Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution, Intravenous [preservative free]:
Ocrevus: 300 mg/10 mL (10 mL)
Pharmacology
Mechanism of Action
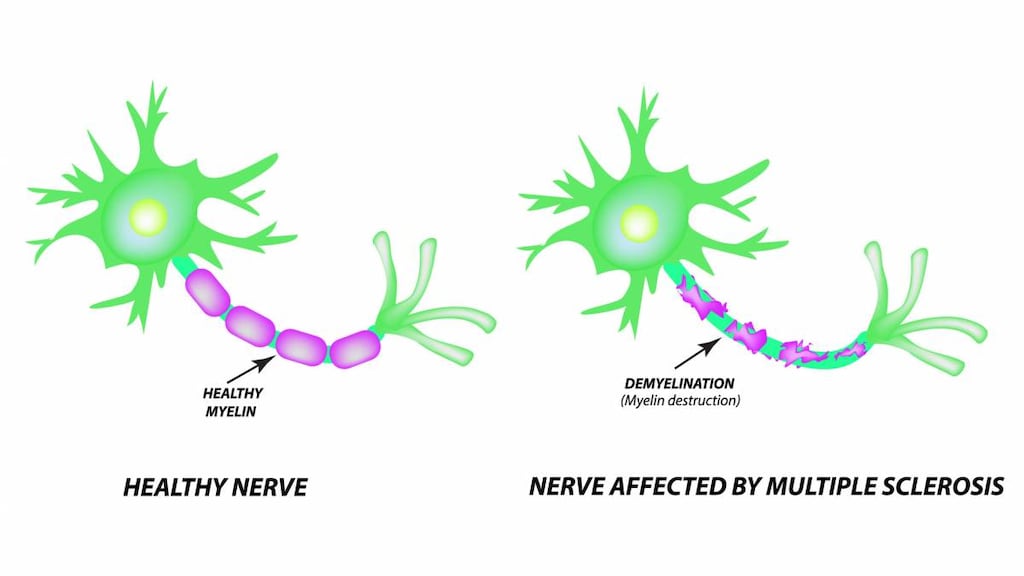
Ocrelizumab is a recombinant humanized IgG monoclonal antibody directed against B-cells which express the cell surface antigen CD20; CD20 is present on pre-B and mature B lymphocytes. B-cells are thought to influence the course of multiple sclerosis through antigen presentation, autoantibody production, cytokine regulation, and formation of ectopic lymphoid aggregates in the meninges (Hauser 2017). Ocrelizumab selectively targets and binds with high affinity to the cell surface to deplete CD20 expressing B-cells through antibody-dependent cell-mediated phagocytosis and cytotoxicity, as well as complement-mediated cytolysis (Hauser 2017; Montalban 2017).
Pharmacokinetics/Pharmacodynamics
Distribution
Central Vd: 2.78 L; Peripheral: 2.68 L
Metabolism
Antibodies are primarily cleared by catabolism
Excretion
Constant clearance (estimated): 0.17 L/day; Initial time-dependent clearance: 0.05 L/day.
Onset of Action
Serum CD-19+ B-cell counts (used as a marker for B-cell counts) are reduced within 14 days after infusion.
Duration of Action
Median time for B-cell recovery (to baseline or the lower limit of normal): 72 weeks (range: 27 to 175 weeks).
Half-Life Elimination
26 days
Use: Labeled Indications
Multiple sclerosis, relapsing or primary progressive: Treatment of primary progressive multiple sclerosis (MS) and relapsing forms of MS, including clinically isolated syndrome, relapsing remitting disease, and active secondary progressive disease.
Contraindications
History of life-threatening infusion reaction to ocrelizumab; active hepatitis B virus (HBV) infection.
