Boxed Warning
Intrathecal and high-dose therapy:
Use only preservative-free methotrexate formulations and diluents for intrathecal and high-dose therapy. Do NOT use formulations or diluents containing preservatives for intrathecal and high-dose therapy because they contain benzyl alcohol.
Appropriate use:
Because of the possibility of serious toxic reactions (which can be fatal), methotrexate should be used only in life threatening neoplastic diseases or in patients with psoriasis or rheumatoid arthritis with severe, recalcitrant, disabling disease which is not adequately responsive to other forms of therapy. Deaths have been reported with the use of methotrexate in the treatment of malignancy, psoriasis, and rheumatoid arthritis. Patients should be closely monitored for bone marrow, liver, lung, skin, and kidney toxicities. Patients should be informed by their physician of the risks involved and be under a physician's care throughout therapy.
The use of methotrexate high-dose regimens recommended for osteosarcoma requires meticulous care. High-dose regimens of methotrexate injection for other neoplastic diseases are investigational, and a therapeutic advantage has not been established.
Pregnancy:
Methotrexate can cause embryo-fetal toxicity, including fetal death. Use in rheumatoid arthritis, polyarticular-course juvenile idiopathic arthritis (pJIA), and psoriasis is contraindicated in pregnancy. Consider the benefits and risks of methotrexate and risks to the fetus when prescribing methotrexate to a pregnant patient with a neoplastic disease. Verify the pregnancy status of females of reproductive potential prior to initiating therapy. Advise females and males of reproductive potential to use effective contraception during and after treatment with methotrexate.
Bone marrow suppression:
Unexpectedly severe (sometimes fatal) bone marrow suppression and aplastic anemia have been reported with concomitant administration of methotrexate (usually in high dosage) along with some nonsteroidal anti-inflammatory drugs (NSAIDs).
Renal impairment:
Methotrexate elimination is reduced in patients with impaired renal function, ascites, or pleural effusions. Such patients require especially careful monitoring for toxicity, and require dose reduction or, in some cases, discontinuation of methotrexate administration.
Hepatotoxicity:
Methotrexate causes hepatotoxicity, fibrosis, and cirrhosis, but generally only after prolonged use. Acutely, liver enzyme elevations are frequently seen. These are usually transient and asymptomatic, and also do not appear predictive of subsequent hepatic disease. Liver biopsy after sustained use often shows histologic changes, and fibrosis and cirrhosis have been reported; these latter lesions may not be preceded by symptoms or abnormal liver function tests in the psoriasis population. For this reason, periodic liver biopsies are usually recommended for psoriatic patients who are under long-term treatment. Persistent abnormalities in liver function tests may precede appearance of fibrosis or cirrhosis in the rheumatoid arthritis population.
Pneumonitis:
Methotrexate-induced lung disease, including acute or chronic interstitial pneumonitis, is a potentially dangerous lesion, which may occur acutely at any time during therapy and has been reported at low doses. It is not always fully reversible and fatalities have been reported. Pulmonary symptoms (especially a dry, nonproductive cough) may require interruption of treatment and careful investigation.
Gastrointestinal toxicity:
Unexpectedly severe (sometimes fatal) gastrointestinal toxicity has been reported with concomitant administration of methotrexate (usually in high dosage) along with some NSAIDs. Diarrhea and ulcerative stomatitis require interruption of therapy; otherwise hemorrhagic enteritis and death from intestinal perforation may occur.
Secondary malignancy:
Malignant lymphomas, which may regress following withdrawal of methotrexate, may occur in patients receiving low-dose methotrexate and, thus, may not require cytotoxic treatment. Discontinue methotrexate first and, if the lymphoma does not regress, appropriate treatment should be instituted.
Tumor lysis syndrome:
Like other cytotoxic drugs, methotrexate may induce tumor lysis syndrome in patients with rapidly growing tumors. Appropriate supportive and pharmacologic measures may prevent or alleviate this complication.
Dermatologic toxicity:
Severe, occasionally fatal skin reactions have been reported following single or multiple doses of methotrexate. Reactions have occurred within days of oral, intramuscular, intravenous, or intrathecal methotrexate administration. Recovery has been reported with discontinuation of therapy.
Opportunistic infections:
Potentially fatal opportunistic infections, especially Pneumocystis jirovecii pneumonia, may occur with methotrexate therapy.
Radiotherapy:
Methotrexate given concomitantly with radiotherapy may increase the risk of soft tissue necrosis and osteonecrosis.
Experienced physician (injection):
Methotrexate should be used only by health care providers whose knowledge and experience include the use of antimetabolite therapy.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Solution, Injection:
Generic: 250 mg/10 mL (10 mL); 50 mg/2 mL (2 mL)
Solution, Injection [preservative free]:
Generic: 1 g/40 mL (40 mL); 100 mg/4 mL (4 mL [DSC]); 200 mg/8 mL (8 mL [DSC]); 250 mg/10 mL (10 mL); 50 mg/2 mL (2 mL)
Solution, Oral:
Xatmep: 2.5 mg/mL (60 mL, 120 mL) [contains methylparaben sodium, propylparaben sodium]
Solution Auto-injector, Subcutaneous [preservative free]:
Otrexup: 7.5 mg/0.4 mL (0.4 mL [DSC]); 10 mg/0.4 mL (0.4 mL); 12.5 mg/0.4 mL (0.4 mL); 15 mg/0.4 mL (0.4 mL); 17.5 mg/0.4 mL (0.4 mL); 20 mg/0.4 mL (0.4 mL); 22.5 mg/0.4 mL (0.4 mL); 25 mg/0.4mL (0.4 mL)
Rasuvo: 7.5 mg/0.15 mL (0.15 mL); 10 mg/0.2 mL (0.2 mL); 12.5 mg/0.25 mL (0.25 mL); 15 mg/0.3 mL (0.3 mL); 17.5 mg/0.35 mL (0.35 mL); 20 mg/0.4 mL (0.4 mL); 22.5 mg/0.45 mL (0.45 mL); 25 mg/0.5 mL (0.5 mL); 27.5 mg/0.55 mL (0.55 mL [DSC]); 30 mg/0.6 mL (0.6 mL)
Solution Reconstituted, Injection [preservative free]:
Generic: 1 g (1 ea)
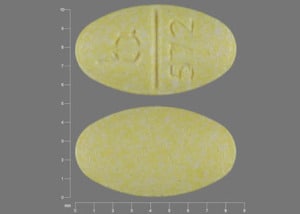
Tablet, Oral:
Rheumatrex: 2.5 mg [DSC]
Trexall: 5 mg, 7.5 mg, 10 mg, 15 mg [scored]
Generic: 2.5 mg
Pharmacology
Mechanism of Action
Methotrexate is a folate antimetabolite that inhibits DNA synthesis, repair, and cellular replication. Methotrexate irreversibly binds to and inhibits dihydrofolate reductase, inhibiting the formation of reduced folates, and thymidylate synthetase, resulting in inhibition of purine and thymidylic acid synthesis, thus interfering with DNA synthesis, repair, and cellular replication. Methotrexate is cell cycle specific for the S phase of the cycle. Actively proliferative tissues are more susceptible to the effects of methotrexate.
The mechanism in the treatment of rheumatoid arthritis and polyarticular-course juvenile idiopathic arthritis is unknown, but may affect immune function. In psoriasis, methotrexate is thought to target rapidly proliferating epithelial cells in the skin.
In Crohn disease, it may have immune modulator and anti-inflammatory activity.
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Highly variable; dose dependent; decreased absorption at higher doses (pediatric patients: >40 mg/m2; adult patients: >80 mg/m2); possibly due to saturation effect; IM injection: Complete
IM injection: Complete
Distribution
Penetrates slowly into 3rd space fluids (eg, pleural effusions, ascites), exits slowly from these compartments (slower than from plasma); sustained concentrations retained in kidney and liver; Vd: IV: 0.18 L/kg (initial); 0.4 to 0.8 L/kg (steady state)
Metabolism
Partially metabolized by intestinal flora (after oral administration) to DAMPA by carboxypeptidase; hepatic aldehyde oxidase converts methotrexate to 7-hydroxy methotrexate; polyglutamates are produced intracellularly and are just as potent as methotrexate; their production is dose- and duration-dependent and they are slowly eliminated by the cell once formed. Polyglutamated forms can be converted back to methotrexate.
Excretion
Dose and route dependent; IV: Urine (80% to 90% as unchanged drug; 5% to 7% as 7-hydroxy methotrexate); feces (<10%)
Onset of Action
Antirheumatic: 3 to 6 weeks; additional improvement may continue longer than 12 weeks
Time to Peak
Serum: Oral: Children: 0.7 to 4 hours (reported for a 15 mg/m2 dose); Adults: 0.75 to 6 hours; Children and Adults: IM: 30 to 60 minutes
Half-Life Elimination
Children: ALL: 0.7 to 5.8 hours (dose range: 6.3 to 30 mg/m2); pJIA: 0.9 to 2.3 hours (dose range: 3.75 to 26.2 mg/m2)
Adults: Low dose: 3 to 10 hours; High dose: 8 to 15 hours
Protein Binding
~50%
Use in Specific Populations
Special Populations: Renal Function Impairment
An increase in serum levels occurs because of decreased elimination in patients with renal function impairment.
Use: Labeled Indications
Oncology uses: Acute lymphoblastic leukemia (ALL) maintenance treatment, ALL meningeal leukemia (preservative-free only; prophylaxis and treatment); treatment of trophoblastic neoplasms (gestational choriocarcinoma, chorioadenoma destruens and hydatidiform mole), breast cancer, head and neck cancer (epidermoid), cutaneous T-Cell lymphoma (advanced mycosis fungoides), lung cancer (squamous cell and small cell), advanced non-Hodgkin lymphomas (NHL), osteosarcoma (preservative-free only).
Nononcology uses: Treatment of psoriasis (severe, recalcitrant, disabling) that is unresponsive to other therapies; severe, active rheumatoid arthritis (RA) that is unresponsive to or intolerant of first-line therapy including full dose nonsteroidal anti-inflammatory agents (NSAIDs); active polyarticular-course juvenile idiopathic arthritis (pJIA) that is unresponsive to or intolerant of first-line therapy including full dose NSAIDs.
Limitations of use: Otrexup and Rasuvo are not indicated for the treatment of neoplastic diseases.
Guideline recommendations: Rheumatoid arthritis: Treatment initiation with a disease-modifying antirheumatic drug (DMARD) is recommended in DMARD-naïve patients with either early rheumatoid arthritis (RA) (disease duration <6 months) or established RA (disease duration ≥6 months). Methotrexate is the preferred initial DMARD for most early or established RA patients (Singh [ACR 2016]).
Use: Off Label
Acute promyelocytic leukemia maintenancea
Data from studies of combination chemotherapy in adult patients with acute promyelocytic leukemia support the use of methotrexate as part of the maintenance phase of treatment Ades 2008, Powell 2010, Sanz 2004.
Bladder cancerayes
Data from a multicenter, randomized, phase III study support the use of methotrexate (in combination with cisplatin, vinblastine, and leucovorin rescue [CMV regimen]) for the neoadjuvant treatment of muscle-invasive bladder cancer Griffiths 2011. Also, data from multiple studies support the use of methotrexate (in combination with vinblastine, doxorubicin, and cisplatin [MVAC regimen or dose-dense MVAC]) in the treatment of advanced bladder cancer Bamias 2004, Choueiri 2014, Grossman 2003, Plimack 2014, Sternberg 2001, Sternberg 2006, von der Maase 2000.
