Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet Extended Release 12 Hour, Oral:
Ranexa: 500 mg, 1000 mg
Generic: 500 mg, 1000 mg
Pharmacology
Mechanism of Action
Ranolazine exerts antianginal and anti-ischemic effects without changing hemodynamic parameters (heart rate or blood pressure). At therapeutic levels, ranolazine inhibits the late phase of the inward sodium channel (late INa) in ischemic cardiac myocytes during cardiac repolarization reducing intracellular sodium concentrations and thereby reducing calcium influx via Na+-Ca2+ exchange. Decreased intracellular calcium reduces ventricular tension and myocardial oxygen consumption. It is thought that ranolazine produces myocardial relaxation and reduces anginal symptoms through this mechanism although this is uncertain. At higher concentrations, ranolazine inhibits the rapid delayed rectifier potassium current (IKr) thus prolonging the ventricular action potential duration and subsequent prolongation of the QT interval.
Pharmacokinetics/Pharmacodynamics
Absorption
Highly variable
Metabolism
Extensive; Hepatic via CYP3A (major) and 2D6 (minor); intestines
Excretion
Primarily urine (75% mostly as metabolites; <5% as unchanged drug); feces (25% mostly as metabolites; <5% as unchanged drug)
Time to Peak
2 to 5 hours
Half-Life Elimination
Ranolazine: Terminal: 7 hours; Metabolites (activity undefined): 6 to 22 hours
Protein Binding
~62%
Use in Specific Populations
Special Populations: Renal Function Impairment
Cmax is increased between 40% to 50%.
Special Populations: Hepatic Function Impairment
Cmax is increased by 30% in cirrhotic patients with mild (Child-Pugh class A) hepatic impairment and 80% in cirrhotic patients with moderate (Child-Pugh class B) hepatic impairment.
Use: Labeled Indications
Chronic angina: Treatment of chronic angina
Note: According to the 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guidelines for patients with stable ischemic heart disease, ranolazine may be useful when prescribed as a substitute for beta blockers for relief of symptoms if initial treatment with beta blockers leads to unacceptable side effects, is less effective, or if initial treatment with beta-blockers is contraindicated. May also be used in combination with beta-blockers, for relief of symptoms when initial treatment with beta-blockers is not successful (Fihn 2012).
Use: Off Label
Ventricular tachycardiacyes
Data from small prospective studies and retrospective analysis suggest that ranolazine may be beneficial for suppression of ventricular tachycardia Bunch 2000, Scirica 2007, Yeung 2014. Additional data may be necessary to further define the role of ranolazine in this condition.
Based on the American Heart Association/American College of Cardiology/Heart Rhythm Society (AHA/ACC/HRS) Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death, ranolazine is effective at suppressing ventricular tachycardia.
Contraindications
Hepatic cirrhosis; concurrent strong CYP3A inhibitors; concurrent CYP3A inducers
Dosage and Administration
Dosing: Adult
Note: May be used with beta-blockers, nitrates, calcium channel blockers, antiplatelet therapy, lipid-lowering therapy, angiotensin-converting enzyme (ACE) inhibitors, and angiotensin-receptor blockers.
Chronic angina: Oral: Initial: 500 mg twice daily; may increase to 1,000 mg twice daily as needed (based on symptoms); maximum recommended dose: 1,000 mg twice daily
Missed doses: If a dose is missed, it should be taken at the next scheduled time; the next dose should not be doubled.
Ventricular tachycardia (off-label use): Oral: 500 to 1,000 mg every 12 hours (AHA/ACC/HRS [Al-Khatib 2017]; Bunch 2000; Scirica 2007)
Dosage adjustment for ranolazine with concomitant medications:
Diltiazem, erythromycin, fluconazole, verapamil, and other moderate CYP3A inhibitors: Ranolazine dose should not exceed 500 mg twice daily
CYP3A inducers or strong CYP3A inhibitors: Concomitant use is contraindicated
P-glycoprotein inhibitors (eg, cyclosporine): Titrate ranolazine based on clinical response
Dosing: Geriatric
Refer to adult dosing. Select dose cautiously, starting at the lower end of the dosing range.
Administration
Oral: Administer with or without meals. Swallow tablet whole; do not crush, break, or chew.