Canadian labeling: Additional contraindications (not in US labeling): Known hypersensitivity to ocrelizumab or any component of the formulation; severe, active infections; current or history of confirmed progressive multifocal leukoencephalopathy (PML); active malignancies; severely immunocompromised states
Dosage and Administration
Dosing: Adult
Note: Premedicate with methylprednisolone (100 mg IV) 30 minutes prior to each infusion, and an antihistamine (eg, diphenhydramine) 30 to 60 minutes prior each infusion; may also consider premedication with acetaminophen. Assess for infection; delay administration for active infection.
Multiple sclerosis, relapsing or primary progressive: IV: 300 mg on day 1, followed by 300 mg 2 weeks later; subsequent doses of 600 mg are administered once every 6 months (beginning 6 months after the first 300 mg dose) (Hauser 2017; Montalban 2017).
Missed doses: If a dose is missed, administer as soon as possible (do not wait until the next scheduled dose), then adjust the dose schedule to administer the next sequential dose 6 months after the missed dose was administered. Doses must be separated by at least 5 months.
Dosing: Adjustment for Toxicity
Dosage adjustment for infusion reactions:
Mild to moderate reactions: Reduce the infusion rate to one-half of the rate at which the reaction occurred; maintain reduced rate for at least 30 minutes. If the reduced rate is tolerated, increase the rate every 30 minutes by 30 mL/hour to a maximum rate of 180 mL/hour (for the 300 mg dose) or 40 mL/hour to a maximum rate of 200 mL/hours (for the 600 mg dose).
Severe reactions: Interrupt infusion immediately and administer supportive management as needed. After all symptoms have resolved, restart infusion beginning at a rate one-half of the rate at onset of reaction. If the reduced rate is tolerated, increase the rate every 30 minutes by 30 mL/hour to a maximum rate of 180 mL/hour (for the 300 mg dose) or 40 mL/hour to a maximum rate of 200 mL/hours (for the 600 mg dose).
Life-threatening reactions: Immediately stop and permanently discontinue infusion for life-threatening or disabling infusion reaction.
Reconstitution
Dilute for infusion in NS (dilute 300 mg dose in a 250 mL bag and 600 mg dose in a 500 mL bag) to a final concentration of approximately 1.2 mg/mL. Do not dilute in any other solutions. Do not shake. Incompatibilities between polyvinyl chloride (PVC) or polyolefin bags and ocrelizumab have not been observed.
Administration
IV: Administer though a dedicated IV line using a 0.2 or 0.22 micron in-line filter. Premedicate with methylprednisolone (100 mg IV) 30 minutes prior to each infusion, and an antihistamine (eg, diphenhydramine) 30 to 60 minutes prior each infusion; may also consider premedication with acetaminophen.
First 2 infusions (300 mg dose): Begin infusion at 30 mL/hour; increase by 30 mL/hour every 30 minutes to a maximum rate of 180 mL/hour. Infusion duration is 2.5 hours or longer.
Subsequent infusions (600 mg dose): Begin infusion at 40 mL/hour; increase by 40 mL/hour every 30 minutes to a maximum rate of 200 mL/hour. Infusion duration is 3.5 hours or longer.
Monitor for infusion reactions during infusion and observe for at least one hour after infusion is complete. If infusion reaction occurs, interrupt infusion, discontinue or decrease the rate, depending on the severity of the reaction.
Storage
Store intact vials at 2°C to 8°C (36°F to 46°F) in the outer carton to protect from light. Do not freeze. Do not shake. Solutions diluted for infusion should be used immediately, however may be stored for up to 24 hours refrigerated and 8 hours at room temperature (including infusion time); discard if infusion cannot be completed on the same day.
