0.216 mEq)]
Generic: 50/12.5: Losartan potassium 50 mg and hydrochlorothiazide 12.5 mg; 100/12.5: Losartan potassium 100 mg and hydrochlorothiazide 12.5 mg; 100/25: Losartan potassium 100 mg and hydrochlorothiazide 25 mg
Pharmacology
Mechanism of Action
Losartan: As a selective and competitive, nonpeptide angiotensin II receptor antagonist, losartan blocks the vasoconstrictor and aldosterone-secreting effects of angiotensin II; losartan interacts reversibly at the AT1 and AT2 receptors of many tissues and has slow dissociation kinetics; its affinity for the AT1 receptor is 1000 times greater than the AT2 receptor. Angiotensin II receptor antagonists may induce a more complete inhibition of the renin-angiotensin system than ACE inhibitors, they do not affect the response to bradykinin, and are less likely to be associated with nonrenin-angiotensin effects (eg, cough and angioedema). Losartan increases urinary flow rate and in addition to being natriuretic and kaliuretic, increases excretion of chloride, magnesium, uric acid, calcium, and phosphate.
Hydrochlorothiazide: Inhibits sodium reabsorption in the distal tubules causing increased excretion of sodium and water as well as potassium and hydrogen ions.
Use: Labeled Indications
Hypertension: Management of hypertension.
Hypertension with left ventricular hypertrophy: To reduce the risk of stroke in patients with hypertension and left ventricular hypertrophy (LVH). Evidence suggests that this benefit does not apply to black patients.
Contraindications
Hypersensitivity to losartan, hydrochlorothiazide, sulfonamide-derived drugs, or any component of the formulation; concomitant use with aliskiren in patients with diabetes mellitus; anuria
Note: Although the product labeling states this medication is contraindicated with other sulfonamide-containing drug classes, the scientific basis of this statement has been challenged. See “Warnings/Precautions” for more detail.
Documentation of allergenic cross-reactivity for angiotensin receptor blockers or thiazide-type diuretics is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Canadian labeling: Additional contraindications (not in U.S. labeling): Concomitant use with aliskiren in patients with moderate-to-severe renal impairment (GFR <60 mL/minute/1.73 m2)
Dosage and Administration
Dosing: Adult
Hypertension: Oral: Note: Dose must be individualized; combination product may be substituted for individual components in patients currently maintained on both agents separately or in patients not adequately controlled with monotherapy. Not indicated for initial therapy of hypertension, except in severe hypertension.
Replacement therapy: Losartan 50 mg/hydrochlorothiazide 12.5 mg or losartan 100 mg/hydrochlorothiazide 12.5 mg or losartan 100 mg/hydrochlorothiazide 25 mg once daily; adjust dose base on blood pressure response. Maximum dose: Losartan 100 mg/hydrochlorothiazide 25 mg per day.
Severe hypertension: Initial: Losartan 50 mg/hydrochlorothiazide 12.5 mg once daily; may titrate dose after ~3 weeks. Maximum dose: Losartan 100 mg/hydrochlorothiazide 25 mg per day.
Hypertension with left ventricular hypertrophy: Oral: Note: Initiate treatment with losartan monotherapy. If blood pressure reduction inadequate, then may initiate losartan/hydrochlorothiazide combination.
Initial: Losartan 50 mg/hydrochlorothiazide 12.5 mg once daily; may increase to losartan 100 mg/hydrochlorothiazide 12.5 mg once daily, followed by losartan 100 mg/hydrochlorothiazide 25 mg once daily if needed to control blood pressure.
Dosing: Geriatric
Refer to adult dosing.
Administration
Administer without regard to meals; however, administer consistently with respect to food intake at about the same time every day.
Dietary Considerations
Some products may contain potassium.
Storage
Store at 25°C (77°C); excursions are permitted between 15°C and 30°C (59°F and 86°F). Protect from light.