Based on the Treatment of Non-Metastatic Muscle-Invasive Bladder Cancer: American Urological Association/American Society of Clinical Oncology/American Society for Radiation Oncology/Society of Urologic Oncology Guideline, methotrexate in combination with vinblastine, doxorubicin, and cisplatin (MVAC regimen) or in combination with cisplatin and vinblastine (CMV regimen) is recommended as neoadjuvant therapy in the management of nonmetastatic, muscle-invasive bladder cancer. Adjuvant therapy (following radical cystectomy) with a cisplatin-containing regimen (such as MVAC, dose-dense MVAC, or CMV) should be offered to patients with high risk pathological features who did not receive neoadjuvant chemotherapy.
Crohn disease (corticosteroid-dependent or remission maintenance)ayes
Data from a double-blind, placebo-controlled, multicenter trial and a systematic review of 5 randomized controlled trials support the use of methotrexate in the maintenance of remission in Crohn disease Feagan 2000, Patel 2014.
Based on the American College of Gastroenterology guidelines for the management of Crohn disease in adults and the American Gastroenterological Association Institute Guideline on the Use of Thiopurines, Methotrexate, and Anti-TNF-a Biologic Drugs for the Induction and Maintenance of Remission in Inflammatory Crohn disease, methotrexate is effective and recommended for patients with steroid-dependent Crohn disease and for maintenance of remission.
Dermatomyositis/polymyositisc
Data from a retrospective cohort study and a retrospective chart review in patients with polymyositis or dermatomyositis suggest a benefit with methotrexate for this condition Joffe 1993, Newman 1995.
Clinical experience also suggests the utility of methotrexate in the treatment of dermatomyositis/polymyositis, typically as a glucocorticoid-sparing agent to reduce the cumulative dose of glucocorticoid required McGrath 2018, Miller 2019, Oddis 2016, Wiendl 2008.
Graft-versus-host disease, acute (prophylaxis)ayes
Data from a randomized study support the use of methotrexate (in combination with cyclosporine and prednisone) to prevent acute graft-versus-host disease (aGVHD) following allogeneic hematopoietic stem cell transplantation Chao 1993. This combination was more effective than using cyclosporine and prednisone alone. Subsequently, data from a follow-up, prospective, randomized study demonstrated that the addition of prednisone did not have an impact on the incidence of acute or chronic GVHD; however, the addition of prednisone was associated with a somewhat lower incidence of early posttransplant complications Chao 2000. Further data suggest that the combination of cyclosporine and prednisone with or without methotrexate results in comparable chronic GVHD-free survival Ross 1999.
Based on the Prophylaxis and Treatment of GVHD: European Society for Blood and Marrow Transplantation-European Leukemia Net Working Group Recommendations for a Standardized Practice, methotrexate as combination therapy given to prevent aGVHD is effective and recommended in the management of this condition Ruutu 2013.
Granulomatosis with polyangiitis (Wegener granulomatosis) and microscopic polyangiitis (maintenance therapy)b
Data from an open-label randomized multicenter study comparing methotrexate to azathioprine support the use of oral methotrexate as maintenance therapy (once remission induction was achieved) in the management of granulomatosis with polyangiitis and microscopic polyangiitis Pagnoux 2008. Another open-label prospective study also supports the use of oral methotrexate as maintenance therapy for managing granulomatosis with polyangiitis and microscopic polyangiitis following remission induction Langford 2003.
Nonleukemic meningeal cancerb
Data from a limited number of patients studied suggested that intrathecal methotrexate and high dose intravenous methotrexate are comparable in the treatment of nonleukemic meningeal cancer Glantz 1998. Additional data from a randomized, controlled study support the use of intrathecal methotrexate in the treatment of nonleukemic meningeal cancer Glantz 1999.
Primary CNS lymphoma, newly diagnosedb
Data from two multicenter phase II trials support the use of methotrexate (in combination with rituximab, leucovorin, procarbazine, and vincristine [R-MPV], followed by radiotherapy and cytarabine, and intrathecal/intra-Ommaya methotrexate if indicated) for the treatment of newly-diagnosed primary CNS lymphoma (PCNSL) Morris 2013, Shah 2007. Data from a single center study also support the use of R-MPV, followed by consolidation high-dose chemotherapy and autologous stem cell transplant in newly diagnosed PCNSL Omuro 2015. Data from a multicenter, phase II study in immunocompetent patients with newly diagnosed primary CNS lymphoma support the use of high dose methotrexate (with deferred whole-brain radiotherapy) in the treatment of CNS lymphoma Batchelor 2003. Data from a multicenter, single-arm, phase II trial suggest that methotrexate (in combination with rituximab and procarbazine) may be an efficacious regimen in newly diagnosed PCNSL patients ≥65 years of age Fritsch 2017. Data from a small phase II study support the use of methotrexate (in combination with leucovorin, temozolomide, and rituximab and followed by high-dose consolidation chemotherapy) for the treatment of newly diagnosed primary CNS lymphoma Rubenstein 2013. Data from the phase II portion of a phase I-II study also support the use of methotrexate (in combination with leucovorin, temozolomide, and rituximab and followed by whole brain radiation therapy and subsequent temozolomide) for the treatment of newly diagnosed primary CNS lymphoma Glass 2016.
Sarcoidosis, second-line therapybyes
Data from a small randomized study, a retrospective study, and a consensus study support the use of methotrexate as second-line therapy for sarcoidosis Baughman 2000, Schutt 2010, Vorselaars 2013. Clinical experience also suggests the utility of methotrexate as an alternative agent or as steroid-sparing therapy in the management of pulmonary sarcoidosis Judson 201.
Based on recommendations from the World Association of Sarcoidosis and Granulomatous Disorders for the use of methotrexate in sarcoidosis, oral methotrexate is a second-line therapy option in patients with steroid-refractory sarcoidosis, in patients with intolerance to steroid therapy, or as steroid-sparing therapy.
Soft tissue sarcoma (desmoid tumors, aggressive fibromatosis), advancedb
Data from a phase II study in patients with primary or recurrent, advanced, inoperable aggressive fibromatosis support the use of methotrexate (in combination with vinblastine) for the treatment of advanced soft tissue sarcoma (desmoid tumors, aggressive fibromatosis) Azzarelli 2001. Methotrexate (in combination with vinblastine) was found to prolong stable disease in a subset of patients with this condition.
Systemic lupus erythematosus, moderate-to-severea
Data from a randomized, double-blind, placebo-controlled study in patients with systemic lupus erythematosus (SLE) support the use of methotrexate in the treatment of moderate-to-severe SLE. In patients with this condition, the use of methotrexate conferred a significant advantage in patients with moderate SLE by lowering prednisone dose and slightly reducing disease activity Fortin 2008.
Takayasu arteritis, refractory or relapsing diseasec
Data from a limited number of patients in an open-label pilot study suggest that methotrexate may be beneficial for the treatment of refractory or relapsing Takayasu arteritis Hoffman 1994.
Termination of intrauterine pregnancybyes
Evidence from a large prospective multicenter non-controlled trial showed safety and efficacy of methotrexate followed by misoprostol for termination of intrauterine pregnancy in pregnancies ≤49 days gestation Creinin 1996. Clinical experience also suggests the utility of methotrexate (followed by misoprostol) in the termination of intrauterine pregnancy Jones 2017.
Based on the American College of Obstetricians and Gynecologists (ACOG) guidelines for the Medical Management of First Trimester Abortion, methotrexate (followed by misoprostol) may be given for medical termination of intrauterine pregnancy with a gestational age up to 49 days ACOG 143 2014. This combination is rarely used in the United States, but may be considered for use in regions where mifepristone regimens are not available or inappropriate ACOG 143 2014, SOGC [Costescu 2016].
Tubal ectopic pregnancybyes
Evidence from multiple case series Barnhart 2003, Ory 1986, Sauer 1987, Stovall 1991, prospective non-randomized trials Barnhart 2007, Mergenthal 2016, Stovall 1989, Stovall 1993, and a prospective randomized study Song 2016 supports the use of methotrexate for the medical management of tubal ectopic pregnancy in appropriately selected patients.
Based on the ACOG Practice Bulletin: Tubal Ectopic Pregnancy ACOG 193 2018 and the American Society for Reproductive Medicine: Medical Treatment of Ectopic Pregnancy: A Committee Opinion ASRM 2013, methotrexate is effective and recommended in the management of tubal ectopic pregnancy. Treatment may be appropriate in hemodynamically stable females with a nonruptured tubal ectopic pregnancy and who do not have absolute contraindications to methotrexate administration specific to this indication ACOG 193 2018. Absolute contraindications include: Anemia (moderate to severe), breastfeeding, hemodynamic instability, hepatic dysfunction (clinically important), hypersensitivity to methotrexate, immunodeficiency, intrauterine pregnancy, leukopenia (moderate to severe), peptic ulcer disease (active), pulmonary disease (active), renal dysfunction (clinically important), ruptured ectopic pregnancy, or thrombocytopenia (moderate to severe). Relative contraindications include: Embryonic cardiac activity, high initial hCG concentration (>5,000 mIU/mL per ASRM), ectopic pregnancy >4 cm, refusal to accept blood transfusion, or not available for follow-up ACOG 193 2018, ASRM 2013.
Uveitisc
Results from noncontrolled studies demonstrate that methotrexate is generally effective in treating uveitis Galor 2008, Gangaputra 2009, Kaplan-Messas 2003, Muñoz-Fernández 2009. However, no controlled clinical trials have been performed. An expert review panel recommends methotrexate as second-line therapy for the treatment of uveitis in adults Díaz-Llopis 2009.
Contraindications
Known hypersensitivity to methotrexate or any component of the formulation; breastfeeding (product-specific; refer to manufacturer's labeling).
Additional contraindications for patients with psoriasis, rheumatoid arthritis or polyarticular-course juvenile idiopathic arthritis: Pregnancy, alcoholism, alcoholic liver disease or other chronic liver disease, immunodeficiency syndromes (overt or laboratory evidence); preexisting blood dyscrasias (eg, bone marrow hypoplasia, leukopenia, thrombocytopenia, significant anemia).
Canadian labeling: Additional contraindications (not in the US labeling): Severe renal impairment (including end-stage renal disease with or without dialysis); females of childbearing potential (until pregnancy is excluded); concomitant use with nitrous oxide anesthesia.
Dosage and Administration
Dosing: Adult
Note: Methotrexate doses between 100 to 500 mg/m2may require leucovorin calcium rescue. Doses >500 mg/m2require leucovorin calcium rescue (refer to Dosing – Adjustment for Toxicity for leucovorin calcium dosing). Doses ≥250 mg/m2 (IV) are associated with moderate emetic potential; antiemetics may be recommended to prevent nausea and vomiting.
Acute lymphoblastic leukemia:
Meningeal leukemia prophylaxis or treatment: Intrathecal: Manufacturer's labeling: 12 mg (maximum 15 mg/dose) every 2 to 7 days; continue for 1 dose beyond cerebrospinal fluid (CSF) cell count normalization. Note: Optimal intrathecal chemotherapy dosing should be based on age rather than on body surface area (BSA); CSF volume correlates with age and not to BSA (Bleyer 1983; Kerr 2001).
CALGB 8811 regimen (Larson 1995; combination therapy):
Early intensification: Intrathecal: 15 mg day 1 of early intensification phase, repeat in 4 weeks.
CNS prophylaxis/interim maintenance phase:
Intrathecal: 15 mg day 1, 8, 15, 22, and 29.
Oral: 20 mg/m2 days 36, 43, 50, 57, and 64.
Prolonged maintenance: Oral: 20 mg/m2 days 1, 8, 15, and 22 every 4 weeks for 24 months from diagnosis.
Dose-intensive regimen (Kantarjian 2000; combination therapy):
IV: 200 mg/m2 over 2 hours, followed by 800 mg/m2 over 24 hours beginning day 1, (followed by leucovorin rescue) of even numbered cycles (in combination with cytarabine; alternates with Hyper-CVAD).
CNS prophylaxis: Intrathecal: 12 mg on day 2 of each cycle; duration depends on risk.
Maintenance: IV: 10 mg/m2/day for 5 days every month for 2 years (in combination with prednisone, vincristine, and mercaptopurine).
