Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Capsule Sprinkle, Oral, as sodium:
AcipHex Sprinkle: 5 mg [contains fd&c blue #2 aluminum lake]
AcipHex Sprinkle: 10 mg [contains fd&c yellow #6 (sunset yellow)]
Generic: 10 mg
Tablet Delayed Release, Oral, as sodium:
Aciphex: 20 mg
Generic: 20 mg
Pharmacology
Mechanism of Action
Potent proton pump inhibitor; suppresses gastric acid secretion by inhibiting the parietal cell H+/K+ ATP pump
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Well absorbed within 1 hour; food delayed absorption up to 4 hours or longer
Metabolism
Hepatic via CYP3A and 2C19 to inactive metabolites; CYP2C19 exhibits a known genetic polymorphism due to its deficiency in some subpopulations (3% to 5% of Caucasians and 17% to 20% of Asians) which results in slower metabolism
Excretion
Urine (90% primarily as thioether carboxylic acid metabolites); remainder in feces
Onset of Action
Within 1 hour
Time to Peak
Plasma:
Children ≤11 years: Sprinkle capsule: 2 to 4 hours
Children ≥12 years and Adolescents: 20 mg tablet: 4.1 ± 0.45 hours (James 2007)
Adults: Tablet: 2 to 5 hours; Sprinkle capsule: 1 to 6.5 hours
Duration of Action
24 hours
Half-Life Elimination
Dose dependent:
Children ≤11 years: 2.5 hours
Children ≥12 years and Adolescents: 20 mg tablet: 0.97 ± 0.19 hours (James 2007)
Adults: 1 to 2 hours
Protein Binding
96.3%
Use in Specific Populations
Special Populations: Hepatic Function Impairment
In mild to moderate hepatic impairment, AUC approximately doubled, total clearance decreased to less than half, and Cmax increased ~20% (not statistically significant) and elimination half-life was 2- to 3-fold higher.
Special Populations: Elderly
AUC values approximately doubled; Cmax increased 60%.
Special Populations: Race
AUCs for Japanese men were 50% to 60% higher.
Use: Labeled Indications
Duodenal ulcers (tablets only): Short-term (4 weeks or fewer) treatment in the healing and symptomatic relief of duodenal ulcers in adults.
Gastroesophageal reflux disease:
Erosive or ulcerative (tablets only): Short-term (4 to 8 weeks) treatment in the healing and symptomatic relief of erosive or ulcerative gastroesophageal reflux disease (GERD) in adults; for maintaining healing and reduction in relapse rates of heartburn symptoms in adults with erosive or ulcerative GERD.
Symptomatic (nonerosive): Treatment of symptomatic GERD for up to 4 weeks in adults (tablets only), up to 8 weeks in children ≥12 years and adolescents (tablets only), and up to 12 weeks in children 1 to 11 years of age (capsules only).
Helicobacter pylori eradication (tablets only): In combination with amoxicillin and clarithromycin as a 3-drug regimen for the treatment of adults with H. pylori infection and duodenal ulcer disease (active or history of within the past 5 years) to eradicate H. pylori.
Pathological hypersecretory conditions (tablets only): Long-term treatment of pathological hypersecretory conditions, including Zollinger-Ellison syndrome in adults.
Use: Off Label
Dyspepsiabyes
Data from a phase 2, multicenter, double-blinded, placebo-controlled trial as well as from a prospective multicenter study supports the use of rabeprazole for the treatment of dyspepsia Dewan 2011, Iwakiri 2013. In addition, data from a systematic review support the use of rabeprazole for treatment of patients with ulcer and reflux-like functional dyspepsia Pinto-Sanchez 2017.
Based on the American College of Gastroenterology (ACG) and Canadian Association of Gastroenterology (CAG) guidelines for the management of dyspepsia, the use of rabeprazole is effective and recommended treatment for dyspepsia and functional dyspepsia in patients <60 years of age who are H. pylori negative or remain symptomatic after H. pylori eradication therapy Moayyedi 2017.
Gastric ulcer (treatment)b
Data from a randomized, placebo-controlled, double-blind study and a randomized, double-blind, active-comparator study support the use of rabeprazole in the treatment of active gastric ulcers Cloud 1998, Dekkers 1998.
NSAID-induced ulcer prophylaxisbyes
According to the American College of Gastroenterology 2009 Guidelines for Prevention of NSAID-Related Ulcer Complications, proton pump inhibitors are effective and recommended in the prophylaxis of gastric and duodenal ulcers in patients receiving NSAID therapy Lanza 2009.
