Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Solution, Oral, as base:
Generic: 15 mg/5 mL (240 mL, 480 mL)
Solution, Oral, as sodium phosphate [strength expressed as base]:
Millipred: 10 mg/5 mL (237 mL [DSC]) [alcohol free, dye free; contains edetate disodium, methylparaben, saccharin sodium; grape flavor]
Pediapred: 5 mg/5 mL (120 mL) [alcohol free, dye free, sugar free; contains edetate disodium, methylparaben; raspberry flavor]
Veripred 20: 20 mg/5 mL (237 mL [DSC]) [alcohol free, dye free; contains edetate disodium, methylparaben, saccharin sodium; grape flavor]
Generic: 10 mg/5 mL (237 mL); 15 mg/5 mL (237 mL); 20 mg/5 mL (237 mL); 25 mg/5 mL (30 mL, 237 mL); 5 mg/5 mL (120 mL)
Syrup, Oral, as base:
Generic: 15 mg/5 mL (240 mL [DSC], 480 mL [DSC])
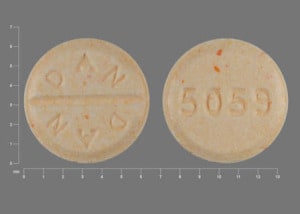
Tablet, Oral, as base:
Millipred: 5 mg [scored; contains fd&c yellow #10 (quinoline yellow), fd&c yellow #6 (sunset yellow), sodium benzoate]
Millipred DP: 5 mg [scored; contains fd&c yellow #10 (quinoline yellow), fd&c yellow #6 (sunset yellow), sodium benzoate]
Millipred DP 12-Day: 5 mg [scored; contains fd&c yellow #10 (quinoline yellow), fd&c yellow #6 (sunset yellow), sodium benzoate]
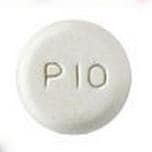
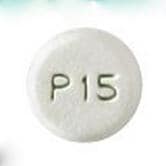
Tablet Disintegrating, Oral, as sodium phosphate [strength expressed as base]:
Orapred ODT: 10 mg, 15 mg, 30 mg [grape flavor]
Generic: 10 mg, 15 mg, 30 mg
Pharmacology
Mechanism of Action
Decreases inflammation by suppression of migration of polymorphonuclear leukocytes and reversal of increased capillary permeability; suppresses the immune system by reducing activity and volume of the lymphatic system
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid; well-absorbed
Distribution
Vd: 0.22 to 0.7 L/kg
Metabolism
Primarily hepatic
Excretion
Primarily urine (as sulfate and glucuronide conjugate)
Time to Peak
Plasma: 1 to 2 hours; prolonged with food
Duration of Action
18 to 36 hours (Pickup 1979)
Half-Life Elimination
2 to 4 hours; reduced in children and prolonged in hepatic disease (Pickup 1979)
Protein Binding
Concentration dependent: 70% to 90% (to albumin and corticosteroid binding globulin); decreased in elderly
Use in Specific Populations
Special Populations: Elderly
Mean unbound fraction of prednisolone was higher and Vss unbound prednisolone was reduced in elderly patients.
Use: Labeled Indications
Allergic states: Control of severe or incapacitating allergic conditions intractable to adequate trials of conventional treatment in asthma, atopic dermatitis, drug hypersensitivity reactions, seasonal or perennial allergic rhinitis, and serum sickness.
Dermatologic diseases: Bullous dermatitis herpetiformis; contact dermatitis; exfoliative erythroderma; exfoliative dermatitis; mycosis fungoides; pemphigus; severe erythema multiforme (Stevens-Johnson syndrome); severe psoriasis; severe seborrheic dermatitis.
Endocrine disorders: Congenital adrenal hyperplasia; hypercalcemia associated with cancer; nonsuppurative thyroiditis; primary or secondary adrenocortical insufficiency (hydrocortisone or cortisone is the first choice; synthetic analogs may be used in conjunction with mineralocorticoids where applicable).
GI diseases: During acute episodes of Crohn disease or ulcerative colitis.
Hematologic disorders: Acquired (autoimmune) hemolytic anemia; congenital (erythroid) hypoplastic anemia (Diamond-Blackfan anemia); erythroblastopenia (RBC anemia); immune thrombocytopenia (formerly known as idiopathic thrombocytopenic purpura), pure red cell aplasia; secondary thrombocytopenia.
Neoplastic diseases: Treatment of acute leukemia and aggressive lymphomas.
Nervous system: Acute exacerbations of multiple sclerosis; cerebral edema associated with primary or metastatic brain tumor, craniotomy, or head injury. Note: Treatment guidelines recommend the use of high dose IV or oral methylprednisolone for acute exacerbations of multiple sclerosis (AAN [Scott 2011]; NICE 2014).
Ophthalmic diseases: Allergic conjunctivitis; allergic corneal marginal ulcers; anterior segment inflammation; chorioretinitis; diffuse posterior uveitis and choroiditis; herpes zoster ophthalmicus; iritis and iridocyclitises; keratitis; optic neuritis; sympathetic ophthalmia; uveitis and other ocular inflammatory conditions unresponsive to topical corticosteroids.