Acute promyelocytic leukemia maintenance phase (off-label use):
Oral: 15 mg/m2 once weekly for 2 years (Ades 2008) or 20 mg/m2 once weekly for 1 year (Powell 2010).
IM: 15 mg/m2 once weekly for 2 years (Sanz 2004).
Bladder cancer (off-label use): IV:
Locally advanced or metastatic disease:
Dose-dense MVAC regimen: 30 mg/m2 on day 1 every 14 days (in combination with vinblastine, doxorubicin, cisplatin, and growth factor support) until disease progression or unacceptable toxicity (Sternberg 2001; Sternberg 2006).
MVAC regimen: 30 mg/m2 on days 1, 15, and 22 every 28 days (in combination with vinblastine, doxorubicin, and cisplatin) for up to 6 cycles (von der Maase 2000) or 30 mg/m2 on days 1, 15, and 22 every 28 days (in combination with vinblastine, doxorubicin, and cisplatin) until disease progression or unacceptable toxicity (Sternberg 2001; Sternberg 2006) or 30 mg/m2 on days 1, 15, and 22 every 28 days (in combination with vinblastine, doxorubicin, cisplatin, and filgrastim) for up to 6 cycles or until loss of clinical benefit (Bamias 2004).
Neoadjuvant treatment:
Note: Patients with non-organ confined disease at cystectomy who did not receive cisplatin-based neoadjuvant chemotherapy should be offered an adjuvant cisplatin-based chemotherapy regimen (AUA/ASCO/ASTRO/SUO [Chang 2017]).
Dose-dense MVAC regimen: 30 mg/m2 on day 1 every 14 days (in combination with vinblastine, doxorubicin, cisplatin, and pegfilgrastim) for 3 or 4 cycles (Choueiri 2014; Plimack 2014).
MVAC regimen: 30 mg/m2 on days 1, 15, and 22 every 28 days (in combination with vinblastine, doxorubicin, and cisplatin) for 3 cycles (Grossman 2003).
CMV regimen: 30 mg/m2 on days 1 and 8 every 21 days (in combination with cisplatin, vinblastine, and leucovorin) for 3 cycles (Griffiths 2011).
Breast cancer: IV: CMF regimen: 40 mg/m2 days 1 and 8 every 4 weeks (in combination with cyclophosphamide and fluorouracil) for 6 to 12 cycles (Bonadonna 1995; Levine 1998).
Crohn disease, corticosteroid dependent or remission maintenance (off-label use): IM, SubQ: 25 mg once weekly; may reduce dose to 15 mg once weekly if steroid-free remission maintained for 4 months (Lichtenstein 2018).
Dermatomyositis/polymyositis (off-label use): Note: Concomitant folic acid is recommended to reduce the side effects; leucovorin can be administered in patients who do not respond to folic acid (Briemberg 2003; Miller 2019).
Oral: Initial: 5 to 15 mg once weekly, usually given adjunctively with prednisone; may increase the dose slowly in 2.5 mg/week increments to 25 mg once weekly (McGrath 2018; Oddis 2016; Wiendl 2008). Some experts prefer to initiate therapy at 15 mg once weekly and if there is an inadequate response after 8 to 12 weeks, begin increasing the dose in 2.5 mg/week increments to 25 mg once weekly (Miller 2019). Note: Doses >25 mg/week have been used historically in refractory/resistant disease, but should be avoided due to the availability of alternative agents; do not exceed a maximum dose of 50 mg/week. If doses >25 mg/week are given, methotrexate should be administered parenterally (McGrath 2018; Miller 2019).
SubQ, IV, IM: The same oral weekly dose may be administered once weekly parenterally in patients unable to tolerate oral administration (subcutaneous administration is preferred, depending on clinical setting) (Miller 2019).
Gestational trophoblastic diseases, choriocarcinoma, chorioadenoma: 15 to 30 mg oral or IM daily for a 5-day course; may repeat for 3 to 5 courses (manufacturer's labeling) or
Gestational trophoblastic neoplasia, low-risk disease (off-label dosing): IV: 100 mg/m2 over 30 minutes followed by 200 mg/m2 over 12 hours (with leucovorin 24 hours after the start of methotrexate), administer a second course if hCG levels plateau for 3 consecutive weeks (Garrett 2002).
Gestational trophoblastic neoplasia, high-risk metastatic disease (off-label dosing): IV:
EMA-CO regimen: 100 mg/m2 IV push followed by 200 mg/m2 over 12 hours on day 1 (with leucovorin 24 hours after the start of methotrexate; in combination with dactinomycin, etoposide, vincristine, and cyclophosphamide) every 14 days and continuing for at least 2 cycles after hCG level is normal (Escobar 2003; Lurain 2006).
EMA-EP regimen:
Patients without brain metastases: 100 mg/m2 IV push followed by 200 mg/m2 over 12 hours on day 1 every 2 weeks (in combination with etoposide, leucovorin, dactinomycin, and cisplatin), continue for 2 cycles after hCG level is normal (Ghaemmaghami 2004).
Patients with brain metastases: 100 mg/m2 IV push followed by 1,000 mg/m2 over 12 hours on day 1 every 2 weeks (in combination with etoposide, leucovorin, dactinomycin, and cisplatin), continue for 4 cycles after hCG level is normal (Ghaemmaghami 2004).
EP-EMA regimen: EMA: 300 mg/m2 over 12 hours on day 1 (in combination with etoposide, leucovorin, and dactinomycin); alternating weekly with EP (etoposide and cisplatin) (Newlands 2000).
Graft-versus-host disease, acute, prophylaxis (off-label use): IV: 15 mg/m2 on day 1 and 10 mg/m2 on days 3 and 6 after allogeneic transplant (in combination with cyclosporine and prednisone) (Chao 1993; Chao 2000; Ross 1999) or 15 mg/m2 on day 1 and 10 mg/m2 on days 3, 6, and 11 after allogeneic transplant (in combination with cyclosporine) (Chao 2000) or 15 mg/m2 on day 1 and 10 mg/m2 on days 3, 6, and 11 after allogeneic transplant (in combination with cyclosporine, followed by leucovorin); may omit day 11 methotrexate for ≥ grade 2 toxicity (Ruutu 2013).
Granulomatosis with polyangiitis (Wegener granulomatosis) and microscopic polyangiitis (maintenance therapy after remission induction) (off-label use): Oral: Initial: 0.3 mg/kg/week (beginning 2 to 3 weeks after the last induction pulse); progressively increase by 2.5 mg each week up to 25 mg/week for 12 months followed by a 3-month taper (Pagnoux 2008) or Initial: 0.3 mg/kg/week (maximum: 15 mg/week), if tolerated, after 1 to 2 weeks, increase dose by 2.5 mg/week (up to 20 to 25 mg/week) for 2 years; if remission is sustained for 2 years, taper off by 2.5 mg each month until discontinued (Langford 2003).
Head and neck cancer, advanced: IV: 40 mg/m2 once weekly until disease progression or unacceptable toxicity (Forastiere 1992; Guardiola 2004; Stewart 2009).
Lymphoma, non-Hodgkin: IV:
CODOX-M/IVAC regimen (Mead 2008): Cycles 1 and 3 of CODOX-M (CODOX-M alternates with IVAC).
Adults ≤65 years of age: IV: 300 mg/m2 over 1 hour (on day 10) followed by 2,700 mg/m2 over 23 hours (with leucovorin rescue).
Adults >65 years of age: IV: 100 mg/m2 over 1 hour (on day 10) followed by 900 mg/m2 over 23 hours (with leucovorin rescue).
Hyper-CVAD alternating with high-dose methotrexate/cytarabine regimen: IV: 1,000 mg/m2 over 24 hours on day 1 during even courses (2, 4, 6, and 8) of 21-day treatment cycles (Thomas 2006) or 200 mg/m2 bolus day 1 followed by 800 mg/m2 over 24 hours during even courses (2, 4, 6, and 8) of 21-day treatment cycles (Khouri 1998) with leucovorin rescue.
Mycosis fungoides (cutaneous T-cell lymphoma): 5 to 50 mg once weekly or 15 to 37.5 mg twice weekly orally or IM for early stages (manufacturer's labeling) or 25 mg orally once weekly, may increase to 50 mg once weekly (Zackheim 2003).
Nonleukemic meningeal cancer (off-label use): Intrathecal: 12 mg/dose twice weekly for 4 weeks, then weekly for 4 doses, then monthly for 4 doses (Glantz 1998) or 10 mg twice weekly for 4 weeks, then weekly for 1 month, then every 2 weeks for 2 months (Glantz 1999) or 10 to 15 mg twice weekly for 4 weeks, then once weekly for 4 weeks, then a maintenance regimen of once a month (Chamberlain 2010).
Osteosarcoma: Adults ≤30 years of age: IV: MAP regimen: 12 g/m2 (maximum: 20 g/dose) over 4 hours (followed by leucovorin rescue) for 4 doses during induction (before surgery) at weeks 4, 5, 9, and 10, and for 8 doses during maintenance (after surgery) at weeks 15, 16, 20, 21, 24, 25, 28, and 29 (in combination with doxorubicin and cisplatin) (Bielack 2015; Whelan 2015); other combinations, intervals, age ranges, and doses (8 to 14 g/m2/dose) have been described (with leucovorin rescue), refer to specific reference for details (Bacci 2000; Bacci 2003; Le Deley 2007; Meyers 1992; Meyers 2005; Weiner 1986; Winkler 1988).
Primary CNS lymphoma, newly diagnosed (off-label use): IV: 8 g/m2 over 4 hours (followed by leucovorin rescue) every 14 days until complete response or a maximum of 8 cycles; if complete response, follow with 2 consolidation cycles at the same dose every 14 days (with leucovorin rescue), followed by 11 maintenance cycles of 8 g/m2 every 28 days with leucovorin rescue (Batchelor 2003) or R-MPV regimen: 3.5 g/m2 over 2 hours on day 2 every 2 weeks (in combination with rituximab, vincristine, procarbazine, and leucovorin [with intra-Ommaya methotrexate 12 mg between days 5 and 12 of each cycle if positive CSF cytology]) for 5 to 7 induction cycles followed by reduced-dose whole brain radiotherapy and then cytarabine (Morris 2013; Shah 2007) or autologous stem cell transplant (Omuro 2015) or R-MP regimen (patients ≥65 years of age): 3 g/m2 over 4 hours on days 2, 16, and 30 of a 42-day cycle (in combination with rituximab, procarbazine, and leucovorin) for 3 cycles (Fritsch 2017) or MT-R regimen: 8 g/m2 once every 2 weeks (adjusted for creatinine clearance [refer to protocol for details] and in combination with leucovorin, temozolomide, and rituximab) for 7 doses, then followed by high-dose consolidation chemotherapy (Rubenstein 2013) or 3.5 g/m2 on weeks 1, 3, 5, 7, and 9 (in combination with leucovorin, temozolomide, and rituximab), followed by whole brain radiotherapy and then post-radiation temozolomide (Glass 2016).
Psoriasis: Note: Some experts recommend concomitant folic acid 1 to 5 mg daily to reduce hematologic, gastrointestinal, and hepatic adverse events related to methotrexate.
Oral: Initial: 2.5 to 5 mg/dose every 12 hours for 3 doses per week or
Oral, IM, IV, SubQ: Initial: 10 to 25 mg given once weekly; adjust dose gradually to optimal response; in general, doses >30 mg per week should not be exceeded.
Note: An initial test dose of 2.5 to 5 mg is recommended in patients with risk factors for hematologic toxicity or renal impairment (Kalb 2009).
Rheumatoid arthritis: Note: Some experts recommend concomitant folic acid at a dose of least 5 mg per week to reduce hematologic, gastrointestinal, and hepatic adverse events related to methotrexate.