Dietary Considerations
Limit the use of grapefruit juice; the ranolazine dose should not exceed 500 mg twice daily when taken with grapefruit juice or grapefruit-containing products.
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
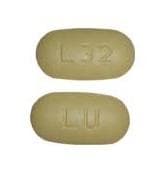
Ranolazine Images
Drug Interactions
Afatinib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Afatinib. Management: Reduce afatinib by 10 mg if not tolerated. Some non-US labeling recommends avoiding combination if possible. If used, administer the P-gp inhibitor simultaneously with or after the dose of afatinib. Consider therapy modification
Angiotensin II Receptor Blockers: Ranolazine may enhance the adverse/toxic effect of Angiotensin II Receptor Blockers. Monitor therapy
Angiotensin-Converting Enzyme Inhibitors: Ranolazine may enhance the adverse/toxic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Antifungal Agents (Azole Derivatives, Systemic): May decrease the metabolism of Ranolazine. Fluconazole and isavuconazonium considerations are addressed in separate monographs. Exceptions: Fluconazole; Isavuconazonium Sulfate. Avoid combination
ARIPiprazole: CYP3A4 Inhibitors (Weak) may increase the serum concentration of ARIPiprazole. Management: Monitor for increased aripiprazole pharmacologic effects. Aripiprazole dose adjustments may or may not be required based on concomitant therapy and/or indication. Consult full interaction monograph for specific recommendations. Monitor therapy
ARIPiprazole: CYP2D6 Inhibitors (Weak) may increase the serum concentration of ARIPiprazole. Management: Monitor for increased aripiprazole pharmacologic effects. Aripiprazole dose adjustments may or may not be required based on concomitant therapy and/or indication. Consult full interaction monograph for specific recommendations. Monitor therapy
AtorvaSTATin: Ranolazine may increase the serum concentration of AtorvaSTATin. Monitor therapy
Betrixaban: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Betrixaban. Management: Decrease the adult betrixaban dose to an initial single dose of 80 mg followed by 40 mg once daily if combined with a P-glycoprotein inhibitor. Consider therapy modification
Bilastine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Bilastine. Management: Consider alternatives when possible; bilastine should be avoided in patients with moderate to severe renal insufficiency who are receiving p-glycoprotein inhibitors. Consider therapy modification
Brentuximab Vedotin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Brentuximab Vedotin. Specifically, concentrations of the active monomethyl auristatin E (MMAE) component may be increased. Monitor therapy
Calcium Channel Blockers (Nondihydropyridine): May increase the serum concentration of Ranolazine. Management: Limit ranolazine dose to a maximum of 500 mg twice daily when used with diltiazem or verapamil. Exceptions: Bepridil. Consider therapy modification
Celiprolol: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Celiprolol. Monitor therapy
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Colchicine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Colchicine. Colchicine distribution into certain tissues (e.g., brain) may also be increased. Management: Colchicine is contraindicated in patients with impaired renal or hepatic function who are also receiving a p-glycoprotein inhibitor. In those with normal renal and hepatic function, reduce colchicine dose as directed. See full monograph for details. Consider therapy modification
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CYP3A4 Inducers (Moderate): May decrease the serum concentration of Ranolazine. Avoid combination
CYP3A4 Inducers (Strong): May decrease the serum concentration of Ranolazine. Avoid combination
CYP3A4 Inhibitors (Moderate): May increase the serum concentration of Ranolazine. Management: Limit the ranolazine adult dose to a maximum of 500 mg twice daily in patients concurrently receiving moderate CYP3A4 inhibitors (e.g., diltiazem, verapamil, erythromycin, etc.). Consider therapy modification
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Ranolazine. Avoid combination
Dabigatran Etexilate: P-glycoprotein/ABCB1 Inhibitors may increase serum concentrations of the active metabolite(s) of Dabigatran Etexilate. Monitor therapy
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Digoxin: Ranolazine may increase the serum concentration of Digoxin. Monitor therapy
Dofetilide: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Dofetilide. Monitor therapy
DOXOrubicin (Conventional): P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to P-glycoprotein inhibitors in patients treated with doxorubicin whenever possible. One U.S. manufacturer (Pfizer Inc.) recommends that these combinations be avoided. Consider therapy modification