Renal disorders: To induce diuresis or remission of proteinuria in nephrotic syndrome, without uremia, of the idiopathic type or that due to lupus erythematosus.
Respiratory diseases: Acute exacerbations of chronic obstructive pulmonary disease (COPD); allergic bronchopulmonary aspergillosis; aspiration pneumonitis; asthma; berylliosis; fulminating or disseminated pulmonary tuberculosis when used concurrently with appropriate antituberculous chemotherapy; hypersensitivity pneumonitis; idiopathic bronchiolitis obliterans with organizing pneumonia; idiopathic eosinophilic pneumonias; idiopathic pulmonary fibrosis; Loeffler syndrome (not manageable by other means); Pneumocystis carinii pneumonia (PCP) associated with hypoxemia occurring in an HIV-positive individual who is also under treatment with appropriate anti-PCP antibiotics; symptomatic sarcoidosis.
Rheumatic disorders: As adjunctive therapy for short-term administration in acute and subacute bursitis, acute gout flares, acute nonspecific tenosynovitis, ankylosing spondylitis, epicondylitis, polymyalgia rheumatica/temporal arteritis, posttraumatic osteoarthritis, psoriatic arthritis, relapsing polychondritis, rheumatoid arthritis (including juvenile rheumatoid arthritis), synovitis of osteoarthritis, acute rheumatic carditis, systemic lupus erythematosus, dermatomyositis/polymyositis, Sjogren syndrome, and certain cases of vasculitis.
Miscellaneous: Acute or chronic solid organ rejection; trichinosis with neurologic or myocardial involvement; tuberculous meningitis with subarachnoid block or impending block, tuberculosis with enlarged mediastinal lymph nodes causing respiratory difficulty, tuberculosis with pleural or pericardial effusion (use appropriate antituberculous chemotherapy concurrently when treating any tuberculosis complications).
Use: Off Label
Alcoholic hepatitis (severe)yes
Based on the American College of Gastroenterology (ACG) for Alcoholic Liver Disease and American Association for the Study of Liver Diseases (AASLD) guidelines, prednisolone (systemic) given for severe alcoholic hepatitis is effective and recommended in the management of this condition.
Asthma exacerbationyes
Based on the Global Initiative for Asthma (GINA): Global Strategy for Asthma Management and Prevention guidelines and the National Heart, Lung, and Blood Institute (NHLBI) and National Asthma Education and Prevention Program (NAEPP) Expert Panel Report 3 guidelines for the diagnosis and management of asthma, prednisolone is effective and recommended in the management of severe asthma exacerbations.
Bell palsyayes
Data from a randomized, double-blind, placebo-controlled, factorial study supports the use of prednisolone (systemic) in the treatment of Bell palsy. Early treatment with prednisolone (systemic) significantly improved the changes of complete recovery at 3 and 9 months Sullivan 2007. Additional data from a randomized, double-blind, placebo-controlled, multicenter study also supports the use of prednisolone (systemic) in the treatment of Bell palsy. Prednisolone (systemic) shortened the time to complete recovery in patients with Bell's palsy Engstom 2008. In another randomized, double-blind, placebo-controlled, multicenter study the use of prednisolone (systemic) in the treatment of Bell palsy was found to significantly reduce mild and moderate sequelae of Bell's palsy Berg 2012.
Based on the American Academy of Otolaryngology, Head and Neck Surgery, Clinical Practice Guideline: Bell's Palsy, prednisolone (systemic) given for Bell's palsy is effective and recommended in the management of this condition.
Chronic obstructive pulmonary disease (COPD) (acute exacerbation)yes
Based on the Global Strategy for Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (GOLD) guidelines, prednisolone (systemic) given for acute exacerbation of COPD is effective and recommended in the management of this condition. Short-term treatment with systemic corticosteroids has been shown to reduce recovery time, risk of early relapse, treatment failure, and length of hospital stay, as well as to improve lung function. However, long-term use is associated with significant adverse effects GOLD 2018.
Contraindications
Hypersensitivity to prednisolone or any component of the formulation; live or attenuated virus vaccines (with immunosuppressive doses of corticosteroids); systemic fungal infections.
Canadian labeling: Additional contraindications (not in US labeling): Chicken pox; measles; uncontrolled active infections.
Documentation of allergenic cross-reactivity for corticosteroids is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Dosage and Administration
Dosing: Adult
Dose depends upon condition being treated and response of patient. Consider alternate day therapy for long-term therapy. Discontinuation of long-term therapy requires gradual withdrawal by tapering the dose.
Usual dose (range): Oral: 5 to 60 mg/day
Adrenal insufficiency, chronic (primary, classic congenital adrenal hyperplasia) (off-label dose; alternative agent): Oral: 3 to 6 mg daily in 1 to 2 divided doses; use of a liquid dosage form may be preferable to allow for better dose titration (Endocrine Society [Bornstein 2016]; Endocrine Society [Speiser 2018]).