Oral: Initial: 10 to 15 mg once weekly, increased by 5 mg every 2 to 4 weeks to a maximum of 20 to 30 mg once weekly has been recommended by some experts. Consider parenteral therapy with inadequate response or intolerance to oral therapy (Visser 2009).
Manufacturer's labeling: Dosing in the prescribing information may not reflect current clinical practice. 7.5 mg once weekly or 2.5 mg every 12 hours for 3 doses per week.
SubQ: Initial: 7.5 mg once weekly; adjust dose gradually based on response and toxicity or (off-label dosing): Initial: 15 mg once weekly; for inadequate response after 16 weeks, may increase to 20 mg once weekly (Braun 2008).
IM: 7.5 mg once weekly; adjust dose gradually based on response and toxicity.
Sarcoidosis, second-line therapy (off-label use) Oral: Initial: 5 to 15 mg once weekly; range: 5 to 20 mg/week; maximum: 20 mg/week (in combination with oral folic acid) (Judson 2012; WASGD [Cremers 2013]) or Initial: 10 mg once weekly; may increase to 15 mg once weekly (in combination with oral folic acid) (Vorselaars 2013) or Initial: 10 mg/week (as divided doses on 2 consecutive days with dosage adjustments as indicated [in combination with oral folic acid]) (Baughman 2000).
Soft tissue sarcoma (desmoid tumors, aggressive fibromatosis), advanced (off-label use): IV: 30 mg/m2 every 7 to 10 days (dose usually rounded to 50 mg) in combination with vinblastine for 1 year (Azzarelli 2001).
Systemic lupus erythematosus, moderate-to-severe (off-label use): Oral: Initial: 7.5 mg once weekly; may increase by 2.5 mg increments weekly (maximum: 20 mg once weekly), in combination with prednisone (Fortin 2008).
Takayasu arteritis, refractory or relapsing disease (off-label use): Oral: Initial dose: 0.3 mg/kg/week (maximum: 15 mg per week), titrated by 2.5 mg increments every 1 to 2 weeks until reaching a maximum tolerated weekly dose of 25 mg (use in combination with a corticosteroid; Hoffman 1994).
Termination of intrauterine pregnancy (off-label use): IM: 50 mg/m2 followed by vaginal misoprostol 3 to 7 days later in pregnancies ≤49 days' gestation (ACOG 143 2014; Creinin 1996).
Tubal ectopic pregnancy (off-label use): IM: Note: Regimens are named for the intended number of doses; actual number of doses given may be greater (Barnhart 2009).
Single-dose regimen: 50 mg/m2 on day 1. Measure serum hCG levels on days 4 and 7; if hCG decrease is <15%, repeat dose (methotrexate 50 mg/m2) on day 7 (ACOG 193 2018; ASRM 2013; RCOG [Elson 2016]; Stovall 1993).
Two-dose regimen: 50 mg/m2 on day 1. Measure serum hCG levels on day 4 and administer a second dose of methotrexate 50 mg/m2. Measure serum hCG levels on day 7. If hCG decrease is <15%, administer a third dose of methotrexate 50 mg/m2 and measure serum hCG again on day 11; if hCG decrease is <15% on day 11, administer a fourth dose of methotrexate 50 mg/m2 and measure serum hCG levels on day 14 (ACOG 193 2018; Barnhart 2007).
Multidose regimen (in combination with leucovorin): 1 mg/kg on days 1, 3, 5, and 7 alternating with leucovorin calcium on days 2, 4, 6, and 8. Measure serum hCG on each day of methotrexate administration. If serum hCG decreases by >15% from previous measurement, discontinue methotrexate (total treatment may be between 1 and 4 doses). If serum hCG decreases by <15% from previous measurement, administer methotrexate (maximum 4 doses) (ACOG 193 2018; ASRM 2013; Sauer 1987; Stovall 1989).
Uveitis (off-label use): Oral: 7.5 to 20 mg once weekly either alone or in conjunction with other corticosteroids/immunosuppressants (Diaz-Llopis 2009; Galor 2008; Kaplan-Messas 2003; Munoz-Fernandez 2009).
Dosing: Geriatric
Refer to adult dosing; adjust for renal impairment.
Breast cancer: Patients >60 years of age: CMF regimen: IV: 30 mg/m2 days 1 and 8 every 4 weeks (in combination with cyclophosphamide and fluorouracil) for up to 12 cycles (Bonadonna 1995).
Meningeal leukemia: Intrathecal: Consider a dose reduction (CSF volume and turnover may decrease with age).
Non-Hodgkin lymphoma: CODOX-M/IVAC regimen (Mead 2008): Cycles 1 and 3 of CODOX-M (CODOX-M alternates with IVAC): IV: 100 mg over 1 hour (on day 10) followed by 900 mg over 23 hours (with leucovorin rescue).
Primary CNS lymphoma, newly diagnosed (off-label use): Patients ≥65 years of age: R-MP regimen: IV: 3 g/m2 over 4 hours on days 2, 16, and 30 of a 42-day cycle (in combination with rituximab, procarbazine, and leucovorin) for 3 cycles (Fritsch 2017).
Rheumatoid arthritis/psoriasis: Oral: Initial: 5 to 7.5 mg per week.
Dosing: Pediatric
Note: Methotrexate doses between 100 to 500 mg/m2may require leucovorin calcium rescue. Methotrexate doses >500 mg/m2require leucovorin calcium rescue.
Note: Dosing may be presented as mg/m2 or mg/kg; verify dosage unit for calculations; extra precautions should be taken. Frequency of dosing is indication specific (generally weekly or daily); patient harm may occur if administered incorrectly; extra precautions should be taken to verify appropriate frequency. For oncology uses, regimens with corresponding dosing and frequency are highly variable and subject to frequent changes; typical dose ranges presented; specific protocols should be consulted.
Acute lymphoblastic leukemia (ALL) of infancy: Limited data available: Note: Intrathecal therapy is also administered (refer to specific reference for intrathecal dosing used within protocol); other combination chemotherapy variable based on protocol, and phase of treatment; refer to specific protocol: Intensification and Consolidation: Infant (<1 year of age) at diagnosis: IV: 4,000 to 5,000 mg/m2 over 24 hours every 7 days for 2 doses; specific days depends on protocol phase (Dreyer 2015; Pieters 2007)
Acute lymphoblastic leukemia (ALL): Note: Intrathecal therapy is also administered (refer to specific reference for intrathecal dosing used within protocol): Limited data available; multiple regimens reported; methotrexate is part of a combination regimen; refer to specific protocols:
Interim maintenance:
High-dose methotrexate: Children and Adolescents IV: 500 mg/m2 over 30 minutes followed by 4,500 mg/m2 over 23.5 hours (to complete a total dose of 5,000 mg/m2 over 24 hours on days 1, 15, 29, and 43 (with leucovorin rescue) (Larsen 2016; Seibel 2008; Winter 2015)
Escalating-dose methotrexate: Children and Adolescents: IV: Initial dose: 100 mg/m2 then escalate dose by 50 mg/m2 every 10 days for 5 doses total (Larsen 2016; Seibel 2008; Winter 2015)
Maintenance: Children and Adolescents: Oral: 20 mg/m2 once weekly (Larsen 2016; Seibel 2008; Winter 2015)
CNS prophylaxis intrathecal therapy: Infants, Children, and Adolescents: Intrathecal: Age-based dosing: Days of administration vary based on risk status and protocol; refer to institutional protocols or reference for details (Larsen 2016; Lin 2008; Matloub 2006):
<1 year: 6 mg
1 to <2 years: 8 mg
2 to <3 years: 10 mg
3 to ≤8 years: 12 mg
>8 years: 15 mg
CNS tumors, malignant (medulloblastoma, PNET, ependymoma, brainstem glioma): Limited data available: Head Start II Protocol (Chi 2004): Children <10 years: IV: 400 mg/kg on Day 4 with leucovorin rescue until level less than 0.1 micromolar (µM) every 21 days for 5 cycles (in combination with cisplatin, vincristine, etoposide, and cyclophosphamide; then followed by an auto-transplant)
Crohn disease: Limited data available: Children and Adolescents: Oral, SubQ: Note: Should be used in patients intolerant or unresponsive to purine analog therapy (eg, azathioprine, mercaptopurine); use in combination with folic acid supplementation
BSA-directed dosing: 15 mg/m2 once weekly; maximum dose: 25 mg (Mack 1998; Rufo 2012; Sandhu 2010; Turner 2007)
Fixed-dosing (Kliegman 2011; Mack 1998; Turner 2007; Weiss 2009)
20 to 29 kg: 10 mg once weekly
30 to 39 kg: 15 mg once weekly
40 to 49 kg: 20 mg once weekly
≥50 kg: 25 mg once weekly
Dermatomyositis: Limited data available: Children and Adolescents:
IM or SubQ: 15 to 20 mg/m2 once a week in combination with corticosteroids and with either folic acid or folinic acid supplementation (Ruperto 2016)
IM or SubQ (preferred): Initial: 15 to 20 mg/m2or 1 mg/kg (whichever is less) once weekly; maximum dose: 40 mg; used in combination with corticosteroids (Huber 2010; Ramanan 2005, Ruperto 2016)
Oral (not preferred): Initial: 15 mg/m2or 1 mg/kg (whichever is less) once weekly; maximum dose: 40 mg; used in combination with corticosteroids (Huber 2010; Ramanan 2005)
Graft-versus-host disease, acute (aGVHD) prophylaxis: Limited data available: Children and Adolescents: IV: 15 mg/m2/dose on day 1 and 10 mg/m2/dose on days 3 and 6 after allogeneic transplant (in combination with cyclosporine and prednisone) (Chao 1993; Chao 2000; Ross 1999) or 15 mg/m2/dose on day 1 and 10 mg/m2/dose on days 3, 6, and 11 after allogeneic transplant (in combination with cyclosporine) (Chao 2000). Leucovorin rescue may be administered according to protocol.
Juvenile idiopathic arthritis (JIA); polyarticular:
BSA-directed dosing: Children and Adolescents 2 to 16 years: Oral, IM, SubQ: Initial: 10 mg/m2 once weekly, adjust gradually up to 20 to 30 mg/m2 once weekly; usual maximum dose: 25 mg; to reduce GI side effects, consider parenteral administration (IM, SubQ) of higher doses (20 to 30 mg/m2)
Weight-directed dosing: Children and Adolescents: Oral, SubQ: Initial: 0.5 mg/kg once weekly; maximum initial dose: 15 mg; if symptoms worsen or unchanged after 4 weeks, may increase to SubQ: 1 mg/kg; maximum dose: 30 mg (Dewitt 2012)
Meningeal leukemia, prophylaxis or treatment: Note: Frequency and duration of treatment based on protocol; treatment dosing may be a frequency of every 2 to 7 days (based on protocol); for treatment, often used combination with cytarabine and hydrocortisone (triple intrathecal therapy); refer to institutional protocols or references for details. Optimal intrathecal chemotherapy dosing should be based on age rather than on body surface area (BSA); CSF volume correlates with age and not to BSA (Bleyer 1983; Kerr 2001): Infants, Children, and Adolescents: Intrathecal:
<1 year: 6 mg/dose
1 to <2 years: 8 mg/dose
2 to <3 years: 10 mg/dose
3 to <9 years: 12 mg/dose
≥9 years: 15 mg/dose (Larsen 2016)
Non-Hodgkin Lymphoma, B-cell:
Intermediate risk: Limited data available (Goldman 2013; Goldman 2014): Note: Some regimens may include periodic intrathecal methotrexate doses; refer to institution specific protocols or references cited, only intravenous dosing provided. Induction 1 and 2 (COPADM regimen) and Consolidation 1 and 2 (CYM regimen): Children and Adolescents: IV: 3,000 mg/m2 over 3 hours with leucovorin rescue, combination chemotherapy varied with protocol phase
High risk: Limited data available (Cairo 2007): Note: Some regimens may include periodic intrathecal methotrexate doses; refer to institution specific protocols or references cited, only intravenous dosing provided. Infants ≥6 months, Children, and Adolescents: IV: 8,000 mg/m2 over 4 hours once followed by leucovorin rescue; specific day of therapy and combination chemotherapy depends on protocol phase and clinical factors (eg, CNS positive)
Non-Hodgkin Lymphoma, T-cell (Anaplastic Large Cell Lymphoma [ALCL]): Limited data available (Reiter 1994; Seideman 2001): NHL-BFM90 protocol: Note: Both intravenous and intrathecal methotrexate dosing were part of protocol; use extra precaution ensuring route and dose. Infants, Children, and Adolescents:
Course B:
IV: 500 mg/m2 over 24 hours; administer 10% of dose over the first 30 minutes and remaining 90% of dose over 23.5 hours on Day 1 (in combination with dexamethasone, cyclophosphamide, doxorubicin, and triple intrathecal therapy)
Intrathecal: On Day 1; administer 2 hours after the start of the methotrexate IV infusion
<1 year: 6 mg/dose
1 to <2 years: 8 mg/dose
2 to 3 years: 10 mg/dose
≥3 years: 12 mg/dose
Course BB:
IV: 5,000 mg/m2 over 24 hours; administer 10% of dose over the first 30 minutes and remaining 90% of dose over 23.5 hours on Day 1 (in combination with dexamethasone, cyclophosphamide, vincristine, doxorubicin, and triple intrathecal therapy)
Intrathecal: On Day 1 administer 2 hours after the start of the methotrexate IV infusion; also administered on Day 5. Note: In patients with overt CNS disease and an implantable intraventricular device, presented doses were reduced by 50% (Seideman 2001).