Data from randomized, double-blind, active-controlled trials support the use of rabeprazole in the prevention of NSAID-induced peptic ulcers Iwakiri 2014, Sanuki 2012.
Prevention of recurrent gastric or duodenal ulcer bleeding postendoscopyb
Data from a small prospective, randomized, controlled trial support the use of high-dose rabeprazole to decrease the risk of rebleeding postendoscopy for acute bleeding peptic ulcers Kim 2012. Additional trials may be necessary to further define the role of rabeprazole in this setting.
Stress ulcer prophylaxis in critically-ill patientsyes
Based on the Surviving Sepsis Campaign International Guidelines for the Management of Severe Sepsis and Septic Shock, stress ulcer prophylaxis using a proton pump inhibitor or a histamine H2-receptor antagonist is recommended in sepsis or septic shock patients who have GI bleeding risk factors.
Contraindications
Hypersensitivity (eg, anaphylaxis, anaphylactic shock, angioedema, bronchospasm, acute interstitial nephritis, urticaria) to rabeprazole, other substituted benzimidazoles, or any component of the formulation; concomitant use with rilpivirine-containing products
Dosage and Administration
Dosing: Adult
Duodenal ulcer: Tablets: Oral: 20 mg once daily for ≤4 weeks; additional therapy to achieve healing may be required for some patients.
Dyspepsia (off-label use): Oral: 20 mg once daily for up to 8 weeks (Dewan 2011, Iwakiri 2013; Pinto-Sanchez 2017)
Gastric ulcer (treatment) (off-label use): Oral: 20 mg once daily (Cloud 1998; Dekkers 1998) for generally 8 weeks based on healing and/or ulcer complications (Boparai 2008; Wolfe 2000).
Gastroesophageal reflux disease (GERD): Tablets: Oral:
Erosive or ulcerative GERD: Treatment: 20 mg once daily for 4 to 8 weeks; if inadequate response, may repeat up to an additional 8 weeks; maintenance: 20 mg once daily
Symptomatic GERD (nonerosive): Treatment: 20 mg once daily for ≤4 weeks; if inadequate response, may repeat for an additional 4 weeks.
Helicobacter pylori eradication: Tablets: Oral:
Manufacturer labeling: 20 mg twice daily administered with amoxicillin 1,000 mg and clarithromycin 500 mg twice daily for 7 days
American College of Gastroenterology guidelines (ACG [Chey 2007; Chey 2017]):
Clarithromycin triple regimen: 20 to 40 mg twice daily in combination with clarithromycin 500 mg twice daily and either amoxicillin 1 g twice daily or metronidazole 500 mg 3 times per day; continue regimen for 14 days. Note: Avoid use of clarithromycin triple therapy in patients with risk factors for macrolide resistance (eg, prior macrolide exposure, local clarithromycin resistance rates ≥15%, eradication rates with clarithromycin-based regimens ≤85%) (ACG [Chey 2017]; Fallone 2016).
Bismuth quadruple regimen: 20 mg twice daily in combination with tetracycline 500 mg 4 times per day, metronidazole 250 mg 4 times per day or 500 mg 3 or 4 times per day, and either bismuth subcitrate 120 to 300 mg 4 times per day or bismuth subsalicylate 300 mg 4 times per day; continue regimen for 10 to 14 days.
Concomitant regimen: 20 mg twice daily in combination with amoxicillin 1 g twice daily, clarithromycin 500 mg twice daily, and either metronidazole or tinidazole 500 mg twice daily; continue regimen for 10 to 14 days.
Sequential regimen: 20 mg twice daily plus amoxicillin 1 g twice daily for 5 to 7 days; then continue rabeprazole along with clarithromycin 500 mg twice daily, and either metronidazole or tinidazole 500 mg twice daily for 5 to 7 days.
Hybrid regimen: 20 mg twice daily plus amoxicillin 1 g twice daily for 7 days; then continue rabeprazole and amoxicillin along with clarithromycin 500 mg twice daily, and either metronidazole or tinidazole 500 mg twice daily for 7 days.
Levofloxacin triple regimen: 20 mg twice daily in combination with amoxicillin 1 g twice daily and levofloxacin 500 mg once daily; continue regimen for 10 to 14 days
Hypersecretory conditions (including Zollinger-Ellison Syndrome): Tablets: Oral: Initial: 60 mg once daily; adjust dose to patient needs (some may require divided doses). Doses as high as 100 mg once daily and 60 mg twice daily have been used; continue as long as clinically indicated.
