|
WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Lybalvi is not approved for the treatment of patients with dementia-related psychosis [see Warnings and Precautions (5.1)]. |
Highlights of prescribing information
INDICATIONS AND USAGE
Lybalvi is a combination of olanzapine, an atypical antipsychotic, and samidorphan, an opioid antagonist, indicated for the treatment of:
- Schizophrenia in adults (1)
- Bipolar I disorder in adults (1)
- Acute treatment of manic or mixed episodes as monotherapy and as adjunct to lithium or valproate
- Maintenance monotherapy treatment
DOSAGE AND ADMINISTRATION
| Indication | Recommended Starting Dose (olanzapine/samidorphan) |
Recommended Dose (olanzapine/samidorphan) |
|
Schizophrenia (2.2) |
5 mg/10 mg or 10 mg/10 mg |
10 mg/10 mg 15 mg/10 mg 20 mg/10 mg |
|
Bipolar I disorder (manic or mixed episodes) (2.3) |
10 mg/10 mg or 15 mg/10 mg |
15 mg/10 mg 5 mg/10 mg 10 mg/10 mg 15 mg/10 mg 20 mg/10 mg |
|
Bipolar I disorder adjunct to lithium or valproate (2.3) |
10 mg/10 mg |
10 mg/10 mg 15 mg/10 mg 20 mg/10 mg |
- See the full prescribing information for the recommended titration and maximum recommended dosage. (2.2, 2.3)
- Administer Lybalvi once daily with or without food. Do not divide tablets or combine strengths. (2.4)
- Recommended starting dosage is 5 mg/10 mg once daily in patients who have a predisposition to hypotensive reactions, have potential for slower metabolism of olanzapine, or may be more pharmacodynamically sensitive to olanzapine. (2.5)
DOSAGE FORMS AND STRENGTHS
Tablets (olanzapine/samidorphan): 5 mg/10 mg, 10 mg/10 mg, 15 mg/10 mg and 20 mg/10 mg. (3)
CONTRAINDICATIONS
- Patients using opioids. (4)
- Patients undergoing acute opioid withdrawal. (4)
- If Lybalvi is administered with lithium or valproate, refer to the lithium or valproate Prescribing Information for the contraindications for those products. (4)
WARNINGS AND PRECAUTIONS
- Cerebrovascular Adverse Reactions in Elderly Patients with DementiaRelated Psychosis: Increased incidence of cerebrovascular adverse reactions (e.g., stroke, transient ischemic attack, including fatalities). (5.2)
- Precipitation of Opioid Withdrawal in Patients Who are Dependent on Opioids: Lybalvi can precipitate opioid withdrawal in patients who are dependent on opioids. Prior to initiating Lybalvi, there should be at least a 7-day opioid-free interval from the last use of short-acting opioids, and at least a 14-day opioid-free interval from the last use of long-acting opioids to avoid precipitation of opioid withdrawal. (2.1, 5.3)
- Vulnerability to Life-Threatening Opioid Overdose:
- Risk of Opioid Overdose from Attempts to Overcome Lybalvi Opioid
- Blockade: Attempts to overcome Lybalvi opioid blockade with high or repeated doses of opioids may lead to fatal opioid intoxication, particularly if Lybalvi therapy is interrupted or discontinued. (5.4)
- Risk of Resuming Opioids in Patients with Prior Opioid Use: Patients with a history of chronic opioid use prior to Lybalvi treatment may have decreased opioid tolerance if Lybalvi therapy is interrupted or discontinued. (5.4)
- Neuroleptic Malignant Syndrome: Manage with immediate discontinuation and close monitoring. (5.5)
- Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS): Discontinue if DRESS is suspected. (5.6)
- Metabolic Changes: Monitor for hyperglycemia/diabetes mellitus, dyslipidemia, and weight gain. (5.7)
- Tardive Dyskinesia: Discontinue if clinically appropriate. (5.8)
- Orthostatic Hypotension and Syncope: Monitor heart rate and blood pressure and warn patients with known cardiovascular or cerebrovascular disease, and risk of dehydration or syncope. (5.9)
- Leukopenia, Neutropenia, and Agranulocytosis: Perform complete blood counts in patients with a history of a clinically significant low white blood cell (WBC) count. Consider discontinuation if clinically significant decline in WBC in the absence of other causative factors. (5.11)
- Seizures: Use cautiously in patients with a history of seizures or with conditions that lower the seizure threshold. (5.13)
- Potential for Cognitive and Motor Impairment: Use caution when operating machinery. (5.14)
- Anticholinergic (Antimuscarinic) Effects: Use with caution with other anticholinergic drugs and in patients with urinary retention, prostatic hypertrophy, constipation, paralytic ileus or related conditions. (5.16)
- Hyperprolactinemia: May elevate prolactin levels. (5.17)
ADVERSE REACTIONS
Most common adverse reactions (incidence ≥5% and at least twice placebo):
- Schizophrenia (Lybalvi): weight increased, somnolence, dry mouth, and headache. (6.1)
- Bipolar I Disorder, Manic or Mixed Episodes (olanzapine): asthenia, dry mouth, constipation, increased appetite, somnolence, dizziness, tremor. (6.1)
- Bipolar I Disorder, Manic or Mixed Episodes, adjunct to Lithium or Valproate (olanzapine): dry mouth, dyspepsia, weight gain, increased appetite, dizziness, back pain, constipation, speech disorder, increased salivation, amnesia, paresthesia. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Alkermes at 1-888-235-8008 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- Strong CYP3A4 Inducers: Not recommended. (7.1)
- Strong CYP1A2 Inhibitors: Consider dosage reduction of olanzapine component of Lybalvi. (7.1)
- CYP1A2 Inducer: Consider dosage increase of the olanzapine component of Lybalvi. (7.1)
- CNS Acting Drugs: May potentiate orthostatic hypotension. (7.1)
- Anticholinergic Drugs: Can increase risk for severe gastrointestinal adverse reactions. (7.1)
- Antihypertensive Agents: Monitor blood pressure. (7.2)
- Levodopa and Dopamine Agonists: Not recommended. (7.2)
USE IN SPECIFIC POPULATIONS
- Pregnancy: May cause extrapyramidal and/or withdrawal symptoms in neonates with third trimester exposure. (8.1)
- Renal Impairment: Use is not recommended in patients with end-stage renal disease. (8.7)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 5/2021
Indications and usage
Lybalvi is indicated for the treatment of:
- Schizophrenia in adults
- Bipolar I disorder in adults
- Acute treatment of manic or mixed episodes as monotherapy and as adjunct to lithium or valproate
- Maintenance monotherapy treatment
Dosage and administration
2.1. Lybalvi Initiation in Patients Using Opioids
Lybalvi is contraindicated in patients using opioids or undergoing acute opioid withdrawal.
In patients who use opioids, delay initiation of Lybalvi for a minimum of 7 days after last use of short-acting opioids and 14 days after last use of long-acting opioids [see Warnings and Precautions (5.3)].
2.2. Recommended Dosage in Schizophrenia
Initiate Lybalvi at 5 mg/10 mg (contains 5 mg of olanzapine and 10 mg of samidorphan) or 10 mg/10 mg (contains 10 mg of olanzapine and 10 mg of samidorphan) orally once daily. The recommended dosage is 10 mg/10 mg, 15 mg/10 mg (contains 15 mg of olanzapine and 10 mg of samidorphan), or 20 mg/10 mg (contains 20 mg of olanzapine and 10 mg of samidorphan) once daily.
Dosage may be adjusted at weekly intervals of 5 mg (based on the olanzapine component of Lybalvi) depending upon clinical response and tolerability, up to the maximum recommended dosage of 20 mg/10 mg once daily.
2.3. Recommended Dosage in Bipolar I Disorder (Manic or Mixed Episodes)
Monotherapy: Initiate Lybalvi at 10 mg/10 mg or 15 mg/10 mg once daily. The recommended dosage is 10 mg/10 mg, 15 mg/10 mg, or 20 mg/10 mg once daily. The maximum recommended dosage is 20 mg/10 mg once daily.
Dosage adjustments should occur at intervals of not less than 24 hours. When dosage adjustments are necessary, dose increments/decrements of 5 mg (based on the olanzapine component of Lybalvi) are recommended.
Maintenance Monotherapy: Administer Lybalvi at 5 mg/10 mg, 10 mg/10 mg, 15 mg/10 mg, or 20 mg/10 mg once daily.
Adjunctive to lithium or valproate: Initiate Lybalvi at 10 mg/10 mg once daily. The recommended dosage is 10 mg/10 mg, 15 mg/10 mg or 20 mg/10 mg, once daily.
Dosage may be adjusted at weekly intervals of 5 mg (based on the olanzapine component of Lybalvi), depending upon clinical response and tolerability, up to the maximum recommended dosage of 20 mg/10 mg once daily.
2.4. Administration Information
Administer Lybalvi orally once daily with or without food as a single tablet. Do not divide tablets or combine strengths.
2.5. Dosage Recommendations in Specific Populations
The recommended starting dosage of Lybalvi is 5 mg/10 mg once daily in patients who have a higher risk of hypotensive reactions, are at risk of slower olanzapine metabolism, or may be more pharmacodynamically sensitive to olanzapine [see Warnings and Precautions (5.9), Drug Interactions (7.2), Use in Specific Populations (8.5), and Clinical Pharmacology (12.3)]. If dose escalation is necessary, increase the dosage slowly in these patients.
Dosage forms and strengths
Lybalvi tablets are available in four strengths (Table 1).
Table 1: Lybalvi Tablet Strengths and Identifying Features
| Tablet strength | Tablet color/shape | Tablet markings |
| 5 mg/10 mg (olanzapine/samidorphan) | Yellow, capsule-shaped | “OS” and “5” |
| 10 mg/10 mg (olanzapine/samidorphan) | Orange, capsule-shaped | “OS” and “10” |
| 15 mg/10 mg (olanzapine/samidorphan) | Blue, capsule-shaped | “OS” and “15” |
| 20 mg/10 mg (olanzapine/samidorphan) | Pink, capsule-shaped | “OS” and “20” |
Contraindications
Lybalvi is contraindicated in patients:
- who are using opioids [see Warnings and Precautions(5.3, 5.4), Drug Interactions (7.3)].
- who are undergoing acute opioid withdrawal [see Warnings and Precautions (5.3, 5.4), Drug Interactions (7.3)].
If Lybalvi is administered with lithium or valproate, refer to the lithium or valproate Prescribing Information for the contraindications for these products [see Warnings and Precautions (5.18)].
Lybalvi Images
Warnings and precautions
5.1 Increased Mortality in Elderly Patients with Dementia-Related Psychosis
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. In placebo-controlled clinical trials of elderly patients with dementiarelated psychosis, the incidence of death in olanzapine-treated patients was significantly greater than in placebo-treated patients (3.5% vs 1.5%, respectively). Analyses of 17 placebo-controlled trials (modal duration of 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in the drug-treated patients of between 1.6 to 1.7 times that seen in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug-treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. Lybalvi is not approved for the treatment of patients with dementia-related psychosis [see Warnings and Precautions (5.2)].
