Boxed Warning
Experienced physician:
Only health care providers experienced in immunosuppressive therapy and management of organ transplant patients should prescribe mycophenolate. Manage patients receiving the drug in facilities equipped and staffed with adequate laboratory and supportive medical resources. The health care provider responsible for maintenance therapy should have complete information requisite for the follow-up of the patient.
Serious infections:
Immunosuppression may lead to increased susceptibility to bacterial, viral, fungal, and protozoal infections, including opportunistic infections and viral reactivation of hepatitis B and C, which may lead to hospitalizations and fatal outcomes.
Malignancies:
Immunosuppression may lead to increased risk of development of lymphoma and other malignancies, particularly of the skin.
Embryo-fetal toxicity:
Use during pregnancy is associated with increased risks of first trimester pregnancy loss and congenital malformations. Avoid if safer treatment options are available. Women of reproductive potential must be counseled regarding pregnancy prevention and planning.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Capsule, Oral, as mofetil:
CellCept: 250 mg [contains fd&c blue #2 (indigotine)]
Generic: 250 mg
Solution Reconstituted, Intravenous, as mofetil hydrochloride:
CellCept Intravenous: 500 mg (1 ea) [contains polysorbate 80]
Generic: 500 mg (1 ea)
Suspension Reconstituted, Oral, as mofetil:
CellCept: 200 mg/mL (160 mL) [contains aspartame, methylparaben, sorbitol, soybean lecithin; mixed fruit flavor]
Generic: 200 mg/mL (160 mL)
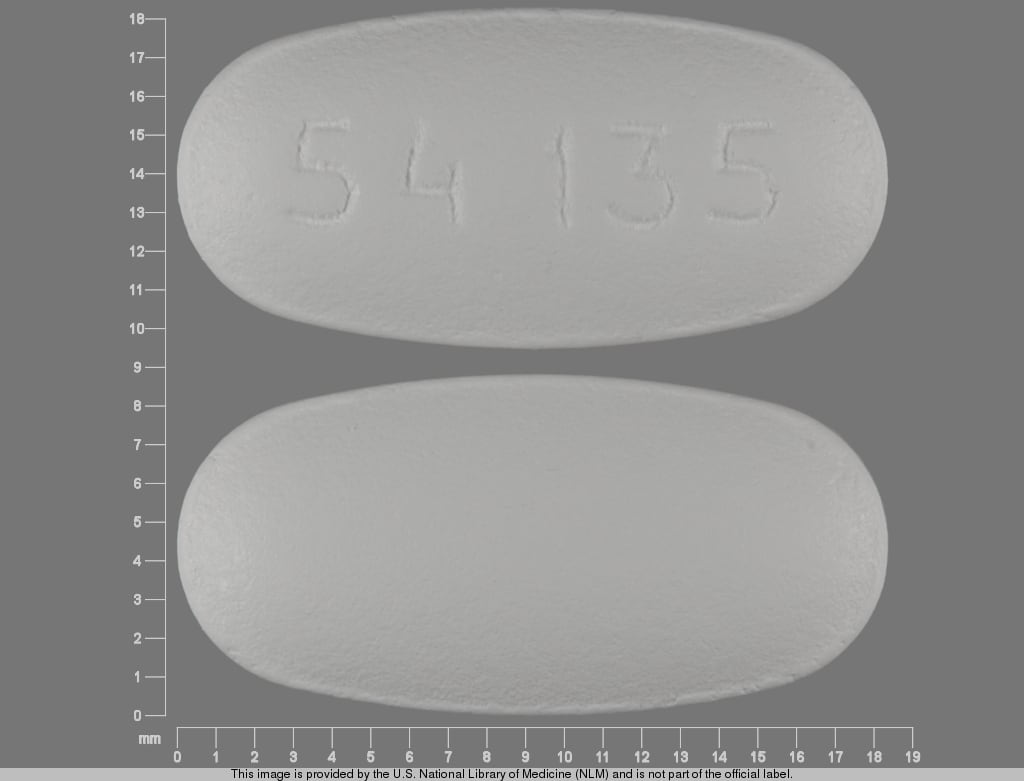
Tablet, Oral, as mofetil:
CellCept: 500 mg [contains fd&c blue #2 aluminum lake]
Generic: 500 mg
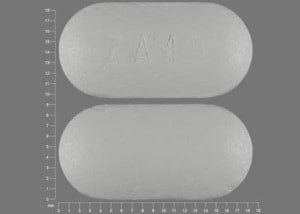
Tablet Delayed Release, Oral, as mycophenolic acid:
Myfortic: 180 mg [contains fd&c blue #2 (indigotine)]
Myfortic: 360 mg
Generic: 180 mg, 360 mg
Pharmacology
Mechanism of Action
MPA exhibits a cytostatic effect on T and B lymphocytes. It is an inhibitor of inosine monophosphate dehydrogenase (IMPDH) which inhibits de novo guanosine nucleotide synthesis. T and B lymphocytes are dependent on this pathway for proliferation.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid and extensive; early post-transplant period mycophenolic acid (MPA) AUC values are lower (~45% to 53%) than later post-transplant period (>3 months) MPA AUC values in both pediatric patients and adults
Oral: Myfortic: 93%
Distribution
CellCept: MPA: ~3.6 ± 1.5 L/kg
Myfortic: MPA: Oral: 54 L (at steady state); 112 L (elimination phase)
Metabolism
Hepatic and via GI tract; CellCept is completely hydrolyzed in the liver to mycophenolic acid (MPA; active metabolite); enterohepatic recirculation of MPA may occur; MPA is glucuronidated to MPAG (inactive metabolite)
Excretion
CellCept: MPA: Urine (<1%), feces (6%); MPAG: Urine (87%)
Myfortic: MPA: Urine (3%), feces; MPAG: Urine (>60%)
Onset of Action
Peak effect: Correlation of toxicity or efficacy is still being developed; however, one study indicated that 12-hour AUCs >40 mcg/mL/hour were correlated with efficacy and decreased episodes of rejection.