Drug Interactions
Baricitinib: Immunosuppressants may enhance the immunosuppressive effect of Baricitinib. Management: Use of baricitinib in combination with potent immunosuppressants such as azathioprine or cyclosporine is not recommended. Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted. Consider therapy modification
BCG (Intravesical): Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Cladribine: May enhance the immunosuppressive effect of Immunosuppressants. Avoid combination
Coccidioides immitis Skin Test: Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. Monitor therapy
Denosumab: May enhance the adverse/toxic effect of Immunosuppressants. Specifically, the risk for serious infections may be increased. Monitor therapy
Echinacea: May diminish the therapeutic effect of Immunosuppressants. Consider therapy modification
Fingolimod: Immunosuppressants may enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). Consider therapy modification
Immunosuppressants: Ocrelizumab may enhance the immunosuppressive effect of Immunosuppressants. Monitor therapy
Leflunomide: Immunosuppressants may enhance the adverse/toxic effect of Leflunomide. Specifically, the risk for hematologic toxicity such as pancytopenia, agranulocytosis, and/or thrombocytopenia may be increased. Management: Consider not using a leflunomide loading dose in patients receiving other immunosuppressants. Patients receiving both leflunomide and another immunosuppressant should be monitored for bone marrow suppression at least monthly. Consider therapy modification
Natalizumab: Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. Avoid combination
Nivolumab: Immunosuppressants may diminish the therapeutic effect of Nivolumab. Consider therapy modification
Pidotimod: Immunosuppressants may diminish the therapeutic effect of Pidotimod. Monitor therapy
Pimecrolimus: May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Roflumilast: May enhance the immunosuppressive effect of Immunosuppressants. Consider therapy modification
Siponimod: Immunosuppressants may enhance the immunosuppressive effect of Siponimod. Monitor therapy
Sipuleucel-T: Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. Consider therapy modification
Tacrolimus (Topical): May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Tertomotide: Immunosuppressants may diminish the therapeutic effect of Tertomotide. Monitor therapy
Tofacitinib: Immunosuppressants may enhance the immunosuppressive effect of Tofacitinib. Management: Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted, and this warning seems particularly focused on more potent immunosuppressants. Consider therapy modification
Trastuzumab: May enhance the neutropenic effect of Immunosuppressants. Monitor therapy
Upadacitinib: Immunosuppressants may enhance the immunosuppressive effect of Upadacitinib. Avoid combination
Vaccines (Inactivated): Immunosuppressants may diminish the therapeutic effect of Vaccines (Inactivated). Management: Vaccine efficacy may be reduced. Complete all age-appropriate vaccinations at least 2 weeks prior to starting an immunosuppressant. If vaccinated during immunosuppressant therapy, revaccinate at least 3 months after immunosuppressant discontinuation. Consider therapy modification
Vaccines (Live): Ocrelizumab may enhance the adverse/toxic effect of Vaccines (Live). Ocrelizumab may diminish the therapeutic effect of Vaccines (Live). Avoid combination
Test Interactions
Ocrelizumab interferes with the CD20 assay for B-cell counts; use the CD19+ assay to measure B-cell counts.
Adverse Reactions
>10%:
Dermatologic: Skin infection (14%)
Hematologic & oncologic: Decreased serum immunoglobulins (≤17%, IgM most affected), decreased neutrophils (13%)
Infection: Infection (58% to 70%)
Respiratory: Upper respiratory tract infection (40% to 49%)
Miscellaneous: Infusion related reaction (34% to 40%)
1% to 10%:
Cardiovascular: Peripheral edema (6%)
Central nervous system: Depression (8%)
Gastrointestinal: Diarrhea (6%)
Infection: Herpes virus infection (5% to 6%)
Neuromuscular & skeletal: Back pain (6%), limb pain (5%)
Respiratory: Lower respiratory tract infection (8% to 10%), cough (7%)
Frequency not defined:
Cardiovascular: Hypotension (infusion related)
Hypersensitivity: Anaphylaxis
Respiratory: Bronchospasm, laryngeal edema, pharyngeal edema
<1%, postmarketing, and/or case reports: Antibody development, malignant neoplasm of breast, severe infusion related reaction
Warnings/Precautions
Concerns related to adverse effects:
- Hepatitis B reactivation: Screen for hepatitis B virus in all patients (HBsAg and anti-HBc measurements) prior to treatment initiation. Although there were no reports of hepatitis B reactivation in MS patients treated with ocrelizumab, fulminant hepatitis, hepatic failure, and death caused by HBV reactivation have occurred in patients treated with other anti-CD20 monoclonal antibodies. Perform HBV screening in all patients prior to treatment initiation. Do not administer ocrelizumab to patients with active HBV confirmed by positive results for HBsAg and anti-HB tests. Consult liver disease specialist prior to starting and during treatment in patients who are negative for surface antigen (HBsAg) and positive for HB core antibody (HBcAb+) or are carriers of HBV (HBsAg+).