Edoxaban: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Edoxaban. Management: See full monograph for details. Reduced doses are recommended for patients receiving edoxaban for venous thromboembolism in combination with certain P-gp inhibitors. Similar dose adjustment is not recommended for edoxaban use in atrial fibrillation. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Erdafitinib: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Everolimus: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Everolimus. Monitor therapy
Flibanserin: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Flibanserin. Monitor therapy
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Haloperidol: QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of Haloperidol. Monitor therapy
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Larotrectinib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Larotrectinib. Monitor therapy
Lasmiditan: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Avoid combination
Lefamulin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Lefamulin. Management: Avoid concomitant use of lefamulin tablets with P-glycoprotein/ABCB1 inhibitors. If concomitant use is required, monitor for lefamulin adverse effects. Consider therapy modification
Lemborexant: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Lemborexant. Management: The maximum recommended dosage of lemborexant is 5 mg, no more than once per night, when coadministered with weak CYP3A4 inhibitors. Consider therapy modification
Lomitapide: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Lomitapide. Management: Patients on lomitapide 5 mg/day may continue that dose. Patients taking lomitapide 10 mg/day or more should decrease the lomitapide dose by half. The lomitapide dose may then be titrated up to a max adult dose of 30 mg/day. Consider therapy modification
Lovastatin: Ranolazine may enhance the myopathic (rhabdomyolysis) effect of Lovastatin. Ranolazine may increase the serum concentration of Lovastatin. Ranolazine may also enhance the distribution of lovastatin to specific cells/tissues/organs where P-glycoprotein is present in large amounts (eg, brain, T-lymphocytes, testes, etc.). Monitor therapy
MetFORMIN: Ranolazine may increase the serum concentration of MetFORMIN. Management: Limit the metformin dose to a maximum of 1,700 mg per day when used together with ranolazine 1,000 mg twice daily. Monitor patients for metformin toxicities, including lactic acidosis and carefully weigh the risks and benefits of this combination. Consider therapy modification
Naldemedine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Naldemedine. Monitor therapy
Naloxegol: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Naloxegol. Monitor therapy
NiMODipine: CYP3A4 Inhibitors (Weak) may increase the serum concentration of NiMODipine. Monitor therapy
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
PAZOPanib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of PAZOPanib. Avoid combination
Perhexiline: CYP2D6 Inhibitors (Weak) may increase the serum concentration of Perhexiline. Monitor therapy
P-glycoprotein/ABCB1 Inhibitors: May increase the serum concentration of Ranolazine. Monitor therapy
P-glycoprotein/ABCB1 Substrates: Ranolazine may increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Pimozide: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Pimozide. Avoid combination
Prucalopride: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Prucalopride. Monitor therapy
QT-prolonging Agents (Highest Risk): QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
RifAMPin: May decrease the serum concentration of Ranolazine. Avoid combination
RifAXIMin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of RifAXIMin. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Silodosin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Silodosin. Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Simvastatin: Ranolazine may increase the serum concentration of Simvastatin. Management: Avoid the concurrent use of ranolazine with simvastatin when possible. If used together, avoid doses of simvastatin greater than 20 mg/day. Consider therapy modification
St John's Wort: May decrease the serum concentration of Ranolazine. Avoid combination
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Tacrolimus (Systemic): Ranolazine may increase the serum concentration of Tacrolimus (Systemic). Monitor therapy
Talazoparib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Talazoparib. Management: These listed exceptions are discussed in detail in separate interaction monographs. Monitor therapy
Tegaserod: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Tegaserod. Monitor therapy
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Topotecan: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Topotecan. Avoid combination
Triazolam: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Triazolam. Management: Consider triazolam dose reduction in patients receiving concomitant weak CYP3A4 inhibitors. Consider therapy modification