Time to Peak
Plasma: Oral: MPA:
CellCept: 1 to 1.5 hours
Myfortic: 1.5 to 2.75 hours
Half-Life Elimination
CellCept: MPA: Oral: 17.9 ± 6.5 hours; IV: 16.6 ± 5.8 hours
Myfortic: MPA: Oral: 8 to16 hours; MPAG: 13 to 17 hours
Protein Binding
MPA: 97%, MPAG 82%
Use in Specific Populations
Special Populations: Renal Function Impairment
CellCept: Mycophenolic acid AUC increased 75%, and mycophenolic acid glucuronide AUC increased 3- to 6-fold in patients with severe renal impairment (glomerular filtration rate [GFR] <25 mL/minute/1.73 m2).
Use: Labeled Indications
Organ transplantation: Prophylaxis of organ rejection in patients receiving allogeneic renal (CellCept [mycophenolate mofetil], Myfortic [enteric-coated mycophenolate sodium]), cardiac (CellCept), or liver (CellCept) transplants, in combination with other immunosuppressants
Note: While traditionally used in combination with cyclosporine, mycophenolate is now used primarily in combination with tacrolimus and, to a lesser extent, with a mammalian target of rapamycin inhibitor (everolimus or sirolimus) for prophylaxis of rejection in renal, cardiac, and hepatic transplants (AASLD [Lucey 2013]; Aliabadi 2012; Eisen 2013; Groetzner 2009; Guethoff 2013; ISHLT [Costanzo 2010]; KDIGO [Chapman 2010]).
Myfortic may also be used to prevent organ rejection in patients receiving cardiac and hepatic transplantations although not labeled for these transplantations (Lehmkuhl 2008; Wang 2015).
Use: Off Label
Acute graft-versus-host disease, refractory (treatment)b
Data from a multicenter, randomized, 4-arm phase II trial in patients with acute graft-versus-host disease (GVHD) who had undergone an allogeneic hematopoietic stem cell transplantation (HSCT) support the use of mycophenolate (in combination with corticosteroids) in the treatment of this condition Alousi 2009. Additional trials may be necessary to further define the role of mycophenolate in this condition.
Autoimmune hepatitis (first-line agent)b
Data from a prospective, open-label, observational study in Greece supports the use of mycophenolate mofetil in combination with corticosteroids as a first-line agent in treatment of autoimmune hepatitis Zachou 2016. Additional trials may be necessary to further define the role of mycophenolate mofetil for first line treatment of this condition.
Autoimmune hepatitis (refractory)yes
Based on the American Association for the Study of Liver Diseases (AASLD) Practice Guidelines: Diagnosis and Management of Autoimmune Hepatitis, mycophenolate mofetil given for the treatment of refractory autoimmune hepatitis is effective and recommended in the management of this condition Manns 2010.
Chronic graft-versus-host disease, refractory (treatment)yes
Based on the American Society for Blood and Marrow Transplant (ASBMT) Consensus Conference on Clinical Practice in Chronic GVHD: Second-Line Treatment of Chronic Graft-versus-Host Disease, mycophenolate is an effective and suitable second-line treatment for this condition.
Graft-versus-host disease (prevention)b
Data from prospective cohort study in patients having undergone allogeneic HSCT treated with mycophenolate (in combination with tacrolimus) support the use of mycophenolate in the prevention of GVHD Sabry 2009. Additional trials may be necessary to further define the role of mycophenolate in this condition.
Lung transplant (prevention of bronchiolitis obliterans syndrome)c
Data from a limited number of clinical trials suggests that mycophenolate in combination with other immunosuppressant medications may be beneficial for prevention of bronchiolitis obliterans syndrome Glanville 2015, McNeil 2006, Speich 2010. Additional data may be necessary to further define the role of mycophenolate in prevention of bronchiolitis obliterans syndrome.
Lung transplant (prevention of rejection)b
Data from several studies and clinical experiences support the use of mycophenolate in combination with other immunosuppressant medications in the prevention of rejection after lung transplant Lama 2003. Additional trials may be necessary to further define the role of mycophenolate in prevention of rejection after lung transplant.
Lupus nephritisayes
Data from a meta-analysis and controlled trials indicate that mycophenolate is as effective as cyclophosphamide for induction therapy and as effective as or superior to azathioprine for maintenance treatment of lupus nephritis Appel 2009, Dooley 2011, Henderson 2013.
Based on the
Myasthenia gravisyes
Based on the Myasthenia Gravis Foundation of America consensus-based guidance for the management of myasthenia gravis, mycophenolate is a recommended immunosuppressive agent in patients with myasthenia gravis who have not met treatment goals after an adequate trial of pyridostigmine. Mycophenolate may be added as monotherapy or in conjunction with glucocorticoids and/or pyridostigmine Meriggioli 2003, Sanders 2016.
Psoriasis (moderate to severe)yes
Based on the American Academy of Dermatology, Guidelines of Care for the Management of Psoriasis and Psoriatic Arthritis, mycophenolate given for the treatment of psoriasis is effective and recommended in the management of this condition Menter 2009.
Systemic sclerosis (scleroderma)c
Data from a limited number of observational clinical studies and case series suggest that mycophenolate may be beneficial for the treatment of systemic sclerosis, specifically for improving skin involvement and stabilizing pulmonary function and fibrosis Derk 2009, Gerbino 2008, Henes 2013, Herrick 2017, Le 2011, Mendoza 2012, Nihtyanova 2007, Simeon-Aznar 2011, Yilmaz 2014. One randomized controlled, double-blind trial in patients with scleroderma-related interstitial lung disease showed an improvement in lung function, measured by percent change in forced vital capacity from baseline, in patients receiving mycophenolate mofetil Tashkin 2016. Additional trials may be necessary to further define the role of mycophenolate in this condition.
