Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Solution, Intravenous:
Osmitrol: 5% (1000 mL); 10% (500 mL); 15% (500 mL); 20% (250 mL, 500 mL)
Generic: 20% (250 mL [DSC], 500 mL); 25% (50 mL)
Solution, Intravenous [preservative free]:
Generic: 20% (500 mL); 25% (50 mL [DSC])
Solution, Irrigation:
Resectisol: 5% (2000 mL)
Pharmacology
Mechanism of Action
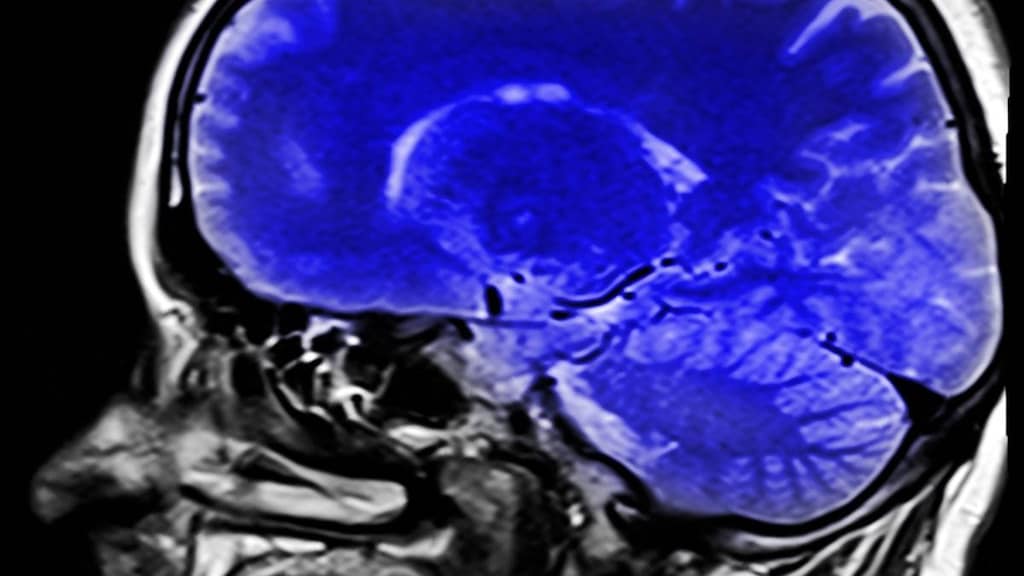
Produces an osmotic diuresis by increasing the osmotic pressure of glomerular filtrate, which inhibits tubular reabsorption of water and electrolytes and increases urinary output . Mechanism of action in reduction of intracranial pressure (ICP) is less clear. However, it is thought that mannitol reduces ICP by reducing blood viscosity which transiently increases cerebral blood flow and oxygen transport and constricts pial arterioles. This in turn reduces cerebral blood volume and ICP. Furthermore, mannitol reduces ICP by withdrawing water from the brain parenchyma and excretes water in the urine (Allen 1998; BTF [Carney 2016]).
Pharmacokinetics/Pharmacodynamics
Distribution
17 L; remains confined to extracellular space (except in extreme concentrations); does not penetrate the blood-brain barrier (generally, penetration is low)
Metabolism
Minimally hepatic to glycogen
Excretion
Urine (~80% as unchanged drug)
Onset of Action
Diuresis: 1 to 3 hours; Reduction in intracranial pressure: ~15 to 30 minutes
Duration of Action
Reduction in intracranial pressure: 3 to 6 hours
Half-Life Elimination
0.5 to 2.5 hours; 6 to 36 hours in renal failure
Use: Labeled Indications
Injection: Reduction of increased intracranial pressure (associated with cerebral edema and/or brain mass); reduction of increased intraocular pressure
Genitourinary irrigation solution: Irrigation in transurethral prostatic resection or other transurethral surgical procedures
Use: Off Label
Improve renal transplant function
Contraindications
Injection: Hypersensitivity to mannitol or any component of the formulation; anuria; severe hypovolemia; active intracranial bleeding except during craniotomy; preexisting severe pulmonary vascular congestion or pulmonary edema.