<1 year: 3 mg/dose
1 to <2 years: 4 mg/dose
2 to <3 years: 5 mg/dose
≥3 years: 6 mg
Osteosarcoma: Limited data available: High-dose methotrexate: Children and Adolescents: IV: 12 g/m2 (maximum dose: 20 g/dose) over 4 hours (followed by leucovorin rescue) for 4 doses during induction (before surgery) at weeks 3, 4, 8, and 9, and for 8 doses during maintenance (after surgery) at weeks 15, 16, 20, 21, 25, 26, 30, and 31 (in combination with doxorubicin and cisplatin) (Meyers 2005); other frequency and duration have also been reported (Ferrari 2005)
Psoriasis, severe; recalcitrant to topical therapy: Limited data available: Children and Adolescents: Oral, SubQ: Usual reported range: 0.2 to 0.4 mg/kg once weekly; reported treatment duration is highly variable: 6 to 178 weeks (Dadlani 2005; deJager 2010)
Scleroderma, localized (juvenile): Limited data available: Infants, Children, and Adolescents: Oral, SubQ (preferred): 1 mg/kg once weekly; maximum dose: 25 mg; alone or in combinations with corticosteroids; duration of therapy: 12 months (Li 2012)
Uveitis, recalcitrant: Limited data available: Children and Adolescents:
BSA-directed dosing: Oral, SubQ: Most frequently reported: 15 mg/m2 once weekly, usual range: 10 to 25 mg/m2 (Foeldvari 2005; Simonini 2013); the SubQ route may be preferred for patients with GI symptoms, poor bioavailability or doses >15 mg/m2 (Simonini 2010)
Weight-directed dosing: SubQ: 0.5 to 1 mg/kg once weekly; maximum dose: 25 mg (Weiss 1998)
Dosing adjustment for toxicity: Infants, Children, and Adolescents:
Nonhematologic toxicity: Diarrhea, stomatitis, or vomiting which may lead to dehydration: Discontinue until recovery
Hematologic toxicity:
Psoriasis, arthritis (JIA): Significant blood count decrease: Discontinue immediately.
Oncologic uses: Profound granulocytopenia and fever: Evaluate immediately; consider broad-spectrum parenteral antimicrobial coverage
Dosing: Adjustment for Toxicity
Methotrexate toxicities:
Nonhematologic toxicity: Diarrhea, stomatitis, or vomiting which may lead to dehydration: Discontinue until recovery
Hematologic toxicity:
Psoriasis, rheumatoid arthritis: Significant blood count decrease: Discontinue immediately
Oncologic uses: Profound granulocytopenia and fever: Evaluate immediately; consider broad-spectrum parenteral antimicrobial coverage
Leucovorin calcium dosing (from methotrexate injection prescribing information; other leucovorin dosing/schedules may be specific to chemotherapy protocols):
Normal methotrexate elimination (serum methotrexate level ~10 micromolar at 24 hours after administration, 1 micromolar at 48 hours, and <0.2 micromolar at 72 hours): Leucovorin calcium 15 mg (oral, IM, or IV) every 6 hours for 60 hours (10 doses) beginning 24 hours after the start of methotrexate infusion
Delayed late methotrexate elimination (serum methotrexate level remaining >0.2 micromolar at 72 hours and >0.05 micromolar at 96 hours after administration): Continue leucovorin calcium 15 mg (oral, IM or IV) every 6 hours until methotrexate level is <0.05 micromolar
Delayed early methotrexate elimination and/or acute renal injury (serum methotrexate level ≥50 micromolar at 24 hours, or ≥5 micromolar at 48 hours, or a doubling of serum creatinine level at 24 hours after methotrexate administration): Leucovorin calcium 150 mg IV every 3 hours until methotrexate level is <1 micromolar, then 15 mg IV every 3 hours until methotrexate level <0.05 micromolar
Leucovorin nomogram dosing for high-dose methotrexate overexposure (generalized leucovorin dosing derived from reference nomogram figures, refer to each reference [Bleyer 1978; Bleyer 1981; Widemann 2006] or institution-specific nomogram for details):
At 24 hours:
For methotrexate levels of ≥100 micromolar at ~24 hours, leucovorin is initially dosed at 1,000 mg/m2 IV every 6 hours
For methotrexate levels of ≥10 to <100 micromolar at 24 hours, leucovorin is initially dosed at 100 mg/m2 IV every 3 or 6 hours
For methotrexate levels of ~1 to 10 micromolar at 24 hours, leucovorin is initially dosed at 10 mg/m2 IV or orally every 3 or 6 hours
At 48 hours:
For methotrexate levels of ≥100 micromolar at 48 hours, leucovorin is dosed at 1,000 mg/m2 IV every 6 hours
For methotrexate levels of ≥10 to <100 micromolar at 48 hours, leucovorin is dosed at 100 mg/m2 IV every 3 hours
For methotrexate levels of ~1 to 10 micromolar at 48 hours, leucovorin is dosed at 100 mg/m2 IV every 6 hours or 10 mg/m2 IV or orally to 100 mg/m2 IV every 3 hours
At 72 hours:
For methotrexate levels of ≥10 micromolar at 72 hours, leucovorin is dosed at 100 to 1,000 mg/m2 IV every 3 to 6 hours
For methotrexate levels of ~1 to 10 micromolar at 72 hours, leucovorin is dosed at 10 mg/m2 IV or orally to 100 mg/m2 IV every 3 hours
For methotrexate levels of ~0.1 to 1 micromolar at 72 hours, leucovorin is dosed at 10 mg/m2 IV or orally every 3 to 6 hours
If serum creatinine is increased more than 50% above baseline, increase the standard leucovorin dose to 100 mg/m2 IV every 3 hours, then adjust according to methotrexate levels above.
Follow methotrexate levels daily, leucovorin may be discontinued when methotrexate level is <0.1 micromolar
Dosing: Obesity
ASCO Guidelines for appropriate chemotherapy dosing in obese adults with cancer (excludes leukemias): Utilize patient's actual body weight (full weight) for calculation of body surface area- or weight-based dosing, particularly when the intent of therapy is curative; manage regimen-related toxicities in the same manner as for nonobese patients; if a dose reduction is utilized due to toxicity, consider resumption of full weight-based dosing with subsequent cycles, especially if cause of toxicity (eg, hepatic or renal impairment) is resolved (Griggs 2012).
Reconstitution
Use preservative-free preparations for intrathecal or high-dose methotrexate administration.
IV: Dilute powder with D5W or NS to a concentration of ≤25 mg/mL (20 mg and 50 mg vials) and 50 mg/mL (1 g vial). May further dilute in D5W or NS.
Intrathecal: Prepare intrathecal solutions with preservative-free NS, lactated Ringer's, or Elliot's B solution to a final volume of up to 12 mL (volume generally based on institution or practitioner preference). Intrathecal methotrexate concentrations may be institution specific or based on practitioner preference, generally ranging from a final concentration of 1 mg/mL (per prescribing information; Grossman 1993; Lin 2008) up to ~2 to 4 mg/mL (de Lemos 2009; Glantz 1999). For triple intrathecal therapy (methotrexate 12 mg/hydrocortisone 24 mg/cytarabine 36 mg), preparation to final volume of 12 mL is reported (Lin 2008). Intrathecal medications should NOT be prepared during the preparation of any other agents.
Administration
Doses ≥250 mg/m2 (IV) are associated with moderate emetic potential; antiemetics may be recommended to prevent nausea and vomiting.
Methotrexate may be administered orally, IM, IV, intrathecally, or SubQ; IV administration may be as slow push (10 mg/minute), bolus infusion, or 24-hour continuous infusion (route and rate of administration depend on indication and/or protocol; refer to specific references). Must use preservative-free formulation for intrathecal or high-dose methotrexate administration.
When administered IM for indications that may terminate a pregnancy, also consult local policies or regulations related to administration.
Specific dosing schemes vary, but high doses should be followed by leucovorin calcium rescue to prevent toxicity.
Oral solution: Ensure accuracy when dispensing and administering to prevent dosing errors. A calibrated oral syringe/dosing cup that can measure and deliver the prescribed dose accurately should be used; do not use a household teaspoon or tablespoon to measure dose.
Otrexup and Rasuvo are autoinjectors for once weekly subcutaneous use in the abdomen or thigh; patient may self-administer after appropriate training. All schedules should be continually tailored to the individual patient. An initial test dose may be given prior to the regular dosing schedule to detect any extreme sensitivity to adverse effects.
Dietary Considerations
Some products may contain sodium.
Storage
Injection: Note: Follow USP 797 recommendations for beyond use dates based on the level of risk for preparation.
IV: Store intact vials and autoinjectors between 20°C and 25°C (68°F and 77°F); excursions may be permitted between 15°C and 30°C (59°F and 86°F). Protect from light. Solution diluted in D5W or NS is stable for 24 hours at room temperature (21°C to 25°C).
Intrathecal: Intrathecal dilutions are preservative free and should be used as soon as possible after preparation. After preparation, store intrathecal medications (until use) in an isolated location or container clearly marked with a label identifying as "intrathecal" use only.
Oral:
Tablets: Store between 20°C and 25°C (68°F and 77°F). Protect from light.
Oral solution: Store at 2°C to 8°C (36°F to 46°F) in a tightly closed container. Patients may store either refrigerated (2°C to 8°C [36°F to 46°F]) or for up to 60 days at room temperature (20°C to 25°C [68°F to 77°F]). Excursions permitted to 15°C to 30°C (59°F to 86°F). Avoid freezing and excessive heat.