Contraindications
Hypersensitivity to mycophenolate mofetil, mycophenolic acid, mycophenolate sodium, or any component of the formulation
CellCept: Intravenous formulation is also contraindicated in patients who are allergic to polysorbate 80 (Tween)
Canadian labeling: Additional contraindications (not in the US labeling): Pregnancy; women of childbearing potential and not using highly effective contraceptive methods; women of childbearing potential not providing a pregnancy test result; breastfeeding
Dosage and Administration
Dosing: Adult
Note: Mycophenolate mofetil (CellCept) and enteric-coated mycophenolate sodium (Myfortic) are not equivalent. Conversion to equimolar doses is necessary. Myfortic 180 mg is considered equivalent to CellCept 250 mg (Budde 2004a; Salvadori 2004).
Autoimmune hepatitis, first-line (off-label use): CellCept: Oral: Initial: 500 mg twice daily for 3 weeks; gradually increase to 1.5 to 2 g/day (in combination initially with an oral corticosteroid [eg, prednisolone]); in the study, mycophenolate was continued for at least 2 years after a complete response (Zachou 2016).
Autoimmune hepatitis, refractory (off-label use): CellCept: Oral: 2 g/day given in divided doses (added to a combination of a corticosteroid and a calcineurin inhibitor) (AASLD [Manns 2010])
Cardiac transplantation:
Oral:
CellCept: Initial: 1.5 g twice daily in combination with cyclosporine and initially with corticosteroids (Eisen 2005; Kobashigawa 2006) or 1 g twice daily in combination with other immunosuppressants (tacrolimus, everolimus, or sirolimus) and initially with corticosteroids (Andreassen 2014; Kaczmarek 2013; Monchaud 2009)
Myfortic (off-label use): Initial: 1.08 g twice daily in combination with cyclosporine and initially with corticosteroids (Hummel 2007; Kobashigawa 2006; Lehmkuhl 2008). Although data do not exist for combination with tacrolimus, everolimus, or sirolimus, use of lower equimolar doses (eg, 720 mg twice daily) to mycophenolate mofetil may be appropriate when used with these other immunosuppressants; higher maintenance doses of 1.08 g twice daily may be required in some patients.
IV: CellCept: See oral dosing for CellCept; IV and oral doses (of mycophenolate mofetil) are equivalent. If converting from Myfortic to IV CellCept, convert Myfortic to equivalent CellCept oral dose first. Transition to oral therapy as soon as tolerated.
Liver transplantation:
Oral:
CellCept: Initial: 1.5 g twice daily when used in combination with cyclosporine or 1 g twice daily when used in combination with other immunosuppressants (eg, tacrolimus) (Eckhoff 1998; Nashan 2009). Maintenance doses vary based on concomitant immunosuppression.
Myfortic (off-label use): 360 mg to 720 mg twice daily in combination with other immunosuppressants (Cantisani 2006; Doria 2009; Lopez-Solis 2014; Toledo 2012; Wang 2015). Higher maintenance doses of 1.08 g twice daily may be required in some patients.
Note: At a minimum of 6 months post-liver transplant in order to avoid toxicities associated with calcineurin inhibitors, may convert gradually from calcineurin inhibitor based immunosuppression to mycophenolate monotherapy over a 2 to 3 month period (Schlitt 2001; Schmeding 2011). Mycophenolate may serve as a safe long-term immunosuppressant in a subgroup of patients (eg, patients with renal insufficiency).
IV: CellCept: See oral dosing for CellCept; IV and oral doses (of mycophenolate mofetil) are equivalent. After transplantation, the manufacturer recommends an initial IV dose of 1 g twice daily (based on clinical trial protocol) (Weisner 2001). Transition to oral therapy as soon as tolerated.
Lung transplantation (prevention of rejection and bronchiolitis obliterans syndrome) (off-label use):
Oral:
CellCept: Initial: 1.5 g twice daily when used in combination with cyclosporine and initially with corticosteroids (Speich 2010) or 1 g twice daily when used in combination with other immunosuppressants (eg, tacrolimus) and initially with corticosteroids (Treede 2001; Zuckermann 2003). Higher maintenance doses of 1.5 g twice daily may be required in some patients.
Myfortic: Initial: 1.08 g twice daily in combination with cyclosporine and initially with corticosteroids (Glanville 2015). Although data do not exist for combination with tacrolimus, everolimus, or sirolimus, use of lower equimolar doses (eg, 720 mg twice daily) to mycophenolate mofetil may be appropriate when used with these other immunosuppressants. Higher maintenance doses of 1.08 g twice daily may be required in some patients.
IV: See oral dosing for CellCept; IV and oral doses (of mycophenolate mofetil) are equivalent. If converting from Myfortic to IV CellCept, convert Myfortic to equivalent CellCept oral dose first. Transition to oral therapy as soon as tolerated.
Lupus nephritis (off-label use): CellCept: Oral:
Induction: 1 g twice daily for 6 months in combination with a glucocorticoid (Ong 2005) or 2 to 3 g daily for 6 months in combination with glucocorticoids (Hahn 2012)
Maintenance: 0.5 to 3 g daily (Contreras 2004) or 1 g twice daily (Dooley 2011) or 1 to 2 g daily (Hahn 2012)
Myasthenia gravis (off-label use): Patients who remain significantly symptomatic on pyridostigmine: CellCept: Oral: Initial: 500 mg twice daily; increase based on response and tolerability to a maintenance dose of 1 g to 1.5 g twice daily. May be added as monotherapy or in conjunction with glucocorticoids and/or pyridostigmine (Meriggioli 2003; Sanders 2016). Onset of clinical response to mycophenolate may take up to 6 to 12 months, with a maximum effect not apparent until 1 to 2 years (Sieb 2014).
Psoriasis, moderate to severe (off-label use): CellCept: Oral: 2 to 3 g daily (Menter 2009)
Renal transplantation:
Oral:
CellCept: Initial: 1 g twice daily. Maintenance dose may vary based on concomitant immunosuppression. Doses >2 g/day have been associated with an increased incidence of adverse effects but may be necessary in some patients (EMMC study group 1999; TMMRT study group 1996).
Myfortic: Oral: Initial: 720 mg twice daily. Maintenance doses may vary based on concomitant immunosuppression.
IV: CellCept: See oral dosing for CellCept; IV and oral doses (of mycophenolate mofetil) are equivalent. If converting from Myfortic to IV CellCept, convert Myfortic to equivalent CellCept oral dose first. Transition to oral therapy as soon as tolerated.