Ubrogepant: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Ubrogepant. Management: In patients taking weak CYP3A4 inhibitors, the initial and second dose (if needed) of ubrogepant should be limited to 50 mg. Consider therapy modification
Venetoclax: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Venetoclax. Management: Consider a venetoclax dose reduction by at least 50% in patients requiring concomitant treatment with P-glycoprotein (P-gp) inhibitors. Consider therapy modification
VinCRIStine (Liposomal): P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of VinCRIStine (Liposomal). Avoid combination
Adverse Reactions
>0.5% to 10%:
Cardiovascular: Bradycardia (≤4%), hypotension (≤4%), orthostatic hypotension (≤4%), palpitation (≤4%), peripheral edema (≤4%), prolonged QT interval on ECG (>500 msec: ≤1%)
Central nervous system: Dizziness (6%; may be dose-related), headache (≤6%), confusion (≤4%), syncope (≤4%), vertigo (≤4%)
Dermatologic: Hyperhidrosis (≤4%)
Gastrointestinal: Constipation (5%), abdominal pain (≤4%), anorexia (≤4%), dyspepsia (≤4%), nausea (≤4%; dose-related), vomiting (≤4%), xerostomia (≤4%)
Genitourinary: Hematuria (≤4%)
Neuromuscular: Weakness (≤4%)
Ophthalmic: Blurred vision (≤4%)
Otic: Tinnitus (≤4%)
Respiratory: Dyspnea (≤4%)
≤0.5%, postmarketing, and/or case reports: Angioedema, ataxia, decreased glycosylated hemoglobin, decreased T-wave amplitude, dysuria, eosinophilia, hallucination, hypoesthesia, hypoglycemia (diabetic patients), increased blood urea nitrogen, increased serum creatinine, leukopenia, pancytopenia, paresthesia, pruritus, pulmonary fibrosis, renal failure, skin rash, thrombocytopenia, torsade de pointes (Morrow 2007), tremor, T-wave changes (notched), urinary retention, urine discoloration
Warnings/Precautions
Concerns related to adverse effects:
- Altered cardiac conduction: Has been shown to prolong QTc interval in a dose/plasma concentration-related manner. At Tmaxfollowing repeat dosing at 1000 mg twice daily, the mean change in QTc is ~6 msec, but 5% of the population (with the highest plasma concentrations) has at least a 15 msec increase. Cirrhotic patients with mild to moderate hepatic impairment demonstrated a 3-fold increase QT prolongation; use is contraindicated in patients with liver cirrhosis. The incidence of symptomatic arrhythmias was similar to placebo in one trial (Morrow 2007). Risk versus benefit should be assessed in patients maintained on a higher dose (>2,000 mg/day) or exposure, concurrent use of other QT-prolonging drugs, potassium-channel variants known to cause QT prolongation, family history of or congenital long QT syndrome, or known acquired QT interval prolongation.
Disease-related concerns:
- Acute coronary syndrome: Ranolazine will not relieve acute angina episode and has not demonstrated benefit in acute coronary syndrome.
- Hepatic impairment: Ranolazine plasma levels increase by 30% in patients with mild (Child-Pugh class A) and by 80% in patients with moderate (Child-Pugh class B) hepatic impairment. Use is contraindicated in patients with cirrhosis.
- Renal impairment: Acute renal failure has been observed in some patients with severe renal impairment (CrCl <30 mL/minute); if acute renal failure develops (marked increase in serum creatinine associated with increased BUN), discontinue ranolazine and manage appropriately. Monitor renal function periodically in patients with moderate to severe renal impairment; particularly for increases in serum creatinine accompanied by increased BUN. In a renal impairment study, patients with severe impairment exhibited an initial elevation in diastolic blood pressure (~12 to 17 mm Hg at day 3), however, this diminished to ~4 mm Hg increase by day 5 (Jerling 2005); consider monitoring blood pressure in patients with renal dysfunction. Ranolazine has not been evaluated in patients requiring dialysis.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information. Use is contraindicated with inducers and strong inhibitors of CYP3A.
Special populations:
- Elderly: Use with caution in patients ≥75 years of age; they may experience more adverse events (including serious adverse events) and drug discontinuations due to adverse events.
Monitoring Parameters
Baseline and follow up ECG to evaluate QT interval; monitor renal function periodically in patients with moderate to severe renal impairment, particularly for increases in serum creatinine accompanied by increased BUN; consider monitoring blood pressure in patients with renal dysfunction; correct and maintain serum potassium in normal limits
Pregnancy
Pregnancy Considerations
Adverse events have been observed in animal reproduction studies.
Patient Education
What is this drug used for?
- It is used to treat a type of long-term chest pain (stable angina) in some people.
Frequently reported side effects of this drug
- Headache
- Dizziness
- Constipation
- Nausea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain.
- Chest pain
- Abnormal heartbeat
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.