Genitourinary irrigation solution: Anuria.
Dosage and Administration
Dosing: Adult
Intracranial pressure (ICP), cerebral edema, reduction (off-label dosing): IV: 0.25 to 1 g/kg/dose; may repeat every 6 to 8 hours as needed (BTF [Carney 2016]; Grape 2012). Some suggest maintaining serum osmolality <320 mOsm/kg (Rabinstein 2006). However, this value is routinely exceeded without ill effect. A better marker for mannitol toxicity may be the serum osmol gap (or osmolal gap) and the target is <18 to 20 (Erstad 2016; García-Morales 2004).
Intraocular pressure (IOP), reduction: IV: 1.5 to 2 g/kg administered over 30 to 60 minutes 1 to 1.5 hours prior to surgery
IOP (traumatic hyphema), reduction: IV: 1.5 g/kg administered over 45 minutes twice daily for IOP >35 mm Hg; may administer every 8 hours in patients with extremely high pressure (Crouch 1999)
Kidney transplant:
Donor: 12.5 g (with adequate hydration) prior to nephrectomy; may repeat (Morris 2008)
Recipient: 50 g before kidney revascularization (Sprung 2000; Tiggeler 1984; van Valenberg 1987; Weimar 1983)
Transurethral irrigation: Use 5% urogenital solution as required for irrigation.
Dosing: Geriatric
Refer to adult dosing. Consider initiation at lower end of dosing range.
Dosing: Pediatric
Note: The manufacturer's labeling recommends a test dose prior to starting IV mannitol therapy in patients with marked oliguria or suspected renal insufficiency.
Acute renal failure (oliguria): Infants, Children, and Adolescents: IV: Initial: 0.5 to 1 g/kg/dose infused over 2 to 6 hours; usual range: 0.25 to 2 g/kg/dose; may repeat dose every 4 to 6 hours; do not repeat dose if oliguria persists. Note: Although FDA-labeled indications, the use of mannitol for the prevention of acute renal failure and/or promotion of diuresis is not routinely recommended (Kellum 2008).
Test dose (to assess adequate renal function): IV: 0.2 g/kg (maximum dose: 12.5 g) over 3 to 5 minutes to produce a urine flow of at least 1 mL/kg/hour for 1 to 3 hours
Intracranial pressure (ICP), reduction: Infants, Children, and Adolescents: IV: Usual range: 0.25 to 1 g/kg/dose infused over 20 to 30 minutes; repeat as needed to maintain serum osmolality <300 to 320 mOsm/kg (BTF [Carney 2016]; Hegenbarth 2008; Kochanek 2012). Note: The manufacturer's labeling allows for higher single doses up to 2 g/kg/dose.
Intraocular pressure (IOP), reduction: Infants, Children, and Adolescents: IV: 1 to 2 g/kg/dose or 30 to 60 g/m2/dose infused over 30 to 60 minutes administered 1 to 1.5 hours prior to surgery
IOP (traumatic hyphema), reduction: Infants, Children, and Adolescents: IV: 1.5 g/kg/dose infused over 45 minutes twice daily for IOP >35 mm Hg; may administer every 8 hours in patients with extremely high pressure (Crouch 1999)
Administration
IV: Concentration and rate of administration depends on indication/severity or may be adjusted to urine flow. For cerebral edema or elevated intracranial pressure, administer over 30 to 60 minutes. Inspect for crystals prior to administration. If crystals are present, redissolve by warming solution. Do not place mannitol 25% injection in polyvinyl chloride (PVC) bags; a white flocculent precipitate may form from contact with PVC surfaces. Use filter-type administration set (≤5 micron) for infusion solutions containing mannitol ≥20% (WHO 2011). Do not administer with blood. Crenation and agglutination of red blood cells may occur if administered with whole blood.
Vesicant (at concentrations >5%); ensure proper catheter or needle position prior to and during IV infusion. Avoid extravasation of IV infusions. Administration into a large central vein is recommended.