Systemic sclerosis (scleroderma) (off-label use):
CellCept: Oral: Initial: 500 mg twice daily for 1 to 4 weeks; increase to a maintenance dose of 500 to 1,500 mg twice daily as tolerated (Derk 2009; Gerbino 2008; Herrick 2017; Le 2011; Mendoza 2012; Tashkin 2016; Yilmaz 2014)
Myfortic: Oral: Initial: 360 mg twice daily for 1 week, then 720 mg twice daily (Henes 2013; Simeon-Aznar 2011)
Dosing: Geriatric
Dosage is the same as younger patients, however, dosing should be cautious due to possibility of increased hepatic, renal, or cardiac dysfunction. Elderly patients may be at an increased risk of certain infections, gastrointestinal hemorrhage, and pulmonary edema, as compared to younger patients.
Dosing: Pediatric
Note: IV formulation may be used for up to 14 days; transition to oral therapy as soon as tolerated. Mycophenolate mofetil (CellCept) tablets, capsules, and suspension should not be interchanged with the delayed-release tablet formulation (Myfortic) due to differences in the rate of absorption. Consult institution-specific protocols.
Kidney transplantation:
Mycophenolate mofetil (CellCept): Infants ≥3 months, Children, and Adolescents:
Oral:
Suspension: 600 mg/m2/dose twice daily; maximum daily dose: 2,000 mg/day.
Tablets or capsules:
BSA 1.25 m2 to 1.5 m2: 750 mg twice daily.
BSA ≥1.5 m2: 1,000 mg twice daily.
Mycophenolate sodium delayed-release tablets (Myfortic): Children ≥5 years and Adolescents: 400 mg/m2/dose twice daily; maximum daily dose: 1,440 mg/day; avoid partial tablet doses by rounding doses to nearest whole tablet size as follows:
BSA <1.19 m2: Use of this formulation is not recommended.
BSA 1.19 to 1.58 m2: 540 mg twice daily.
BSA >1.58 m2: 720 mg twice daily.
Note: Mycophenolate sodium delayed release 720 mg twice daily was shown to be bioequivalent to mycophenolate mofetil 1,000 mg twice daily.
Lupus nephritis: Limited data available: Mycophenolate mofetil (CellCept): Children and Adolescents: Oral:
BSA-based dosing: Induction and Maintenance: 300 to 600 mg/m2/dose twice daily; maximum daily dose: 3,000 mg/day (Aragon 2010; Baskin 2010; Cooper 2018; Cramer 2007; Marks 2010; Wong 2009).
Nephrotic syndrome: Limited data available: Mycophenolate mofetil (CellCept): Children and Adolescents: Oral:
Frequently relapsing:
BSA-based dosing: 600 mg/m2/dose twice daily for at least 12 months; maximum daily dose: 2,000 mg/day (Beck 2013; Gipson 2009; KDIGO 2012).
Weight-based dosing: 12.5 to 18 mg/kg/dose twice daily; maximum daily dose: 2,000 mg/day for 1 to 2 years with a tapering dose of prednisone (Gipson 2009).
Steroid-dependent (for steroid sparing effect):
BSA-based dosing: 600 mg/m2/dose twice daily for at least 12 months; maximum daily dose: 2,000 mg/day (Gipson 2009; KDIGO 2012).
Weight-based dosing: 12 to 18 mg/kg/dose twice daily; maximum daily dose: 2,000 mg/day (Gipson 2009).
Dosing adjustment for toxicity: Hematologic: ANC <1.3 x 103/μL or anemia; Dosing should be interrupted or the dose reduced.
Dosing: Adjustment for Toxicity
Neutropenia (ANC <1.3 x 103/μL): Dosing should be interrupted or the dose reduced, appropriate diagnostic tests performed and patients managed appropriately
Reconstitution
Oral suspension: Should be constituted prior to dispensing to the patient and not mixed with any other medication. Add 47 mL of water to the bottle and shake well for ~1 minute. Add another 47 mL of water to the bottle and shake well for an additional minute. Final concentration is 200 mg/mL of mycophenolate mofetil.
IV: Reconstitute the contents of each vial with 14 mL of 5% dextrose injection; dilute the contents of a vial with 5% dextrose in water to a final concentration of 6 mg mycophenolate mofetil per mL. Note: Vial is vacuum-sealed; if a lack of vacuum is noted during preparation, the vial should not be used.
Extemporaneously Prepared
A 50 mg/mL oral suspension may be made with mycophenolate mofetil capsules, Ora-Plus, and cherry syrup. In a vertical flow hood, empty six 250 mg capsules into a mortar; add 7.5 mL Ora-Plus and mix to a uniform paste. Mix while adding 15 mL of cherry syrup in incremental proportions; transfer to a calibrated bottle, rinse mortar with cherry syrup, and add sufficient quantity of cherry syrup to make 30 mL. Label "shake well". Stable for 210 days at 5°C, for 28 days at 25°C to 37°C, and for 11 days at 45°C.
Venkataramanan R, McCombs JR, Zuckerman S, et al, "Stability of Mycophenolate Mofetil as an Extemporaneous Suspension," Ann Pharmacother, 1998, 32(7-8):755-7.9681090
Administration
Oral: May be administered with or without food as effects of food on bioavailability are minor (Abd Rahman 2013; Bullingham 1996; Bullingham 1998; Shipkova 2005). Oral suspension may be administered via a nasogastric tube (minimum 8 French, 1.7 mm interior diameter); do not mix oral suspension with other medications. Delayed-release tablets (Myfortic) should be swallowed whole and should not be crushed, cut, or chewed. If a dose is missed, administer as soon as it is remembered. If it is close to the next scheduled dose, skip the missed dose and resume at next regularly scheduled time; do not double a dose to make up for a missed dose.
IV: Intravenous solutions should be administered over at least 2 hours (either peripheral or central vein); do not administer intravenous solution by rapid or bolus injection.
Dietary Considerations
Some products may contain phenylalanine.