5.2 Cerebrovascular Adverse Reactions, Including Stroke in Elderly Patients with Dementia-Related Psychosis
Cerebrovascular adverse reactions (e.g., stroke, transient ischemic attack), including fatalities, were reported in patients in trials of olanzapine in elderly patients with dementia-related psychosis. In placebo-controlled trials, there was a significantly higher incidence of cerebrovascular adverse reactions in patients treated with olanzapine compared to patients treated with placebo. Lybalvi is not approved for the treatment of patients with dementiarelated psychosis [see Warnings and Precautions (5.1)].
5.3 Precipitation of Severe Opioid Withdrawal in Patients Who Are Physiologically Dependent on Opioids
Samidorphan, an opioid antagonist that is a component of Lybalvi, can precipitate opioid withdrawal in patients who are dependent on opioids, which can lead to an opioid withdrawal syndrome, sometimes requiring hospitalization. Therefore, Lybalvi is contraindicated in Reference ID: 4803431 6 patients who are using opioids or undergoing acute opioid withdrawal. Prior to initiating Lybalvi, there should be at least a 7-day opioid-free interval from last use of short-acting opioids, and at least a 14-day opioid-free interval from the last use of long-acting opioids. Explain the risks associated with precipitated withdrawal and the importance of giving an accurate account of last opioid use to patients and caregivers [see Dosage and Administration (2.1), Drug Interactions (7.3)].
5.4 Vulnerability to Life-Threatening Opioid Overdose
Risk of Opioid Overdose from Attempts to Overcome Samidorphan Blockade
Lybalvi contains samidorphan, an opioid antagonist. Attempting to overcome Lybalvi’s opioid blockade with high or repeated doses of exogenous opioids (e.g., because of ineffective analgesia or opioid withdrawal symptoms) could lead to life-threatening or fatal opioid intoxication (e.g., respiratory arrest, circulatory collapse), particularly if Lybalvi therapy is interrupted or discontinued, subjecting the patient to high levels of unopposed opioid agonist as the samidorphan blockade wanes. Inform patients of the potential consequences of trying to overcome the opioid blockade and the serious risks of taking opioids concurrently with Lybalvi or while transitioning off Lybalvi.
In emergency situations, if a Lybalvi-treated patient requires opioid treatment as part of anesthesia or analgesia:
- Discontinue Lybalvi,
- Opioids should be administered by individual(s) trained in the use of anesthetic drugs and the management of the respiratory effects of opioids, specifically the establishment and maintenance of a patent airway and assisted ventilation, and
- Appropriately trained personnel should continuously monitor the patient in a setting equipped and staffed for cardiopulmonary resuscitation. For recommendations on starting opioids in Lybalvi-treated patients in non-emergent situations, see Drug Interactions (7.3).
Risk of Resuming Opioids in Patients with Prior Opioid Use
Patients with a history of chronic opioid use prior to treatment with Lybalvi may have decreased opioid tolerance if Lybalvi therapy is interrupted or discontinued. Advise patients that this decreased tolerance may increase the risk of opioid overdose if opioids are resumed at the previously tolerated dosage.
5.5 Neuroleptic Malignant Syndrome
Neuroleptic Malignant Syndrome (NMS), a potentially fatal symptom complex, has been reported in association with administration of antipsychotic drugs. Clinical manifestations of NMS are hyperpyrexia, muscle rigidity, delirium, and autonomic instability. Additional signs may include elevated creatine phosphokinase, myoglobinuria (rhabdomyolysis), and acute renal failure.
If NMS is suspected, immediately discontinue Lybalvi and provide intensive symptomatic treatment and monitoring.
5.6 Drug Reaction with Eosinophilia and Systemic Symptoms
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS) has been reported with exposure to olanzapine, a component of Lybalvi [see Adverse Reactions (6.2)]. DRESS may present with a cutaneous reaction (such as rash or exfoliative dermatitis), eosinophilia, fever, and/or lymphadenopathy with systemic complications such as hepatitis, nephritis, pneumonitis, myocarditis, and/or pericarditis. DRESS is sometimes fatal. Discontinue Lybalvi if DRESS is suspected.
5.7 Metabolic Changes
Atypical antipsychotic drugs, including Lybalvi, have been associated with metabolic changes that include hyperglycemia, diabetes mellitus, dyslipidemia, and body weight gain [see Adverse Reactions (6.1)]. While all drugs in the class have been shown to produce some metabolic changes, each drug has its own specific risk profile.
Hyperglycemia, in some cases extreme and associated with ketoacidosis or hyperosmolar coma or death, has been reported in patients treated with atypical antipsychotics. Any patient treated with Lybalvi should be monitored for symptoms of hyperglycemia including polydipsia, polyuria, polyphagia, and weakness. Patients who develop symptoms of hyperglycemia during treatment with Lybalvi should undergo fasting blood glucose testing. In some cases, hyperglycemia has resolved when the atypical antipsychotic was discontinued; however, some patients required anti-diabetic treatment despite discontinuation of the suspect drug. Patients starting treatment with Lybalvi should undergo fasting blood glucose testing at the beginning of treatment and periodically during treatment.
Antipsychotics have caused adverse alterations in lipids. Patients starting treatment with Lybalvi should undergo fasting lipid profile testing at the beginning of treatment and periodically during treatment.
Weight gain has been observed with use of antipsychotics. Monitor weight prior to initiating Lybalvi and frequently thereafter.
5.8 Tardive Dyskinesia
Tardive dyskinesia, a syndrome consisting of potentially irreversible, involuntary, dyskinetic movements, may develop in patients treated with antipsychotic drugs. The risk appears to be highest among the elderly, especially elderly women, but it is not possible to predict which patients are likely to develop the syndrome. Whether antipsychotic drug products differ in their potential to cause tardive dyskinesia is unknown.
The risk of developing tardive dyskinesia and the likelihood that it will become irreversible increases with the duration of treatment and the cumulative dose. The syndrome can develop after a relatively brief treatment period, even at low doses. It may also occur after discontinuation of treatment.
Tardive dyskinesia may remit, partially or completely, if antipsychotic treatment is discontinued. Antipsychotic treatment itself, however, may suppress (or partially suppress) the signs and symptoms of the syndrome, possibly masking the underlying process. The effect of symptomatic suppression on the long-term course of the syndrome is unknown.
Given these considerations, Lybalvi should be prescribed in a manner that is most likely to reduce the risk of tardive dyskinesia. Chronic antipsychotic treatment should generally be reserved for patients: 1) who suffer from a chronic illness that is known to respond to antipsychotic drugs; and 2) for whom alternative, effective, but potentially less harmful treatments are not available or appropriate. In patients who do require chronic treatment, use the lowest dose and the shortest duration of treatment producing a satisfactory clinical response should be sought. Periodically reassess the need for continued treatment.
If signs and symptoms of tardive dyskinesia appear in a patient on Lybalvi, drug discontinuation should be considered. However, some patients may require treatment with Lybalvi despite the presence of the syndrome.
5.9 Orthostatic Hypotension and Syncope
Atypical antipsychotics cause orthostatic hypotension and syncope. Generally, the risk is greatest during initial dose titration and when increasing the dose. In the 4-week, placebo-controlled study, from analysis of the vital signs data, rates of orthostatic hypotension were less than 2% in Lybalvi- and placebo-, and olanzapine-treated patients. In the 24-week, olanzapine-controlled study, from analysis of the vital signs data, rates of orthostatic hypotension in Lybalvi-treated patients were 3.7%, compared to 0.4% in olanzapine-treated patients.
Monitor orthostatic vital signs in patients who are vulnerable to hypotension (e.g., elderly patients, patients with dehydration, hypovolemia, concomitant treatment with antihypertensive medications or CNS depressants [see Drug Interactions (7.1, 7.2)], patients with known cardiovascular disease (history of myocardial infarction, ischemic heart disease, heart failure, or conduction abnormalities), and patients with cerebrovascular disease. Lybalvi has not been evaluated in patients with a recent history of myocardial infarction or unstable cardiovascular disease. Such patients were excluded from the premarketing clinical trials.
5.10 Falls
Antipsychotics, including Lybalvi, may cause somnolence, postural hypotension, motor and sensory instability, which may lead to falls and, consequently, fractures or other injuries. For patients with diseases, conditions, or medications that could exacerbate these effects, complete fall risk assessments when initiating antipsychotic treatment and recurrently for patients on longterm antipsychotic therapy.
5.11 Leukopenia, Neutropenia, and Agranulocytosis
Leukopenia and neutropenia have been reported during treatment with antipsychotic agents, including Lybalvi [see Adverse Reactions (6.1)]. Agranulocytosis (including fatal cases) has been reported with other agents in this class.
Possible risk factors for leukopenia and neutropenia include pre-existing low white blood cell count (WBC) or absolute neutrophil count (ANC) and history of drug-induced leukopenia or neutropenia. In patients with a pre-existing low WBC or ANC or a history of drug-induced leukopenia or neutropenia, perform a complete blood count (CBC) frequently during the first few months of therapy. In such patients, consider discontinuation of Lybalvi at the first sign of a clinically significant decline in WBC in the absence of other causative factors.
Monitor patients with clinically significant neutropenia for fever or other symptoms or signs of infection and treat promptly if such symptoms or signs occur. Discontinue Lybalvi in patients with severe neutropenia (absolute neutrophil count <1000/mm3) and follow their WBC until recovery.
5.12. Dysphagia
Esophageal dysmotility and aspiration have been associated with antipsychotic drug use. Antipsychotic drugs, including Lybalvi, should be used cautiously in patients at risk for aspiration.
5.13 Seizures
Like other antipsychotic drugs, Lybalvi may cause seizures. This risk is greatest in patients with a history of seizures or with conditions that lower the seizure threshold. Conditions that lower the seizure threshold may be more prevalent in older patients.
5.14. Potential for Cognitive and Motor Impairment
Lybalvi, like other antipsychotics, may cause somnolence and has the potential to impair judgment, thinking, or motor skills. In a Lybalvi placebo-controlled study, somnolence occurred in 9% of Lybalvi-treated patients compared to 2.2% in patients treated with placebo.
Patients should be cautioned about operating hazardous machinery, including motor vehicles, until they are reasonably certain that Lybalvi therapy does not affect them adversely.
5.15. Body Temperature Dysregulation
Atypical antipsychotics may disrupt the body’s ability to reduce core body temperature. Strenuous exercise, exposure to extreme heat, dehydration, and anticholinergic medications may contribute to an elevation in core body temperature; use Lybalvi with caution in patients who may experience these conditions.
5.16. Anticholinergic (Antimuscarinic) Effects
Olanzapine, a component of Lybalvi, exhibits in vitro muscarinic receptor affinity [see Clinical Pharmacology (12.2)]. In premarketing clinical trials with oral olanzapine, olanzapine was associated with constipation, dry mouth, and tachycardia, all adverse reactions possibly related to cholinergic antagonism. Such adverse reactions were not often the basis for discontinuations, but Lybalvi should be used with caution in patients with a current diagnosis or prior history of urinary retention, clinically significant prostatic hypertrophy, constipation, or a history of paralytic ileus or related conditions. In postmarketing experience, the risk for severe adverse reactions (including fatalities) was increased with concomitant use of anticholinergic medications [see Drug Interactions (7.1)].
5.17. Hyperprolactinemia
As with other drugs that antagonize dopamine D2 receptors, olanzapine, a component of Lybalvi, elevates prolactin levels, and the elevation can persist during chronic administration. Hyperprolactinemia may suppress hypothalamic GnRH, resulting in reduced pituitary gonadotropin secretion. This, in turn, may inhibit reproductive function by impairing gonadal steroidogenesis in both female and male patients. Galactorrhea, amenorrhea, gynecomastia, and impotence have been reported in patients receiving prolactin-elevating compounds.
