Boxed Warning
Increased risk of VTE:
Increased risk of deep vein thrombosis and pulmonary embolism have been reported with raloxifene. Women with active or past history of VTE should not take raloxifene.
Cardiovascular disease:
Increased risk of death due to stroke occurred in a trial in postmenopausal women with documented coronary heart disease or increased risk for major coronary events. Consider the risk-benefit balance in women at risk for stroke.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral, as hydrochloride:
Evista: 60 mg [contains fd&c blue #2 aluminum lake]
Generic: 60 mg
Pharmacology
Mechanism of Action
Raloxifene is an estrogen agonist/antagonist (a selective estrogen receptor modulator [SERM]); selective binding activates estrogenic pathways in some tissues and antagonizes estrogenic pathways in other tissues. Raloxifene acts like an estrogen agonist in the bone to prevent bone loss and has estrogen antagonist activity to block some estrogen effects in the breast and uterine tissues. Raloxifene decreases bone resorption, increasing bone mineral density and decreasing fracture incidence.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid; ~60%
Distribution
2,348 L/kg
Metabolism
Hepatic, extensive first-pass metabolism; metabolized to glucuronide conjugates
Excretion
Feces (primarily); urine (<0.2% as unchanged drug; <6% as glucuronide conjugates)
Half-Life Elimination
27.7 hours (following a single dose); 32.5 hours (following multiple doses)
Protein Binding
Highly protein bound (95% to albumin and α-glycoprotein); does not bind to sex-hormone-binding globulin
Use in Specific Populations
Special Populations: Renal Function Impairment
Raloxifene AUC was 122% higher in patients with moderate to severe renal impairment.
Special Populations: Hepatic Function Impairment
Raloxifene apparent clearance was reduced 56% and plasma concentrations were increased 150% in patients with mild hepatic impairment.
Use: Labeled Indications
Osteoporosis: Treatment and prevention of osteoporosis in postmenopausal females.
Risk reduction for invasive breast cancer: Risk reduction of invasive breast cancer in postmenopausal females with osteoporosis; risk reduction of invasive breast cancer in postmenopausal females with high risk for invasive breast cancer (high risk is defined as at least 1 breast biopsy showing lobular carcinoma in situ or atypical hyperplasia, one or more first-degree relatives with breast cancer, or a 5-year predicted risk of breast cancer 1.66% or more [based on the modified Gail model]; factors included in the modified Gail model include current age, number of first-degree relatives with breast cancer, number of breast biopsies, age at menarche, nulliparity, or age of first live birth).
Limitations of use: Raloxifene does not eliminate the risk of breast cancer; patients should have a breast exam and mammogram prior to initiating raloxifene and continue regular breast exams and mammograms as per current guideline recommendations. Raloxifene is not indicated for the treatment of invasive breast cancer or reduction of the risk of recurrence. Raloxifene is not indicated for the reduction of the risk of noninvasive breast cancer. There are no data available regarding the effect of raloxifene on invasive breast cancer incidence in females with inherited mutations BRCA1, BRCA2 to be able to make specific recommendations on the effectiveness of raloxifene.
Contraindications
History of or current venous thromboembolic disorders (including DVT, PE, and retinal vein thrombosis); pregnancy
Dosage and Administration
Dosing: Adult
Note: Patients with osteoporosis should receive supplemental calcium and vitamin D if dietary intake is inadequate.
Osteoporosis (postmenopausal females):
Treatment (alternative agent) and prevention: Note: May be considered as an alternative treatment option to reduce the risk of vertebral fractures in patients for whom bisphosphonates and denosumab are unsuitable, or in patients with a high risk of fracture and a high risk of invasive breast cancer, if they also have a low risk of deep vein thrombosis (AACE [Camacho 2016]; ES [Eastell 2019]).
Oral: 60 mg once daily.
Duration of therapy: Continued raloxifene therapy is necessary to maintain increases in bone mineral density (BMD). In 1 study, BMD increases were maintained during 7 years of therapy in postmenopausal females with osteoporosis (Siris 2005). Effects on BMD diminish relatively quickly (eg, within 1 to 2 years) when raloxifene is discontinued (AACE [Camacho 2016]; Siris 2005).