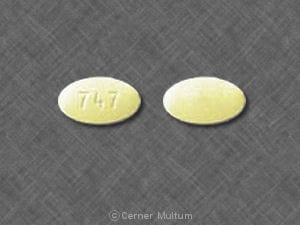
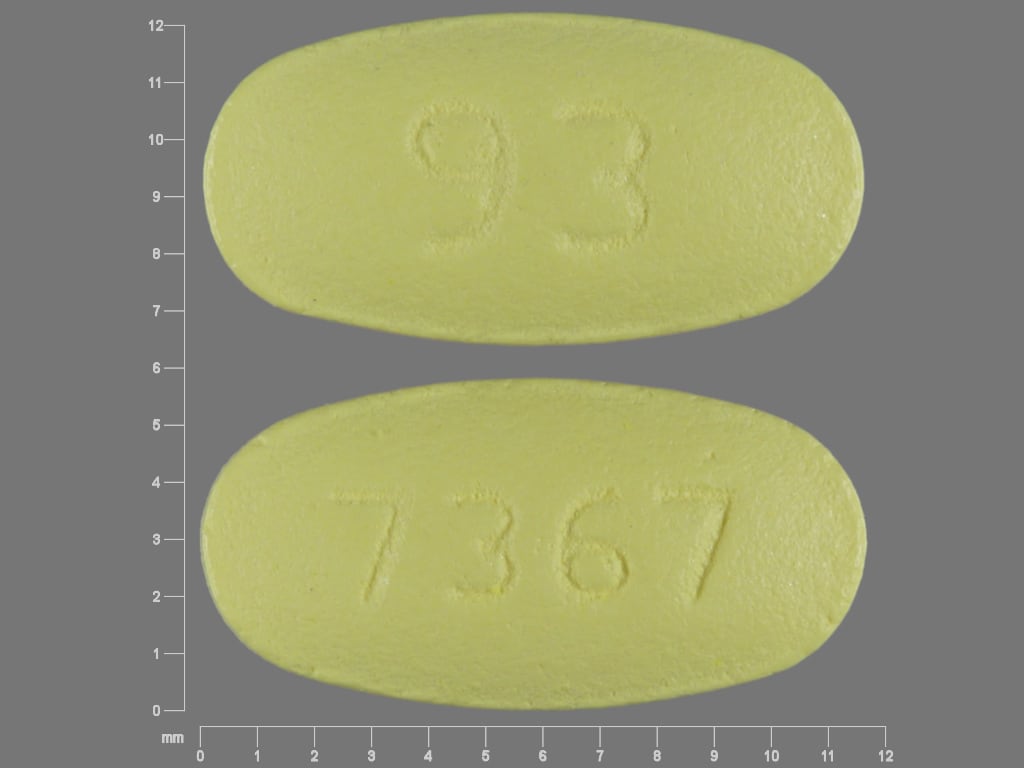
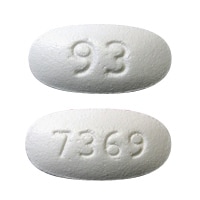
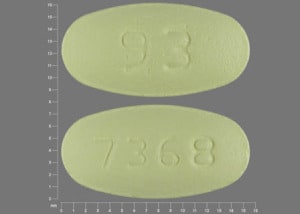
Losartan and Hydrochlorothiazide Images
Drug Interactions
Ajmaline: Sulfonamides may enhance the adverse/toxic effect of Ajmaline. Specifically, the risk for cholestasis may be increased. Monitor therapy
Alcohol (Ethyl): May enhance the orthostatic hypotensive effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Aliskiren: May enhance the hyperkalemic effect of Angiotensin II Receptor Blockers. Aliskiren may enhance the hypotensive effect of Angiotensin II Receptor Blockers. Aliskiren may enhance the nephrotoxic effect of Angiotensin II Receptor Blockers. Management: Aliskiren use with ACEIs or ARBs in patients with diabetes is contraindicated. Combined use in other patients should be avoided, particularly when CrCl is less than 60 mL/min. If combined, monitor potassium, creatinine, and blood pressure closely. Consider therapy modification
Allopurinol: Thiazide and Thiazide-Like Diuretics may enhance the potential for allergic or hypersensitivity reactions to Allopurinol. Thiazide and Thiazide-Like Diuretics may increase the serum concentration of Allopurinol. Specifically, Thiazide Diuretics may increase the concentration of Oxypurinol, an active metabolite of Allopurinol. Monitor therapy
Alpelisib: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Monitor therapy
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Aminolevulinic Acid (Systemic): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Systemic). Avoid combination
Aminolevulinic Acid (Topical): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Topical). Monitor therapy
Amphetamines: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Angiotensin II: Receptor Blockers may diminish the therapeutic effect of Angiotensin II. Monitor therapy
Angiotensin-Converting Enzyme Inhibitors: Angiotensin II Receptor Blockers may enhance the adverse/toxic effect of Angiotensin-Converting Enzyme Inhibitors. Angiotensin II Receptor Blockers may increase the serum concentration of Angiotensin-Converting Enzyme Inhibitors. Management: In US labeling, use of telmisartan and ramipril is not recommended. It is not clear if any other combination of an ACE inhibitor and an ARB would be any safer. Consider alternatives to the combination when possible. Consider therapy modification
Anticholinergic Agents: May increase the serum concentration of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Antidiabetic Agents: Thiazide and Thiazide-Like Diuretics may diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Antidiabetic Agents: Hyperglycemia-Associated Agents may diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Antifungal Agents (Azole Derivatives, Systemic): May decrease the metabolism of Losartan. Applicable Isavuconazonium considerations are addressed in separate monographs. Exceptions: Isavuconazonium Sulfate. Monitor therapy
Antihepaciviral Combination Products: May increase the serum concentration of Losartan. Management: Per antihepaciviral combination product US prescribing information, consider decreasing the losartan dose and monitoring for evidence of hypotension and worsening renal function if these agents are used in combination. Consider therapy modification
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Beta2-Agonists: May enhance the hypokalemic effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Bile Acid Sequestrants: May decrease the absorption of Thiazide and Thiazide-Like Diuretics. The diuretic response is likewise decreased. Consider therapy modification
