Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Liquid, Oral, as hydrochloride:
Childrens Silfedrine: 15 mg/5 mL (118 mL, 237 mL) [grape flavor]
Nasal Decongestant: 30 mg/5 mL (118 mL) [contains fd&c red #40, methylparaben, saccharin sodium, sodium benzoate; raspberry flavor]
Sudafed Childrens: 15 mg/5 mL (118 mL) [alcohol free, sugar free; contains brilliant blue fcf (fd&c blue #1), edetate disodium, fd&c red #40, menthol, polyethylene glycol, saccharin sodium, sodium benzoate; grape flavor]
Syrup, Oral, as hydrochloride:
Nasal Decongestant: 30 mg/5 mL (473 mL [DSC]) [contains fd&c red #40, methylparaben, saccharin sodium, sodium benzoate; raspberry flavor]
Tablet, Oral, as hydrochloride:
Genaphed: 30 mg
Nasal Decongestant: 30 mg [contains fd&c red #40 aluminum lake, fd&c yellow #6 aluminum lake]
Nasal Decongestant: 30 mg [contains fd&c red #40 aluminum lake, polysorbate 80]
Shopko Nasal Decongestant Max: 30 mg [contains fd&c red #40 aluminum lake]
Simply Stuffy: 30 mg
Sudafed: 30 mg [contains fd&c red #40 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Sudafed Congestion: 30 mg [contains fd&c red #40 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Sudafed Sinus Congestion: 30 mg [contains fd&c red #40 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
SudoGest: 30 mg [DSC] [contains corn starch, fd&c red #40 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
SudoGest: 30 mg [contains fd&c red #40 aluminum lake, fd&c yellow #6 aluminum lake]
SudoGest: 60 mg
SudoGest: 60 mg [scored]
SudoGest Maximum Strength: 30 mg [gluten free; contains fd&c red #40 aluminum lake]
Generic: 30 mg, 60 mg
Tablet Abuse-Deterrent, Oral, as hydrochloride:
Nexafed: 30 mg
Zephrex-D: 30 mg
Tablet Extended Release 12 Hour, Oral, as hydrochloride:
Decongestant 12Hour Max St: 120 mg [contains polysorbate 80]
Shopko Nasal Decongestant: 120 mg
Sudafed 12 Hour: 120 mg [DSC]
Sudafed Sinus Congestion 12HR: 120 mg
SudoGest 12 Hour: 120 mg
Generic: 120 mg
Tablet Extended Release 24 Hour, Oral, as hydrochloride:
Sudafed Sinus Congestion 24HR: 240 mg
Pharmacology
Mechanism of Action
Directly stimulates alpha-adrenergic receptors of respiratory mucosa causing vasoconstriction; directly stimulates beta-adrenergic receptors causing bronchial relaxation, increased heart rate and contractility
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid (Simons, 1996)
Distribution
Children: ~2.5 L/kg (Simons, 1996); Adults: 2.64-3.51 L/kg (Kanfer, 1993)
Metabolism
Undergoes n-demethylation to norpseudoephedrine (active) (Chua, 1989; Kanfer, 1993); Hepatic (<1%) (Kanfer, 1993)
Excretion
Urine (43% to 96% as unchanged drug, 1% to 6% as active norpseudoephedrine); dependent on urine pH and flow rate; alkaline urine decreases renal elimination of pseudoephedrine (Kanfer, 1993)
Onset of Action