Long-standing hyperprolactinemia when associated with hypogonadism may lead to decreased bone density in both female and male subjects.
Tissue culture experiments indicate that approximately one-third of human breast cancers are prolactin-dependent in vitro, a factor of potential importance if the prescription of these drugs is considered in a patient with previously-detected breast cancer. As is common with compounds which increase prolactin release, an increase in mammary gland neoplasia was observed in the olanzapine carcinogenicity studies conducted in mice and rats [see Nonclinical Toxicology (13.1)]. Neither clinical studies nor epidemiologic studies conducted to date have shown an association between chronic administration of this class of drugs and tumorigenesis in humans, but the available evidence is too limited to be conclusive.
In the 4-week placebo-controlled trial, shifts from normal to high prolactin values (>30 ng/mL for females; >20 ng/mL for males) occurred in 41.4% of females and 32.9% of males treated with Lybalvi, in 56.1% of females and 37.1% of males treated with olanzapine, and in 10% of females and 4.8% of males treated with placebo [see Use in Specific Populations (8.3)].
In the 24-week, olanzapine-controlled study, shifts from normal to high prolactin values occurred in 32.9% of females and 22.5% of males treated with Lybalvi, and in 41.7% of females and 28.5% of males treated with olanzapine.
5.18. Risks Associated with Combination Treatment with Lithium or Valproate
If Lybalvi is administered with lithium or valproate, refer to the lithium or valproate Prescribing Information for a description of the risks for these products including, but not limited to, the warnings and precautions for lithium or valproate [see Contraindications (4)].
Adverse reactions
The following adverse reactions are discussed in detail in other sections of the labeling:
- Increased Mortality in Elderly Patients with Dementia-related Psychosis [see Boxed Warning, Warnings and Precautions (5.1)]
- Cerebrovascular Adverse Reactions, Including Stroke, in Elderly Patients with Dementia-Related Psychosis [see Warnings and Precautions (5.2)]
- Precipitation of Opioid Withdrawal in Patients Who Are Dependent on Opioids [see
- Warnings and Precautions (5.3)]
- Vulnerability to Life-Threatening Opioid Overdose [see Warnings and Precautions (5.4)]
- Neuroleptic Malignant Syndrome [see Warnings and Precautions (5.5)]
- Drug Reaction with Eosinophilia and Systemic Symptoms [see Warnings and Precautions (5.6)]
- Metabolic Changes [see Warnings and Precautions (5.7)]
- Tardive Dyskinesia [see Warnings and Precautions (5.8)]
- Orthostatic Hypotension and Syncope [see Warnings and Precautions (5.9)]
- Falls [see Warnings and Precautions (5.10)]
- Leukopenia, Neutropenia, and Agranulocytosis [see Warnings and Precautions (5.11)]
- Dysphagia [see Warnings and Precautions (5.12)]
- Seizures [see Warnings and Precautions (5.13)]
- Potential for Cognitive and Motor Impairment [see Warnings and Precautions (5.14)]
- Body Temperature Regulation [see Warnings and Precautions (5.15)]
- Anticholinergic (Antimuscarinic) Effects [see Warnings and Precautions (5.16)]
- Hyperprolactinemia [see Warnings and Precautions (5.17)]
- Risks Associated with Combination Treatment with Lithium or Valproate [see Warnings and Precautions (5.18)]
6.1 Clinical Studies Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
Adverse Reactions in Patients with Schizophrenia
Patient exposure
The safety of Lybalvi was evaluated in 1262 patients (18 to 67 years of age) diagnosed with schizophrenia in four double-blind, controlled studies and three long-term safety extension studies of up to 3 years of duration. This experience corresponds to approximately 910 person- years. In these studies, there were a total of 663 patients exposed to Lybalvi for at least 6 months, and 386 patients for at least one year.
Adverse reactions in the short-term (4 week) placebo-controlled trial in adults with schizophrenia
The most common adverse reactions (incidence of at least 5% of patients exposed to Lybalvi and greater than twice the rate of placebo) are weight increased, somnolence, dry mouth, and headache.
Adverse reactions associated with the use of Lybalvi (incidence of 2% or greater and greater than in placebo-treated patients) are shown in Table 2.
Table 2: Adverse Reactions Reported in ≥2% of Lybalvi-Treated Patients and Greater than Placebo in a 4-Week Schizophrenia Trial
| Adverse reaction |
Placebo |
Lybalvi |
| Weight increased | 3 | 19 |
| Somnolence | 2 | 9 |
| Dry mouth | 1 | 7 |
| Headache | 3 | 6 |
| Blood insulin increased | 1 | 3 |
| Sedation | 0 | 2 |
| Dizziness | 1 | 2 |
| Neutrophil count decreased | 0 | 2 |
Adverse reactions that led to discontinuation in Lybalvi-treated patients in the short-term placebo-controlled trial in adults with schizophrenia include schizophrenia (1%) and abnormal liver function tests (1%).
Adverse reactions in the long-term (24-week), active-controlled trial in adults with schizophrenia
In the 24-week, olanzapine-controlled trial in patients with stable schizophrenia, adverse reactions associated with the use of Lybalvi (incidence of 2% or greater) include: weight increased (25%), somnolence (21%), dry mouth (13%), increased appetite (11%), waist circumference increased (6%), blood creatine phosphokinase increased (5%), headache (4%), lethargy (4%), sedation (4%), akathisia (3%), alanine aminotransferase increased (3%), aspartate aminotransferase increased (3%), constipation (3%), dizziness (3%), fatigue (3%), nausea (3%), blood pressure increased (3%), neutrophil count decreased (3%), blood insulin increased (2%), weight decreased (2%), and dyslipidemia (2%).
Adverse reactions that led to Lybalvi treatment discontinuation in more than one patient include somnolence (2%), weight increased (2%), neutropenia (2%), glycosylated hemoglobin increased (1%), schizophrenia (1%), and liver function test abnormal (1%).
Hyperglycemia
Mean increases in blood glucose have been observed in patients treated (median exposure of 9.2 months) with olanzapine in phase 1 of the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE). The mean increase of serum glucose (fasting and nonfasting samples) from baseline to the average of the 2 highest serum concentrations was 15.0 mg/dL. Hyperglycemia, as defined by fasting glucose ≥126 mg/dL, has been observed in patients treated with Lybalvi.
In the 4-week placebo-controlled trial in adult patients with schizophrenia, shifts in fasting glucose from normal to high occurred in 4% of patients treated with Lybalvi, 1% of patients treated with olanzapine, and no patients treated with placebo.
In the 24-week olanzapine-controlled trial, patients treated with Lybalvi were more likely to experience abnormal shifts in glycemic parameters than patients treated with olanzapine
Table 3: Changes in Glycemic Parameters in a 24-Week trial of Patients with Schizophrenia
| Lybalvi | Olanzapine | |
| Proportion of patients with shifts, % (n/N)* | ||
|
Glucose |
12 (26/223) | 8 (18/219) |
|
Impaired (>100 mg/dL and <126 mg/dL) to High (≥126 mg/dL) |
24 (9/38) | 11 (5/47) |
| Increase >10 mg/dL | 66 (174/265) | 57 (154/270) |
|
Hemoglobin A1c |
42 (86/204) | 35 (68/197) |
| Normal to High (<5.7% to ≥6.5%) | 0.5 (1/204) | 1.5 (3/197) |
| Impaired (>5.7% and <6.5%) to High (>6.5%) | 9.5 (6/63) | 9.2 (7/76) |
* n: number of patients with reported abnormal shifts; N: number of patients who had assessments at both baseline and endpoint for mean change, or normal at baseline and at least 1 post-baseline assessment for shift.
Dyslipidemia
In the 4-week, placebo-controlled trial in adult patients with schizophrenia, shifts in fasting triglycerides from normal to high occurred in 14% of patients treated with Lybalvi and 4% of patients treated with placebo.
In the 24-week olanzapine-controlled study, mean changes in fasting total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides were similar in patients treated with Lybalvi and in patients treated with olanzapine.
Weight Gain
In the 4-week placebo-controlled study in adult patients with schizophrenia, mean changes in weight, and proportion of patients with ≥7% weight increase, were greater in patients treated with Lybalvi and olanzapine than in patients on placebo. In that study, mean weight gain was 3.0 kg in patients treated with Lybalvi, 2.4 kg in patients treated with olanzapine, and 0.2 kg in patients treated with placebo. The proportion of patients with ≥7% weight increase was 26% in patients treated with Lybalvi, 20% in patients treated with olanzapine, and 5% in patients treated with placebo.
In the 24-week trial, Lybalvi-treated patients gained on average 4.2% of baseline body weight. The proportion of patients treated with Lybalvi with ≥10% body weight gain was 17.8% [see Clinical Studies (14)].
Extrapyramidal Symptoms
In the 4-week placebo-controlled trial in adult patients with schizophrenia, patients were assessed using the Simpson-Angus Rating Scale (SAS) for extrapyramidal symptoms (EPS)
(total score ranges from 1 to 14), the Barnes Akathisia Rating Scale (BARS) for akathisia (total score ranges from 0 to 14), and the Abnormal Involuntary Movement Scale (AIMS) for dyskinesias (total score ranges from 0 to 28). The mean changes from baseline to last study visit for the SAS, BARS, and AIMS was similar in Lybalvi-treated patients and in placebo-treated patients. The mean changes for Lybalvi- vs placebo-treated patients were 0.00 vs -0.2 for AIMS, 0.0 vs -0.1 for BARS, and 0.0 vs -0.3 for SAS, respectively. The rate of parkinsonism (SAS total score >3) was lower in patients treated with Lybalvi (4%) compared to those on placebo (10%). The rates of akathisia (BARS global clinical assessment score ≥2) and dyskinesia (AIMS score ≥3 on any of the first 7 items, or a score ≥2 on two or more of any of the first 7 items) were similar in patients treated with Lybalvi and in those on placebo. Rates of akathisia were 6.0% and 8.2% in patients treated with Lybalvi and placebo, respectively, and the rate of dyskinesia was 1.5% both in Lybalvi-treated and in placebo-treated patients.
The frequency of reported adverse reactions related to extrapyramidal symptoms, including akathisia, restlessness, muscle spasms, bradykinesia, tremor, extrapyramidal disorder, and parkinsonism was 2% both in Lybalvi-treated and in placebo-treated patients.
In the 24-week active-controlled trial, the mean change from baseline to the last visit for the SAS, BARS, and AIMS was similar in Lybalvi-treated patients and in those treated with the active control. Extrapyramidal adverse reactions, including parkinsonism, akathisia, and dyskinesia, had a similar incidence in Lybalvi-treated patients and in those treated with the active control: any extrapyramidal symptom was 8%, akathisia was 3%.
Dystonia
Symptoms of dystonia, (prolonged abnormal contractions of muscle groups) may occur in susceptible individual ls during the first few days of treatment. Dystonic symptoms include: spasm of the neck muscles, sometimes progressing to tightness of the throat, swallowing difficulty, difficulty breathing, and/or protrusion of the tongue. Although these symptoms can occur at low doses, they occur more frequently and with greater severity with high potency and at higher doses of first-generation antipsychotic drugs. An elevated risk of acute dystonia is observed in males and younger age groups.