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Brigatinib: May diminish the antihypertensive effect of Antihypertensive Agents. Brigatinib may enhance the bradycardic effect of Antihypertensive Agents. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Calcium Salts: Thiazide and Thiazide-Like Diuretics may decrease the excretion of Calcium Salts. Continued concomitant use can also result in metabolic alkalosis. Monitor therapy
Cardiac Glycosides: Thiazide and Thiazide-Like Diuretics may enhance the adverse/toxic effect of Cardiac Glycosides. Specifically, cardiac glycoside toxicity may be enhanced by the hypokalemic and hypomagnesemic effect of thiazide diuretics. Monitor therapy
Corticosteroids (Orally Inhaled): May enhance the hypokalemic effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Corticosteroids (Systemic): May enhance the hypokalemic effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Cyclophosphamide: Thiazide and Thiazide-Like Diuretics may enhance the adverse/toxic effect of Cyclophosphamide. Specifically, granulocytopenia may be enhanced. Monitor therapy
CycloSPORINE (Systemic): Angiotensin II Receptor Blockers may enhance the hyperkalemic effect of CycloSPORINE (Systemic). Monitor therapy
CYP2C9 Inhibitors (Moderate): May decrease the metabolism of CYP2C9 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP2C9 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dapoxetine: May enhance the orthostatic hypotensive effect of Angiotensin II Receptor Blockers. Monitor therapy
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Dexketoprofen: May enhance the adverse/toxic effect of Sulfonamides. Monitor therapy
Dexmethylphenidate: May diminish the therapeutic effect of Antihypertensive Agents. Monitor therapy
Diacerein: May enhance the therapeutic effect of Diuretics. Specifically, the risk for dehydration or hypokalemia may be increased. Monitor therapy
Diazoxide: Thiazide and Thiazide-Like Diuretics may enhance the adverse/toxic effect of Diazoxide. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Dichlorphenamide: Thiazide and Thiazide-Like Diuretics may enhance the hypokalemic effect of Dichlorphenamide. Monitor therapy
Dofetilide: HydroCHLOROthiazide may enhance the QTc-prolonging effect of Dofetilide. HydroCHLOROthiazide may increase the serum concentration of Dofetilide. Avoid combination
Drospirenone: Angiotensin II Receptor Blockers may enhance the hyperkalemic effect of Drospirenone. Monitor therapy
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Enzalutamide: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP2C9 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP2C9 substrate should be performed with caution and close monitoring. Consider therapy modification
Eplerenone: May enhance the hyperkalemic effect of Angiotensin II Receptor Blockers. Monitor therapy
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Fexinidazole [INT]: Thiazide and Thiazide-Like Diuretics may enhance the arrhythmogenic effect of Fexinidazole [INT]. Avoid combination
Fluconazole: May decrease the serum concentration of Losartan. Specifically, fluconazole may decrease the serum concentration of E3174, the more potent active metabolite of losartan. Monitor therapy
Heparin: May enhance the hyperkalemic effect of Angiotensin II Receptor Blockers. Monitor therapy
Heparins (Low Molecular Weight): May enhance the hyperkalemic effect of Angiotensin II Receptor Blockers. Monitor therapy
Herbs (Hypertensive Properties): May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Ipragliflozin: May enhance the adverse/toxic effect of Thiazide and Thiazide-Like Diuretics. Specifically, the risk for intravascular volume depletion may be increased. Monitor therapy