NSAID-induced ulcer prophylaxis (off-label use): Oral: 5 to 20 mg once daily for 12 to 24 weeks (Iwakiri 2014; Sanuki 2012)
Prevention of recurrent gastric or duodenal ulcer bleeding postendoscopy (off-label use): Oral: 20 mg twice daily for 72 hours (Kim 2012)
Discontinuation of therapy: Oral: Some experts recommend a step-down approach in order to avoid worsening or rebound symptoms. One recommendation is to decrease the dose by 50% over 2 weeks to 4 weeks. If the patient is already on the lowest possible dose, alternate day therapy may be considered. If symptoms worsen during treatment or after discontinuation, patient should be re-evaluated (Kim 2018).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
GERD, symptomatic: Note: Guidelines recommend a 4- to 8-week treatment course; if improvement seen after 4 to 8 weeks, consider possible wean; if no response after 4 to 8 weeks, reevaluate diagnosis and consider referral to pediatric GI specialist (NASPGHAN/ESPGHAN [Rosen 2018]).
Infants: Limited data available: Oral: Sprinkle capsules: 5 to 10 mg once daily; dosing based on a double-blind, placebo-controlled trial which randomized patients aged 1 to 11 months (n=268) with symptomatic GERD to 10 mg, 5 mg, or placebo (n=88, n=90, n=90, respectively); the study found no difference in the degree of improvement with rabeprazole (at any dose) compared to those receiving placebo (Hussain 2014).
Children ≤11 years: Oral: Sprinkle capsules:
<15 kg: 5 mg once daily; if inadequate response may increase to 10 mg once daily.
≥15 kg: 10 mg once daily; higher doses of 20 mg/day have also been described (Haddad 2014).
Children ≥12 years and Adolescents: Oral: Tablets: 20 mg once daily.
Helicobacter pylori eradication: Limited data available: Note: Usual duration of therapy is 14 days as part of triple therapy; use in combination with 2 antimicrobials (eg, clarithromycin, metronidazole, amoxicillin); preferred agents determined by susceptibility. Bismuth may be added to regimens as an alternative if resistance is present or susceptibility is unknown (NASPGHAN/ESPGHAN [Jones 2017]).
Children and Adolescents <16 years: Note: Dosing based on a pharmacokinetic modeling study to determine a dose that achieved AUC comparable to adults receiving 20 mg twice daily (Kimko 2015).
6 to <10 kg: Oral: 10 mg twice daily.
10 to <30 kg: Oral: 15 mg twice daily.
≥30 kg: Oral: 20 mg twice daily.
Discontinuation of therapy: Oral: Based on experience in adults, some experts recommend a step-down approach in order to avoid worsening or rebound symptoms. One recommendation is to decrease the dose by 50% over 2 to 4 weeks. If the patient is already on the lowest possible dose, alternate day therapy may be considered. If symptoms worsen during treatment or after discontinuation, patient should be reevaluated (Kim 2018).
Administration
May be administered with an antacid.
Capsules: Administer 30 minutes before a meal. Open capsule and sprinkle entire contents on a small amount of soft food (eg, applesauce, fruit or vegetable based baby food, yogurt) or empty contents into a small amount of liquid (eg, infant formula, apple juice, pediatric electrolyte solution); food or liquid should be at or below room temperature. Do not swallow capsule whole, or chew or crush granules; administer whole dose within 15 minutes of preparation (do not store for future use).
Tablets: Swallow whole; do not crush, split, or chew; may administer with or without food. However, when used for the treatment of duodenal ulcers, administer after a meal; when used for the eradication of H. pylori, administer with the morning and evening meals.
Dietary Considerations
Capsules: Take 30 minutes before a meal.
Tablets: When used for the treatment of duodenal ulcers, administer after a meal; when used for the eradication of Helicobacter pylori, administer with the morning and evening meals.
Storage
Store at 25°C (77°F); excursions are permitted between 15°C and 30°C (59°F and 86°F). Protect from moisture.