Adverse Reactions in Patients with Bipolar Disorder
The safety of Lybalvi for the treatment of bipolar I disorder (mixed or manic) monotherapy and adjunct to lithium or valproate relies on information from adequate and well-controlled studies of olanzapine tablets in bipolar I disorder.
The most common adverse reactions (incidence of at least 5% of patients exposed to olanzapine and greater than or equal to twice the rate of placebo) from short-term trials of olanzapine (manic or mixed episodes) are somnolence, dry mouth, dizziness, asthenia, constipation, dyspepsia, increased appetite, and tremor.
The most common adverse reactions (incidence of at least 5% of patients exposed to olanzapine and greater than or equal to twice the rate of placebo) from short-term trials of olanzapine as adjunct to lithium or valproate (manic or mixed episodes) are dry mouth, weight gain, increased appetite, dizziness, back pain, constipation, speech disorder, increased salivation, amnesia, paresthesia.
6.2. Postmarketing Experience
The following adverse reactions have been identified during post-approval use of olanzapine. Because these reactions are reported voluntarily from a population of uncertain size, it is difficult to reliably estimate their frequency or evaluate a causal relationship to drug exposure.
- allergic reactions (e.g., anaphylactoid reaction, angioedema, pruritus or urticaria)
- cholestatic or mixed liver injury, hepatitis, jaundice
- diabetic coma, diabetic ketoacidosis
- discontinuation reaction (diaphoresis, nausea or vomiting)
- Drug reaction with eosinophilia and systemic symptoms (DRESS)
- hyperlipidemia (random cholesterol levels of ≥240 mg/dL and random triglyceride levels of ≥1000 mg/dL have been reported)
- neutropenia
- pancreatitis
- priapism
- rash
- restless legs syndrome
- rhabdomyolysis
- salivary hypersecretion
- stuttering1
- venous thromboembolic events (including pulmonary embolism and deep venous thrombosis)
1 Stuttering was only studied in oral and long acting injection (LAI) formulations.
Drug interactions
7.1. Effects of Other Drugs on Lybalvi
Table 4 describes clinically significant drug interactions where the concomitant use of other drugs affects Lybalvi.
Table 4: Effects of Other Drugs on Lybalvi
| Strong CYP3A4 Inducer | |
| Clinical Implication: | Coadministration of Lybalvi with a strong CYP3A4 inducer decreases AUCinf of olanzapine and samidorphan [see Clinical Pharmacology (12.3)], which may reduce Lybalvi efficacy |
|
Prevention or Management: |
Concomitant use of Lybalvi with strong CYP3A4 inducers is not recommended. |
|
Strong CYP1A2 Inhibitor |
|
|
Clinical Implication: |
Concomitant use of Lybalvi with a strong CYP1A2 inhibitor increases olanzapine AUC and Cmax [see Clinical Pharmacology (12.3)], which may increase the risk of Lybalvi adverse reactions. |
|
Prevention or Management: |
Consider reducing the dosage of the olanzapine component in Lybalvi when used concomitantly with strong CYP1A2 inhibitors. |
|
CYP1A2 Inducer |
|
|
Clinical Implication: |
Concomitant use of Lybalvi with CYP1A2 inducers decreases olanzapine exposure [see Clinical Pharmacology (12.3)], which may reduce Lybalvi efficacy. |
|
Prevention or Management: |
Consider increasing the dosage of the olanzapine component in Lybalvi when used concomitantly with CYP1A2 inducers. |
|
Diazepam, Alcohol, and Other CNS Acting Drugs |
|
|
Clinical Implication: |
Concomitant use of diazepam, alcohol, or other CNS acting drugs with Lybalvi may potentiate the orthostatic hypotension observed with olanzapine [see Warnings and Precautions (5.9)]. |
|
Prevention or Management: |
Lybalvi should be used with caution in patients receiving concomitantly diazepam or other CNS acting drugs, or using alcohol. |
|
Anticholinergic Drugs |
|
|
Clinical Implication: |
Concomitant treatment with olanzapine and other drugs with anticholinergic activity can increase the risk for severe gastrointestinal adverse reactions related to hypomotility. |
|
Prevention or Management: |
Lybalvi should be used with caution in patients receiving medications having anticholinergic (antimuscarinic) effects [see Warnings and Precautions (5.16)]. |
7.2. Effects of Lybalvi on Other Drugs
Table 5 describes clinically significant drug interactions where concomitant use of Lybalvi affects other drugs.
Table 5: Effects of Lybalvi on Other Drugs
|
Antihypertensive Agents |
|
|
Clinical Implication: |
Lybalvi may enhance the effects of certain antihypertensive agents. |
|
Prevention or Management: |
Monitor blood pressure and reduce dosage of antihypertensive drug in accordance with its approved product labeling. |
| Levodopa and Dopamine Agonists | |
| Clinical Implication: | Lybalvi may antagonize the effects of levodopa and dopamine agonists. |
| Prevention or Management: | Concomitant use of Lybalvi is not recommended with levodopa and dopamine agonists. |
7.3. Opioids
Lybalvi is contraindicated in patients who are using opioids or undergoing acute opioid withdrawal [see Contraindications (4)].
Lybalvi increases the risk of precipitating acute opioid withdrawal in patients who are dependent on opioids. Prior to initiating Lybalvi, there should be at least a 7-day opioid-free interval from the last use of short-acting opioids, and at least a 14-day opioid-free interval from the last use of long-acting opioids [see Dosage and Administration (2.1), Warnings and Precautions (5.3)].
In emergency situations, if a Lybalvi-treated patient requires opioid treatment for anesthesia or analgesia, discontinue Lybalvi. The opioid should be administered by properly trained individua l(s), and the patient should be properly monitored in a setting equipped and staffed for cardiopulmonary resuscitation [see Warnings and Precautions (5.4)].
In non-emergency situations, if a Lybalvi-treated patient is expected to require opioid treatment (e.g., for analgesia during or after an elective surgical procedure) discontinue Lybalvi at least 5 days before opioid treatment and start olanzapine or another antipsychotic, if needed.
Given that Lybalvi contains samidorphan, an opioid antagonist, opioid treatment may be less effective or ineffective shortly after Lybalvi discontinuation because of the presence of samidorphan.
Use in specific populations
8.1. Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to atypical antipsychotics, including Lybalvi, during pregnancy. Healthcare providers are encouraged to register patients by contacting the National Pregnancy Registry for Atypical Antipsychotics at 1-866-961-2388 or visit
https://womensmentalhealth.org/research/pregnanc yregistry/atypicalantipsyc hotic/.
Risk Summary
Neonates exposed to antipsychotic drugs, including the olanzapine component of Lybalvi, during the third trimester are at risk for extrapyramidal and/or withdrawal symptoms following delivery (see Clinical Considerations). Overall published epidemiologic studies of pregnant women exposed to olanzapine have not established a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes (see Data). There are no available data on the use of samidorphan or the combination of olanzapine and samidorphan in pregnant women to determine a drug-associated risk of major birth defects, miscarriage or adverse maternal or fetal outcomes. There are risks to the mother associated with untreated schizophrenia or bipolar I disorder and with exposure to antipsychotics, including Lybalvi, during pregnancy (see Clinical Considerations).
Lybalvi
In an animal reproduction study, oral administration of olanzapine and samidorphan to pregnant rats during the period of organogenesis produced adverse effects on embryofetal development and fetal toxicity at maternally toxic doses that are 6 times and >400 times the maximum recommended human dose (MRHD) of 20 mg/10 mg olanzapine/samidorphan in Lybalvi, respectively based on AUC. There were no adverse effects on embryofetal development at doses of olanzapine and samidorphan that are approximately 1 and 80 times, respectively, the MRHD based on AUC (see Data).
Olanzapine
In animal reproduction studies, there was no evidence of malformations in rats or rabbits when orally administered olanzapine at doses up to 9 and 30 times the MRHD dose (20 mg) based on mg/m2 body surface area, respectively. In an oral rat embryofetal developmental toxicity study, early resorptions and increased numbers of nonviable fetuses were observed at a dose 9 times the MRHD based on mg/m2 body surface area and gestation was prolonged at 5 times the MRHD based on mg/m2 body surface area. In an oral rabbit embryofetal developmental toxicity study, fetal toxicity (manifested as increased resorptions and decreased fetal weight) occurred at a maternally toxic dose of olanzapine which is 30 times the MRHD based on mg/m2 body surface area (see Data).
Samidorphan
In animal reproduction studies, oral administration of samidorphan to pregnant rats and rabbits during the period of organogenesis caused fetal toxicities in rats only at maternally toxic doses that are >248 times the human exposure at the MRHD of 10 mg/day based on AUC. Oral administration of samidorphan to pregnant rats during pregnancy and lactation resulted in lower pup survival and decreased pup weights at 188 times the human exposure at the MRHD based on AUC (see Data).
The estimated background risk of major birth defects and miscarriage for the indicated populations is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Disease-Associated Maternal and/or Embryofetal Risk
There is risk to the mother from untreated schizophrenia or bipolar I disorder, including increased risk of relapse, hospitalization and suicide. Schizophrenia and bipolar I disorder are associated with increased adverse perinatal outcomes, including preterm birth. It is not known if this is a direct result of the illness or other comorbid factors.
Fetal/ Neonatal Risks
Extrapyramidal and/or withdrawal symptoms, including agitation, hypertonia, hypotonia, tremor, somnolence, respiratory distress and feeding disorder have been reported in neonates who were exposed to antipsychotic drugs, including the olanzapine component of Lybalvi, during the third trimester of pregnancy. These symptoms have varied in severity. Monitor neonates for extrapyramidal and/or withdrawal symptoms and manage symptoms appropriately. Some neonates recovered within hours or days without specific treatment; others required prolonged hospitalization.
Human Data
Published data from observational studies, birth registries, and case reports on the use of atypical antipsychotics during pregnancy do not report a clear association with antipsychotics and major birth defects. A retrospective cohort study from a Medicaid database of 9258 women exposed to antipsychotics during pregnancy did not indicate an overall increased risk for major birth defects.
Animal Data
Lybalvi
Olanzapine and samidorphan were orally administered to pregnant rats during the period of organogenesis at doses of 0.5/10, 2/50, 6/200, and 0/200 mg/kg/day (olanzapine/samidorphan) which are approximately <1/10 times to 6/448 times the MRHD of 20 mg/10 mg, olanzapine/samidorphan, respectively, based on AUC. Maternal toxicity consisting of decreased body weight and food consumption was observed at all dose levels.
Administration of samidorphan alone (200 mg/kg/day) and 6/200 mg/kg/day olanzapine/samidorphan decreased mean fetal body weights, increased litter incidence of bent ribs and bent scapula; however, the incidence of bent scapula and bent ribs was not increased when samidorphan was administered in combination with olanzapine compared to the incidence with samidorphan alone. Administration of olanzapine/samidorphan at 6/200 mg/kg/day also increased resorptions and post-implantation loss, with correlating lower mean viable fetuses and litter size. The no observed adverse effect level (NOAEL) for embryofetal development is 2/50 mg/kg/day, which is approximately 1/80 times the MRHD of 20 mg/10 mg olanzapine/samidorphan respectively, based on AUC.