Ivabradine: Thiazide and Thiazide-Like Diuretics may enhance the arrhythmogenic effect of Ivabradine. Monitor therapy
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Levosulpiride: Thiazide and Thiazide-Like Diuretics may enhance the adverse/toxic effect of Levosulpiride. Avoid combination
Licorice: May enhance the hypokalemic effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Lithium: Thiazide and Thiazide-Like Diuretics may decrease the excretion of Lithium. Consider therapy modification
Lithium: Angiotensin II Receptor Blockers may increase the serum concentration of Lithium. Management: Lithium dosage reductions will likely be needed following the addition of an angiotensin II receptor antagonist. Consider therapy modification
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Mecamylamine: Sulfonamides may enhance the adverse/toxic effect of Mecamylamine. Avoid combination
Methenamine: Thiazide and Thiazide-Like Diuretics may diminish the therapeutic effect of Methenamine. Monitor therapy
Methylphenidate: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
MiFEPRIStone: May increase the serum concentration of CYP2C9 Substrates (High risk with Inhibitors). Management: Use CYP2C9 substrates at the lowest recommended dose, and monitor closely for adverse effects, during and in the 2 weeks following mifepristone treatment. Consider therapy modification
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Multivitamins/Fluoride (with ADE): May enhance the hypercalcemic effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): Thiazide and Thiazide-Like Diuretics may enhance the hypercalcemic effect of Multivitamins/Minerals (with ADEK, Folate, Iron). Monitor therapy
Multivitamins/Minerals (with AE, No Iron): Thiazide and Thiazide-Like Diuretics may increase the serum concentration of Multivitamins/Minerals (with AE, No Iron). Specifically, thiazide diuretics may decrease the excretion of calcium, and continued concomitant use can also result in metabolic alkalosis. Monitor therapy
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Neuromuscular-Blocking Agents (Nondepolarizing): Thiazide and Thiazide-Like Diuretics may enhance the neuromuscular-blocking effect of Neuromuscular-Blocking Agents (Nondepolarizing). Monitor therapy
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hyperkalemic effect of Angiotensin II Receptor Blockers. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents: Thiazide and Thiazide-Like Diuretics may enhance the nephrotoxic effect of Nonsteroidal Anti-Inflammatory Agents. Nonsteroidal Anti-Inflammatory Agents may diminish the therapeutic effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents: Angiotensin II Receptor Blockers may enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Specifically, the combination may result in a significant decrease in renal function. Nonsteroidal Anti-Inflammatory Agents may diminish the therapeutic effect of Angiotensin II Receptor Blockers. The combination of these two agents may also significantly decrease glomerular filtration and renal function. Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Opioid Agonists: May enhance the adverse/toxic effect of Diuretics. Opioid Agonists may diminish the therapeutic effect of Diuretics. Monitor therapy
OXcarbazepine: Thiazide and Thiazide-Like Diuretics may enhance the adverse/toxic effect of OXcarbazepine. Specifically, there may be an increased risk for hyponatremia. Monitor therapy
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Porfimer: Photosensitizing Agents may enhance the photosensitizing effect of Porfimer. Monitor therapy