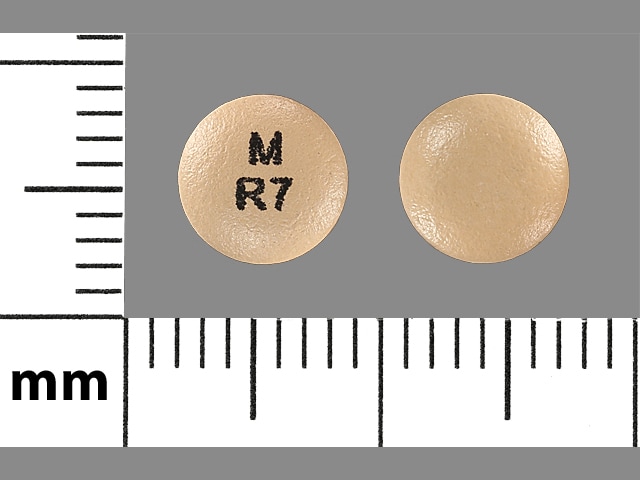
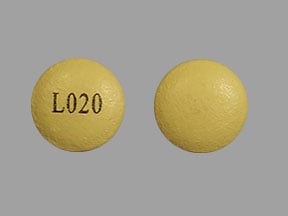
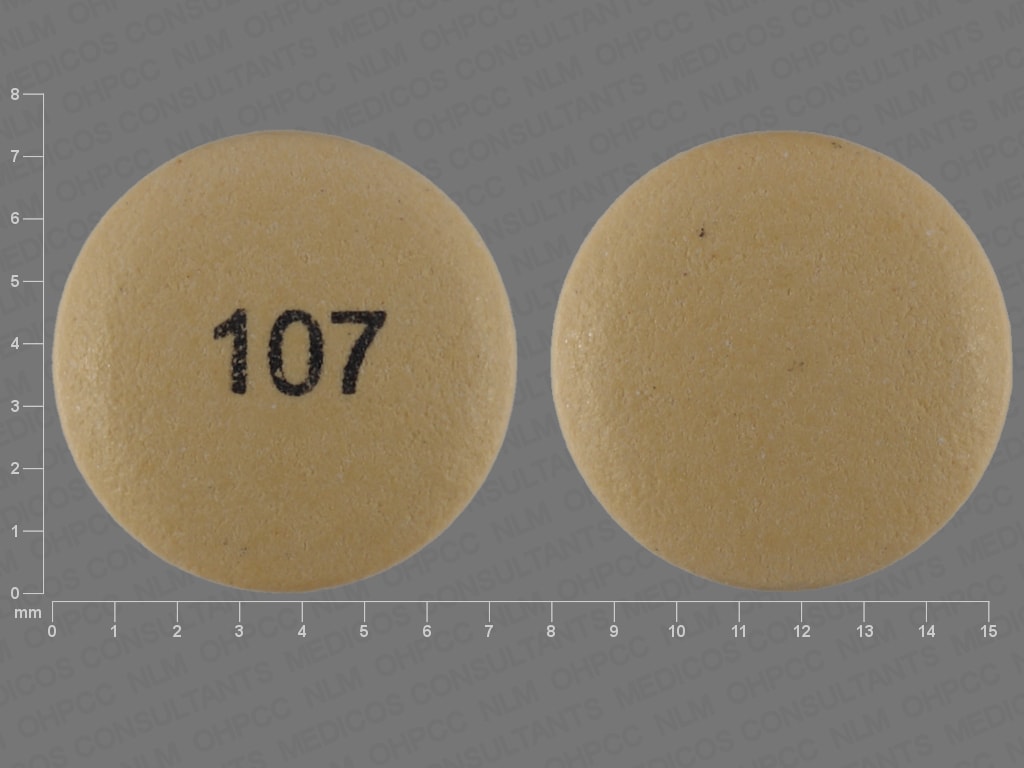
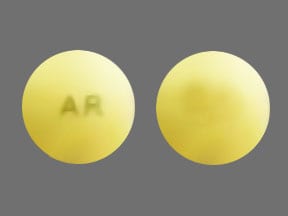
RABEprazole Images
Drug Interactions
Acalabrutinib: Proton Pump Inhibitors may decrease the serum concentration of Acalabrutinib. Avoid combination
Amphetamine: Proton Pump Inhibitors may increase the absorption of Amphetamine. Monitor therapy
Atazanavir: Proton Pump Inhibitors may decrease the serum concentration of Atazanavir. Management: See full drug interaction monograph for details. Consider therapy modification
Bisphosphonate Derivatives: Proton Pump Inhibitors may diminish the therapeutic effect of Bisphosphonate Derivatives. Monitor therapy
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Bosutinib: Proton Pump Inhibitors may decrease the serum concentration of Bosutinib. Management: Consider alternatives to proton pump inhibitors, such as short-acting antacids or histamine-2 receptor antagonists. Administer alternative agents more than 2 hours before or after bosutinib. Consider therapy modification
Capecitabine: Proton Pump Inhibitors may diminish the therapeutic effect of Capecitabine. Monitor therapy
Cefditoren: Proton Pump Inhibitors may decrease the serum concentration of Cefditoren. Management: If possible, avoid use of cefditoren with proton pump inhibitors (PPIs). Consider alternative methods to minimize/control acid reflux (eg, diet modification) or alternative antimicrobial therapy if use of PPIs can not be avoided. Consider therapy modification
Cefpodoxime: Proton Pump Inhibitors may decrease the serum concentration of Cefpodoxime. Monitor therapy
Cefuroxime: Proton Pump Inhibitors may decrease the absorption of Cefuroxime. Avoid combination
CYP2C19 Inducers (Moderate): May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Monitor therapy
CYP2C19 Inducers (Strong): May increase the metabolism of CYP2C19 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
Cysteamine (Systemic): Proton Pump Inhibitors may diminish the therapeutic effect of Cysteamine (Systemic). Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP2C19 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dacomitinib: Proton Pump Inhibitors may decrease the serum concentration of Dacomitinib. Management: Avoid concurrent use of dacomitinib with proton pump inhibitors. Antacids may be used. Histamine H2-receptor antagonists (HR2A) may be used if dacomitinib is given at least 6 hours before or 10 hours after the H2RA. Avoid combination
Dasatinib: Proton Pump Inhibitors may decrease the serum concentration of Dasatinib. Management: Antacids (taken 2 hours before or after dasatinib administration) can be used in place of the proton pump inhibitor if some acid-reducing therapy is needed. Avoid combination
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Delavirdine: Proton Pump Inhibitors may decrease the serum concentration of Delavirdine. Management: Chronic therapy with proton pump inhibitors (PPIs) should be avoided in patients treated with delavirdine. The clinical significance of short-term PPI therapy with delavirdine is uncertain, but such therapy should be undertaken with caution. Avoid combination
Dexmethylphenidate: Proton Pump Inhibitors may increase the absorption of Dexmethylphenidate. Specifically, proton pump inhibitors may interfere with the normal release of drug from the extended-release capsules (Focalin XR brand), which could result in both increased absorption (early) and decreased delayed absorption. Monitor therapy
Dextroamphetamine: Proton Pump Inhibitors may increase the absorption of Dextroamphetamine. Specifically, the dextroamphetamine absorption rate from mixed amphetamine salt extended release (XR) capsules may be increased in the first hours after dosing. Monitor therapy
Dichlorphenamide: OAT1/3 Inhibitors may increase the serum concentration of Dichlorphenamide. Monitor therapy