- Herpes infection: In clinical studies, herpes infections (herpes zoster, herpes simplex, oral herpes, genital herpes, and herpes virus infection) were reported more frequently in patients who received ocrelizumab compared to patients who received comparator drug and oral herpes was reported more frequently with ocrelizumab than with placebo. Infections were predominantly mild to moderate in severity. There were no reports of disseminated herpes.
- Infection: Assess for infections prior to treatment initiation and delay treatment in patients with an active infection until the infection is resolved. In clinical studies, a slightly higher incidence of infections was reported in patients receiving ocrelizumab, compared to patients receiving the comparator drug or placebo. Over half of patients who received ocrelizumab experienced one or more infections. In multiple sclerosis patients, ocrelizumab is associated with an increased risk for respiratory tract infections (upper and lower), skin infections, and herpes-related infections, although was not associated with an increased risk of serious infections. Respiratory tract infections were predominantly mild to moderate and consisted mostly of upper respiratory tract infections and bronchitis.
- Infusion reactions: Ocrelizumab may cause infusion reactions; symptoms include pruritus, rash, urticaria, erythema, bronchospasm, throat irritation, oropharyngeal pain, dyspnea, pharyngeal or laryngeal edema, flushing, hypotension, pyrexia, fatigue, headache, dizziness, nausea, tachycardia, and anaphylaxis. The incidence of infusion reactions in patients who received methylprednisolone (or an equivalent steroid) and potentially other pre-medication to reduce the risk of infusion reactions prior to each infusion was 34% to 40% in multiple sclerosis studies; the highest incidence was with the first infusion. There were no fatal infusion reactions, although serious infusion reactions occurred (rarely), some reactions required hospitalization. Monitor for infusion reactions during the infusion and for at least one hour after the end of the infusion. Infusion reactions can occur up to 24 hours after the infusion. Administer premedications (methylprednisolone [or equivalent] and an antihistamine, with or without acetaminophen) to reduce the frequency and severity of infusion reactions. Depending on the severity of the reaction, infusion reaction may require infusion interruption, decreased infusion rate, or discontinuation; may also require symptomatic supportive management.
- Malignancy: Ocrelizumab may be associated with an increased risk of malignancy. Malignancies (including breast cancer) occurred more frequently in ocrelizumab-treated patients in clinical studies. Breast cancer occurred in 0.8% of females who received ocrelizumab and none of the females who received the comparator drug or placebo. Patients should follow standard breast cancer screening guidelines.
- Progressive multifocal leukoencephalopathy: Although no cases of progressive multifocal leukoencephalopathy (PML) were identified in ocrelizumab studies, John Cunningham (JC) virus infection resulting in PML has been observed in patients treated with other anti-CD20 antibodies and other MS therapies and has been associated with some risk factors such as patients who are immunocompromised or use polytherapy with immunosuppressants. PML is an opportunistic viral infection of the brain caused by the JC virus and usually leads to death or severe disability; PML typically only occurs in patients who are immunocompromised. Symptoms associated with PML are diverse and progress over days to weeks, and include progressive weakness on one side of the body or clumsiness of limbs, vision disturbance, and changes in thinking, memory, and/or orientation leading to confusion and personality changes. Withhold treatment and perform appropriate diagnostic evaluation at the first sign or symptom suggestive of PML (MRI findings may be apparent prior to clinical signs/symptoms).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
- Immunizations: Administer live-attenuated or live immunizations at least 4 weeks and non-live immunizations at least 2 weeks prior to treatment initiation. Immunization with live-attenuated or live vaccines is not recommended during treatment or after discontinuation until B-cell repletion. Prior to administration of live-attenuated or live vaccinations in infants exposed to ocrelizumab in utero, confirm recovery of B-cell counts. Non-live vaccines may be administered; however, consideration should be given to evaluating the immune response.