Alcoholic hepatitis (severe) (Maddrey Discriminant Function [MDF] score ≥32) (off-label use): Oral: 40 mg daily for 28 days, followed by a 2 to 4 week taper (AASLD [O'Shea 2010]; ACG [Singal 2018])
Asthma exacerbations: Oral:
Global Initiative for Asthma guidelines (GINA 2018): Management in primary care or acute care facility: 1 mg/kg/day (maximum: 50 mg/day) as a single daily dose usually given for 5 to 7 days
National Asthma Education and Prevention Program guidelines (NAEPP 2007):
Asthma exacerbations (emergency care or hospital doses): 40 to 80 mg/day in a single dose or in 2 divided doses until peak expiratory flow is 70% of predicted or personal best
Short-course outpatient "burst" (acute asthma): 40 to 60 mg/day in a single dose or in 2 divided doses for 5 to 10 days. Note: Burst should be continued until symptoms resolve and peak expiratory flow is at least 80% of personal best; usually requires 3 to 10 days of treatment; longer treatment may be required
Long-term treatment: 7.5 to 60 mg daily given as a single dose in the morning or every other day as needed for asthma control
Bell’s palsy (off-label use): Oral: 60 mg once daily for 5 days, then taper dose downward by 10 mg daily for 5 days (total treatment duration: 10 days) (Berg 2012; Engstrom 2008) or 50 mg daily (in 1 or 2 divided doses) for 10 days (begin within 72 hours of onset of symptoms) (Baugh 2013; Sullivan 2007)
Chronic obstructive pulmonary disease (acute exacerbation) (off-label use): Oral: 40 mg daily for 5 to 7 days (GOLD 2018).
Gout, acute flares: Oral: 0.5 mg/kg/day for 5 to 10 days followed by discontinuation (ACR [Khanna 2012]) or 30 to 40 mg/day given once daily or in 2 divided doses until symptom improvement, followed by a 7- to 10-day taper (or 14- to 21-day taper in patients with multiple prior flares) (Becker 2018)
Multiple sclerosis:
Note: Treatment guidelines recommend the use of high dose IV or oral methylprednisolone for acute exacerbations of multiple sclerosis (AAN [Scott 2011]; NICE 2014).
Oral: 200 mg daily for 1 week followed by 80 mg every other day for 1 month
Dosing: Geriatric
Refer to adult dosing; use lowest effective dose.
Dosing: Pediatric
Note: Dose depends upon condition being treated and response of patient; dosage for infants and children should be based on disease severity and patient response, rather than by rigid adherence to dosage guidelines by age, weight, or body surface area. Consider alternate day therapy for long-term therapy. Discontinuation of long-term therapy requires gradual withdrawal by tapering the dose.
Bronchopulmonary dysplasia, treatment: Infants: Oral: 2 mg/kg/day divided twice daily for 5 days, followed by 1 mg/kg/day once daily for 3 days, followed by 1 mg/kg/dose every other day for 3 doses was used in 131 former premature neonates (postmenstrual age: ≥36 weeks) with BPD; results showed weaning of supplemental oxygen was facilitated in patients with capillary pCO2 <48.5 mm Hg and pulmonary acuity score <0.5 (Bhandari 2008)
Asthma: NIH Asthma Guidelines (NAEPP 2007):
Infants and Children <12 years: Oral:
Asthma exacerbations (emergency care or hospital doses): 1 to 2 mg/kg/day in 2 divided doses (maximum: 60 mg/day) until peak expiratory flow is 70% of predicted or personal best
Short-course "burst" (acute asthma): 1 to 2 mg/kg/day in divided doses 1 to 2 times/day for 3 to 10 days; maximum dose: 60 mg/day; Note: Burst should be continued until symptoms resolve or patient achieves peak expiratory flow 80% of personal best; usually requires 3 to 10 days of treatment (~5 days on average); longer treatment may be required
Long-term treatment: 0.25 to 2 mg/kg/day given as a single dose in the morning or every other day as needed for asthma control; maximum dose: 60 mg/day
Children ≥12 years and Adolescents: Oral:
Asthma exacerbations (emergency care or hospital doses): 40 to 80 mg/day in divided doses 1 to 2 times/day until peak expiratory flow is 70% of predicted or personal best
Short-course "burst" (acute asthma): 40 to 60 mg/day in divided doses 1 to 2 times/day for 3 to 10 days; Note: Burst should be continued until symptoms resolve and peak expiratory flow is at least 80% of personal best; usually requires 3 to 10 days of treatment (~5 days on average); longer treatment may be required
Long-term treatment: 7.5 to 60 mg daily given as a single dose in the morning or every other day as needed for asthma control
Anti-inflammatory or immunosuppressive dose: Infants, Children, and Adolescents: Oral: 0.1 to 2 mg/kg/day in divided doses 1 to 4 times/day
Kawasaki disease (KD), treatment: Limited data available: Note: Use to transition patients receiving IV corticosteroids for treatment of KD (in combination with IVIG and aspirin). Infants and Children: Oral: 2 mg/kg/day in divided doses every 8 hours until CRP normalizes; maximum daily dose: 60 mg/day; once CRP normalized, decrease dose every 5 days using the following taper: 2 mg/kg/day for 5 days (maximum daily dose: 60 mg/day), then 1 mg/kg/day for 5 days (maximum daily dose: 30 mg/day), then 0.5 mg/kg/day for 5 days (maximum daily dose: 15 mg/day), then discontinue; a longer course, tapering over 2 to 3 weeks, may be considered (AHA [McCrindle 2017]; Kobayashi 2012; Kobayashi 2013)
Nephrotic syndrome; steroid-sensitive (SSNS): Children and Adolescents: Note: Obese patients should be dosed based on ideal body weight: Oral:
Initial episode: 2 mg/kg/day or 60 mg/m2/day once daily, maximum daily dose: 60 mg/day for 4 to 6 weeks; then adjust to an alternate-day schedule of 1.5 mg/kg/dose or 40 mg/m2/dose on alternate days as a single dose, maximum dose: 40 mg/dose (Gipson 2009; KDIGO 2012; KDOQI 2013); duration of therapy based on patient response.