Storage
Capsules: Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
Tablets: Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from light.
Oral suspension: Store powder for oral suspension at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Once reconstituted, the oral solution may be stored at 2°C to 8°C (36°F to 46°F) or 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Do not freeze. The mixed suspension is stable for 60 days.
Injection: Store intact vials and solutions diluted in D5W at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Begin infusion within 4 hours of reconstitution.
Mycophenolate Images
Drug Interactions
Acyclovir-Valacyclovir: May increase the serum concentration of Mycophenolate. Mycophenolate may increase the serum concentration of Acyclovir-Valacyclovir. Monitor therapy
Antacids: May decrease the absorption of Mycophenolate. Management: Separate doses of mycophenolate and antacids by at least 2 hours. Monitor for reduced effects of mycophenolate if taken concomitant with antacids. Exceptions: Sodium Bicarbonate. Consider therapy modification
Baricitinib: Immunosuppressants may enhance the immunosuppressive effect of Baricitinib. Management: Use of baricitinib in combination with potent immunosuppressants such as azathioprine or cyclosporine is not recommended. Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted. Consider therapy modification
BCG (Intravesical): Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Bile Acid Sequestrants: May decrease the serum concentration of Mycophenolate. Avoid combination
Cholestyramine Resin: May decrease the serum concentration of Mycophenolate. Avoid combination
Cladribine: May enhance the immunosuppressive effect of Immunosuppressants. Avoid combination
Coccidioides immitis Skin Test: Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. Monitor therapy
CycloSPORINE (Systemic): May decrease the serum concentration of Mycophenolate. Specifically, cyclosporine may decrease concentrations of the active metabolite mycophenolic acid. Management: Mycophenolate requirements may be greater in patients receiving cyclosporine. Monitor mycophenolate dosing and response to therapy particularly closely when adjusting concurrent cyclosporine (starting, stopping, or changing dose). Consider therapy modification
Denosumab: May enhance the adverse/toxic effect of Immunosuppressants. Specifically, the risk for serious infections may be increased. Monitor therapy
Echinacea: May diminish the therapeutic effect of Immunosuppressants. Consider therapy modification
Estrogen Derivatives (Contraceptive): Mycophenolate may decrease the serum concentration of Estrogen Derivatives (Contraceptive). Average AUC values were unchanged, but there was evidence of substantial patient-to-patient variability in response to this combination. Management: Women of childbearing potential who are receiving mycophenolate mofetil should consider using an alternative and/or additional form of contraception. Consider therapy modification
Fingolimod: Immunosuppressants may enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). Consider therapy modification
Ganciclovir-Valganciclovir: Mycophenolate may increase the serum concentration of Ganciclovir-Valganciclovir. Ganciclovir-Valganciclovir may increase the serum concentration of Mycophenolate. Monitor therapy
Isavuconazonium Sulfate: May increase the serum concentration of Mycophenolate. Monitor therapy
Leflunomide: Immunosuppressants may enhance the adverse/toxic effect of Leflunomide. Specifically, the risk for hematologic toxicity such as pancytopenia, agranulocytosis, and/or thrombocytopenia may be increased. Management: Consider not using a leflunomide loading dose in patients receiving other immunosuppressants. Patients receiving both leflunomide and another immunosuppressant should be monitored for bone marrow suppression at least monthly. Consider therapy modification
Magnesium Salts: May decrease the serum concentration of Mycophenolate. Management: Separate doses of mycophenolate and oral magnesium salts. Monitor for reduced effects of mycophenolate if taken concomitant with oral magnesium salts. Consider therapy modification
MetroNIDAZOLE (Systemic): May decrease the serum concentration of Mycophenolate. Specifically, metronidazole may decrease concentrations of the active metabolite of mycophenolate. Monitor therapy
Natalizumab: Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. Avoid combination
Nitisinone: May increase the serum concentration of OAT1/3 Substrates. Monitor therapy
Nivolumab: Immunosuppressants may diminish the therapeutic effect of Nivolumab. Consider therapy modification
Ocrelizumab: May enhance the immunosuppressive effect of Immunosuppressants. Monitor therapy
Penicillins: May decrease serum concentrations of the active metabolite(s) of Mycophenolate. This effect appears to be the result of impaired enterohepatic recirculation. Monitor therapy
Pidotimod: Immunosuppressants may diminish the therapeutic effect of Pidotimod. Monitor therapy
Pimecrolimus: May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Pretomanid: May increase the serum concentration of OAT1/3 Substrates. Monitor therapy
Probenecid: May increase the serum concentration of Mycophenolate. Monitor therapy
Progestins (Contraceptive): Mycophenolate may decrease the serum concentration of Progestins (Contraceptive). Management: Use of an additional or alternative (nonhormonal) method of contraception should be considered. Consider therapy modification
Proton Pump Inhibitors: May decrease the serum concentration of Mycophenolate. Specifically, concentrations of the active mycophenolic acid may be reduced. Monitor therapy
Quinolones: May decrease the serum concentration of Mycophenolate. Specifically, quinolones may decrease concentrations of the active metabolite of mycophenolate. Monitor therapy
Rifamycin Derivatives: May decrease the serum concentration of Mycophenolate. Specifically, rifamycin derivatives may decrease the concentration of the active metabolite mycophenolic acid. Avoid combination
Roflumilast: May enhance the immunosuppressive effect of Immunosuppressants. Consider therapy modification
Sevelamer: May decrease the serum concentration of Mycophenolate. Management: Administer mycophenolate at least 2 hours prior to sevelamer administration. Consider therapy modification
Siponimod: Immunosuppressants may enhance the immunosuppressive effect of Siponimod. Monitor therapy
Sipuleucel-T: Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. Consider therapy modification
Smallpox and Monkeypox Vaccine (Live): Immunosuppressants may diminish the therapeutic effect of Smallpox and Monkeypox Vaccine (Live). Monitor therapy
Tacrolimus (Topical): May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Teriflunomide: May increase the serum concentration of OAT1/3 Substrates. Monitor therapy
Tertomotide: Immunosuppressants may diminish the therapeutic effect of Tertomotide. Monitor therapy
Tofacitinib: Immunosuppressants may enhance the immunosuppressive effect of Tofacitinib. Management: Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted, and this warning seems particularly focused on more potent immunosuppressants. Consider therapy modification
Tolvaptan: May increase the serum concentration of OAT1/3 Substrates. Management: Patients being treated with the Jynarque brand of tolvaptan should avoid concomitant use of OAT1/3 substrates. Concentrations and effects of the OAT1/3 substrate would be expected to increase with any combined use. Consider therapy modification
Trastuzumab: May enhance the neutropenic effect of Immunosuppressants. Monitor therapy
Upadacitinib: Immunosuppressants may enhance the immunosuppressive effect of Upadacitinib. Avoid combination
Vaccines (Inactivated): Immunosuppressants may diminish the therapeutic effect of Vaccines (Inactivated). Management: Vaccine efficacy may be reduced. Complete all age-appropriate vaccinations at least 2 weeks prior to starting an immunosuppressant. If vaccinated during immunosuppressant therapy, revaccinate at least 3 months after immunosuppressant discontinuation. Consider therapy modification
Vaccines (Live): Immunosuppressants may enhance the adverse/toxic effect of Vaccines (Live). Immunosuppressants may diminish the therapeutic effect of Vaccines (Live). Management: Avoid use of live organism vaccines with immunosuppressants; live-attenuated vaccines should not be given for at least 3 months after immunosuppressants. Exceptions: Smallpox and Monkeypox Vaccine (Live). Avoid combination
Adverse Reactions
Incidences include concomitant use with cyclosporine and corticosteroids. In general, lower doses used in renal rejection patients had less adverse effects than higher doses. Rates of adverse effects were similar for each indication, except for those unique to the specific organ involved.