Extravasation management: If extravasation occurs, stop infusion immediately and disconnect (leave needle/cannula in place); gently aspirate extravasated solution (do NOT flush the line); initiate hyaluronidase antidote; remove needle/cannula; apply dry cold compresses (Hurst 2004; Reynolds 2014); elevate extremity.
Hyaluronidase: Intradermal or SubQ: Inject a total of 1 to 1.7 mL (15 units/mL) as five separate 0.2 to 0.3 mL injections (using a tuberculin syringe) into area of extravasation at the leading edge in a clockwise manner (Reynolds 2014) or SubQ: Administer multiple 0.5 to 1 mL injections of a 15 units/mL solution around the periphery of the extravasation (Kumar 2003).
Irrigation: Administer using only the appropriate transurethral urologic instrumentation.
Storage
Injection: Store at controlled room temperature; do not freeze. Crystallization of solution may occur at low temperatures; do not use solutions that contain crystals. To dissolve crystals in plastic containers, heat solution up to 60°C to 70°C (140°F to 158°F) (recommended temperature may vary; refer to manufacturer’s labeling), with agitation; do not immerse in water or microwave (may contaminate or damage product); allow solution to return to room or body temperature before use. To dissolve crystals in vials/bottles, warm vial in hot water at 80°C (176°F) and periodically shake vigorously or vial may be autoclaved at 121°C (250°F) for 20 minutes at 15 psi. Allow solution to return to room or body temperature before use.
Irrigation: Store at room temperature of 25°C (77°F); excursions permitted up to 40°C. Avoid excessive heat; do not warm above 150°F (66°C). Do not freeze.
Drug Interactions
Amikacin (Oral Inhalation): May enhance the nephrotoxic effect of Mannitol (Systemic). Avoid combination
Aminoglycosides: Mannitol (Systemic) may enhance the nephrotoxic effect of Aminoglycosides. Avoid combination
Diacerein: May enhance the therapeutic effect of Diuretics. Specifically, the risk for dehydration or hypokalemia may be increased. Monitor therapy
Opioid Agonists: May enhance the adverse/toxic effect of Diuretics. Opioid Agonists may diminish the therapeutic effect of Diuretics. Monitor therapy
Sodium Phosphates: Diuretics may enhance the nephrotoxic effect of Sodium Phosphates. Specifically, the risk of acute phosphate nephropathy may be enhanced. Management: Consider avoiding this combination by temporarily suspending treatment with diuretics, or seeking alternatives to oral sodium phosphate bowel preparation. If the combination cannot be avoided, hydrate adequately and monitor fluid and renal status. Consider therapy modification
Tobramycin (Oral Inhalation): Mannitol (Systemic) may enhance the nephrotoxic effect of Tobramycin (Oral Inhalation). Avoid combination
Test Interactions
May cause false positive results for blood ethylene glycol concentrations. High mannitol concentrations may cause false low results for inorganic phosphorus blood concentrations if assay based on the conversion of phosphate (orthophosphate) to the phosphomolybdate complex is used.
Adverse Reactions
Frequency not defined:
Cardiovascular: Cardiac failure, chest pain, edema, hypertension, localized phlebitis, palpitations, peripheral edema, tachycardia, thrombophlebitis
Central nervous system: Chills, coma, confusion, dizziness, headache, increased intracranial pressure (rebound), lethargy, malaise, pain, seizure
Dermatologic: Diaphoresis, localized erythema, localized rash, pruritus, skin necrosis, skin rash, urticaria
Endocrine & metabolic: Dehydration, fluid and electrolyte disturbance, hyperkalemia, hypernatremia, hypervolemia, hypokalemia, hyponatremia, hypovolemia, increased thirst, metabolic acidosis, metabolic alkalosis
Gastrointestinal: Nausea, vomiting, xerostomia
Genitourinary: Anuria, azotemia, diuresis, hematuria, oliguria, osmotic nephrosis, urinary retention
Hematologic & oncologic: Hemoconcentration
Local: Local inflammation, local pain, local pruritus
Neuromuscular & skeletal: Arm and/or wrist pain, asthenia, muscle rigidity, myalgia
Ophthalmic: Blurred vision
Renal: Polyuria
Respiratory: Cough, pulmonary congestion, pulmonary edema, rhinitis
Miscellaneous: Fever
Postmarketing: Acute renal failure, anaphylaxis, central nervous system toxicity, dyspnea, hypersensitivity reaction, hypotension
Warnings/Precautions
Concerns related to adverse effects:
- Extravasation: Vesicant (at concentrations >5%); ensure proper catheter or needle position prior to and during IV infusion. Avoid extravasation of IV infusions; may cause compartment syndrome. Administration into a large central vein is recommended.