Risk reduction for invasive breast cancer in postmenopausal females: Oral: 60 mg once daily.
Duration of therapy for breast cancer risk reduction: 5 years; may be used longer than 5 years in females with osteoporosis where breast cancer risk reduction is a secondary benefit (Visvanathan 2013).
Dosing: Geriatric
Refer to adult dosing.
Administration
May be administered at any time of day without regard to meals.
Dietary Considerations
Osteoporosis prevention or treatment: Ensure adequate calcium and vitamin D intake; if dietary intake is inadequate, dietary supplementation is recommended. Females and males should consume:
Calcium: 1,000 mg/day (males: 50 to 70 years) or 1,200 mg/day (females ≥51 years and males ≥71 years) (IOM 2011; NOF [Cosman 2014]).
Vitamin D: 800 to 1,000 int. units daily (males and females ≥50 years) (NOF [Cosman 2014]). Recommended Dietary Allowance (RDA): 600 int. units daily (males and females ≤70 years) or 800 int. units daily (males and females ≥71 years) (IOM 2011).
Storage
Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
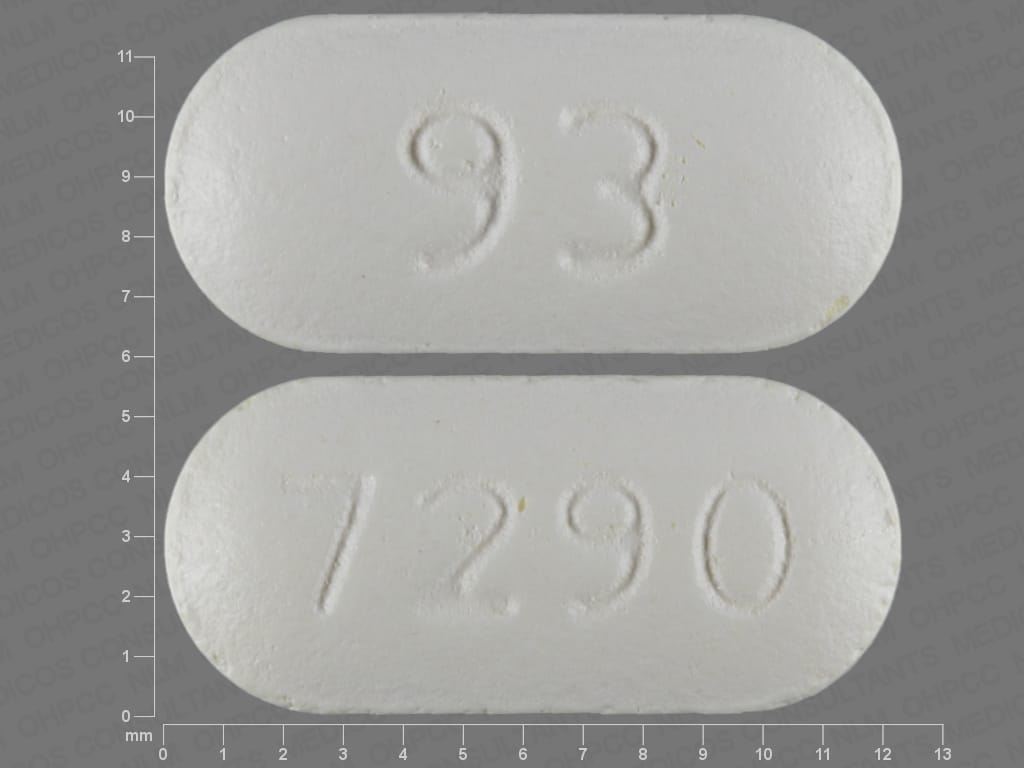
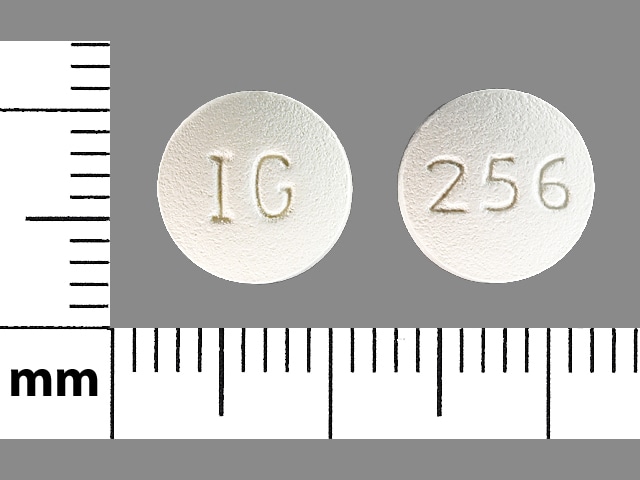
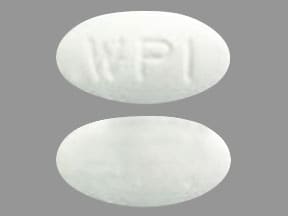
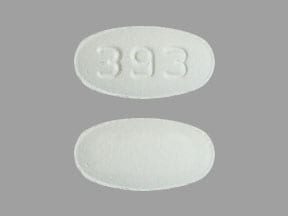
Raloxifene Images
Drug Interactions
Bile Acid Sequestrants: May decrease the absorption of Raloxifene. Consider therapy modification
Levothyroxine: Raloxifene may decrease the absorption of Levothyroxine. Consider therapy modification
Ospemifene: Selective Estrogen Receptor Modulators may enhance the adverse/toxic effect of Ospemifene. Ospemifene may also enhance adverse/toxic effects of other Selective Estrogen Receptor Modulators. Selective Estrogen Receptor Modulators may diminish the therapeutic effect of Ospemifene. Ospemifene may also diminish the therapeutic effects of other Selective Estrogen Receptor Modulators. Avoid combination
Adverse Reactions
>10%:
Cardiovascular: Peripheral edema (3% to 14%)
Endocrine & metabolic: Hot flash (8% to 29%)
Infection: Infection (11%)