Potassium Salts: May enhance the hyperkalemic effect of Angiotensin II Receptor Blockers. Monitor therapy
Potassium-Sparing Diuretics: Angiotensin II Receptor Blockers may enhance the hyperkalemic effect of Potassium-Sparing Diuretics. Monitor therapy
Promazine: Thiazide and Thiazide-Like Diuretics may enhance the QTc-prolonging effect of Promazine. Avoid combination
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Ranolazine: May enhance the adverse/toxic effect of Angiotensin II Receptor Blockers. Monitor therapy
Reboxetine: May enhance the hypokalemic effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Resveratrol: May decrease serum concentrations of the active metabolite(s) of Losartan. Resveratrol may increase the serum concentration of Losartan. Monitor therapy
RifAMPin: May decrease the serum concentration of Losartan. Monitor therapy
Rifapentine: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Selective Serotonin Reuptake Inhibitors: May enhance the hyponatremic effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Sodium Phosphates: Angiotensin II Receptor Blockers may enhance the nephrotoxic effect of Sodium Phosphates. Specifically, the risk of acute phosphate nephropathy may be enhanced. Management: Consider avoiding this combination by temporarily suspending treatment with ARBs, or seeking alternatives to oral sodium phosphate bowel preparation. If the combination cannot be avoided, maintain adequate hydration and monitor renal function closely. Consider therapy modification
Sodium Phosphates: Diuretics may enhance the nephrotoxic effect of Sodium Phosphates. Specifically, the risk of acute phosphate nephropathy may be enhanced. Management: Consider avoiding this combination by temporarily suspending treatment with diuretics, or seeking alternatives to oral sodium phosphate bowel preparation. If the combination cannot be avoided, hydrate adequately and monitor fluid and renal status. Consider therapy modification
Tacrolimus (Systemic): Angiotensin II Receptor Blockers may enhance the hyperkalemic effect of Tacrolimus (Systemic). Monitor therapy
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Tolvaptan: May enhance the hyperkalemic effect of Angiotensin II Receptor Blockers. Monitor therapy
Topiramate: Thiazide and Thiazide-Like Diuretics may enhance the hypokalemic effect of Topiramate. Thiazide and Thiazide-Like Diuretics may increase the serum concentration of Topiramate. Management: Monitor for increased topiramate levels/adverse effects (e.g., hypokalemia) with initiation/dose increase of a thiazide diuretic. Closely monitor serum potassium concentrations with concomitant therapy. Topiramate dose reductions may be necessary. Consider therapy modification
Toremifene: Thiazide and Thiazide-Like Diuretics may enhance the hypercalcemic effect of Toremifene. Monitor therapy
Trimethoprim: May enhance the hyperkalemic effect of Angiotensin II Receptor Blockers. Monitor therapy
Valsartan: HydroCHLOROthiazide may enhance the hypotensive effect of Valsartan. Valsartan may increase the serum concentration of HydroCHLOROthiazide. Monitor therapy
Verteporfin: Photosensitizing Agents may enhance the photosensitizing effect of Verteporfin. Monitor therapy
Vitamin D Analogs: Thiazide and Thiazide-Like Diuretics may enhance the hypercalcemic effect of Vitamin D Analogs. Monitor therapy
Yohimbine: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Test Interactions
See individual agents.
Adverse Reactions
Based on clinical trials of the combination product in patients with primary hypertension. Also see individual agents.