Relapse: 2 mg/kg/day or 60 mg/m2/day once daily, maximum daily dose: 60 mg/day; continue until complete remission for at least 3 days; then adjust to an alternate-day schedule of 1.5 mg/kg/dose or 40 mg/m2/dose on alternate days as a single dose, maximum dose: 40 mg/dose, recommended duration of alternate day dosing is variable: may continue for at least 4 weeks then taper. Longer duration of treatment may be necessary in patients who relapse frequently, some patients may require up to 3 months of treatment (Gipson 2009; KDIGO 2012; KDOQI 2013).
Maintenance therapy for frequently relapsing SSNS: Taper previous dose down to lowest effective dose which maintains remission using an alternate day schedule; usual effective range: 0.1 to 0.5 mg/kg/dose on alternating days; other patients may require doses up to 0.7 mg/kg/dose every other day (KDIGO 2012; KDOQI 2013)
Administration
Oral: Administer after meals or with food or milk to decrease GI upset.
Orapred ODT: Do not break, cut, split or use partial tablet. Remove tablet from blister pack just prior to use. May swallow whole or allow to dissolve on tongue.
Dietary Considerations
Should be taken after meals or with food or milk to decrease GI upset; increase dietary intake of pyridoxine, vitamin C, vitamin D, folate, calcium, and phosphorus.
Storage
Millipred: Store at 20°C to 25°C (68°F to 77°F).
Oral solution (generic): Storage recommendations may vary by manufacturer; refer to manufacturer’s labeling for storage requirements.
Orapred ODT: Store at 20°C to 25°C (68°F to 77°F) in blister pack. Protect from moisture.
Orapred, Veripred 20: Store at 2°C to 8°C (36°F to 46°F).
Pediapred: Store at 4°C to 25°C (39°F to 77°F); may be refrigerated.
PrednisoLONE (Systemic) Images
Drug Interactions
Acetylcholinesterase Inhibitors: Corticosteroids (Systemic) may enhance the adverse/toxic effect of Acetylcholinesterase Inhibitors. Increased muscular weakness may occur. Monitor therapy
Aldesleukin: Corticosteroids may diminish the antineoplastic effect of Aldesleukin. Avoid combination
Amphotericin B: Corticosteroids (Systemic) may enhance the hypokalemic effect of Amphotericin B. Monitor therapy
Androgens: Corticosteroids (Systemic) may enhance the fluid-retaining effect of Androgens. Monitor therapy
Antacids: May decrease the bioavailability of Corticosteroids (Oral). Management: Consider separating doses by 2 or more hours. Budesonide enteric coated tablets could dissolve prematurely if given with drugs that lower gastric acid, with unknown impact on budesonide therapeutic effects. Consider therapy modification
Antidiabetic Agents: Hyperglycemia-Associated Agents may diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Aprepitant: May increase the serum concentration of Corticosteroids (Systemic). Management: No dose adjustment is needed for single 40 mg aprepitant doses. For other regimens, reduce oral dexamethasone or methylprednisolone doses by 50%, and IV methylprednisolone doses by 25%. Antiemetic regimens containing dexamethasone reflect this adjustment. Consider therapy modification
Axicabtagene Ciloleucel: Corticosteroids (Systemic) may diminish the therapeutic effect of Axicabtagene Ciloleucel. Management: Avoid use of corticosteroids as premedication before axicabtagene ciloleucel. Corticosteroids may, however, be required for treatment of cytokine release syndrome or neurologic toxicity. Consider therapy modification
Baricitinib: Immunosuppressants may enhance the immunosuppressive effect of Baricitinib. Management: Use of baricitinib in combination with potent immunosuppressants such as azathioprine or cyclosporine is not recommended. Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted. Consider therapy modification
BCG (Intravesical): Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Bile Acid Sequestrants: May decrease the absorption of Corticosteroids (Oral). Monitor therapy
Calcitriol (Systemic): Corticosteroids (Systemic) may diminish the therapeutic effect of Calcitriol (Systemic). Monitor therapy
Carbimazole: May decrease the serum concentration of PrednisoLONE (Systemic). Monitor therapy
Cladribine: May enhance the immunosuppressive effect of Immunosuppressants. Avoid combination
Coccidioides immitis Skin Test: Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. Monitor therapy
Corticorelin: Corticosteroids may diminish the therapeutic effect of Corticorelin. Specifically, the plasma ACTH response to corticorelin may be blunted by recent or current corticosteroid therapy. Monitor therapy
Cosyntropin: Corticosteroids (Systemic) may diminish the diagnostic effect of Cosyntropin. Monitor therapy