Olanzapine
Olanzapine was orally administered to pregnant rats and rabbits during the period of organogenesis at doses up to 18 mg/kg/day in rats and at doses up to 30 mg/kg/day in rabbits (9 times and 30 times the MRHD of 20 mg/day based on mg/m2 body surface area, respectively), and no evidence of malformations was observed. In an oral rat embryofetal developmental toxicity study, early resorptions and increased numbers of nonviable fetuses were observed at a dose of 18 mg/kg/day (9 times the MRHD based on mg/m2 body surface area). Gestation was prolonged at 10 mg/kg/day (5 times the MRHD based on mg/m2 body surface area). In an oral rabbit embryofetal developmental toxicity study, fetal toxicity (manifested as increased resorptions and decreased fetal weight) occurred at a maternally toxic dose of olanzapine at 30 mg/kg/day (30 times the MRHD based on mg/m2 body surface area).
Samidorphan
Samidorphan was orally administered to pregnant rats during the period of organogenesis at doses of 25, 100, and 300 mg/kg/day, which are approximately 29 to 742 times the MRHD of 10 mg/day based on AUC. Samidorphan was associated with an increased incidence of skeletal variations (unossified sternebrae and bent ribs) at maternally toxic doses of ≥100 mg/kg/day, and skeletal malformations (bent or misshapen forelimbs, hindlimbs, and/or scapula) at 300 mg/kg/day which are >248 and 742 times the MRHD based on AUC, respectively. The NOAEL for embryofetal development is 25 mg/kg/day, which is approximately 29 times the MRHD based on AUC.
Samidorphan did not cause adverse effects on embryofetal development when orally administered to pregnant rabbits during the period of organogenesis at doses of 10, 30, and 90 mg/kg/day, which are up to approximately 143 times the MRHD based on AUC.
Samidorphan was orally administered to pregnant rats during pregnancy and lactation at doses of 10, 30, or 100 mg/kg/day, which are approximately 7 to 188 times the MRHD based on AUC. Reduced pup survival, lower birth weights, and decreased pup body weight gains were observed at 100 mg/kg/day, which is 188 times the MRHD based on AUC. The NOAEL of 30 mg/kg/day is approximately 36 times the MRHD based on AUC. There were no adverse effects on pup developmental landmarks, learning, memory, reflexes, or fertility.
8.2. Lactation
Risk Summary
Olanzapine is present in human milk. There are reports of excess sedation, irritability, poor feeding and extrapyramidal symptoms (tremors and abnormal muscle movements) in infants exposed to olanzapine through breast milk. There is no information on the effects of olanzapine on milk production. There are no data on the presence of samidorphan or the combination of olanzapine and samidorphan in human milk, the effects on the breastfed infant or the effects on milk production. When samidorphan was administered to lactating rats, samidorphan and a metabolite were detected in the plasma of nursing pups, likely due to the presence of samidorphan in milk. Infants exposed to Lybalvi should be monitored for excess sedation, irritability, poor feeding and extrapyramidal symptoms (tremors and abnormal muscle movements).
The development and health benefits of breastfeeding should be considered along with the mother's clinical need for Lybalvi and any potential adverse effects on the breastfed infant from Lybalvi or from the underlying maternal condition.
8.3. Females and Males of Reproductive Potential
Infertility
Females
Based on the pharmacologic action of olanzapine (D2 antagonism), treatment with Lybalvi may result in an increase in serum prolactin levels, which may lead to a reversible reduction in fertility in females of reproductive potential [see Warnings and Precautions (5.17)].
8.4. Pediatric Use
The safety and effectiveness of Lybalvi have not been established in pediatric patients.
8.5. Geriatric Use
Clinical studies of Lybalvi did not include sufficient numbers of patients 65 years of age and older to determine whether they responded differently than younger adult patients.
Olanzapine
Of the 2,500 patients in premarketing clinical studies with orally administered olanzapine, 11% (263) were 65 years of age or over. Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Lybalvi is not approved for the treatment of patients with dementia-related psychosis [see Dosage and Administration (2.5), Warnings and Precautions (5.1)].
Studies in elderly patients with dementia-related psychosis have suggested that there may be a different tolerability profile in this population compared to younger patients with schizophrenia. Elderly patients with dementia-related psychosis treated with olanzapine are at an increased risk of death compared to placebo.
- In placebo-controlled studies of olanzapine in elderly patients with dementia-related psychosis, there was a higher incidence of cerebrovascular adverse events (e.g., stroke, transient ischemic attack) in patients treated with olanzapine, compared to patients treated with placebo.
- In five placebo-controlled studies of olanzapine in elderly patients with dementia- related psychosis (n=1,184), the following adverse reactions were reported in olanzapine-treated patients at an incidence of at least 2% and significantly greater than in placebo-treated patients: falls, somnolence, peripheral edema, abnormal gait, urinary incontinence, lethargy, increased weight, asthenia, pyrexia, pneumonia, dry mouth and visual hallucinations. The rate of discontinuation due to adverse reactions was greater with olanzapine than with placebo (13% vs 7%).
Consider a lower dosage of the olanzapine component of Lybalvi in geriatric patients who may have decreased clearance or an exaggerated pharmacodynamic response to olanzapine (e.g., oversedation) [see Dosage and Administration (2.5)].
8.6. Hepatic Impairment
Olanzapine and samidorphan plasma exposures were found to be higher in subjects with moderate hepatic impairment than in subjects with normal hepatic function. The effect of severe hepatic impairment was not studied. The higher plasma exposure in patients with moderate
hepatic impairment was not expected to be clinically relevant. No dose adjustment of Lybalvi is needed in patients with hepatic impairment [see Clinical Pharmacology (12.3)].
8.7. Renal Impairment
Plasma exposure to olanzapine and samidorphan was higher in patients with severe renal impairment (eGFR 15 to 29 mL/minute/1.73 m2) compared to those with normal renal function [see Clinical Pharmacology (12.3)]. No dose adjustment of Lybalvi is needed in patients with mild (eGFR 60 to 89 mL/minute/1.73 m2), moderate (eGFR 30 to 59 mL/minute/1.73 m2), or severe renal impairment (eGFR 15 to 29 mL/minute/1.73 m2).
The effect of Lybalvi in patients with end-stage renal disease was not studied. Lybalvi is not recommended for patients with end-stage renal disease (eGFR of <15 mL/minute/1.73 m2).
Overdosage
Human Experience
There is limited clinical experience with overdose with Lybalvi. In premarketing clinical trials of Lybalvi involving 861 patients, overdose of Lybalvi was identified in 7 patients. This included 4 patients with accidental overdose, 2 with intentional overdose, and 1 due to a medication administration error. None of the reported overdoses was associated with a fatal outcome. There was a reported ingestion of 11 tablets of Lybalvi 10 mg/10 mg (5.5 times and 11 times the maximum recommended daily dosage of the olanzapine and samidorphan components of Lybalvi, respectively). The patient was found unresponsive and admitted to the hospital. Medical treatment included fluids, electrolytes, a diuretic, and a detoxicant; the patient stabilized within 2 days.
In postmarketing reports of overdose with olanzapine, a component of Lybalvi, symptoms included agitation/aggressiveness, dysarthria, tachycardia, various extrapyramidal symptoms, and reduced level of consciousness ranging from sedation to coma. Less commonly reported symptoms include: aspiration, cardiopulmonary arrest, cardiac arrhythmias (such as supraventricular tachycardia and 1 patient experiencing sinus pause with spontaneous resumption of normal rhythm), delirium, possible neuroleptic malignant syndrome, respiratory depression/arrest, convulsion, hypertension, and hypotension. In 1 case of death, the amount of acutely ingested olanzapine was reported to be possibly as low as 450 mg; however, in another case, a patient was reported to survive an acute olanzapine ingestion of approximately 2,000 mg.
Management of Overdose
No specific antidotes for Lybalvi are known. In managing overdose, provide supportive care, including close medical supervision and monitoring, and consider the possibility of multiple drug involvement. If an overdose occurs, consult a certified Poison Control Center (1-800-222-1222) for additional overdosage management recommendations.
Description
Lybalvi is a combination of olanzapine, an atypical antipsychotic, and samidorphan (as samidorphan L-malate), an opioid antagonist.
Olanzapine is 2-methyl-4-(4-methyl-1-piperazinyl)-10H-thieno[2,3-b][1,5]be nzodia zepine. The molecular formula of olanzapine is: C17H20N4S and the molecular weight is 312.44 g/mol. It is a yellow crystalline powder and has pKa values of 7.80 and 5.44. The chemical structure is:
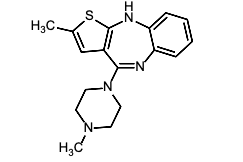
Samidorphan L-malate is morphinan-3-carboxamide, 17-(cyclopropylmethyl)-4, 14-dihydroxy- 6-oxo-, (2S)-2-hydroxybutanedioate. The molecular formula of samidorphan L-malate is C21H26N2O4 • C4H6O5 and the molecular weight is 504.54 g/mol. It is a white to off-white crystalline powder and has pKa values of 8.3 (amine) and 10.1 (phenol). The chemical structure is: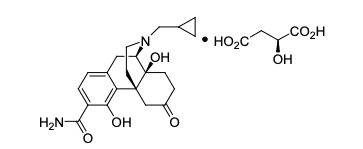
Lybalvi is intended for oral administration and is available as film-coated, bilayer tablets in the following strengths: 5 mg/10 mg, 10 mg/10 mg, 15 mg/10 mg, and 20 mg/10 mg of olanzapine and samidorphan (equivalent to 13.6 mg of samidorphan L-malate).
Inactive ingredients include colloida l silicon dioxide, crospovidone, lactose monohydrate, magnesium stearate, and microcrystalline cellulose. The film coating ingredients include hypromellose, titanium dioxide, triacetin, and color additives [iron oxide yellow (5 mg/10 mg); iron oxide yellow and iron oxide red (10 mg/10 mg); FD&C Blue No. 2/ indigo carmine aluminum lake (15 mg/10 mg); iron oxide red (20 mg/10 mg)].
Clinical pharmacology
12.1. Mechanism of Action
The mechanism of action of olanzapine is unclear; however, its efficacy in the treatment of schizophrenia or bipolar I disorder could be mediated through a combination of dopamine and serotonin type 2 (5HT2) antagonism.
The mechanism of action of samidorphan could be mediated through opioid receptor antagonism.
12.2. Pharmacodynamics
Olanzapine
Olanzapine binds with high affinity to the following receptors: serotonin 5HT2A/2C, 5HT6 (Ki=4, 11, and 5 nM, respectively), dopamine D1-4 (Ki=11–31 nM), histamine H1 (Ki=7 nM), and adrenergic α1 receptors (Ki=19 nM). Olanzapine is an antagonist with moderate affinity binding for serotonin 5HT3 (Ki=57 nM) and muscarinic M1-5 (Ki=73, 96, 132, 32, and 48 nM, respectively). Olanzapine binds with low affinity to GABAA, BZD, and β-adrenergic receptors (Ki>10 µM).
Samidorphan
Samidorphan binds to the mu-, kappa-, and delta-opioid receptors (Ki=0.052, 0.23, and 2.7 nM, respectively). Samidorphan is an antagonist at the mu-opioid receptors with partial agonist activity at kappa- and delta-opioid receptors.