>10%:
Cardiovascular: Hypertension (18% to 79%), edema (17% to 68%), hypotension (34%), tachycardia (22% to 23%), lower extremity edema (16%)
Central nervous system: Pain (25% to 79%), headache (11% to 59%), insomnia (24% to 52%), dizziness (34%), depression (20%), chills (3% to <20%), confusion (3% to <20%), drowsiness (3% to <20%), hypertonia (3% to <20%), malaise (3% to <20%), myasthenia (3% to <20%), paresthesia (3% to <20%)
Dermatologic: Skin rash (26%), ecchymoses (20%), cellulitis (3% to <20%)
Endocrine & metabolic: Hyperglycemia (44% to 48%), hypercholesterolemia (46%), hypomagnesemia (20% to 39%), hypokalemia (9% to 37%), hypocalcemia (11% to 30%), increased lactate dehydrogenase (24%), hyperkalemia (22%), acidosis (3% to <20%), weight loss (3% to <20%), hyperuricemia (13%), hyperlipidemia (10% to 12%), hypophosphatemia (9% to 11%)
Gastrointestinal: Abdominal pain (22% to 63%), nausea (27% to 56%), diarrhea (24% to 53%), constipation (38% to 44%), vomiting (20% to 39%), decreased appetite (25%), dyspepsia (19% to 23%), esophagitis (3% to <20%), gastric ulcer (3% to <20%), gastritis (3% to <20%), gastrointestinal hemorrhage (3% to <20%), hernia of abdominal cavity (3% to <20%), intestinal obstruction (3% to <20%), stomatitis (3% to <20%), upper abdominal pain (14%), flatulence (10% to 13%)
Genitourinary: Urinary tract infection (29% to 33%), hematuria (3% to <20%)
Hematologic & oncologic: Leukopenia (19% to 46%), anemia (20% to 45%), leukocytosis (22% to 43%), thrombocytopenia (24% to 38%), benign skin neoplasm (3% to <20%), disorder of hemostatic components of blood (3% to <20%), neoplasm (3% to <20%), pancytopenia (3% to <20%), skin carcinoma (3% to <20%; non-melanoma: 1% to 12%)
Hepatic: Increased liver enzymes (25%), hepatitis (3% to <20%), increased serum alkaline phosphatase (3% to <20%)
Infection: Bacterial infection (27% to 40%), viral infection (31%), cytomegalovirus disease (4% to 22%), fungal infection (11% to 12%)
Neuromuscular & skeletal: Asthenia (35% to 49%), tremor (12% to 34%), back pain (6% to 12%), arthralgia (7% to 11%)
Renal: Increased serum creatinine (10% to 42%), increased blood urea nitrogen (37%)
Respiratory: Dyspnea (31% to 44%), cough (41%), pleural effusion (34%)
Miscellaneous: Fever (13% to 56%)
1% to 10%:
Cardiovascular: Exacerbation of hypertension (<10%), peripheral edema (<10%), phlebitis (4%), thrombosis (4%)
Central nervous system: Anxiety (<10%), fatigue (<10%)
Dermatologic: Acne vulgaris (<10%), pruritus (<10%)
Endocrine & metabolic: Diabetes mellitus (<10%)
Gastrointestinal: Abdominal distension (<10%), gastroesophageal reflux disease (<10%), gingival hyperplasia (<10%), oral candidiasis (<10%)
Genitourinary: Urinary retention (<10%)
Hematologic & oncologic: Lymphocele (<10%), severe neutropenia (2% to 4%), malignant neoplasm (≤2%), malignant lymphoma (1%), lymphoproliferative disorder (≤1%)
Hepatic: Abnormal hepatic function tests (<10%)
Infection: Influenza (<10%), wound infection (<10%), herpes simplex infection (6% to 8%), herpes zoster infection (4% to 5%), sepsis (2% to 5%)
Neuromuscular & skeletal: Muscle cramps (<10%), myalgia (<10%), peripheral pain (<10%)
Ophthalmic: Blurred vision (<10%)
Renal: Renal insufficiency (<10%), renal tubular necrosis (<10%)
Respiratory: Dyspnea on exertion (<10%), nasopharyngitis (<10%), pneumonia (<10%), sinusitis (<10%), upper respiratory tract infection (<10%)
Frequency not defined:
Gastrointestinal: Mucocutaneous candidiasis
Infection: Protozoal infection
Respiratory: Pharyngitis, respiratory tract infection
<1%, postmarketing and/or case reports: Agranulocytosis, alopecia, anorexia, atypical mycobacterial infection, BK virus, bone marrow failure, bronchiectasis (Boddana 2011; Rook 2006), colitis, duodenal ulcer, endocarditis, esophageal ulcer, gastrointestinal perforation, hematemesis, hemorrhagic colitis, hemorrhagic gastritis, hypersensitivity reaction, hypogammaglobulinemia (Boddana 2011; Keven 2003; Robertson 2009), interstitial pulmonary disease, Kaposi sarcoma, lymphadenopathy, lymphopenia, melena, meningitis, osteomyelitis, pancreatitis, peritonitis, polyomavirus infection, progressive multifocal leukoencephalopathy, pulmonary edema, pulmonary fibrosis, pure red cell aplasia, reactivation of disease (HCV), reactivation of HBV, tuberculosis, venous thrombosis, wheezing, xerostomia
Warnings/Precautions
Concerns related to adverse effects:
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery, driving).