CycloSPORINE (Systemic): PrednisoLONE (Systemic) may decrease the serum concentration of CycloSPORINE (Systemic). CycloSPORINE (Systemic) may increase the serum concentration of PrednisoLONE (Systemic). PrednisoLONE (Systemic) may increase the serum concentration of CycloSPORINE (Systemic). Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of PrednisoLONE (Systemic). Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of PrednisoLONE (Systemic). Monitor therapy
Deferasirox: Corticosteroids (Systemic) may enhance the adverse/toxic effect of Deferasirox. Specifically, the risk for GI ulceration/irritation or GI bleeding may be increased. Monitor therapy
Deferasirox: Corticosteroids may enhance the adverse/toxic effect of Deferasirox. Specifically, the risk for GI ulceration/irritation or GI bleeding may be increased. Monitor therapy
Denosumab: May enhance the adverse/toxic effect of Immunosuppressants. Specifically, the risk for serious infections may be increased. Monitor therapy
Desirudin: Corticosteroids (Systemic) may enhance the anticoagulant effect of Desirudin. More specifically, corticosteroids may increase hemorrhagic risk during desirudin treatment. Management: Discontinue treatment with systemic corticosteroids prior to desirudin initiation. If concomitant use cannot be avoided, monitor patients receiving these combinations closely for clinical and laboratory evidence of excessive anticoagulation. Consider therapy modification
Desmopressin: Corticosteroids (Systemic) may enhance the hyponatremic effect of Desmopressin. Avoid combination
DilTIAZem: May increase the serum concentration of Corticosteroids (Systemic). Monitor therapy
Echinacea: May diminish the therapeutic effect of Immunosuppressants. Consider therapy modification
Estrogen Derivatives: May increase the serum concentration of Corticosteroids (Systemic). Monitor therapy
Fexinidazole [INT]: Corticosteroids (Systemic) may enhance the arrhythmogenic effect of Fexinidazole [INT]. Avoid combination
Fingolimod: Immunosuppressants may enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). Consider therapy modification
Fosaprepitant: May increase the serum concentration of Corticosteroids (Systemic). The active metabolite aprepitant is likely responsible for this effect. Consider therapy modification
Hyaluronidase: Corticosteroids may diminish the therapeutic effect of Hyaluronidase. Management: Patients receiving corticosteroids (particularly at larger doses) may not experience the desired clinical response to standard doses of hyaluronidase. Larger doses of hyaluronidase may be required. Consider therapy modification
Indacaterol: May enhance the hypokalemic effect of Corticosteroids (Systemic). Monitor therapy
Indium 111 Capromab Pendetide: Corticosteroids (Systemic) may diminish the diagnostic effect of Indium 111 Capromab Pendetide. Avoid combination
Isoniazid: Corticosteroids (Systemic) may decrease the serum concentration of Isoniazid. Monitor therapy
Leflunomide: Immunosuppressants may enhance the adverse/toxic effect of Leflunomide. Specifically, the risk for hematologic toxicity such as pancytopenia, agranulocytosis, and/or thrombocytopenia may be increased. Management: Consider not using a leflunomide loading dose in patients receiving other immunosuppressants. Patients receiving both leflunomide and another immunosuppressant should be monitored for bone marrow suppression at least monthly. Consider therapy modification
Loop Diuretics: Corticosteroids (Systemic) may enhance the hypokalemic effect of Loop Diuretics. Monitor therapy
Macimorelin: Corticosteroids (Systemic) may diminish the diagnostic effect of Macimorelin. Avoid combination
MethIMAzole: May decrease the serum concentration of PrednisoLONE (Systemic). Monitor therapy
Mifamurtide: Corticosteroids (Systemic) may diminish the therapeutic effect of Mifamurtide. Avoid combination
MiFEPRIStone: May diminish the therapeutic effect of Corticosteroids (Systemic). MiFEPRIStone may increase the serum concentration of Corticosteroids (Systemic). Management: Avoid mifepristone in patients who require long-term corticosteroid treatment of serious illnesses or conditions (e.g., for immunosuppression following transplantation). Corticosteroid effects may be reduced by mifepristone treatment. Avoid combination
Mitotane: May decrease the serum concentration of Corticosteroids (Systemic). Consider therapy modification
Natalizumab: Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. Avoid combination
Neuromuscular-Blocking Agents (Nondepolarizing): May enhance the adverse neuromuscular effect of Corticosteroids (Systemic). Increased muscle weakness, possibly progressing to polyneuropathies and myopathies, may occur. Consider therapy modification
Nicorandil: Corticosteroids (Systemic) may enhance the adverse/toxic effect of Nicorandil. Gastrointestinal perforation has been reported in association with this combination. Monitor therapy
Nivolumab: Immunosuppressants may diminish the therapeutic effect of Nivolumab. Consider therapy modification
Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective): Corticosteroids (Systemic) may enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective). Monitor therapy
Nonsteroidal Anti-Inflammatory Agents (Nonselective): Corticosteroids (Systemic) may enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents (Nonselective). Monitor therapy
Ocrelizumab: May enhance the immunosuppressive effect of Immunosuppressants. Monitor therapy
Pidotimod: Immunosuppressants may diminish the therapeutic effect of Pidotimod. Monitor therapy
Pimecrolimus: May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Quinolones: Corticosteroids (Systemic) may enhance the adverse/toxic effect of Quinolones. Specifically, the risk of tendonitis and tendon rupture may be increased. Monitor therapy
Ritodrine: Corticosteroids may enhance the adverse/toxic effect of Ritodrine. Monitor therapy
Ritonavir: May increase the serum concentration of PrednisoLONE (Systemic). Management: Consider prednisolone dose reductions in patients receiving ritonavir and monitor for increased adverse effects with concomitant use. Consider therapy modification
Roflumilast: May enhance the immunosuppressive effect of Immunosuppressants. Consider therapy modification
Salicylates: May enhance the adverse/toxic effect of Corticosteroids (Systemic). These specifically include gastrointestinal ulceration and bleeding. Corticosteroids (Systemic) may decrease the serum concentration of Salicylates. Withdrawal of corticosteroids may result in salicylate toxicity. Monitor therapy
Sargramostim: Corticosteroids (Systemic) may enhance the therapeutic effect of Sargramostim. Specifically, corticosteroids may enhance the myeloproliferative effects of sargramostim. Monitor therapy
Siponimod: Immunosuppressants may enhance the immunosuppressive effect of Siponimod. Monitor therapy
Sipuleucel-T: Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. Consider therapy modification
Somatropin: Corticosteroids (Systemic) may diminish the therapeutic effect of Somatropin. Monitor therapy
Tacrolimus (Systemic): Corticosteroids (Systemic) may decrease the serum concentration of Tacrolimus (Systemic). Conversely, when discontinuing corticosteroid therapy, tacrolimus concentrations may increase. Monitor therapy
Tacrolimus (Topical): May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Tertomotide: Immunosuppressants may diminish the therapeutic effect of Tertomotide. Monitor therapy
Thiazide and Thiazide-Like Diuretics: Corticosteroids (Systemic) may enhance the hypokalemic effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Tisagenlecleucel: Corticosteroids (Systemic) may diminish the therapeutic effect of Tisagenlecleucel. Management: Avoid use of corticosteroids as premedication or at any time during treatment with tisagenlecleucel, except in the case of life-threatening emergency (such as resistant cytokine release syndrome). Consider therapy modification
Tofacitinib: Immunosuppressants may enhance the immunosuppressive effect of Tofacitinib. Management: Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted, and this warning seems particularly focused on more potent immunosuppressants. Consider therapy modification
Trastuzumab: May enhance the neutropenic effect of Immunosuppressants. Monitor therapy
Upadacitinib: Immunosuppressants may enhance the immunosuppressive effect of Upadacitinib. Avoid combination
Urea Cycle Disorder Agents: Corticosteroids (Systemic) may diminish the therapeutic effect of Urea Cycle Disorder Agents. More specifically, Corticosteroids (Systemic) may increase protein catabolism and plasma ammonia concentrations, thereby increasing the doses of Urea Cycle Disorder Agents needed to maintain these concentrations in the target range. Monitor therapy
Vaccines (Inactivated): Immunosuppressants may diminish the therapeutic effect of Vaccines (Inactivated). Management: Vaccine efficacy may be reduced. Complete all age-appropriate vaccinations at least 2 weeks prior to starting an immunosuppressant. If vaccinated during immunosuppressant therapy, revaccinate at least 3 months after immunosuppressant discontinuation. Consider therapy modification
Vaccines (Live): Corticosteroids (Systemic) may enhance the adverse/toxic effect of Vaccines (Live). Corticosteroids (Systemic) may diminish the therapeutic effect of Vaccines (Live). Management: Doses equivalent to less than 2 mg/kg or 20 mg per day of prednisone administered for less than 2 weeks are not considered sufficiently immunosuppressive to create vaccine safety concerns. Higher doses and longer durations should be avoided. Consider therapy modification
Warfarin: Corticosteroids (Systemic) may enhance the anticoagulant effect of Warfarin. Monitor therapy
Test Interactions
May decrease response to skin tests.
Adverse Reactions
Frequency not defined.