Methotrexate Images
Drug Interactions
Acitretin: May enhance the hepatotoxic effect of Methotrexate. Avoid combination
Alcohol (Ethyl): May enhance the hepatotoxic effect of Methotrexate. Management: Limit alcohol consumption in patients taking methotrexate. The use of methotrexate for the treatment of psoriasis or rheumatoid arthritis is contraindicated in patients with alcoholism or alcoholic liver disease. Consider therapy modification
Alitretinoin (Systemic): May enhance the hepatotoxic effect of Methotrexate. Monitor therapy
Baricitinib: Immunosuppressants may enhance the immunosuppressive effect of Baricitinib. Management: Use of baricitinib in combination with potent immunosuppressants such as azathioprine or cyclosporine is not recommended. Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted. Consider therapy modification
BCG (Intravesical): Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG (Intravesical): Myelosuppressive Agents may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Bile Acid Sequestrants: May decrease the absorption of Methotrexate. Monitor therapy
Cephalothin: May diminish the therapeutic effect of Methotrexate. Monitor therapy
Chloramphenicol (Ophthalmic): May enhance the adverse/toxic effect of Myelosuppressive Agents. Monitor therapy
Ciprofloxacin (Systemic): May increase the serum concentration of Methotrexate. Monitor therapy
Cladribine: May enhance the immunosuppressive effect of Immunosuppressants. Avoid combination
Cladribine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Avoid combination
CloZAPine: Myelosuppressive Agents may enhance the adverse/toxic effect of CloZAPine. Specifically, the risk for neutropenia may be increased. Monitor therapy
Coccidioides immitis Skin Test: Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. Monitor therapy
CycloSPORINE (Systemic): May increase the serum concentration of Methotrexate. This may result in nausea, vomiting, oral ulcers, hepatotoxicity and/or nephrotoxicity. Methotrexate may increase the serum concentration of CycloSPORINE (Systemic). This may result in nephrotoxicity. Consider therapy modification
Deferiprone: Myelosuppressive Agents may enhance the neutropenic effect of Deferiprone. Management: Avoid the concomitant use of deferiprone and myelosuppressive agents whenever possible. If this combination cannot be avoided, monitor the absolute neutrophil count more closely. Consider therapy modification
Denosumab: May enhance the adverse/toxic effect of Immunosuppressants. Specifically, the risk for serious infections may be increased. Monitor therapy
Dexketoprofen: May increase the serum concentration of Methotrexate. Management: Concurrent use of dexketoprofen with methotrexate doses of 15 mg/week or more is inadvisable. Use with lower methotrexate doses should only be performed with caution and increased monitoring. Consider therapy modification
Dichlorphenamide: May increase the serum concentration of Methotrexate. Avoid combination
Diethylamine Salicylate: May increase the serum concentration of Methotrexate. Monitor therapy
Dipyrone: May enhance the adverse/toxic effect of Methotrexate. Methotrexate may enhance the adverse/toxic effect of Dipyrone. Specifically, the risk for agranulocytosis and pancytopenia may be increased. Avoid combination
Echinacea: May diminish the therapeutic effect of Immunosuppressants. Consider therapy modification
Eltrombopag: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. Monitor therapy
Erdafitinib: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Fingolimod: Immunosuppressants may enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). Consider therapy modification
Foscarnet: May enhance the nephrotoxic effect of Methotrexate. Avoid combination
Fosphenytoin-Phenytoin: Methotrexate may decrease the serum concentration of Fosphenytoin-Phenytoin. Fosphenytoin-Phenytoin may increase the serum concentration of Methotrexate. Specifically, fosphenytoin-phenytoin may displace methotrexate from serum proteins, increasing the concentration of free, unbound drug. Monitor therapy
Gemfibrozil: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. See separate drug interaction monographs for agents listed as exceptions. Monitor therapy
Ibrutinib: May increase the serum concentration of Methotrexate. Monitor therapy
Lasmiditan: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Avoid combination
Leflunomide: Methotrexate may enhance the adverse/toxic effect of Leflunomide. Particular concerns are an increased risk of pancytopenia and/or hepatotoxicity. Monitor therapy
Lenograstim: Antineoplastic Agents may diminish the therapeutic effect of Lenograstim. Management: Avoid the use of lenograstim 24 hours before until 24 hours after the completion of myelosuppressive cytotoxic chemotherapy. Consider therapy modification
LevETIRAcetam: May increase the serum concentration of Methotrexate. Monitor therapy
Lipegfilgrastim: Antineoplastic Agents may diminish the therapeutic effect of Lipegfilgrastim. Management: Avoid concomitant use of lipegfilgrastim and myelosuppressive cytotoxic chemotherapy. Lipegfilgrastim should be administered at least 24 hours after the completion of myelosuppressive cytotoxic chemotherapy. Consider therapy modification
Loop Diuretics: Methotrexate may diminish the therapeutic effect of Loop Diuretics. Loop Diuretics may increase the serum concentration of Methotrexate. Methotrexate may increase the serum concentration of Loop Diuretics. Management: Monitor for increased methotrexate and/or loop diuretic levels/toxicity with concomitant use of these agents and monitor for decreased therapeutic effects of loop diuretics. Methotrexate and/or loop diuretic dose reductions may be necessary. Consider therapy modification
Lumacaftor and Ivacaftor: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. Lumacaftor and Ivacaftor may increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Mercaptopurine: Methotrexate may increase the serum concentration of Mercaptopurine. Conversely, intracellular concentrations of thioguanine nucleotides may be decreased with the combination. Monitor therapy
Mesalamine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Mipomersen: May enhance the hepatotoxic effect of Methotrexate. Monitor therapy
Natalizumab: Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. Avoid combination
Nitisinone: May increase the serum concentration of OAT1/3 Substrates. Monitor therapy
Nitrous Oxide: May enhance the adverse/toxic effect of Methotrexate. Avoid combination
Nivolumab: Immunosuppressants may diminish the therapeutic effect of Nivolumab. Consider therapy modification
Nonsteroidal Anti-Inflammatory Agents: May increase the serum concentration of Methotrexate. Management: Alternative anti-inflammatory therapy should be considered whenever possible, especially if the patient is receiving higher, antineoplastic doses of methotrexate. Consider therapy modification
Ocrelizumab: May enhance the immunosuppressive effect of Immunosuppressants. Monitor therapy
Palifermin: May enhance the adverse/toxic effect of Antineoplastic Agents. Specifically, the duration and severity of oral mucositis may be increased. Management: Do not administer palifermin within 24 hours before, during infusion of, or within 24 hours after administration of myelotoxic chemotherapy. Consider therapy modification
Penicillins: May increase the serum concentration of Methotrexate. Monitor therapy
P-glycoprotein/ABCB1 Inducers: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inducers may also further limit the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
P-glycoprotein/ABCB1 Inhibitors: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inhibitors may also enhance the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
Pidotimod: Immunosuppressants may diminish the therapeutic effect of Pidotimod. Monitor therapy
Pimecrolimus: May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Pretomanid: May increase the serum concentration of OAT1/3 Substrates. Monitor therapy
Probenecid: May increase the serum concentration of Methotrexate. Management: Avoid concomitant use of probenecid and methotrexate if possible. If used together, consider lower methotrexate doses and monitor for evidence of methotrexate toxicity. Consider therapy modification
Promazine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Proton Pump Inhibitors: May increase the serum concentration of Methotrexate. Monitor therapy
Pyrimethamine: May enhance the adverse/toxic effect of Methotrexate. Monitor therapy
Ranolazine: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Roflumilast: May enhance the immunosuppressive effect of Immunosuppressants. Consider therapy modification
Salicylates: May increase the serum concentration of Methotrexate. Salicylate doses used for prophylaxis of cardiovascular events are not likely to be of concern. Consider therapy modification
Sapropterin: Methotrexate may decrease the serum concentration of Sapropterin. Specifically, methotrexate may decrease tissue concentrations of tetrahydrobiopterin. Monitor therapy
Siponimod: Immunosuppressants may enhance the immunosuppressive effect of Siponimod. Monitor therapy
Sipuleucel-T: Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. Consider therapy modification
SulfaSALAzine: May enhance the hepatotoxic effect of Methotrexate. Monitor therapy
Sulfonamide Antibiotics: May enhance the adverse/toxic effect of Methotrexate. Management: Consider avoiding concomitant use of methotrexate and therapeutic doses of sulfonamides (eg, trimethoprim/sulfamethoxazole). Patients receiving prophylactic doses of trimethoprim/sulfamethoxazole and methotrexate should be carefully monitored. Consider therapy modification
Tacrolimus (Topical): May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Tegafur: Methotrexate may enhance the adverse/toxic effect of Tegafur. Monitor therapy
Teriflunomide: May increase the serum concentration of OAT1/3 Substrates. Monitor therapy
Teriflunomide: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. Monitor therapy
Tertomotide: Immunosuppressants may diminish the therapeutic effect of Tertomotide. Monitor therapy
Theophylline Derivatives: Methotrexate may increase the serum concentration of Theophylline Derivatives. Monitor therapy
Tofacitinib: Methotrexate may enhance the immunosuppressive effect of Tofacitinib. Management: Avoid the use of tofacinib in combination with potent immunosuppressive methotrexate-containing regimens. Monitor therapy
Tolvaptan: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. Consider therapy modification
Tolvaptan: May increase the serum concentration of OAT1/3 Substrates. Management: Patients being treated with the Jynarque brand of tolvaptan should avoid concomitant use of OAT1/3 substrates. Concentrations and effects of the OAT1/3 substrate would be expected to increase with any combined use. Consider therapy modification
Trastuzumab: May enhance the neutropenic effect of Immunosuppressants. Monitor therapy
Trimethoprim: May enhance the adverse/toxic effect of Methotrexate. Management: Consider avoiding concomitant use of methotrexate and either sulfamethoxazole or trimethoprim. If used concomitantly, monitor for the development of signs and symptoms of methotrexate toxicity (e.g., bone marrow suppression). Consider therapy modification
Upadacitinib: Methotrexate may enhance the immunosuppressive effect of Upadacitinib. Monitor therapy
Vaccines (Inactivated): Immunosuppressants may diminish the therapeutic effect of Vaccines (Inactivated). Management: Vaccine efficacy may be reduced. Complete all age-appropriate vaccinations at least 2 weeks prior to starting an immunosuppressant. If vaccinated during immunosuppressant therapy, revaccinate at least 3 months after immunosuppressant discontinuation. Consider therapy modification
Vaccines (Live): Methotrexate may enhance the adverse/toxic effect of Vaccines (Live). Methotrexate may diminish the therapeutic effect of Vaccines (Live). Management: Low-dose methotrexate (0.4 mg/kg/week or less) is not considered sufficiently immunosuppressive to create vaccine safety concerns. Higher doses of methotrexate should be avoided. Consider therapy modification
Adverse Reactions
Note: Adverse reactions vary by route and dosage. Frequency not always defined.