- Infections: [US Boxed Warning]: Risk for bacterial, viral, fungal, and protozoal infections, including opportunistic infections and viral reactivation of hepatitis B and C, is increased with immunosuppressant therapy; infections may be serious and potentially fatal. Due to the risk of oversuppression of the immune system, which may increase susceptibility to infection, combination immunosuppressant therapy should be used with caution.
- New or reactivated viral infections: Polyomavirus associated nephropathy (PVAN), JC virus-associated progressive multifocal leukoencephalopathy (PML), cytomegalovirus (CMV) infections, and reactivation of hepatitis B (HBV) or hepatitis C (HCV) have been reported with use. A reduction in immunosuppression should be considered for patients with new or reactivated viral infections; however, in transplant recipients, the risk that reduced immunosuppression presents to the functioning graft should also be considered. PVAN, primarily from activation of BK virus, may lead to the deterioration of renal function and/or renal graft loss. PML, a potentially fatal condition, commonly presents with apathy, ataxia, cognitive deficiencies, confusion, and hemiparesis. Risk factors for development of PML include treatment with immunosuppressants and immune function impairment; consultation with a neurologist should be considered in any patient with neurological symptoms receiving immunosuppressants. Risk of CMV viremia or disease is increased in transplant recipients CMV seronegative at the time of transplant who receive a graft from a CMV seropositive donor; however, routine approaches to limiting CMV exist and should be utilized. In patients infected with HBV or HCV, viral reactivation may occur; these patients should be monitored for signs of active HBV or HCV.
- Lymphoproliferative disorders: [US Boxed Warning]: Risk of development of lymphoma and skin malignancy is increased. The risk for malignancies is related to intensity/duration of therapy. Patients should be monitored appropriately, instructed to limit exposure to sunlight/UV light to decrease the risk of skin cancer, and given supportive treatment should these conditions occur. Post-transplant lymphoproliferative disorder related to EBV infection has been reported in immunosuppressed organ transplant patients; risk is highest in EBV seronegative patients (including many young children).
- Neutropenia: Neutropenia (including severe neutropenia) may occur, requiring dose reduction or interruption of treatment (risk greater from day 31 to 180 post-transplant).
- Pure red cell aplasia (PRCA): PRCA, a type of anemia which can range from subclinical to severe, has been reported in patients receiving mycophenolate concomitantly with other immunosuppressive agents (eg, tacrolimus, cyclosporine, corticosteroids). Symptoms may include fatigue, lethargy, or pallor. Although not precisely known, risk factors for the development of PRCA may include immunosuppression and treatment with immunosuppressant therapy. Dose reduction or discontinuation of immunosuppressive therapy may reverse PRCA; however, in transplant recipients, the risk of reduced immunosuppression and graft rejection should be considered.
Disease-related concerns:
- Gastrointestinal disorders: Use may rarely be associated with gastric or duodenal ulcers, GI bleeding, and/or perforation. Use caution in patients with active serious digestive system disease; patients with active peptic ulcers were not included in clinical studies. The purpose of the enteric-coated formulation (Myfortic) was to decrease GI side effects; however, studies have demonstrated similar rates of GI side effects between mycophenolate mofetil and the enteric-coated formulation (Budde 2004a; Budde 2010; Salvadori 2004).
- Hypoxanthine-guanine phosphoribosyltransferase deficiency: Theoretically, use should be avoided in patients with the rare hereditary deficiency of hypoxanthine-guanine phosphoribosyltransferase (such as Lesch-Nyhan or Kelley-Seegmiller syndrome).
- Renal impairment: Use with caution in patients with renal impairment as toxicity may be increased; may require dosage adjustment in severe impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Non-interchangeability of dosage forms: Mycophenolate sodium and mycophenolate mofetil should not be used interchangeably without health care provider supervision because the rate of absorption following the administration of these two products is not equivalent. Single dose pharmacokinetic studies in adult renal transplant patients suggest that bioavailability is similar between oral mycophenolate mofetil (1 g) and delayed-release mycophenolic acid (720 mg) (Arns 2005). In clinical trials, comparative efficacy and safety profiles have been observed in adult renal transplant patients randomized to either oral mycophenolate mofetil (1 g twice daily) or delayed-release mycophenolic acid (720 mg twice daily) (Budde 2004b; Salvadori 2003).
- Phenylalanine: Some dosage forms may contain phenylalanine.
- Polysorbate 80: Some dosage forms may contain polysorbate 80 (also known as Tweens). Hypersensitivity reactions, usually a delayed reaction, have been reported following exposure to pharmaceutical products containing polysorbate 80 in certain individuals (Isaksson, 2002; Lucente 2000; Shelley, 1995). Thrombocytopenia, ascites, pulmonary deterioration, and renal and hepatic failure have been reported in premature neonates after receiving parenteral products containing polysorbate 80 (Alade 1986; CDC 1984). See manufacturer's labeling.