Neuromuscular & skeletal: Arthralgia (11% to 16%), leg cramps (≤12%), muscle spasm (≤12%)
Respiratory: Flu-like symptoms (14% to 15%)
1% to 10%:
Cardiovascular: Chest pain (3%), syncope (<2%), venous thromboembolism (1% to 2%; includes deep vein thrombosis, pulmonary embolism, retinal vein thrombosis)
Central nervous system: Insomnia (6%), hypoesthesia (<2%), neuralgia (<2%)
Dermatologic: Skin rash (6%), diaphoresis (3%)
Endocrine & metabolic: Weight gain (9%)
Gastrointestinal: Abdominal pain (7%), vomiting (5%), gastrointestinal disease (3%), flatulence (2% to 3%), gastroenteritis (≤3%)
Genitourinary: Vaginal hemorrhage (3% to 6%), mastalgia (4%), leukorrhea (3%), urinary tract abnormality (3%), uterine disease (3%), endometrium disease (≤3%)
Neuromuscular & skeletal: Myalgia (8%), tendon disease (4%)
Respiratory: Bronchitis (10%), sinusitis (10%), pharyngitis (8%), pneumonia (3%), laryngitis (≤2%)
<1%, postmarketing, and/or case reports: Cerebrovascular accident, decreased LDL cholesterol (Delmas 1997; Walsh 1998), decreased serum cholesterol (Delmas 1997; Walsh 1998), decreased serum fibrinogen (Walsh 1998), hypertriglyceridemia (in women with a history of increased triglycerides in response to oral estrogens), retinal vein occlusion, superficial thrombophlebitis
Warnings/Precautions
Concerns related to adverse effects:
- Thromboembolic events: [US Boxed Warning]: Raloxifene may increase the risk for deep vein thrombosis (DVT) and pulmonary embolism (PE); use is contraindicated in patients with history of or current venous thromboembolic disorders (including DVT, PE, or retinal vein thrombosis). Consider risks versus benefits in females at risk for thromboembolism (heart failure [HF], superficial thrombophlebitis, active malignancy). The risk for DVT and PE are higher during the first 4 months of treatment. Superficial thrombophlebitis has also been reported.
Disease-related concerns:
- Breast cancer history: The use of raloxifene has not been adequately studied in females with a prior history of breast cancer.