Doxycycline: Proton Pump Inhibitors may decrease the bioavailability of Doxycycline. Monitor therapy
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Enzalutamide: May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Conversely, concentrations of active metabolites may be increased for those drugs activated by CYP2C19. Management: Concurrent use of enzalutamide with CYP2C19 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP2C19 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erlotinib: Proton Pump Inhibitors may decrease the serum concentration of Erlotinib. Avoid combination
Fluconazole: May increase the serum concentration of Proton Pump Inhibitors. Monitor therapy
Gefitinib: Proton Pump Inhibitors may decrease the serum concentration of Gefitinib. Management: Avoid use of proton pump inhibitors (PPIs) with gefitinib when possible. If required, administer gefitinib 12 hours after administration of the PPI or 12 hours before the next dose of the PPI. Consider therapy modification
Indinavir: Proton Pump Inhibitors may decrease the serum concentration of Indinavir. Monitor therapy
Iron Preparations: Proton Pump Inhibitors may decrease the absorption of Iron Preparations. Exceptions: Ferric Carboxymaltose; Ferric Citrate; Ferric Derisomaltose; Ferric Gluconate; Ferric Hydroxide Polymaltose Complex; Ferric Pyrophosphate Citrate; Ferumoxytol; Iron Dextran Complex; Iron Sucrose. Monitor therapy
Itraconazole: Proton Pump Inhibitors may increase the serum concentration of Itraconazole. Proton Pump Inhibitors may decrease the serum concentration of Itraconazole. Management: Exposure to Tolsura brand itraconazole may be increased by PPIs; consider itraconazole dose reduction. Exposure to Sporanox brand itraconazole capsules may be decreased by PPIs. Give Sporanox brand itraconazole at least 2 hrs before or 2 hrs after PPIs Consider therapy modification
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Ketoconazole (Systemic): Proton Pump Inhibitors may decrease the absorption of Ketoconazole (Systemic). Ketoconazole (Systemic) may increase the serum concentration of Proton Pump Inhibitors. Management: Administer ketoconazole with an acidic beverage, such as non-diet cola, to increase gastric acidity and improve absorption if concomitant use with proton pump inhibitors is necessary. Consider therapy modification
Ledipasvir: Proton Pump Inhibitors may decrease the serum concentration of Ledipasvir. Management: PPI doses equivalent to omeprazole 20 mg or lower may be given with ledipasvir under fasted conditions. Administration with higher doses of PPIs, 2 hours after a PPI, or in combination with food and PPIs may reduce ledipasvir bioavailability. Consider therapy modification
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Mesalamine: Proton Pump Inhibitors may diminish the therapeutic effect of Mesalamine. Proton pump inhibitor-mediated increases in gastrointestinal pH may cause the premature release of mesalamine from specific sustained-release mesalamine products. Management: Consider avoiding concurrent administration of high-dose proton pump inhibitors (PPIs) with sustained-release mesalamine products. Consider therapy modification
Methotrexate: Proton Pump Inhibitors may increase the serum concentration of Methotrexate. Monitor therapy
Methylphenidate: Proton Pump Inhibitors may increase the absorption of Methylphenidate. Specifically, proton pump inhibitors may interfere with the normal release of drug from the extended-release capsules (Ritalin LA brand), which could result in both increased absorption (early) and decreased delayed absorption. Monitor therapy
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Multivitamins/Minerals (with ADEK, Folate, Iron): Proton Pump Inhibitors may decrease the serum concentration of Multivitamins/Minerals (with ADEK, Folate, Iron). Specifically, the absorption of iron may be decreased. Monitor therapy