1% to 10%:
Central nervous system: Dizziness (6%)
Neuromuscular & skeletal: Back pain (2%)
Respiratory: Upper respiratory tract infection (6%)
<2%, postmarketing, case reports, or frequency not defined (some reactions attributed to single component): Abdominal pain, adult respiratory distress syndrome, agranulocytosis, anaphylaxis, anemia, anorexia, aplastic anemia, arthralgia, blurred vision (transient), chest pain, constipation, cutaneous lupus erythematous, diarrhea, dysgeusia, dyspepsia, edema, electrolyte disturbance, erectile dysfunction, erythroderma, fever, gastric irritation, glycosuria, headache, hemolytic anemia, hepatic insufficiency, hepatitis, hyperglycemia, hyperuricemia, hypokalemia, hyponatremia, impotence, insomnia, interstitial nephritis, jaundice (intrahepatic cholestatic jaundice), leukopenia, malaise, migraine, muscle cramps, muscle spasm, myalgia, nasal congestion, nausea, necrotizing angiitis (vasculitis, cutaneous vasculitis), orthostatic effect (dose-related), palpitations, pancreatitis, paranasal sinus disease, paresthesia, pharyngitis, pruritus, purpura, renal failure, renal insufficiency, respiratory distress (including pneumonitis and pulmonary edema), restlessness, rhabdomyolysis, sialadenitis, skin photosensitivity, skin rash, swelling, tachycardia, thrombocytopenia, toxic epidermal necrolysis, urticaria, vomiting, weakness, xanthopsia
Warnings/Precautions
Concerns related to adverse effects:
- Angioedema: Angioedema has been reported rarely with some angiotensin II receptor antagonists (ARBs) and may occur at any time during treatment (especially following first dose). It may involve the head and neck (potentially compromising airway) or the intestine (presenting with abdominal pain). Patients with idiopathic or hereditary angioedema or previous angioedema associated with ACE-inhibitor therapy may be at an increased risk. Prolonged frequent monitoring may be required, especially if tongue, glottis, or larynx are involved, as they are associated with airway obstruction. Patients with a history of airway surgery may have a higher risk of airway obstruction. Discontinue therapy immediately if angioedema occurs. Aggressive early management is critical. Intramuscular (IM) administration of epinephrine may be necessary. Do not readminister to patients who have had angioedema with ARBs.
- Electrolyte disturbances: Hyperkalemia may occur with losartan; risk factors include renal dysfunction, diabetes mellitus, and concomitant use of potassium-sparing diuretics, potassium supplements, and/or potassium-containing salts. Use cautiously, if at all, with these agents and monitor potassium closely. Thiazide diuretics may cause hypokalemia, hypochloremic alkalosis, hypomagnesemia, and hyponatremia.
- Hypersensitivity reactions: Hypersensitivity reactions may occur with hydrochlorothiazide. Risk is increased in patients with a history of allergy or bronchial asthma.
- Hypotension: Symptomatic hypotension may occur upon initiation in patients who are salt- or volume-depleted (eg, those treated with high-dose diuretics); correct volume depletion prior to administration. This transient hypotensive response is not a contraindication to further treatment with losartan/hydrochlorothiazide.
- Ocular effects: Hydrochlorothiazide may cause acute transient myopia and acute angle-closure glaucoma, typically occurring within hours to weeks following initiation; discontinue therapy immediately in patients with acute decreases in visual acuity or ocular pain. Additional treatments may be needed if uncontrolled intraocular pressure persists. Risk factors may include a history of sulfonamide or penicillin allergy.
- Photosensitivity: Photosensitization may occur with use of hydrochlorothiazide.
- Renal function deterioration: May be associated with deterioration of renal function and/or increases in serum creatinine, particularly in patients with low renal blood flow (eg, renal artery stenosis, heart failure) whose glomerular filtration rate (GFR) is dependent on efferent arteriolar vasoconstriction by angiotensin II; deterioration may result in oliguria, acute renal failure, and progressive azotemia. Small increases in serum creatinine may occur following initiation; consider discontinuation only in patients with progressive and/or significant deterioration in renal function.
- Sulfonamide (“sulfa”) allergy: The product labeling for many medications containing a sulfonamide chemical group includes a broad contraindication in patients with a prior allergic reaction to sulfonamides. There is a potential for cross-reactivity between members of a specific class (eg, two antibiotic sulfonamides). However, concerns for cross-reactivity have previously extended to all compounds containing the sulfonamide structure (SO2NH2). An expanded understanding of allergic mechanisms indicates cross-reactivity between antibiotic sulfonamides and nonantibiotic sulfonamides may not occur or at the very least this potential is extremely low (Brackett 2004; Johnson 2005; Slatore 2004; Tornero 2004). In particular, mechanisms of cross-reaction due to antibody production (anaphylaxis) are unlikely to occur with nonantibiotic sulfonamides. T-cell-mediated (type IV) reactions (eg, maculopapular rash) are less well understood and it is not possible to completely exclude this potential based on current insights. In cases where prior reactions were severe (Stevens-Johnson syndrome/TEN), some clinicians choose to avoid exposure to these classes.