The N-dealkylated major human metabolite binds to the mu-, kappa-, and delta-opioid receptors (Ki=0.26, 23, and 56 nM, respectively), and functions as a mu-opioid receptor agonist. The N-oxide major human metabolite binds to mu-, kappa-, and delta-opioid receptors (Ki=8, 110, and 280 nM, respectively) and functions as a mu-opioid receptor antagonist.
Cardiac Electrophysiology
At doses up to 30 mg/30 mg (1.5 times and 3 times the maximum recommended daily dosage of olanzapine and samidorphan, respectively), Lybalvi does not prolong QTc interval to any clinically relevant extent.
12.3. Pharmacokinetics
The pharmacokinetics of both olanzapine and samidorphan are linear over the clinical dose range and there is no PK interaction between olanzapine and samidorphan after oral administration of Lybalvi. Steady-state concentrations of olanzapine and samidorphan are reached within 7 days of commencement of once-daily administration of Lybalvi. The primary pharmacological activities of Lybalvi are due to the parent drugs, olanzapine and samidorphan.
Following a single dose administration of Lybalvi (10 mg olanzapine/10 mg samidorphan), the mean AUC0-inf and Cmax of olanzapine was 628 ng·h/mL and 16 ng/mL, respectively. The mean AUC0-inf and Cmax of olanzapine after 10 mg single dose administration of olanzapine tablet was 610 ng·h/mL and 16 ng/mL, respectively.
Pharmacokinetic properties of the components of Lybalvi are provided in Table 6.
Table 6: Pharmacokinetic Properties of the Components of Lybalvi
|
Parameters |
Olanzapine |
Samidorphan |
|
General |
||
|
Steady State Exposure (20 mg olanzapine/10 mg samidorphan) |
||
|
Cmax (ng/mL)a |
64.6 (28.9) |
45.1 (11.4) |
|
AUC24h (ng∙hr/mL)a |
1086 (556) |
364 (112) |
|
Time to reach steady state |
7 days |
5 days |
|
Accumulation at steady state |
2-fold |
1.3-fold |
|
Absorption |
||
|
Absolute oral bioavailability |
NA |
69% |
|
Tmax (h)b |
4.5–7 |
1–2 |
|
Effect of Food |
||
|
Cmax ratioc |
0.88 (0.82, 0.95) |
0.85 (0.76, 0.94) |
|
AUC ratioc |
0.93 (0.91, 0.96) |
1.03 (1.00, 1.05) |
|
Distribution |
||
|
Plasma protein binding |
93% |
23% - 33% |
|
Blood-to-plasma ratio |
Not Determined |
0.8 |
|
Elimination |
||
|
t1/2 (h)d |
35–52 |
7–11 |
|
CL/F (L/h)d |
15–22 |
35–45 |
|
Metabolism |
||
|
Primary pathway(s) |
UGT1A4, CYP1A2 |
CYP3A4 |
|
Minor pathway(s) |
CYP2D6 |
CYP3A5, CYP2C19, CYP2C8 |
|
Major circulating metabolites |
10-N-glucuronide and 4′-N- desmethyl-olanzapine. Both metabolites lack pharmacological activity at the therapeutic concentrations |
N-dealkylated and cis-N-oxide metabolites. Neither metabolite contributes to the pharmacological effects of samidorphan |
|
Excretion |
||
|
Primary route of elimination |
Metabolism |
Metabolism |
|
Urine (unchanged) |
7% |
18% |
|
Urine (unchanged + metabolites) |
57% |
67% |
|
Feces (unchanged + metabolites) |
30% |
16% |
Abbreviations: AUC24h=area under the concentration-time curve over the 24-hour dosing interval; Cmax=maximum plasma concentration; CYP=cytochrome P450; NA=not applicable; Tmax=time to Cmax; t½=terminal elimination half-life; UGT=Uridine 5'-diphospho-glucuronosyltransferase.
a. Presented as arithmetic mean (standard deviation).
b. Presented as range of the median across multiple studies.
c. Geometric mean ratio (90% confidence interval) [high fat meal/fasting]. High fat meal defined as meal containing approximately 900-1000 calories and 50% fat content. No clinically relevant food effect.
d. Presented as range of the mean across multiple studies.
Specific Populations
Geriatric Patients
The pharmacokinetics of olanzapine may be altered in geriatric patients [see Dosage and Administration (2.5), Use in Specific Populations (8.5)]. In a study involving 24 healthy subjects, the mean elimination half-life of olanzapine was about 1.5 times greater in elderly subjects (≥65 years) than in non-elderly subjects (<65 years).
No effect of age on samidorphan pharmacokinetics was found in a study involving 12 elderly [aged 66-80 years old (6 male, 6 female)] and 24 young [aged 18-39 years old (12 male, 12 female)] healthy subjects administered a single oral dose of 10 mg samidorphan.
Male and Female Patients
Clearance of olanzapine is approximately 30% lower in females than males. In clinical trials, however, there were no apparent differences between males and females in efficacy or adverse reactions. In clinical studies and population pharmacokinetic analysis, Lybalvi pharmacokinetics were consistent with that of olanzapine (as monotherapy) with no apparent effect of sex on samidorphan pharmacokinetics.
Racial or Ethnic Groups
In vivo studies of olanzapine as monotherapy have shown that olanzapine exposures are similar among Japanese, Chinese, and Caucasians, especially after normalization for body weight difference. A population pharmacokinetic analysis found that the clearance of olanzapine is greater in Black subjects (N=255) than non-Black subjects (N=329 White and N=17 other races), and that samidorphan pharmacokinetics are not affected by race.
Patients with Hepatic and Renal Impairment
Effects of hepatic and renal impairment on the exposure of olanzapine and samidorphan are summarized in Figure 1.
Figure 1: Effects of Hepatic Impairment and Renal Impairment on Olanzapine and Samidorphan Pharmacokinetics
* Based on PBPK simulations, the predicted Cmax and AUC ratios for samidorphan in subjects with severe hepatic impairment relative to healthy subjects were 2.1 and 2.3, respectively.
Smoking Status
Olanzapine clearance was approximately 40% higher in smokers than in non-smokers. Samidorphan pharmacokinetics were not affected by smoking.
Combined Effects
The combined effects of age, smoking, and sex could lead to substantial difference in olanzapine pharmacokinetics. The clearance of olanzapine in young smoking males, for example, may be 3 times higher than that in elderly nonsmoking females. Population pharmacokinetic analysis indicated that samidorphan pharmacokinetics was not affected by age, sex, race, and smoking status.
Drug Interaction Studies
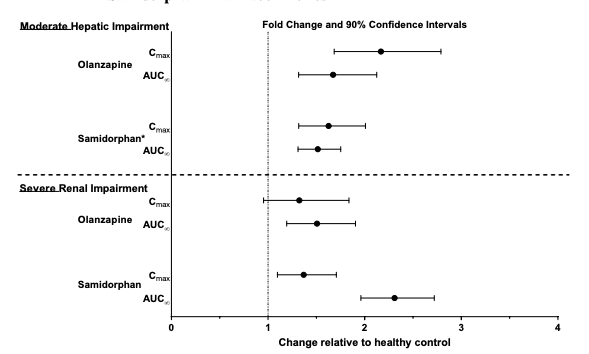
Effect of Other Drugs on Lybalvi
Coadministration of Lybalvi with rifampin, a strong CYP3A4 inducer, decreased the total systemic exposure (based on area under the concentration-time curve from time 0 extrapolated to infinity [AUCinf]) of olanzapine and samidorphan by 48% and 73%, respectively (Figure 2).
Fluvoxamine, a strong CYP1A2 inhibitor, decreases clearance of olanzapine. This results in a mean increase in olanzapine Cmax following fluvoxamine of 54% in female nonsmokers and 77% in male smokers. The mean increase in olanzapine AUC in female nonsmokers and male smokers is 52% and 108%, respectively.
Carbamazepine therapy (200 mg bid) causes an approximately 50% increased clearance of olanzapine. This increase is likely due to the fact that carbamazepine is a CYP1A2 inducer.
Based on PBPK simulations, Itraconazole, a strong CYP3A inhibitor, is predicted to increase samidorphan Cmax by 25% and AUC by 56%.
Figure 2: Effect of Other Drugs on Lybalvi
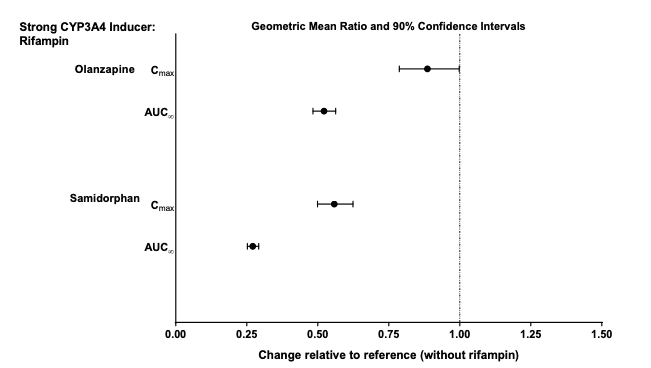
Effect of Lybalvi on Other Drugs
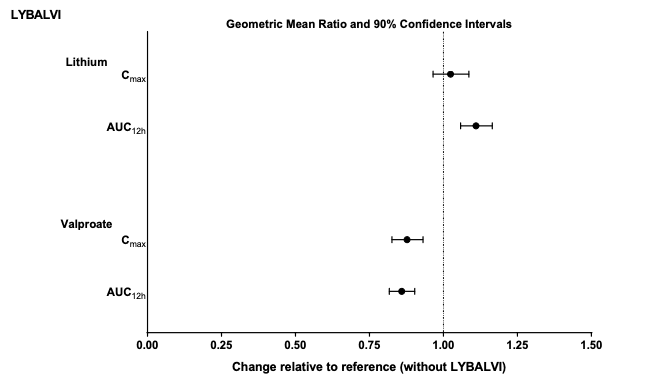
Coadministration of Lybalvi and lithium or valproate did not have a clinically significant effect on the PK of lithium or valproate (Figure 3). Based on these results, no dosage adjustment of lithium or valproate is necessary when coadministered with Lybalvi.
Figure 3: Effects of Lybalvi on Other Drugs
In vitro Studies
Cytochrome P450 (CYP) Enzymes: Olanzapine does not inhibit CYP1A2, CYP2C9, CYP2C19, CYP2D6, or CYP3A4/5. Samidorphan does not inhibit CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, or CYP3A4/5. Samidorphan does not induce CYP1A2, CYP2B6, or CYP3A4/5.
Transporter Systems: Samidorphan is not a substrate of P-glycoprotein (P-gp; multidrug resistance protein 1), organic anion transporter (OATP) 1B1, or OATP1B3. Samidorphan does not inhibit these transporters or breast cancer resistance protein (BCRP), organic anion transporter (OAT)1, OAT3, or organic cation transporter (OCT)2.