Mycophenolate: Proton Pump Inhibitors may decrease the serum concentration of Mycophenolate. Specifically, concentrations of the active mycophenolic acid may be reduced. Monitor therapy
Nelfinavir: Proton Pump Inhibitors may decrease serum concentrations of the active metabolite(s) of Nelfinavir. Proton Pump Inhibitors may decrease the serum concentration of Nelfinavir. Avoid combination
Neratinib: Proton Pump Inhibitors may decrease the serum concentration of Neratinib. Specifically, proton pump inhibitors may reduce neratinib absorption. Avoid combination
Nilotinib: Proton Pump Inhibitors may decrease the serum concentration of Nilotinib. Management: Avoid this combination when possible since separation of doses is not likely to be an adequate method of minimizing the interaction. Consider therapy modification
PAZOPanib: Proton Pump Inhibitors may decrease the serum concentration of PAZOPanib. Avoid combination
Pexidartinib: Proton Pump Inhibitors may decrease the serum concentration of Pexidartinib. Management: If acid-reduction is needed, consider administering an antacid 2 hours before or after pexidartinib, or administer pexidartinib 2 hours before or 10 hours after an H2 receptor antagonist. Avoid combination
Posaconazole: Proton Pump Inhibitors may decrease the serum concentration of Posaconazole. Consider therapy modification
Raltegravir: Proton Pump Inhibitors may increase the serum concentration of Raltegravir. Monitor therapy
Rilpivirine: Proton Pump Inhibitors may decrease the serum concentration of Rilpivirine. Avoid combination
Riociguat: Proton Pump Inhibitors may decrease the serum concentration of Riociguat. Monitor therapy
Risedronate: Proton Pump Inhibitors may diminish the therapeutic effect of Risedronate. Proton Pump Inhibitors may increase the serum concentration of Risedronate. This applies specifically to use of delayed-release risedronate. Consider therapy modification
Saquinavir: Proton Pump Inhibitors may increase the serum concentration of Saquinavir. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Secretin: Proton Pump Inhibitors may diminish the diagnostic effect of Secretin. Specifically, use of PPIs may cause a hyperresponse in gastrin secretion in response to secretin stimulation testing, falsely suggesting gastrinoma. Management: Avoid concomitant use of proton pump inhibitors (PPIs) and secretin, and discontinue PPIs several weeks prior to secretin administration, with the duration of separation determined by the specific PPI. See full monograph for details. Consider therapy modification
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
SORAfenib: Proton Pump Inhibitors may decrease the absorption of SORAfenib. Monitor therapy
Tacrolimus (Systemic): Proton Pump Inhibitors may increase the serum concentration of Tacrolimus (Systemic). Management: Tacrolimus dose adjustment may be required. Rabeprazole, pantoprazole, or selected H2-receptor antagonists (i.e., ranitidine or famotidine) may be less likely to interact. Genetic testing may predict patients at highest risk. Consider therapy modification
Tipranavir: May decrease the serum concentration of Proton Pump Inhibitors. These data are derived from studies with Ritonavir-boosted Tipranavir. Monitor therapy
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Velpatasvir: Proton Pump Inhibitors may decrease the serum concentration of Velpatasvir. Avoid combination
Voriconazole: May increase the serum concentration of Proton Pump Inhibitors. Proton Pump Inhibitors may increase the serum concentration of Voriconazole. Monitor therapy
Test Interactions
Chromogranin A: PPIs may falsely elevate serum chromogranin A (CgA) levels. The increased CgA level may cause false-positive results in the diagnosis of a neuroendocrine tumor. Temporarily stop rabeprazole ≥14 days prior to assessing CgA level; repeat level if initially elevated; use the same laboratory for all testing of CgA levels.