Disease-related concerns:
- Aortic/mitral stenosis: Use losartan with caution in patients with significant aortic/mitral stenosis.
- Bariatric surgery: Dehydration: Avoid diuretics in the immediate postoperative period after bariatric surgery; electrolyte disturbances and dehydration may occur. Diuretics may be resumed, if indicated, once oral fluid intake goals are met (Ziegler 2009).
- Diabetes: Use hydrochlorothiazide with caution in patients with prediabetes or diabetes mellitus; may see a change in glucose control.
- Gout: In certain patients with a history of gout, a familial predisposition to gout, or chronic renal failure, gout can be precipitated by hydrochlorothiazide. This risk may be increased with doses ≥25 mg (Gurwitz 1997).
- Hepatic impairment: Use is not recommended for initial therapy in patients with hepatic impairment. Use with caution in hepatic impairment or progressive hepatic disease; avoid electrolyte and acid/base imbalances that might lead to hepatic encephalopathy/coma.
- Hypercalcemia: Thiazide diuretics may decrease renal calcium excretion; consider avoiding use in patients with hypercalcemia.
- Hypercholesterolemia: Use with caution in patients with moderate or high cholesterol concentrations; increased cholesterol and triglyceride levels have been reported with thiazides.
- Parathyroid disease: Thiazide diuretics reduce calcium excretion; pathologic changes in the parathyroid glands with hypercalcemia and hypophosphatemia have been observed with prolonged use; should be discontinued prior to testing for parathyroid function.
- Renal artery stenosis: Use losartan with caution in patients with unstented unilateral/bilateral renal artery stenosis. When unstented bilateral renal artery stenosis is present, use is generally avoided due to the elevated risk of deterioration in renal function unless possible benefits outweigh risks.
- Renal impairment: Use losartan with caution with preexisting renal insufficiency. Avoid hydrochlorothiazide in severe renal disease (ineffective); may precipitate azotemia; discontinue or consider withholding if renal impairment occurs. Contraindicated in patients with anuria.
- Systemic lupus erythematosus (SLE): Hydrochlorothiazide can cause SLE exacerbation or activation.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Black patients: When used to reduce the risk of stroke in patients with HTN and LVH, may not be effective in the black population.
- Pregnancy: [US Boxed Warning]: Drugs that act on the renin-angiotensin system can cause injury and death to the developing fetus. Discontinue as soon as possible once pregnancy is detected.
- Surgical patients: In patients on chronic angiotensin receptor blocker (ARB) therapy, intraoperative hypotension may occur with induction and maintenance of general anesthesia; however, discontinuation of therapy prior to surgery is controversial. If continued preoperatively, avoidance of hypotensive agents during surgery is prudent (Hillis, 2011).
Other warnings/precautions:
- Appropriate use: Not indicated for initial therapy of hypertension, except in severe hypertension where the benefit of a prompt blood pressure reduction exceeds the risk of initiating combination therapy. Do not use as initial therapy in patients with intravascular volume depletion; correct prior to use.
Monitoring Parameters
Baseline and periodic blood pressure, serum electrolytes, renal function
Pregnancy
Pregnancy Considerations
[US Boxed Warning]: Drugs that act directly on the renin-angiotensin system can cause injury and death to the developing fetus. When pregnancy is detected, discontinue therapy as soon as possible.
Refer to individual monographs for additional information.
Patient Education
What is this drug used for?
- It is used to treat high blood pressure.
- It is used to prevent strokes.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Dizziness
- Common cold symptoms
- Back pain
- Runny nose
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- High blood sugar like confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit.
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain.
- Fluid and electrolyte problems like mood changes, confusion, muscle pain or weakness, abnormal heartbeat, severe dizziness, passing out, fast heartbeat, increased thirst, seizures, loss of strength and energy, lack of appetite, unable to pass urine or change in amount of urine passed, dry mouth, dry eyes, nausea, or vomiting.
- Lupus like rash on the cheeks or other body parts, sunburn easy, muscle or joint pain, chest pain or shortness of breath, or swelling in the arms or legs.
- Swelling of arms or legs
- Skin changes
- Vision changes
- Eye pain
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.