Nonclinical toxicology
13.1. Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Olanzapine
Oral carcinogenicity studies were conducted in mice and rats. Olanzapine was administered to mice in two 78-week studies at doses of 3, 10, 30/20 mg/kg/day (equivalent to 0.8 to 5 times the MRHD of 20 mg/day based on mg/m2 body surface area) and 0.25, 2, 8 mg/kg/day (equivalent to 0.06 to 2 times the MRHD based on mg/m2 body surface area). Rats were dosed for 2 years at doses of 0.25, 1, 2.5, 4 mg/kg/day (males) and 0.25, 1, 4, 8 mg/kg/day (females) (equivalent to 0.13 to 2 and 0.13 to 4 times the MRHD based on mg/m2 body surface area, respectively). The incidence of liver hemangiomas and hemangiosarcomas was significantly increased in 1 mouse study in female mice dosed at 8 mg/kg/day (2 times the MRHD based on mg/m2 body surface area). These tumors were not increased in another mouse study in females dosed at 10 or 30/20 mg/kg/day (2 to 5 times the MRHD based on mg/m2 body surface area); in this study, there was a high incidence of early mortalities in males of the 30/20 mg/kg/day group. The incidence of mammary gland adenomas and adenocarcinomas was significantly increased in female mice dosed at ≥2 mg/kg/day and in female rats dosed at ≥4 mg/kg/day (0.5 and 2 times the MRHD based on mg/m2 body surface area, respectively). Antipsychotic drugs have been shown to chronically elevate prolactin levels in rodents. Serum prolactin levels were not measured during the olanzapine carcinogenicity studies; however, measurements during subchronic toxicity studies showed that olanzapine elevated serum prolactin levels up to 4-fold in rats at the same doses used in the carcinogenicity study. An increase in mammary gland neoplasms has been found in rodents after chronic administration of other antipsychotic drugs and is considered to be prolactin mediated. The relevance for human risk of the finding of prolactin mediated endocrine tumors in rodents is unknown [see Warnings and Precautions (5.17)].
Samidorphan
Samidorphan did not increase the incidence of tumors in rats administered oral doses of 20, 35, or 75 mg/kg/day (males) and 15, 30, or 60 mg/kg/day (females) for 96 (males) and 95 (females) weeks, which are up to 32 and 237 times the MRHD of 10 mg/day in males and females, respectively based on AUC. Samidorphan did not increase the incidence of tumors in transgenic rasH2 mice administered oral doses of 125, 250, or 500 mg/kg/day for 26 weeks.
Mutagenesis
Olanzapine
No evidence of genotoxic potential for olanzapine was found in the Ames reverse mutation test, in vivo micronucleus test in mice, the chromosome aberration test in Chinese hamster ovary cells, unscheduled DNA synthesis test in rat hepatocytes, induction of forward mutation test in mouse lymphoma cells, or in vivo sister chromatid exchange test in bone marrow of Chinese hamsters.
Samidorphan
No evidence of genotoxicity of samidorphan was found in the in vitro Ames bacterial reverse mutation test, the in vitro chromosome aberration assay in human peripheral blood lymphocytes or in the in vivo mouse bone marrow micronucleus assay.
Impairment of Fertility
Olanzapine
In an oral fertility and reproductive performance study in rats, male mating performance, but not fertility, was impaired at a dose of 22.4 mg/kg/day and female fertility was decreased at a dose of 3 mg/kg/day (11 and 1.5 times the MRHD of 20 mg/day based on mg/m2 body surface area, respectively). Discontinuance of olanzapine treatment reversed the effects on male mating performance. In female rats, the precoital period was increased and the mating index reduced at 5 mg/kg/day (2.5 times the MRHD based on mg/m2 body surface area). Diestrus was prolonged and estrus delayed at 1.1 mg/kg/day (0.6 times the daily oral MRHD based on mg/m2 body surface area); therefore, olanzapine may produce a delay in ovulation.
Samidorphan
Samidorphan did not impair fertility when administered orally to female rats at doses of 30, 150, or 450 mg/kg/day prior to and throughout mating and continuing to gestation day 7. The doses are approximately 32, 297, and >680 times the MRHD of 10 mg/day based on AUC, respectively. However, estrous cycle lengths were increased, and the total number of estrous cycles were decreased in females at the highest dose of 450 mg/kg/day. Samidorphan did not affect fertility when orally administered to male rats at doses of 10, 30, or 100 mg/kg/day prior to and throughout mating; the highest dose is approximately 16 times the MRHD based on AUC.
13.2 Animal Toxicology and/or Pharmacology
Olanzapine
In animal studies with olanzapine, the principal hematologic findings were reversible peripheral cytopenia in individua l dogs dosed at 10 mg/kg (17 times the MRHD of 20 mg olanzapine based on mg/m2 body surface area), dose-related decreases in lymphocytes and neutrophils in mice, and lymphopenia in rats. A few dogs treated with 10 mg/kg developed reversible neutropenia and/or reversible hemolytic anemia between 1 and 10 months of treatment. Dose-related decreases in lymphocytes and neutrophils were seen in mice given doses of 10 mg/kg (equal to 2 times the MRHD based on mg/m2 body surface area) in studies of 3 months’ duration.
Nonspecific lymphopenia, consistent with decreased body weight gain, occurred in rats receiving 22.5 mg/kg (11 times the MRHD based on mg/m2 body surface area) for 3 months or 16 mg/kg (8 times the MRHD based on mg/m2 body surface area) for 6 or 12 months. No evidence of bone marrow cytotoxicity was found in any of the species examined. Bone marrows were normocellular or hypercellular, indicating that the reductions in circulating blood cells were probably due to peripheral (non-marrow) factors.
Clinical studies
14.1. Schizophrenia
The efficacy of Lybalvi in the treatment of schizophrenia in adults is based, in part, upon adequate and well-controlled studies of orally administered olanzapine. Efficacy of Lybalvi was also evaluated in a 4-week, randomized, double-blind, placebo- and active-controlled study (Study 1).
In Study 1 (NCT02634346), adult patients who met DSM-5 criteria for schizophrenia were randomized in a 1:1:1 ratio to Lybalvi, olanzapine, or placebo for 4 weeks of daily dosing. Dosing was flexible based on clinical response and tolerability for the first 2 weeks of the study; doses thereafter were fixed. Patients assigned to Lybalvi could receive either 10 mg/10 mg or 20 mg/10 mg, and patients assigned to olanzapine could receive either 10 mg or 20 mg. The study was designed to compare Lybalvi with placebo, not with olanzapine.
Eligible patients were 18 to 70 years of age, with a body mass index (BMI) of 18.0–40.0 kg/m2, Positive and Negative Syndrome Scale (PANSS) total score of ≥80, and a score of ≥4 on at least 3 of the selected Positive Scale items. Patients were also required to have a Clinical Global Impression-Severity (CGI-S) score ≥4.
The primary efficacy endpoint was change from baseline in PANSS total score at Week 4. The PANSS is a 30-item scale that measures positive symptoms of schizophrenia (7 items), negative symptoms of schizophrenia (7 items), and general psychopathology (16 items), each rated on a scale of 1 (absent) to 7 (extreme). Total PANSS scores range from 30 to 210, with a higher score reflecting greater symptom severity. The secondary efficacy endpoint was defined as the change from baseline in CGI-S score at Week 4. The CGI-S is a validated scale that requires clinicians to rate a patient’s current illness severity and overall clinical state based on experience with the illness population. Scores range from 1 (normal, not at all ill) to 7 (extremely ill).
Compared with patients on placebo, a statistically significant improvement in the change from baseline in PANSS total score at Week 4 was observed in patients treated with Lybalvi (Table 7). The inclusion of samidorphan in Lybalvi did not appear to negatively impact the antipsychotic efficacy of olanzapine.
Table 7: Primary Efficacy Results for Change from Baseline in PANSS Total Score at Week 4 in Patients with Schizophrenia (Study 1)
|
Treatment group |
Total PANSS score |
||
| Baseline mean score (SD) | LS Mean change from baseline (SE) | Placebo-subtracted differencea (95% CI) | |
|
Lybalvi (10 mg/10 mg, 20 mg/10 mg) (N=132) |
101.8 (11.6) |
-23.9 (1.3) |
–6.4 (-10.0, -2.8) |
|
Placebo (N=133) |
102.7 (11.9) |
-17.5 (1.3) |
-- |
|
Olanzapine (10 mg, 20 mg (N=132) |
100.6 (12.1) |
-22.8 (1.3) |
-5.3 (-8.9, -1.7) |
Abbreviations: CI: confidence interval; LS: least squares; SD: standard deviation; SE: standard error.
a. Difference (drug minus placebo) in least squares mean change from baseline. A negative value for the placebo subtracted difference represents improvement.
The change from baseline in PANSS total score in Study 1 is displayed in Figure 4.
Figure 4: Change from Baseline in PANSS Total Score by Time (Week) in Patients with Schizophrenia (Study 1)
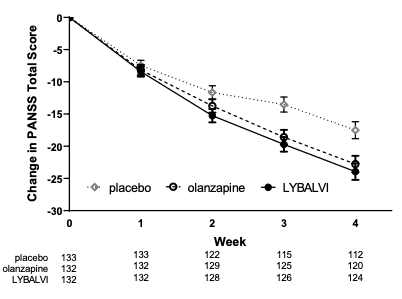
Error bars represent standard error. The numbers under the figure indicate the number of patients at each time point.
Compared with patients on placebo, a statistically significant improvement in CGI-S score at Week 4 was observed in patients treated with Lybalvi.
Evaluation of Weight Changes in Patients with Schizophrenia
In Study 2 (NCT02694328), adult patients who met DSM-5 criteria for schizophrenia were randomized in a 1:1 ratio to Lybalvi or olanzapine for 24 weeks of daily dosing. Dosing was flexible for the first 4 weeks of the study, and doses were fixed thereafter. Patients were treated with doses of Lybalvi of 10 mg/10 mg or 20 mg/10 mg, or with doses of olanzapine of 10 mg or 20 mg.
Eligible patients were 18 to 55 years of age with a body mass index (BMI) of 18 to 30 kg/m2,
PANSS total score of 50 to 90, CGI-S score of ≤4, and symptoms suitable for outpatient treatment; patients with diabetes mellitus were excluded.
The proportions of patients who discontinued study drug in the 24-week trial was 36% for both the Lybalvi and olanzapine-treated groups.
Weight Gain
The co-primary endpoints were percent change from baseline in body weight and the proportion of patients who gained ≥10% body weight at Week 24. Lybalvi was compared to olanzapine for each co-primary endpoint [see Adverse Reactions (6)]. Patients on stable, chronic olanzapine therapy were not specifically studied, so the weight effect of switching from olanzapine to Lybalvi is unknown.
Treatment with Lybalvi was associated with statistically significantly less weight gain than treatment with olanzapine, and with a smaller proportion of patients who gained ≥10% body weight (Table 8). Figure 5 displays the percent change in body weight over time.
Table 8: Primary Efficacy Results for Change from Baseline in Weight at Week 24 in Patients with Schizophrenia (Study 2)
|
Treatment Group |
% Change From Baseline in Body Weight |
≥10% Body Weight Gain |
|||
| Baseline Mean, kg (SD) |
LS Mean % Change From Baseline (SE) |
Olanzapine- subtracted Difference (95% CI) | Percentage of Patients | Olanzapine- subtracted Risk Difference (95% CI) | |
|
Lybalvi (10 mg/10 mg, 20 mg/10 mg) (N=266) |
77.0 (13.7) |
4.2 (0.7) |
-2.4 (-3.9, -0.9) |
17.8 |
-13.7 (-22.8, -4.6) |
|
Olanzapine (10 mg, 20 mg) (N=272) |
77.5 (13.5) |
6.6 (0.7) |
-- |
29.8 |
-- |
Abbreviations: CI: confidence interval; LS: least squares; SD: standard deviation; SE: standard error.