Special populations:
- Pregnancy: [US Boxed Warning]: Mycophenolate is associated with an increased risk of congenital malformations and first trimester pregnancy loss when used by pregnant women. Avoid use if safer treatment options are available. Women of reproductive potential must be counseled about pregnancy prevention and planning. Alternative agents should be considered for women planning a pregnancy. Women of reproductive potential should have a negative pregnancy test with a sensitivity of ≥25 milliunits/mL immediately before therapy and the test should be repeated 8 to 10 days later. Pregnancy tests should be repeated during routine follow-up visits. Acceptable forms of contraception should be used during treatment and for 6 weeks after therapy is discontinued. Sexually active male patients and/or their female partners should use effective contraception during treatment of the male patient and for at least 3 months after last dose.
Other warnings/precautions:
- Blood donations: Patients should not donate blood or blood products during treatment and for at least 6 weeks after the last dose.
- Discontinuation of therapy: Myasthenia gravis: Abrupt cessation of this or any immunosuppressant, especially in clinically unstable individuals, may result in rapid deterioration of myasthenic symptoms and possibly myasthenic crisis (Melzer 2016).
- Experienced physician: [US Boxed Warning]: Should be administered under the supervision of a physician experienced in immunosuppressive therapy.
- Immunizations: Live attenuated vaccines should be avoided during use; vaccinations may be less effective during therapy.
- IV administration: Intravenous solutions should be given over at least 2 hours; never administer intravenous solution by rapid or bolus injection.
- Semen donations: Male patients should not donate semen during treatment and for 3 months after the last dose.
Monitoring Parameters
Complete blood count (weekly for first month, twice monthly during months 2 and 3, then monthly thereafter through the first year); renal and liver function; signs and symptoms of organ rejection; signs and symptoms of bacterial, fungal, protozoal, new or reactivated viral, or opportunistic infections; neurological symptoms (eg, hemiparesis, confusion, cognitive deficiencies, ataxia) suggestive of PML, pregnancy test (sensitivity of ≥25 milliunits/mL; immediately prior to initiation and 8 to 10 days later in females of childbearing potential, followed by repeat tests during therapy); monitor skin (for lesions suspicious of skin cancer); monitor for signs of lymphoma; monitor for signs of pure red cell aplasia or autoimmune hemolytic anemia (Elimelakh 2007; Hodo 2006; Schecter 2007).
Pregnancy
Pregnancy Risk Factor
D
Pregnancy Considerations
[US Boxed Warning]: Use during pregnancy is associated with increased risks of first trimester pregnancy loss and congenital malformations. Avoid if safer treatment options are available. Females of reproductive potential must be counseled regarding pregnancy prevention and planning.
The following congenital malformations have been reported following exposure during pregnancy: External ear abnormalities, cleft lip and palate, anomalies of the distal limbs, heart, esophagus, kidney, and nervous system. The combination of ear, eye, and lip/palate abnormalities has been identified as mycophenolate embryopathy (Perez-Aytes 2017). First trimester pregnancy loss has also been reported.
Females of reproductive potential (girls who have entered puberty and women with a uterus who have not passed through clinically confirmed menopause) should have a negative pregnancy test with a sensitivity of ≥25 milliunits/mL immediately before mycophenolate therapy and the test should be repeated 8 to 10 days later. Pregnancy tests should then be repeated during routine follow-up visits. Acceptable forms of contraception should be used during treatment and for 6 weeks after therapy is discontinued. The effectiveness of hormonal contraceptive agents may be affected by mycophenolate. Sexually active male patients and/or their female partners should use effective contraception during treatment of the male patient and for at least 3 months after last dose.
Current guidelines recommend that pregnancy be delayed following a kidney transplant until 1 year has passed without an acute rejection; this time period may be adjusted as clinically appropriate. Women planning a pregnancy and who are already taking mycophenolate following a kidney transplant should be switched to a different medication and mycophenolate should be discontinued for at least 6 weeks before pregnancy is attempted (KDIGO 2009). Mycophenolate is not recommended for the treatment of psoriasis in pregnant women (Menter 2009). Mycophenolate should not be used during pregnancy in women with lupus nephritis; women who become pregnant during mycophenolate therapy should be switched to a different medication (KDIGO 2012). For women with lupus nephritis taking mycophenolate and who are planning a pregnancy, mycophenolate should be discontinued at least 6 weeks prior to trying to conceive (Hahn 2012).
Health care providers should report female exposures to mycophenolate during pregnancy or within 6 weeks of discontinuing therapy to the Mycophenolate Pregnancy Registry (800-617-8191).
The Transplant Pregnancy Registry International (TPR) is a registry that follows pregnancies that occur in maternal transplant recipients or those fathered by male transplant recipients. The TPR encourages reporting of pregnancies following solid organ transplant by contacting them at 1-877-955-6877 or https://www.transplantpregnancyregistry.org.
Patient Education
What is this drug used for?
- It is used to keep the body from harming the organ after an organ transplant.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Injection site irritation
- Nausea
- Vomiting
- Back pain
- Constipation
- Diarrhea
- Lack of appetite
- Joint pain
- Passing gas
- Tremors
- Trouble sleeping
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Skin infection
- High blood sugar like confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit.
- Electrolyte problems like mood changes, confusion, muscle pain or weakness, abnormal heartbeat, seizures, lack of appetite, or severe nausea or vomiting.
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding.
- Progressive multifocal leukoencephalopathy like confusion, depression, trouble with memory, behavioral changes, change in strength on one side is greater than the other, difficulty speaking, change in balance, or vision changes.
- Severe pulmonary disorder like lung or breathing problems like difficulty breathing, shortness of breath, or a cough that is new or worse.
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain.
- Chest pain
- Fast heartbeat
- Slow heartbeat
- Abnormal heartbeat
- Severe headache
- Edema
- Excessive weight loss
- Severe loss of strength and energy
- Burning or numbness feeling
- Muscle cramps
- Mole changes
- Skin growths
- Severe dizziness
- Passing out
- Vision changes
- Night sweats
- Severe abdominal pain
- Swollen glands
- Pale skin
- Thrush
- Vaginal pain, itching, and discharge
- Yellow skin
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.