Cardiovascular: Cardiac failure, cardiomyopathy, edema, facial edema, hypertension
Central nervous system: Headache, insomnia, malaise, myasthenia, nervousness, pseudotumor cerebri, psychological disorder, seizure, vertigo
Dermatologic: Diaphoresis, facial erythema, skin atrophy, suppression of skin test reaction, urticaria
Endocrine & metabolic: Cushing's syndrome, diabetes mellitus, growth suppression, hirsutism, HPA-axis suppression, hyperglycemia, hypernatremia, hypokalemia, hypokalemic alkalosis, menstrual disease, negative nitrogen balance, weight gain
Gastrointestinal: Abdominal distention, carbohydrate intolerance, dyspepsia, increased appetite, nausea, pancreatitis, peptic ulcer, ulcerative esophagitis
Hematologic & oncologic: Bruise, petechia
Hepatic: Increased liver enzymes (usually reversible)
Neuromuscular & skeletal: Amyotrophy, arthralgia, aseptic necrosis of bones (humeral/femoral heads), bone fracture, rupture of tendon, weakness
Ophthalmic: Cataract, exophthalmos, eye irritation, eyelid edema, glaucoma, increased intraocular pressure
Respiratory: Epistaxis
Miscellaneous: Wound healing impairment
<1%, postmarketing, and/or case reports: Venous thrombosis (Johannesdottir 2013)
Warnings/Precautions
Concerns related to adverse effects:
- Adrenal suppression: May cause hypercortisolism or suppression of hypothalamic-pituitary-adrenal (HPA) axis, particularly in younger children or in patients receiving high doses for prolonged periods. HPA axis suppression may lead to adrenal crisis. Withdrawal and discontinuation of a corticosteroid should be done slowly and carefully. Particular care is required when patients are transferred from systemic corticosteroids to inhaled products due to possible adrenal insufficiency or withdrawal from steroids, including an increase in allergic symptoms. Adult patients receiving >20 mg per day of prednisone (or equivalent) may be most susceptible. Fatalities have occurred due to adrenal insufficiency in asthmatic patients during and after transfer from systemic corticosteroids to aerosol steroids; aerosol steroids do not provide the systemic steroid needed to treat patients having trauma, surgery, or infections.
- Anaphylactoid reactions: Rare cases of anaphylactoid reactions have been observed in patients receiving corticosteroids.
- Immunosuppression: Prolonged use of corticosteroids may also increase the incidence of secondary infection, cause activation of latent infections, mask acute infection (including fungal infections) or prolong or exacerbate viral infections or limit response to killed or inactivated vaccines. Exposure to chickenpox or measles should be avoided; corticosteroids should not be used to treat ocular herpes simplex. Corticosteroids should not be used for cerebral malaria or viral hepatitis. Close observation is required in patients with latent tuberculosis and/or TB reactivity; restrict use in active TB (only fulminating or disseminated TB in conjunction with antituberculosis treatment). Amebiasis should be ruled out in any patient with recent travel to tropic climates or unexplained diarrhea prior to initiation of corticosteroids. Use with extreme caution in patients with Strongyloides infections; hyperinfection, dissemination and fatalities have occurred.
- Kaposi sarcoma: Prolonged treatment with corticosteroids has been associated with the development of Kaposi's sarcoma (case reports); if noted, discontinuation of therapy should be considered (Goedert 2002).
- Myopathy: Acute myopathy has been reported with high dose corticosteroids, usually in patients with neuromuscular transmission disorders; may involve ocular and/or respiratory muscles; monitor creatine kinase; recovery may be delayed.
- Psychiatric disturbances: Corticosteroid use may cause psychiatric disturbances, including severe depression, euphoria, insomnia, mood swings, personality changes, and frank psychotic manifestations. Preexisting psychiatric conditions may be exacerbated by corticosteroid use.
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with HF and/or hypertension; use has been associated with fluid retention, electrolyte disturbances, and hypertension. Use with caution following acute MI; corticosteroids have been associated with myocardial rupture.
- Diabetes: Use corticosteroids with caution in patients with diabetes mellitus; may alter glucose production/regulation leading to hyperglycemia.
- Gastrointestinal disease: Use with caution in patients with GI diseases (diverticulitis, fresh intestinal anastomoses, active or latent peptic ulcer, ulcerative colitis, abscess or other pyogenic infection) due to perforation risk. Avoid ethanol may enhance gastric mucosal irritation.
- Head injury: Increased mortality was observed in patients receiving high-dose IV methylprednisolone. High-dose corticosteroids should not be used for the management of head injury.
- Hepatic impairment: Use with caution in patients with hepatic impairment, including cirrhosis; long-term use has been associated with fluid retention.
- Myasthenia gravis: Use with caution in patients with myasthenia gravis; exacerbation of symptoms has occurred especially during initial treatment with corticosteroids.
- Ocular disease: Use with caution in patients with cataracts and/or glaucoma; increased intraocular pressure, open-angle glaucoma, and cataracts have occurred with prolonged use. Use with caution in patients with a history of ocular herpes simplex; corneal perforation has occurred; do not use in active ocular herpes simplex. Not recommended for the treatment of optic neuritis; may increase frequency of new episodes. Consider routine eye exams in chronic users.
- Osteoporosis: Use with caution in patients with osteoporosis; high doses and/or long-term use of corticosteroids have been associated with increased bone loss and osteoporotic fractures.
- Renal impairment: Use with caution in patients with renal impairment; fluid retention may occur.
- Seizure disorders: Use corticosteroids with caution in patients with a history of seizure disorder; seizures have been reported with adrenal crisis.