Cardiovascular: Arterial thrombosis, cerebral thrombosis, chest pain, deep vein thrombosis, hypotension, pericardial effusion, pericarditis, plaque erosion (psoriasis), pulmonary embolism, retinal thrombosis, thrombophlebitis, vasculitis
Central nervous system: Dizziness (≤3%), headache (pJIA 1%), abnormal cranial sensation, brain disease, chemical arachnoiditis (intrathecal; acute), chills, cognitive dysfunction (has been reported at low dosage), drowsiness, fatigue, leukoencephalopathy (intravenous administration after craniospinal irradiation or repeated high-dose therapy; may be chronic), malaise, mood changes (has been reported at low dosage), neurological signs and symptoms (at high dosages; including confusion, hemiparesis, transient blindness, seizures, and coma), severe neurotoxicity (reported with unexpectedly increased frequency among pediatric patients with acute lymphoblastic leukemia who were treated with intermediate-dose intravenous methotrexate), speech disturbance
Dermatologic: Alopecia (≤10%), burning sensation of skin (psoriasis 3% to 10%), skin photosensitivity (3% to 10%), skin rash (≤3%), dermatitis (rheumatoid arthritis 1% to 3%), pruritus (rheumatoid arthritis 1% to 3%), acne vulgaris, dermal ulcer, diaphoresis, ecchymoses, erythema multiforme, erythematous rash, exfoliative dermatitis, furunculosis, hyperpigmentation, hypopigmentation, skin abnormalities related to radiation recall, skin necrosis, Stevens-Johnson syndrome, telangiectasia, toxic epidermal necrolysis, urticaria
Endocrine & metabolic: Decreased libido, decreased serum albumin, diabetes mellitus, gynecomastia, menstrual disease
Gastrointestinal: Diarrhea (≤11%), nausea and vomiting (≤11%), stomatitis (2% to 10%), abdominal distress, anorexia, aphthous stomatitis, enteritis, gastrointestinal hemorrhage, gingivitis, hematemesis, intestinal perforation, melena, pancreatitis
Genitourinary: Azotemia, cystitis, defective oogenesis, defective spermatogenesis, dysuria, hematuria, impotence, infertility, oligospermia, proteinuria, severe renal disease, vaginal discharge
Hematologic & oncologic: Thrombocytopenia (rheumatoid arthritis 3% to 10%; platelet count <100,000/mm3), leukopenia (1% to 3%; WBC <3000/mm3), pancytopenia (rheumatoid arthritis 1% to 3%), agranulocytosis, anemia, aplastic anemia, bone marrow depression (nadir: 7-10 days), decreased hematocrit, eosinophilia, gastric ulcer, hypogammaglobulinemia, lymphadenopathy, lymphoma, lymphoproliferative disorder, neutropenia, non-Hodgkin’s lymphoma (in patients receiving low-dose oral methotrexate), tumor lysis syndrome
Hepatic: Increased liver enzymes (14% to 15%), cirrhosis (chronic therapy), hepatic failure, hepatic fibrosis (chronic therapy), hepatitis (acute), hepatotoxicity
Hypersensitivity: Anaphylactoid reaction
Infection: Cryptococcosis, cytomegalovirus disease (including cytomegaloviral pneumonia, sepsis, nocardiosis), herpes simplex infection, herpes zoster, histoplasmosis, infection, vaccinia (disseminated; following smallpox immunization)
Neuromuscular & skeletal: Arthralgia, myalgia, myelopathy (subacute), osteonecrosis (with radiotherapy), osteoporosis
Ophthalmic: Blurred vision, conjunctivitis, eye pain, visual disturbance
Otic: Tinnitus
Renal: Renal failure
Respiratory: Interstitial pneumonitis (rheumatoid arthritis 1%), chronic obstructive pulmonary disease, cough, epistaxis, pharyngitis, pneumonia (including Pneumocystis jirovecii), pulmonary alveolitis, pulmonary disease, pulmonary fibrosis, respiratory failure, upper respiratory tract infection
Miscellaneous: Fever, nodule, tissue necrosis
<1%, postmarketing, and/or case reports: Acute respiratory distress (Morgan 2011), bone fracture (stress), cerebrovascular accident (Morgan 2011), mesenteric ischemia (acute; Morgan 2011)
Warnings/Precautions
Concerns related to adverse effects:
- Acute renal failure: May cause renal damage leading to acute renal failure, especially with high-dose methotrexate; monitor renal function and methotrexate levels closely, maintain adequate hydration and urinary alkalinization. Use with caution in osteosarcoma patients treated with high-dose methotrexate in combination with nephrotoxic chemotherapy (eg, cisplatin).
- Bone marrow suppression: [US Boxed Warning]: Unexpectedly severe (sometimes fatal) bone marrow suppression and aplastic anemia have been reported with concomitant administration of methotrexate (usually in high dosage) along with some nonsteroidal anti-inflammatory drugs (NSAIDs); anemia, pancytopenia, leukopenia, neutropenia, and/or thrombocytopenia may occur. Monitor blood counts. Use with caution in patients with preexisting bone marrow suppression. Discontinue treatment (immediately) in rheumatoid arthritis (RA) or psoriasis if a significant decrease in hematologic components is noted.
- CNS effects: May cause neurotoxicity. Leukoencephalopathy has been reported (case reports), usually in patients who have received cranial irradiation and IV methotrexate. Chronic leukoencephalopathy has been reported with high-dose methotrexate (with leucovorin rescue and even without cranial irradiation) and with intrathecal methotrexate; discontinuing methotrexate does not always result in complete recovery; may be progressive and fatal. Serious neurotoxicity, including generalized and focal seizures has occurred (usually in pediatric ALL patients receiving intermediate-dose (1 g/m2 IV methotrexate); leukoencephalopathy and/or microangiopathic calcifications were noted on diagnostic imaging studies in symptomatic patients. A transient acute stroke-like encephalopathy has been observed, usually with high-dose regimens; manifestations may include confusion, hemiparesis, transient blindness, seizure, and coma. Chemical arachnoiditis (headache, back pain, nuchal rigidity, fever) and myelopathy may result from intrathecal administration. May cause dizziness and fatigue; may affect the ability to drive or operate heavy machinery.
- Dermatologic toxicity: [US Boxed Warning]: Severe, occasionally fatal skin reactions have been reported following single or multiple doses of methotrexate. Reactions have occurred within days of oral, intramuscular, intravenous, or intrathecal methotrexate administration. Recovery has been reported with discontinuation of therapy. Severe dermatologic reactions have included toxic epidermal necrolysis, Stevens-Johnson syndrome, exfoliative dermatitis, skin necrosis, and erythema multiforme; discontinue methotrexate if severe reactions occur. Radiation recall dermatitis and sunburn may be precipitated by methotrexate administration. Psoriatic lesions may be worsened by concomitant exposure to ultraviolet radiation.
- Gastrointestinal toxicity: [US Boxed Warning]: Gastrointestinal toxicity may occur (may be unexpectedly severe, usually occurs with high doses along with concomitant use of some NSAIDs); diarrhea and ulcerative stomatitis may require treatment interruption; otherwise hemorrhagic enteritis and death from intestinal perforation may occur. Diarrhea or stomatitis may also require discontinuation. Use with caution in patients with peptic ulcer disease or ulcerative colitis; the risk of GI adverse effects may be increased. In pediatrics, doses ≥12 g/m2 (IV) are associated with a high emetic potential, while a 5 g/m2 (IV) dose is associated with a moderate emetic potential (Dupuis 2011; Paw Cho Sing 2019); doses ≥250 mg/m2 (IV) in adults are associated with moderate emetic potential. Antiemetics may be recommended to prevent nausea and vomiting.
- Hepatotoxicity: [US Boxed Warning]: Methotrexate causes hepatotoxicity, fibrosis, and cirrhosis, but generally only after prolonged use. Acutely, liver enzyme elevations are frequently seen. These are usually transient and asymptomatic, and also do not appear predictive of subsequent hepatic disease. Liver biopsy after sustained use often shows histologic changes, and fibrosis and cirrhosis have been reported; these latter lesions often are not preceded by symptoms or abnormal liver function tests in the psoriasis population. For this reason, periodic liver biopsies are usually recommended for psoriatic patients who are under long-term treatment. Persistent abnormalities in liver function tests may precede appearance of fibrosis or cirrhosis in the rheumatoid arthritis population. Risk is related to cumulative dose (≥1.5 g) and prolonged exposure. Monitor closely (with liver function tests, including serum albumin) for liver toxicities. Liver enzyme elevations may be noted, but may not be predictive of hepatic disease in long term treatment for psoriasis (but generally is predictive in RA treatment). Discontinue methotrexate with moderate to severe change in liver biopsy. Risk factors for hepatotoxicity include history of above moderate ethanol consumption, persistent abnormal liver chemistries, history of chronic liver disease (including hepatitis B or C), family history of inheritable liver disease, diabetes, obesity, hyperlipidemia, lack of folate supplementation during methotrexate therapy, cumulative methotrexate dose exceeding 1.5 g, continuous daily methotrexate dosing, history of significant exposure to hepatotoxic drugs, and advanced age. Use with caution with preexisting liver impairment; may require dosage reduction. Use with caution when used with other hepatotoxic agents (azathioprine, retinoids, sulfasalazine).
- Hypersensitivity: Anaphylaxis may occur; if anaphylaxis or other serious hypersensitivity reaction occurs, discontinue methotrexate immediately and institute appropriate management.
- Infections: [US Boxed Warning]: Immune suppression may lead to potentially fatal opportunistic infections, including Pneumocystis jirovecii pneumonia (PCP). Methotrexate use increases the risk for developing life-threatening or fatal bacterial, fungal, or viral infections, including invasive fungal infections, hepatitis B reactivation, tuberculosis (primary infection or reactivation), disseminated herpes zoster infection and/or cytomegalovirus infection. Use methotrexate with extreme caution in patients with an active infection (contraindicated in patients with immunodeficiency syndrome). Monitor for signs/symptoms of infection during and after treatment; manage promptly if infections occurs. Dose reduction or discontinuation may be necessary for serious infection.
- Pneumonitis: [US Boxed Warning]: Methotrexate-induced lung disease, including acute or chronic interstitial pneumonitis, is a potentially dangerous lesion, which may occur acutely at any time during therapy and has been reported at low doses. It is not always fully reversible and fatalities have been reported. Pulmonary symptoms (especially a dry, nonproductive cough) may require interruption of treatment and careful investigation. Pulmonary symptoms may occur at any time during therapy and at any dosage; monitor closely for pulmonary symptoms, particularly dry, nonproductive cough. Other potential symptoms include fever, dyspnea, hypoxemia, or pulmonary infiltrate.
- Secondary malignancy: [US Boxed Warning]: Malignant lymphomas, which may regress following withdrawal of methotrexate, may occur in patients receiving low-dose methotrexate and, thus, may not require cytotoxic treatment. Discontinue methotrexate first and, if the lymphoma does not regress, appropriate treatment should be instituted. Other secondary tumors have been reported.
- Tumor lysis syndrome: [US Boxed Warning]: Tumor lysis syndrome may occur in patients with high tumor burden; appropriate supportive and pharmacologic measures may prevent or alleviate tumor lysis syndrome.
Disease-related concerns:
- Ascites/pleural effusions: [US Boxed Warning]: Elimination is reduced in patients with ascites and/or pleural effusions; resulting in prolonged half-life and toxicity; may require dose reduction or discontinuation. Monitor closely for toxicity.
- Hepatic impairment: Use with caution in patients with preexisting liver impairment.
- Peptic ulcer disease: Use with caution in patients with peptic ulcer disease; diarrhea and stomatitis may occur.
- Renal impairment: [US Boxed Warning]: Methotrexate elimination is reduced in patients with renal impairment; monitor closely for toxicity; may require dose reduction or, in some cases, discontinuation of methotrexate administration.
- Ulcerative colitis: Use with caution in patients with ulcerative colitis; diarrhea and stomatitis may occur.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
- Hepatotoxic agents: Use caution when used with other hepatotoxic agents (azathioprine, retinoids, sulfasalazine).
- Mercaptopurine: Methotrexate may increase the levels and effects of mercaptopurine; may require dosage adjustments.
- Nephrotoxic chemotherapy: Use with caution in osteosarcoma patients treated with high-dose methotrexate in combination with nephrotoxic chemotherapy (eg, cisplatin).
- NSAIDs: Do not administer NSAIDs prior to or during high dose methotrexate therapy; may increase and prolong serum methotrexate levels. Doses used for psoriasis may still lead to unexpected toxicities; use with caution when administering NSAIDs or salicylates with lower doses of methotrexate for RA.
- Proton pump inhibitors: Concomitant use of proton pump inhibitors with methotrexate (primarily high-dose methotrexate) may elevate and prolong serum methotrexate levels and metabolite (hydroxymethotrexate) levels (based on case reports and pharmacokinetic studies). May lead to toxicities; use with caution.
- Vaccines: Immunization may be ineffective during methotrexate treatment. Immunization with live vaccines is not recommended; cases of disseminated vaccinia infections due to live vaccines have been reported.
- Vitamins: Vitamins containing folate may decrease response to systemic methotrexate; folate deficiency may increase methotrexate toxicity.
Special populations:
- Elderly: Use caution and monitor closely in elderly patients; increased risk of toxicity.