Secretin stimulation test: Hyper-response in gastrin secretion in adults in response to secretin stimulation test has been reported, falsely suggesting gastrinoma. Temporarily stop treatment at least 14 days before assessing to allow gastrin levels to return to baseline.
Tetrahydrocannabinol urine screening tests: False positive urine screening tests for tetrahydrocannabinol (THC) have been reported. Alternative confirmatory methods should be considered to verify positive results.
Adverse Reactions
>10%: Gastrointestinal: Diarrhea (children and adolescents: 5% to 21%; adults: <2%), abdominal pain (children: 16%; adolescents and adults: ≤4%), vomiting (children: 10% to 14%; adolescents: 4%)
1% to 10%:
Cardiovascular: Peripheral edema (adults: <2%)
Central nervous system: Headache (children and adolescents: 5% to 10% adults: <2%), pain (adults: 3%), dizziness (adults: <2%)
Gastrointestinal: Nausea (children and adolescents: 2% to 9%), flatulence (adults: 3%), constipation (adults: 2%), xerostomia (<2%)
Hepatic: Hepatic encephalopathy (adults: <2%), hepatitis (adults: <2%), increased liver enzymes (adults: <2%)
Infection: Infection (adults: 2%)
Neuromuscular & skeletal: Arthralgia (adults: <2%), myalgia (adults: <2%)
Respiratory: Pharyngitis (adults: 3%)
<1%, postmarketing, and/or case reports: Agranulocytosis, anaphylaxis, angioedema, blurred vision, bone fracture, bullous rash, Clostridioides (formerly Clostridium) difficile-associated diarrhea, coma, cutaneous lupus erythematous, delirium, disorientation, erythema multiforme, hemolytic anemia, hepatotoxicity (idiosyncratic) (Chalasani 2014), hyperammonemia, hypomagnesemia, increased thyroid stimulating hormone level, interstitial nephritis, jaundice, leukopenia, pancytopenia, pneumonia (interstitial), polyp (fundic gland), renal disease (chronic; Lazarus 2016), rhabdomyolysis, severe dermatological reaction, Stevens-Johnson syndrome, systemic lupus erythematosus, thrombocytopenia, toxic epidermal necrolysis, vertigo
Warnings/Precautions
Concerns related to adverse effects:
- Atrophic gastritis: Long-term omeprazole therapy has caused atrophic gastritis (by biopsy); this may also occur with rabeprazole.
- Carcinoma: No reports of adenomatoid, dysplastic or neoplastic changes of enterochromaffin-like (ECL) cells in the gastric mucosa have occurred.
- Clostridioides (formerly Clostridium) difficile-associated diarrhea (CDAD): Use of proton pump inhibitors (PPIs) may increase risk of CDAD, especially in hospitalized patients; consider CDAD diagnosis in patients with persistent diarrhea that does not improve. Use the lowest dose and shortest duration of PPI therapy appropriate for the condition being treated.
- Cutaneous and systemic lupus erythematosus: Has been reported as new onset or exacerbation of existing autoimmune disease; most cases were cutaneous lupus erythematosus (CLE), most commonly, subacute CLE (occurring within weeks to years after continuous therapy). Systemic lupus erythematosus (SLE) is less common (typically occurs within days to years after initiating treatment) and occurred primarily in young adults up to the elderly. Discontinue therapy if signs or symptoms of CLE or SLE occur and refer to specialist for evaluation; most patients improve 4 to 12 weeks after discontinuation of rabeprazole.
- Fractures: Increased incidence of osteoporosis-related bone fractures of the hip, spine, or wrist may occur with proton pump inhibitor (PPI) therapy. Patients on high-dose (multiple daily doses) or long-term therapy (≥1 year) should be monitored. Use the lowest effective dose for the shortest duration of time, use vitamin D and calcium supplementation, and follow appropriate guidelines to reduce risk of fractures in patients at risk.
- Fundic gland polyps: Use of PPIs increases risk of fundic gland polyps, especially with long term use (>1 year). May occur without symptoms but nausea, vomiting, or abdominal pain may occur; gastrointestinal bleeding and/or anemia may occur with ulcerated polyps. Diagnosis of polyps may also increase risk for small intestinal blockage. Use the lowest dose and shortest duration of PPI therapy appropriate for the condition being treated.
- Gastrointestinal infection (eg, Salmonella, Campylobacter): Use of proton pump inhibitors may increase risk of these infections.