Decongestant: Oral: 30 minutes (Chua, 1989); Peak effect: Decongestant: Oral: ~1-2 hours (Chua, 1989)
Time to Peak
Children (immediate release) ~2 hours (Simons, 1996)
Adults (immediate release): 1-3 hours (dose dependent) (Kanfer, 1993)
Duration of Action
Immediate release tablet: 3-8 hours (Chua, 1989)
Half-Life Elimination
Varies by urine pH and flow rate; alkaline urine decreases renal elimination of pseudoephedrine (Kanfer, 1993)
Children: ~3 hours (urine pH ~6.5) (Simons, 1996)
Adults: 9-16 hours (pH 8); 3-6 hours (pH 5) (Chua, 1989)
Use: Labeled Indications
Nasal congestion: Temporary symptomatic relief of nasal congestion due to common cold, hay fever, or upper respiratory allergies; temporary relief of sinus congestion and pressure; promotes nasal or sinus drainage; temporarily restores freer breathing through the nose
Contraindications
Concurrent administration with or within 2 weeks of discontinuing an MAO inhibitor
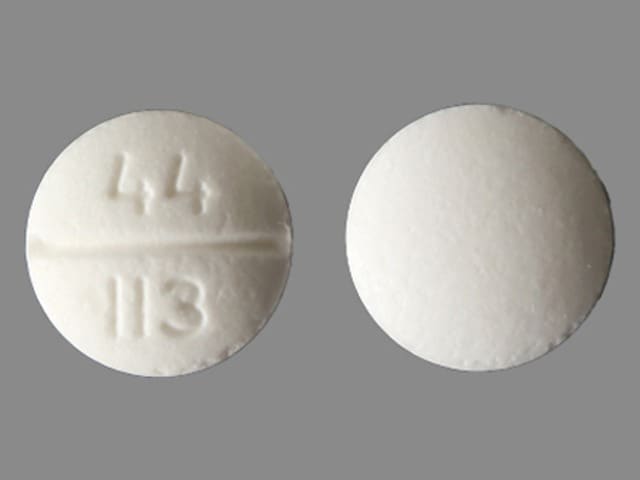
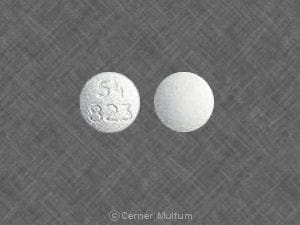
Pseudoephedrine Images
Dosage and Administration
Dosing: Adult
Nasal congestion: General dosing guidelines: Oral: Immediate release: 60 mg every 4 to 6 hours; Extended release: 120 mg every 12 hours or 240 mg every 24 hours; maximum: 240 mg per 24 hours
Dosing: Geriatric
Nasal congestion: Use caution in this population; initiate using immediate release formulation: 30 to 60 mg every 6 hours as needed
Dosing: Pediatric
Note: Safety and efficacy for the use of cough and cold products in infants and young children is limited; the AAP warns against the use of these products for respiratory illnesses in infants and young children; the FDA does not recommend OTC use in infants and children <2 years of age due to the risk of serious and life-threatening adverse effects (including death) and recommends to use with caution in pediatric patients ≥2 years of age (AAP 2018; FDA 2017).
Nasal congestion (decongestant): Oral:
Children <4 years: Limited data available: Immediate release: 1 mg/kg/dose every 6 hours; maximum dose: 15 mg/dose (Gentile 2000)
Children 4 to <6 years: Immediate release:
Fixed dose: 15 mg every 4 to 6 hours; maximum daily dose: 60 mg/24 hours
Weight-directed dosing: 1 mg/kg/dose every 6 hours; maximum dose: 15 mg/dose (Gentile 2000)
Children 6 to <12 years: Immediate release: 30 mg every 4 to 6 hours; maximum daily dose: 120 mg/24 hours
Children ≥12 years and Adolescents:
Immediate release: 60 mg every 4 to 6 hours; maximum daily dose: 240 mg/day
Extended release: 120 mg every 12 hours or 240 mg once daily; maximum daily dose: 240 mg/24 hours
Administration
Do not crush extended release drug product, swallow whole. May administer with or without food. Sudafed 24 Hour tablet may not completely dissolve and appear in stool
Dietary Considerations
Some products may contain sodium.