- Cardiovascular disease: [US Boxed Warning]: The risk of death due to stroke is increased in postmenopausal females with coronary heart disease or at increased risk for major coronary events; consider risks versus benefits in females at risk for stroke. Do not use for primary or secondary prevention of cardiovascular disease. Assess risks versus benefits in females at risk for stroke (eg, prior stroke, transient ischemic attack, atrial fibrillation, hypertension, smokers).
- Hepatic impairment: Use with caution in patients with hepatic impairment; safety and efficacy have not been established.
- Hypertriglyceridemia: Females with a history of marked elevated triglycerides (>5.6 mmol/L or >500 mg/dL) in response to treatment with oral estrogens (or estrogen/progestin) may also develop elevated triglycerides when treated with raloxifene; monitor triglycerides.
- Renal impairment: Use with caution in patients with moderate to severe renal impairment; safety and efficacy have not been established.
- Uterine bleeding: Investigate unexplained uterine bleeding.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
- Estrogens: Concurrent use with systemic estrogen therapy is not recommended; safety has not been established.
Special populations:
- Males: Safety and efficacy have not been established in men. Raloxifene is not indicated for use in men.
- Premenopausal females: Safety has not been established in premenopausal females; use is not indicated and not recommended.
Other warnings/precautions:
- Appropriate use: Raloxifene does not eliminate the risk of breast cancer; investigate unexplained breast abnormality that occurs during treatment. Raloxifene is not indicated for treatment of invasive breast cancer, to reduce the risk of recurrence of invasive breast cancer, or to reduce the risk of noninvasive breast cancer. The efficacy (for breast cancer risk reduction) in females with inherited BRCA1 and BRCA1 mutations has not been established. The American Society of Clinical Oncology (ASCO) guidelines for breast cancer risk reduction (Visvanathan 2013) recommend raloxifene (for 5 years) as an option to reduce the risk of ER-positive invasive breast cancer in postmenopausal females with a 5-year projected risk (based on NCI trial model) of ≥1.66%, or with lobular carcinoma in situ. Raloxifene should not be used in premenopausal females. Females with osteoporosis may use raloxifene beyond 5 years of treatment.
- Prolonged immobilization: Discontinue raloxifene at least 72 hours prior to and during prolonged immobilization (postoperative recovery or prolonged bed rest); restart only once patient fully ambulatory. Advise patients to move periodically during prolonged travel.
Monitoring Parameters
Lipid profile (in females at risk for hypertriglyceridemia); mammogram and breast exam (prior to and regularly during treatment).
Osteoporosis: Serial bone mineral density (BMD) should be evaluated at baseline and every 1 to 3 years (usually at ~2 years following initiation of therapy, then more or less frequently depending on patient-specific factors and stability of BMD) (AACE/ACE [Camacho 2016]; ES [Eastell 2019]; NOF [Cosman 2014]); annual measurements of height and weight, assessment of chronic back pain; serum calcium and 25(OH)D; may consider monitoring biochemical markers of bone turnover (eg, fasting serum CTX or urinary NTX) at baseline, 3 months, and 6 months, to assess treatment response and adherence to therapy (ES [Eastell 2019]).
Pregnancy
Pregnancy Considerations
Raloxifene is contraindicated during pregnancy.
Patient Education
What is this drug used for?
- It is used to put off soft, brittle bones (osteoporosis) in women after change of life.
- It is used to treat soft, brittle bones (osteoporosis) in women after change of life.
- It is used to help prevent breast cancer in women after the change of life who have soft, brittle bones (osteoporosis) or those with more of a chance of getting breast cancer.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Hot flashes
- Joint pain
- Leg cramps
- Sweating a lot
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Severe cerebrovascular disease like change in strength on one side is greater than the other, trouble speaking or thinking, change in balance, or change in eyesight.
- DVT like edema, warmth, numbness, change in color, or pain in the extremities.
- Chest pain
- Shortness of breath
- Coughing up blood
- Vision changes
- Lump in breast
- Breast soreness or pain
- Nipple discharge
- Enlarged breasts
- Vaginal bleeding
- Flu-like symptoms
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.