Other warnings/precautions:
- Appropriate use: Ocrelizumab has not been studied in combination with other MS therapies. When initiating ocrelizumab after an immunosuppressive therapy or initiating an immunosuppressive following ocrelizumab therapy, consider the potential for increased immunosuppressive effects.
Monitoring Parameters
Hepatitis B virus screening in all patients (HBsAg and anti-HBc measurements) prior to therapy initiation.
Screening recommendations for other anti-CD20 monoclonal antibodies (American Society of Clinical Oncology provisional clinical opinion update [Hwang 2015]): Hepatitis B virus (HBV): Screen for HBV infection with hepatitis B surface antigen (HBsAg) and hepatitis B core antibody (anti-HBc) tests prior to treatment initiation; either a total anti-HBc (with both immunoglobulin G [IgG] and immunoglobulin M [IgM]) or anti-HBc IgG test should be used to screen for chronic or unresolved HBV infection (do not use anti-HBc IgM as it may only confirm acute HBV infection). HBsAg-negative/anti-HBc-positive patients should be monitored for HBV reactivation with HBV DNA and ALT testing approximately every 3 months during treatment.
Monitor for infusion reactions during infusion and for at least 1 hour following the end of the infusion; monitor for signs/symptoms of infection, malignancy, and progressive multifocal leukoencephalopathy.
Pregnancy
Pregnancy Considerations
Ocrelizumab is a humanized monoclonal antibody (IgG1). Potential placental transfer of human IgG is dependent upon the IgG subclass and gestational age, generally increasing as pregnancy progresses. The lowest exposure would be expected during the period of organogenesis (Palmeira 2012; Pentsuk 2009).
Information related to the use of ocrelizumab in pregnancy is limited (Fragoso 2018; Juanatey 2018). Transient peripheral B-cell depletion and lymphocytopenia have been observed in infants born to mothers who received similar agents; immune response to live or live-attenuated vaccines may be decreased in infants exposed to ocrelizumab in utero. Evaluate immune response by measuring CD19+B-cells in exposed infants prior to the administration of live or live-attenuated vaccines.
In general, disease-modifying therapies for multiple sclerosis (MS) are stopped prior to a planned pregnancy, and not initiated during pregnancy, except in females at high risk of MS activity (AAN [Rae-Grant 2018]). Consider use of agents other than ocrelizumab for females at high risk of disease reactivation who are planning a pregnancy. Delaying pregnancy is recommended for females with persistent high disease activity; when disease-modifying therapy is needed in these patients, other agents are preferred (ECTRIMS/EAN [Montalban 2018]).
Females of reproductive potential should use effective contraception during therapy and for 6 months after the last ocrelizumab infusion.
Patient Education
What is this drug used for?
- It is used to treat MS (multiple sclerosis).
Frequently reported side effects of this drug
- Common cold symptoms
- Back pain
- Diarrhea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Infusion reaction
- Skin infection
- Burning, numbness, or tingling feeling in genitals
- Shingles
- Shortness of breath
- Flushing
- Dizziness
- Passing out
- Loss of strength and energy
- Headache
- Nausea
- Fast heartbeat
- Lump in breast
- Breast soreness
- Swelling in the arms or legs
- Depression
- Progressive multifocal leukoencephalopathy like confusion, depression, trouble with memory, behavioral changes, change in strength on one side is greater than the other, difficulty speaking, change in balance, or vision changes.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.