- Fluid/electrolyte imbalance: May cause hypervolemia and electrolyte disturbances; monitor for new onset or worsening cardiac or pulmonary congestion. Also may cause profound diuresis with fluid and electrolyte loss; close medical supervision and dose evaluation are required. Correct electrolyte disturbances; adjust dose to avoid dehydration.
- Hypersensitivity: Serious hypersensitivity reactions (eg, anaphylaxis), including fatalities, have been reported. Discontinue mannitol immediately if hypersensitivity reaction develops and treat accordingly.
- Nephrotoxicity: May cause renal dysfunction especially with high doses; use caution in patients taking other nephrotoxic agents, with sepsis or preexisting renal disease. To minimize adverse renal effects, adjust to keep serum osmolality <320 mOsm/L. Discontinue if evidence of acute tubular necrosis.
Disease-related concerns:
- Cerebral edema: In patients being treated for cerebral edema, mannitol may accumulate in the brain (causing rebound increases in intracranial pressure) if circulating for long periods of time as with continuous infusion; intermittent boluses preferred. Cardiovascular status should also be evaluated; do not administer electrolyte-free mannitol solutions with blood. If hypotension occurs, monitor cerebral perfusion pressure to ensure adequate.
- CNS effects: CNS toxicity (eg, coma, confusion, lethargy) may occur; risk may be increased in patients with impaired renal function or with concomitant use of neurotoxic drugs. Discontinue mannitol if CNS toxicity develops.
- Renal impairment: Use with caution. In patients with severe impairment, do not use until adequacy of renal function and urine flow is established; use 1 to 2 test doses to assess renal response.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Monitoring Parameters
Renal function, daily fluid I & O, serum electrolytes, serum and urine osmolality. Monitor infusion site.
For treatment of elevated intracranial pressure, some suggest maintaining serum osmolality <320 mOsm/kg due to the potential risk of acute renal tubular damage (Grape 2012; Rabenstein 2006). However, this value is routinely exceeded without ill effect. A better marker for mannitol toxicity may be the serum osmole gap and the target used by most clinicians is <18 to 20 (Erstad 2016; García-Morales 2004).
Pregnancy
Pregnancy Considerations
Mannitol crosses the placenta.
Outcome information following surgical use in pregnancy is limited; amniotic fluid volume may be decreased (Handlogten 2015; Kazemi 2014).
Patient Education
What is this drug used for?
- It is used to get rid of extra fluid.
- It is used to treat brain swelling.
- It is used to lower high eye pressure.
- It is used to help get rid of unwanted substances in the body.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Headache
- Runny nose
- Nausea
- Vomiting
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain.
- Fluid and electrolyte problems like mood changes, confusion, muscle pain or weakness, abnormal heartbeat, severe dizziness, passing out, fast heartbeat, increased thirst, seizures, loss of strength and energy, lack of appetite, unable to pass urine or change in amount of urine passed, dry mouth, dry eyes, or nausea or vomiting.
- Acidosis like confusion, fast breathing, fast heartbeat, abnormal heartbeat, severe abdominal pain, nausea, vomiting, fatigue, shortness of breath, or loss of strength and energy.
- Skin infection
- Shortness of breath
- Severe dizziness
- Passing out
- Excessive weight gain
- Swelling in the arms or legs
- Chest pain
- Fast heartbeat
- Blurred vision
- Vision changes
- Edema
- Chills
- Skin discoloration
- Injection site skin breakdown or irritation
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.