- Hypomagnesemia: Reported rarely, usually with prolonged PPI use of ≥3 months (most cases >1 year of therapy). May be symptomatic or asymptomatic; severe cases may cause tetany, seizures, and cardiac arrhythmias. Consider obtaining serum magnesium concentrations prior to beginning long-term therapy, especially if taking concomitant digoxin, diuretics, or other drugs known to cause hypomagnesemia; and periodically thereafter. Hypomagnesemia may be corrected by magnesium supplementation, although discontinuation of rabeprazole may be necessary; magnesium levels typically return to normal within 1 week of stopping.
- Interstitial nephritis: Acute interstitial nephritis has been observed in patients taking PPIs; may occur at any time during therapy and is generally due to an idiopathic hypersensitivity reaction. Discontinue if acute interstitial nephritis develops.
- Vitamin B12 deficiency: Prolonged treatment (>3 years) may lead to vitamin B12 malabsorption and subsequent vitamin B12 deficiency. The magnitude of the deficiency is dose-related and the association is stronger in females and those younger in age (<30 years of age); prevalence is decreased after discontinuation of therapy (Lam 2013).
Disease-related concerns:
- Gastric malignancy: Relief of symptoms does not preclude the presence of a gastric malignancy.
- Hepatic impairment: Avoid use in patients with severe hepatic impairment; if treatment is necessary monitor for adverse reactions.
Concurrent drug therapy issues:
- Clopidogrel: PPIs may diminish the therapeutic effect of clopidogrel, thought to be due to reduced formation of the active metabolite of clopidogrel. The manufacturer of clopidogrel recommends either avoidance of both omeprazole (even when scheduled 12 hours apart) and esomeprazole or use of a PPI with comparatively less effect on the active metabolite of clopidogrel. Avoidance of rabeprazole appears prudent due to potent in vitro CYP2C19 inhibition (Li 2004) and lack of sufficient comparative in vivo studies with other PPIs. In contrast to these warnings, others have recommended the continued use of PPIs, regardless of the degree of inhibition, in patients with a history of GI bleeding or multiple risk factors for GI bleeding who are also receiving clopidogrel since no evidence has established clinically meaningful differences in outcome; however, a clinically-significant interaction cannot be excluded in those who are poor metabolizers of clopidogrel (Abraham 2010; Levine 2011).
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Appropriate use: Helicobacter pylori eradication: Short-term combination therapy (≤7 days) has been associated with a higher incidence of treatment failure. The American College of Gastroenterology recommends 10 to 14 days of therapy (triple or quadruple) for eradication of H. pylori (Chey 2017).
Monitoring Parameters
Magnesium levels (prior to initiation of therapy and periodically thereafter) in patients on long-term treatment or those taking digoxin, diuretics, or other drugs that cause hypomagnesemia; susceptibility testing recommended in patients who fail H. pylori eradication regimen.
Pregnancy
Pregnancy Considerations
Recommendations for the treatment of GERD in pregnancy are available. As in nonpregnant patients, lifestyle modifications followed by other medications are the initial treatments (Body 2016; Huerta-Iga 2016; Katz 2013; van der Woude 2014). Based on available data, PPIs may be used when clinically indicated (use of agents with more data in pregnancy may be preferred) (Body 2016; Matok 2012; Pasternak 2010; van der Woude 2014).
Patient Education
What is this drug used for?
- It is used to treat gastroesophageal reflux disease (GERD; acid reflux).
- It is used to treat heartburn.
- It is used to treat or prevent GI (gastrointestinal) ulcers caused by infection.
- It is used to treat or prevent ulcers of the swallowing tube (esophagus).
- It is used to treat syndromes caused by lots of stomach acid.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Headache
- Abdominal pain
- Nausea
- Vomiting
- Diarrhea
- Constipation
- Passing gas
- Sore throat
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Low magnesium like mood changes; muscle pain or weakness; muscle cramps or spasms; seizures; tremors; lack of appetite; severe nausea or vomiting; or an abnormal heartbeat
- Kidney problems like not able to pass urine, blood in the urine, change in amount of urine passed, or weight gain
- Lupus like rash on the cheeks or other body parts, sunburn easy, muscle or joint pain, chest pain or shortness of breath, or swelling in the arms or legs
- Severe dizziness
- Passing out
- Bone pain
- Chills
- Excessive weight loss
- Severe loss of strength and energy
• Clostridioides (formerly Clostridium) difficile (C. diff)-associated diarrhea like abdominal pain or cramps, severe diarrhea or watery stools, or bloody stools
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.