Figure 5: Percent Change from Baseline in Body Weight by Time (week) in Patients with Schizophrenia (Study 2)
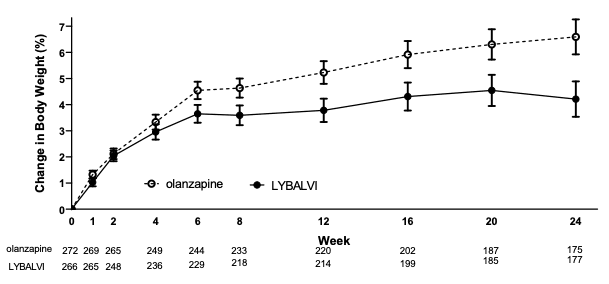
Error bars represent standard error. The numbers under the figure indicate the number of patients at each time point.
14.2. Bipolar I Disorder
The efficacy of Lybalvi in the treatment of adult patients with bipolar I disorder has been established based on adequate and well-controlled studies of orally administered olanzapine. The information below describes the results of adequate and well-controlled studies of olanzapine in patients with bipolar I disorder.
Monotherapy
The efficacy of oral olanzapine in the treatment of manic or mixed episodes was established in 2 short-term (one 3-week and one 4-week) placebo-controlled studies in adult patients who met the DSM-IV criteria for bipolar I disorder with manic or mixed episodes. These studies included patients with or without psychotic features and with or without a rapid-cycling course.
The primary rating instrument used for assessing manic symptoms in these studies was the Young Mania Rating Scale (Y-MRS), an 11-item clinician-rated scale traditionally used to assess the degree of manic symptomatology in a range from 0 (no manic features) to 60 (maximum score). The primary outcome in these studies was change from baseline in the Y-MRS total score. The results of the studies follow:
In one 3-week placebo-controlled study (n=67) which involved a dose range of olanzapine
(5 mg/day to 20 mg/day, once daily, starting at 10 mg/day), olanzapine was superior to placebo in the reduction of Y-MRS total score. In an identically designed study conducted simultaneously with the first study olanzapine demonstrated a similar treatment difference but, possibly due to sample size and site variability, was not shown to be superior to placebo on this outcome.
In a 4-week placebo-controlled study (n=115) which involved a dose range of olanzapine
(5 mg/day to 20 mg/day, once daily, starting at 15 mg/day), olanzapine was superior to placebo in the reduction of Y-MRS total score.
In another study, 361 patients meeting DSM-IV criteria for a manic or mixed episode of bipolar I disorder who had responded during an initial open-label treatment phase for about 2 weeks, on average, to olanzapine 5 mg/day to 20 mg/day were randomized to either continuation of olanzapine at their same dose (n=225) or to placebo (n=136), for observation of relapse. Approximately 50% of the patients had discontinued from the olanzapine group by day 59 and 50% of the placebo group had discontinued by day 23 of double-blind treatment. Response during the open-label phase was defined by having a decrease of the Y-MRS total score to ≤12 and HAM-D 21 to ≤8. Relapse during the double-blind phase was defined as an increase of the Y-MRS or HAM-D 21 total score to ≥15, or being hospitalize d for either mania or depression. In the randomized phase, patients receiving continued olanzapine experienced a significantly longer time to relapse.
Adjunct to Lithium or Valproate
The efficacy of oral olanzapine with concomitant lithium or valproate in the treatment of manic or mixed episodes was established in 2 controlled studies in patients who met the DSM-IV criteria for bipolar I disorder with manic or mixed episodes. These studies included patients with or without psychotic features and with or without a rapid-cycling course. The results of the studies follow:
In one 6-week placebo-controlled combination study, 175 outpatients on lithium or valproate therapy with inadequately controlled manic or mixed symptoms (Y-MRS ≥16) were randomized to receive either olanzapine or placebo, in combination with their original therapy. Olanzapine (in a dose range of 5 mg/day to 20 mg/day, once daily, starting at 10 mg/day) combined with lithium or valproate (in a therapeutic range of 0.6 mEq/L to 1.2 mEq/L or 50 µg/mL to 125 µg/mL, respectively) was superior to lithium or valproate alone in the reduction of Y-MRS total score.
In a second 6-week placebo-controlled combination study, 169 outpatients on lithium or valproate therapy with inadequately controlled manic or mixed symptoms (Y-MRS ≥16) were randomized to receive either olanzapine or placebo, in combination with their original therapy. Olanzapine (in a dose range of 5 mg/day to 20 mg/day, once daily, starting at 10 mg/day) combined with lithium or valproate (in a therapeutic range of 0.6 mEq/L to 1.2 mEq/L or 50 µg/mL to 125 µg/mL, respectively) was superior to lithium or valproate alone in the reduction of Y-MRS total score.
16. How supplied - storage and handling
How Supplied
Lybalvi (olanzapine and samidorphan) tablets have markings on both sides and are available as described in Table 9.
Table 9: Lybalvi Tablet Presentations
| Tablet strength(s) (olanzapine/samidorphan) |
Tablet description | Package configurations | NDC Number |
| 5 mg/10 mg | Yellow, capsule-shaped, debossed with “OS” on one side and “5” on the other side | 7-count bottle with child resistant closure | 65757-651-40 |
| 30-count bottle with child resistant closure | 65757-651-42 | ||
| 90-count bottle with child resistant closure | 65757-651-44 | ||
| 10 mg/10 mg | Orange, capsule-shaped, debossed with “OS” on one side and “10” on the other side | 7-count bottle with child resistant closure | 65757-652-40 |
| 30-count bottle with child resistant closure | 65757-652-42 | ||
| 90-count bottle with child resistant closure | 65757-652-44 | ||
| 15 mg/10 mg | Blue, capsule-shaped, debossed with “OS” on one side and “15” on the other side | 7-count bottle with child resistant closure | 65757-653-40 |
| 30-count bottle with child resistant closure | 65757-653-42 | ||
| 90-count bottle with child resistant closure | 65757-653-44 | ||
| 20 mg/10 mg | Pink, capsule-shaped, debossed with “OS” on one side and “20” on the other side | 7-count bottle with child resistant closure | 65757-654-40 |
| 30-count bottle with child resistant closure | 65757-654-42 | ||
| 90-count bottle with child resistant closure | 65757-654-44 |
Storage and Handling
Store at room temperature 20°C to 25°C (68°F to 77°F) with excursions permitted between 15°C and 30°C (59°F and 86°F) [see USP controlled room temperature].
Store in the original bottle with desiccant. Keep bottle tightly closed and protect from moisture.
Patient counseling information
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Concomitant Use with Opioids is Contraindicated
Advise patients to inform their healthcare provider if they are taking, or plan to take any opioids for any reason, as Lybalvi is contraindicated with use of opioids or those undergoing acute opioid withdrawal [see Dosage and Administration (2.1), Contraindications (4), Warnings and Precautions (5.3), Drug Interactions (7.3)].
Precipitation of Opioid Withdrawal
Advise patients not to take Lybalvi when using opioids because of the risks of opioid withdrawal syndrome, sometimes requiring hospitalization. Advise patients that they should have an opioid-free period of a minimum of 7 days after last use of short-acting opioids and 14 days from last use of long-acting opioids before initiating Lybalvi [see Contraindications (4), Warnings and Precautions (5.3)].
Risk of Opioid Overdosage
Advise patients that they may be at increased risk of opioid overdosage if they attempt to use high or repeated opioid doses. Inform patients of the potential consequences of trying to overcome the opioid blockade and the serious risks of taking opioids concurrently with Lybalvi or while transitioning off Lybalvi [see Warnings and Precautions (5.4)].
Risk of Resuming Opioids in Patients with Prior Opioid Use
Advise patients that if they used opioids prior to Lybalvi treatment, they may have decreased opioid tolerance if they use opioids after Lybalvi discontinuation or interruption [see Warnings and Precautions (5.4)].
Neuroleptic Malignant Syndrome
Counsel patients about a potentially fatal adverse reaction, Neuroleptic Malignant Syndrome (NMS), that has been reported with administration of antipsychotic drugs. Advise patients, family members, or caregivers to contact the healthcare provider or to report to the emergency room if they experience signs and symptoms of NMS [see Warnings and Precautions (5.5)].
Drug Reaction with Eosinophilia and Systemic Symptoms
Advise patients to report to their health care provider at the earliest onset of any signs and symptoms that may be associated with Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS) [see Warnings and Precautions (5.6)].
Metabolic Changes
Educate patients about the risk of metabolic changes, how to recognize symptoms of hyperglycemia and diabetes mellitus, and the need for specific monitoring, including blood glucose, lipids, and weight [see Warnings and Precautions (5.7)].
Tardive Dyskinesia
Counsel patients on the signs and symptoms of tardive dyskinesia and to contact their healthcare provider if these abnormal movements occur [see Warnings and Precautions (5.8)].
Orthostatic Hypotension and Syncope
Educate patients about the risk of orthostatic hypotension and syncope, especially early in treatment, and also at times of re-initiating treatment [see Warnings and Precautions (5.9), Drug Interactions (7.2)].
Leukopenia/Neutropenia
Advise patients with a pre-existing low WBC or a history of drug induced leukopenia/ neutropenia that they should have their CBC monitored while taking Lybalvi [see Warnings and Precautions (5.11)].
Potential for Cognitive and Motor Impairment
Caution patients about performing activities requiring mental alertness, such as operating hazardous machinery or operating a motor vehicle, until they are reasonably certain that Lybalvi therapy does not affect them adversely [see Warnings and Precautions (5.14)].
Concomitant Medication
Advise patients to inform their healthcare providers if they are taking, or plan to take any other olanzapine containing medication. Advise patients to inform their healthcare providers of any changes to their current prescription or over-the-counter medications because there is a potential for interactions [see Drug Interactions (7.1, 7.2, 7.3)].
Body Temperature Dysregulation
Educate patients regarding appropriate care in avoiding overheating and dehydration [see Warnings and Precautions (5.15)].
Alcohol
Advise patients to use caution consuming alcohol while taking Lybalvi [see Drug Interactions (7.1)].
Pregnancy
Advise patients to notify their healthcare provider if they become pregnant or intend to become pregnant during treatment with Lybalvi. Advise patients that Lybalvi used during the third trimester may cause extrapyramidal and/or withdrawal symptoms (agitation, hypertonia, hypotonia, tremor, somnolence, respiratory distress, and feeding disorder) in a neonate. Advise patients that there is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to Lybalvi during pregnancy [see Use in Specific Populations (8.1)].
Lactation
Advise breastfeeding women using Lybalvi to monitor infants for excess sedation, irritability, poor feeding, and extrapyramidal symptoms (tremors and abnormal muscle movements) and to seek medical care if they notice these signs [see Use in Specific Populations (8.2)].
Infertility
Advise females of reproductive potential that Lybalvi may impair fertility due to an increase in serum prolactin levels. The effects on fertility are reversible [see Use in Specific Populations (8.3)].
Administration Information
Advise patients to take Lybalvi once daily and not split or combine tablets [see Dosage and Administration (2.4)].
Distributed by:
Alkermes, Inc.
852 Winter Street
Waltham, MA 02451-1420
©2021 Alkermes, Inc. All rights reserved.
ALKERMES® is a registered trademark of Alkermes, Inc. and
LYBALVI™ is a trademark used by Alkermes, Inc. under license.