- Systemic sclerosis (scleroderma): Use of higher-dose corticosteroid therapy (≥15 mg/day of prednisone or equivalent) in patients with systemic sclerosis may increase the risk of scleroderma renal crisis; avoid use when possible (Steen 1998; Trang 2012).
- Thyroid disease: Changes in thyroid status may necessitate dosage adjustments; metabolic clearance of corticosteroids increases in hyperthyroid patients and decreases in hypothyroid ones.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Use cautiously in elderly patients with the smallest possible effective dose for the shortest duration.
- Pediatric: May affect growth velocity; growth should be routinely monitored in pediatric patients.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol derivative with caution in neonates. See manufacturer’s labeling.
- Propylene glycol: Some dosage forms may contain propylene glycol; large amounts are potentially toxic and have been associated hyperosmolality, lactic acidosis, seizures, and respiratory depression; use caution (AAP 1997; Zar 2007).
Other warnings/precautions:
- Discontinuation of therapy: Withdraw therapy with gradual tapering of dose.
- Stress: Patients may require higher doses when subject to stress (ie, trauma, surgery, severe infection).
Monitoring Parameters
Blood pressure; blood glucose, electrolytes; weight; intraocular pressure (use >6 weeks); bone mineral density; growth and development in children; chest x-ray during prolonged therapy; HPA axis suppression.
Pregnancy
Pregnancy Risk Factor
C/D (manufacturer specific)
Pregnancy Considerations
Adverse events have been observed with corticosteroids in animal reproduction studies. Prednisolone crosses the placenta; prior to reaching the fetus, prednisolone is converted by placental enzymes to prednisone. As a result, the amount of prednisolone reaching the fetus is ~8 to 10 times lower than the maternal serum concentration (healthy women at term; similar results observed with preterm pregnancies complicated by HELLP syndrome) (Beitins 1972; van Runnard Heimel 2005). Some studies have shown an association between first trimester systemic corticosteroid use and oral clefts or decreased birth weight; however, information is conflicting and may be influenced by maternal dose/indication for use (Lunghi 2010; Park-Wyllie 2000; Pradat 2003). Hypoadrenalism may occur in newborns following maternal use of corticosteroids in pregnancy; monitor.
Prednisolone may be used (alternative agent) to treat primary adrenal insufficiency (PAI) in pregnant women. Pregnant females with PAI should be monitored at least once each trimester (Endocrine Society [Bornstein 2016]). Prednisolone may be used to treat females during pregnancy who require therapy for congenital adrenal hyperplasia (Endocrine Society [Speiser 2018]).
When systemic corticosteroids are needed in pregnancy for rheumatic disorders, it is generally recommended to use the lowest effective dose for the shortest duration of time, avoiding high doses during the first trimester (Götestam Skorpen 2016; Makol 2011; Østensen 2009).
For dermatologic disorders in pregnant females, systemic corticosteroids are generally not preferred for initial therapy; should be avoided during the first trimester; and used during the second or third trimester at the lowest effective dose (Bae 2012; Leachman 2006). Topical agents are preferred for managing atopic dermatitis in pregnancy; for severe symptomatic or recalcitrant atopic dermatitis, a short course of prednisolone may be used during the third trimester (Koutroulis 2011).
Uncontrolled asthma is associated with adverse events on pregnancy (increased risk of perinatal mortality, preeclampsia, preterm birth, low birth weight infants). Poorly controlled asthma or asthma exacerbations may have a greater fetal/maternal risk than what is associated with appropriately used asthma medications. Inhaled corticosteroids are recommended for the treatment of asthma during pregnancy; however, systemic corticosteroids should be used to control acute exacerbations or treat severe persistent asthma (ACOG 2008; GINA 2018; Namazy 2016).
Patient Education
What is this drug used for?
- It is used for many health problems like allergy signs, asthma, adrenal gland problems, blood problems, skin rashes, or swelling problems.
- This is not a list of all health problems that this drug may be used for. Talk with the doctor.
Frequently reported side effects of this drug
- Nausea
- Increased hunger
- Weight gain
- Trouble sleeping
- Agitation
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- High blood sugar like confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit
- Cushing syndrome like weight gain in upper back or abdomen; moon face; severe headache; or slow healing
- Adrenal gland problems like severe nausea, vomiting, severe dizziness, passing out, muscle weakness, severe fatigue, mood changes, lack of appetite, or weight loss
- Low potassium like muscle pain or weakness, muscle cramps, or an abnormal heartbeat
- Pancreatitis like severe abdominal pain, severe back pain, severe nausea, or vomiting
- Skin changes like acne, stretch marks, slow healing, or hair growth
- Severe loss of strength and energy
- Irritability
- Tremors
- Fast heartbeat
- Confusion
- Sweating a lot
- Dizziness
- Passing out
- Severe headache
- Shortness of breath
- Excessive weight gain
- Swelling of arms or legs
- Chest pain
- Menstrual changes
- Joint pain
- Bone pain
- Vision changes
- Behavioral changes
- Depression
- Seizures
- Burning or numbness feeling
- Bruising
- Bleeding
- Severe abdominal pain
- Black, tarry, or bloody stools
- Vomiting blood
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.