- Pregnancy: [US Boxed Warning]: Methotrexate can cause embryo-fetal toxicity, including fetal death. Use in RA, polyarticular-course juvenile idiopathic arthritis, and psoriasis is contraindicated in pregnancy. Consider the benefits and risks of methotrexate and risks to the fetus when prescribing methotrexate to a pregnant patient with a neoplastic disease. Verify the pregnancy status of females of reproductive potential prior to initiating therapy. Advise females and males of reproductive potential to use effective contraception during and after treatment with methotrexate.
- Radiotherapy recipients: [US Boxed Warning]: Concomitant methotrexate administration with radiotherapy may increase the risk of soft tissue necrosis and osteonecrosis.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol with caution in neonates. See manufacturer's labeling.
- Intrathecal and high-dose therapy: [US Boxed Warning]: Use only preservative-free methotrexate formulations and diluents for intrathecal and high-dose therapy. Do NOT use formulations or diluents containing preservatives for intrathecal and high-dose therapy because they contain benzyl alcohol.
Other warnings/precautions:
- Administration schedules: Errors have occurred (some resulting in death) when methotrexate was administered as a “daily” dose instead of a “weekly” dose intended for some indications. The ISMP Targeted Medication Safety Best Practices for Hospitals recommends hospitals use a weekly dosage regimen default for oral methotrexate orders in electronic order entry systems, with a hard stop verification required of appropriate oncology indication for daily orders; manual systems should require clarification of an oncology indication prior to dispensing oral methotrexate for daily administration. Provide patient and/or caregiver education for patients discharged on weekly oral methotrexate; education should include written leaflets that contain clear instructions about the weekly dosing schedule and explain the danger of taking extra doses (ISMP 2018).
- Appropriate use: [US Boxed Warning]: Because of the possibility of serious toxic reactions (which can be fatal), methotrexate should be used only in life threatening neoplastic diseases or in patients with psoriasis or rheumatoid arthritis with severe, recalcitrant, disabling disease which is not adequately responsive to other forms of therapy. Deaths have been reported with the use of methotrexate in the treatment of malignancy, psoriasis, and rheumatoid arthritis. Patients should be closely monitored for bone marrow, liver, lung, skin, and kidney toxicities. Patients should be informed by their physician of the risks involved and be under a physician's care throughout therapy. The use of methotrexate high-dose regimens recommended for osteosarcoma requires meticulous care. High-dose regimens of methotrexate injection for other neoplastic diseases are investigational, and a therapeutic advantage has not been established.
- Experienced physician: [US Boxed Warning]: Should be administered under the supervision of a physician experienced in the use of antimetabolite therapy.
- Intrathecal safety: When used for intrathecal administration, should not be prepared during the preparation of any other agents. After preparation, store intrathecal medications in an isolated location or container clearly marked with a label identifying as "intrathecal" use only. Delivery of intrathecal medications to the patient should only be with other medications intended for administration into the central nervous system (Jacobson 2009).
- Methotrexate overexposure: Glucarpidase is an enzyme that rapidly hydrolyzes extracellular methotrexate into inactive metabolites, allowing for a rapid reduction of methotrexate concentrations. Glucarpidase may be used for methotrexate overexposure; it is approved for the treatment of toxic plasma methotrexate concentrations (>1 micromole/L) in patients with delayed clearance due to renal impairment. Refer to Glucarpidase monograph.
Monitoring Parameters
Evaluate pregnancy status prior to use in females of reproductive potential.
Oncologic uses: Baseline and frequently during treatment: CBC with differential and platelets, serum creatinine, BUN, LFTs; methotrexate levels and urine pH (with high-dose methotrexate); closely monitor fluid and electrolyte status in patients with impaired methotrexate elimination; chest x-ray (baseline); pulmonary function test (if methotrexate-induced lung disease suspected); monitor carefully for toxicities (due to impaired elimination) in patients with ascites, pleural effusion, decreased folate stores, renal impairment, and/or hepatic impairment
Psoriasis (Kalb 2009; Menter 2009):
CBC with differential and platelets (baseline, 7 to 14 days after initiating therapy or dosage increase, every 2 to 4 weeks for first few months, then every 1 to 3 months depending on leukocyte count and stability of patient) monitor more closely in patients with risk factors for hematologic toxicity (eg, renal insufficiency, advanced age, hypoalbuminemia); BUN and serum creatinine (baseline and every 2 to 3 months) calculate glomerular filtration rate if at risk for renal dysfunction; consider PPD for latent TB screening (baseline); LFTs (baseline, monthly for first 6 months, then every 1 to 2 months; more frequently if at risk for hepatotoxicity or if clinically indicated; liver function tests should be performed at least 5 days after the last dose); chest x-ray (baseline if underlying lung disease); pulmonary function test (if methotrexate-induced lung disease suspected)
Liver biopsy for patients with risk factors for hepatotoxicity: Baseline or after 2 to 6 months of therapy and with each 1 to 1.5 g cumulative dose interval
Liver biopsy for patients without risk factors for hepatotoxicity: If persistent elevations in 5 of 9 AST levels during a 12-month period, or decline of serum albumin below the normal range with normal nutritional status. Consider biopsy after cumulative dose of 3.5 to 4 g and after each additional 1.5 g.
Rheumatoid arthritis:
CBC with differential and platelets, serum creatinine, and LFTs: Baseline and every 2 to 4 weeks for 3 months after initiation or following dose increases, then every 8 to 12 weeks during 3 to 6 months of treatment, followed by every 12 weeks beyond 6 months of treatment; monitor more frequently if clinically indicated (Singh [ACR 2016]).
Chest x-ray (within 1 year prior to initiation), Hepatitis B and C serology (if at high risk); tuberculosis testing annually for patients who live, travel or work in areas with likely TB exposure (Kremer 1994).
Liver biopsy: Baseline (consider only for patients with persistent abnormal baseline LFTs, history of alcoholism, or chronic hepatitis B or C) or during treatment if persistent LFT elevations (6 of 12 tests abnormal over 1 year or 5 of 9 results when LFTs performed at 6-week intervals) (Kremer 1994).
Polyarticular-course juvenile idiopathic arthritis: Complete blood counts (at least monthly), renal function (every 1 to 2 months), liver function (every 1 to 2 months). Increase monitoring frequency during initial dosing, dose changes, or during periods of increased risk of elevated methotrexate blood levels (eg, dehydration). Monitor pulmonary function tests if methotrexate-induced lung disease is suspected, especially if baseline values are available.
Crohn disease (off-label use; Lichtenstein 2009): CBC with differential and platelets (baseline and periodic) and liver function tests (baseline and every 1 to 2 months); baseline liver biopsy (in patients with abnormal baseline LFTs or with chronic liver disease); liver biopsy at 1 year if (over a 1-year span) AST consistently elevated or serum albumin consistently decreased; chest x-ray (baseline)
Tubal ectopic pregnancy (off-label use):
Prior to therapy, serial hCG measurements 2 to 7 days apart along with other procedures to exclude the presence of a viable intrauterine pregnancy (ACOG 193 2018; RCOG [Elson 2016]). CBC with differential, liver function tests, serum creatinine, blood type and Rh (ASRM 2013). Evaluate for medical conditions considered absolute contraindications for methotrexate treatment of ectopic pregnancy (ACOG 193 2018).
Single-dose regimen: Post treatment serum hCG levels on days 4 and 7, if decrease is >15%, continue to measure serum hCG weekly until reaching a non-pregnant level. Consider surgical management if serum hCG does not decrease after two doses. If hCG levels plateau or increase during follow-up period, consider methotrexate for treatment of persistent ectopic pregnancy or surgical management (ACOG 193 2018).
Two-dose regimen: Post treatment serum hCG levels on days 4 and 7, if decrease is >15%, continue to measure serum hCG weekly until reaching a non-pregnant level. Consider surgical management if serum hCG does not decrease after four doses. If hCG levels plateau or increase during follow-up period, consider methotrexate for treatment of persistent ectopic pregnancy or surgical management (ACOG 193 2018).
Multidose regimen (in combination with leucovorin): Measure serum hCG on days of methotrexate administration. Once decrease is >15%, continue to measure serum hCG weekly until reaching a non-pregnant level. Consider surgical management if serum hCG does not decrease after four doses. If hCG levels plateau or increase during follow-up period, consider methotrexate for treatment of persistent ectopic pregnancy or surgical management (ACOG 193 2018).
Pregnancy
Pregnancy Risk Factor
X (psoriasis, rheumatoid arthritis)
Pregnancy Considerations
Methotrexate crosses the placenta (Schleuning 1987).
[US Boxed Warning]: Methotrexate can cause embryo-fetal toxicity, including fetal death. Following exposure during the first trimester, methotrexate may increase the risk of spontaneous abortion, skull anomalies, facial dysmorphism, CNS, limb and cardiac abnormalities; intellectual impairment may also occur. Intrauterine growth restriction and functional abnormalities may occur following second or third trimester exposure.
[US Boxed Warning]: Consider the benefits and risks of methotrexate and risks to the fetus when prescribing methotrexate to a pregnant patient with a neoplastic disease. Methotrexate is approved for the treatment of trophoblastic neoplasms (gestational choriocarcinoma, chorioadenoma destruens, and hydatidiform mole). Methotrexate is recommended for the medical management of ectopic pregnancy in appropriately selected patients (ACOG 193 2018; ASRM 2013). Methotrexate has been used for the medical termination of intrauterine pregnancy with a gestational age up to 49 days (ACOG 143 2014).
[US Boxed Warning]: Use in rheumatoid arthritis, polyarticular-course juvenile idiopathic arthritis, and psoriasis is contraindicated in pregnancy. It is currently recommended that females with inflammatory bowel disease, rheumatoid arthritis, or psoriasis discontinue methotrexate 3 months prior to a planned pregnancy (Flint 2016; Mahadevan 2019; Nguyen 2016; Rademaker 2018).
[US Boxed Warning]: Verify the pregnancy status of females of reproductive potential prior to initiating therapy.Advise females and males of reproductive potential to use effective contraception during and after treatment with methotrexate. Effective contraception is recommended for females during therapy and for ≥6 months. Effective contraception is recommended for males during therapy and for ≥3 months after the final dose of methotrexate.
The use of methotrexate may impair fertility and cause menstrual irregularities or oligospermia during treatment and following therapy. It is not known if infertility may be reversed in all affected males or females. Low-dose methotrexate, when used for rheumatoid arthritis, inflammatory bowel disease or psoriasis, is considered compatible for use in male patients planning to father a child (Flint 2016; Lamb 2019; Rademaker 2018).
Patient Education
What is this drug used for?
- It is used to treat cancer.
- It is used to treat rheumatoid arthritis.
- It is used to treat juvenile arthritis.
- It is used to treat psoriasis.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Hair loss
- Nausea
- Vomiting
- Lack of appetite
- Abdominal pain
- Loss of strength and energy
- Common cold symptoms
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes
- Tumor lysis syndrome like fast heartbeat or abnormal heartbeat; any passing out; trouble passing urine; muscle weakness or cramps; nausea, vomiting, diarrhea, or lack of appetite; or feel sluggish
- Infection
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any bleeding that is very bad or that will not stop
- Pancreas problem like pancreatitis; severe abdominal pain, severe back pain, severe nausea, vomiting
- Kidney problems like not able to pass urine, blood in urine, change in amount of urine passed, weight gain
- Liver problems like dark urine, feeling tired, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin or eyes
- Severe pulmonary disorder like lung or breathing problems like trouble breathing, shortness of breath, or a cough that is new or worse.
- Severe cerebrovascular disease like change in strength on one side is greater than the other, trouble speaking or thinking, change in balance, or change in eyesight.
- DVT like edema, warmth, numbness, change in color, or pain in the extremities.
- Pinpoint red spots on skin
- Severe dizziness
- Passing out
- Seizures
- Confusion
- Fatigue
- Vision changes
- Bone pain
- Headache
- Neck rigidity
- Burning or numbness feeling
- Muscle weakness
- Difficulty moving
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.