Drug Interactions
Alkalinizing Agents: May increase the serum concentration of Alpha-/Beta-Agonists (Indirect-Acting). Monitor therapy
Alpha1-Blockers: May diminish the vasoconstricting effect of Alpha-/Beta-Agonists. Similarly, Alpha-/Beta-Agonists may antagonize Alpha1-Blocker vasodilation. Monitor therapy
AtoMOXetine: May enhance the hypertensive effect of Sympathomimetics. AtoMOXetine may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
Benzylpenicilloyl Polylysine: Alpha-/Beta-Agonists may diminish the diagnostic effect of Benzylpenicilloyl Polylysine. Management: Consider use of a histamine skin test as a positive control to assess a patient's ability to mount a wheal and flare response. Consider therapy modification
Cannabinoid-Containing Products: May enhance the tachycardic effect of Sympathomimetics. Exceptions: Cannabidiol. Monitor therapy
Carbonic Anhydrase Inhibitors: May increase the serum concentration of Alpha-/Beta-Agonists (Indirect-Acting). Monitor therapy
Chloroprocaine: May enhance the hypertensive effect of Alpha-/Beta-Agonists. Monitor therapy
Cocaine (Topical): May enhance the hypertensive effect of Sympathomimetics. Management: Consider alternatives to use of this combination when possible. Monitor closely for substantially increased blood pressure or heart rate and for any evidence of myocardial ischemia with concurrent use. Consider therapy modification
Doxofylline: Sympathomimetics may enhance the adverse/toxic effect of Doxofylline. Monitor therapy
Ergot Derivatives: May enhance the hypertensive effect of Alpha-/Beta-Agonists. Ergot Derivatives may enhance the vasoconstricting effect of Alpha-/Beta-Agonists. Exceptions: Ergoloid Mesylates; Nicergoline. Avoid combination
FentaNYL: Alpha-/Beta-Agonists (Indirect-Acting) may decrease the serum concentration of FentaNYL. Specifically, fentanyl nasal spray serum concentrations may decrease and onset of effect may be delayed. Monitor therapy
Guanethidine: May enhance the arrhythmogenic effect of Sympathomimetics. Guanethidine may enhance the hypertensive effect of Sympathomimetics. Monitor therapy
Iobenguane Radiopharmaceutical Products: Alpha-/Beta-Agonists (Indirect-Acting) may diminish the therapeutic effect of Iobenguane Radiopharmaceutical Products. Management: Discontinue all drugs that may inhibit or interfere with catecholamine transport or uptake for at least 5 biological half-lives before iobenguane administration. Do not administer these drugs until at least 7 days after each iobenguane dose. Avoid combination
Linezolid: May enhance the hypertensive effect of Sympathomimetics. Management: Reduce initial doses of sympathomimetic agents, and closely monitor for enhanced pressor response, in patients receiving linezolid. Specific dose adjustment recommendations are not presently available. Consider therapy modification
Monoamine Oxidase Inhibitors: May enhance the hypertensive effect of Alpha-/Beta-Agonists (Indirect-Acting). While linezolid is expected to interact via this mechanism, management recommendations differ from other monoamine oxidase inhibitors. Refer to linezolid specific monographs for details. Exceptions: Linezolid. Avoid combination
Serotonin/Norepinephrine Reuptake Inhibitors: May enhance the tachycardic effect of Alpha-/Beta-Agonists. Serotonin/Norepinephrine Reuptake Inhibitors may enhance the vasopressor effect of Alpha-/Beta-Agonists. Consider therapy modification
Solriamfetol: Sympathomimetics may enhance the hypertensive effect of Solriamfetol. Monitor therapy
Spironolactone: May diminish the vasoconstricting effect of Alpha-/Beta-Agonists. Monitor therapy
Sympathomimetics: May enhance the adverse/toxic effect of other Sympathomimetics. Monitor therapy
Tedizolid: May enhance the hypertensive effect of Sympathomimetics. Tedizolid may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
Tricyclic Antidepressants: May enhance the vasopressor effect of Alpha-/Beta-Agonists. Management: Avoid, if possible, the use of alpha-/beta-agonists in patients receiving tricyclic antidepressants. If combined, monitor for evidence of increased pressor effects and consider reductions in initial dosages of the alpha-/beta-agonist. Consider therapy modification
Urinary Acidifying Agents: May decrease the serum concentration of Alpha-/Beta-Agonists (Indirect-Acting). Monitor therapy
Test Interactions
Interferes with urine detection of amphetamine (false-positive)
Adverse Reactions
Frequency not defined.
Cardiovascular: Cardiac arrhythmia, chest tightness, circulatory shock (with hypotension), hypertension, palpitations, tachycardia
Central nervous system: Ataxia, central nervous system stimulation (transient), chills, confusion, dizziness, drowsiness, excitability, fatigue, hallucination, headache, insomnia, nervousness, neuritis, restlessness, seizure, vertigo
Dermatologic: Diaphoresis, skin photosensitivity, skin rash, urticaria
Gastrointestinal: Anorexia, constipation, diarrhea, dry throat, ischemic colitis, nausea, vomiting, xerostomia
Genitourinary: Difficulty in micturition, dysuria, urinary retention
Hematologic & oncologic: Agranulocytosis, hemolytic anemia, thrombocytopenia
Hypersensitivity: Anaphylaxis
Neuromuscular & skeletal: Tremor, weakness
Ophthalmic: Blurred vision, diplopia
Otic: Tinnitus
Renal: Polyuria
Respiratory: Dry nose, dyspnea, nasal congestion, pharyngeal edema, thickening of bronchial secretions, wheezing
Warnings/Precautions
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with cardiovascular disease (including hypertension and ischemic heart disease).
- Diabetes: Use with caution in patients with diabetes mellitus.
- Increased intraocular pressure/glaucoma: Use with caution in patients with increased intraocular pressure or angle-closure glaucoma.
- Prostatic hyperplasia/urinary obstruction: Use with caution in patients with prostatic hyperplasia and/or GU obstruction.
- Renal impairment: Use caution in patient with renal impairment; consider dosage adjustments.
- Seizure disorder: Use with caution in patients with seizure disorder; may produce CNS stimulation.
- Thyroid dysfunction: Use with caution in patients with thyroid dysfunction.
Special populations:
- Elderly: Use with caution in the elderly; may be more sensitive to adverse effects.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC, 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors, 2001); avoid or use dosage forms containing benzyl alcohol derivative with caution in neonates. See manufacturer’s labeling.
- Sodium: Some products may contain sodium.
Other warnings/precautions:
- Self-medication (OTC use): When used for self-medication (OTC), notify healthcare provider if symptoms do not improve within 7 days or are accompanied by fever. Discontinue and contact healthcare provider if nervousness, dizziness, or sleeplessness occur. Not for OTC use in children <4 years of age.
Pregnancy
Pregnancy Considerations
Use of pseudoephedrine during the first trimester may be associated with a possible risk of gastroschisis, small intestinal atresia, and hemifacial microsomia due to pseudoephedrine's vasoconstrictive effects; additional studies are needed to define the magnitude of risk. Single doses of pseudoephedrine were not found to adversely affect the fetus during the third trimester of pregnancy (limited data); however, fetal tachycardia was noted in a case report following maternal use of an extended release product for multiple days. Decongestants are not the preferred agents for the treatment of rhinitis during pregnancy. Oral pseudoephedrine should be avoided during the first trimester.
Patient Education
What is this drug used for?
- It is used to treat nose stuffiness.
Frequently reported side effects of this drug
- Trouble sleeping
- Tablet shell in stool
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Chest pain
- Fast heartbeat
- Severe anxiety
- Severe headache
- Severe dizziness
- Passing out
- Severe abdominal pain
- Severe vomiting
- Severe nausea
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.