Boxed Warning
Premature discontinuation increases the risk of thrombotic events:
Premature discontinuation of any oral anticoagulant, including rivaroxaban, increases the risk of thrombotic events. If anticoagulation with rivaroxaban is discontinued for a reason other than pathological bleeding or completion of a course of therapy, consider coverage with another anticoagulant.
Spinal/Epidural hematomas:
Epidural or spinal hematomas have occurred in patients treated with rivaroxaban who are receiving neuraxial anesthesia or undergoing spinal puncture. These hematomas may result in long-term or permanent paralysis. Consider these risks when scheduling patients for spinal procedures. Factors that can increase the risk of developing epidural or spinal hematomas in these patients include use of indwelling epidural catheters; concomitant use of other drugs that affect hemostasis, such as nonsteroidal anti-inflammatory drugs (NSAIDs), platelet inhibitors, or other anticoagulants; a history of traumatic or repeated epidural or spinal punctures; or a history of spinal deformity or spinal surgery. The optimal timing between the administration of rivaroxaban and neuraxial procedures is not known.
Monitor patients frequently for signs and symptoms of neurological impairment. If neurological compromise is noted, urgent treatment is necessary.
Consider the benefits and risks before neuraxial intervention in patients who are anticoagulated or are to be anticoagulated for thromboprophylaxis.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Xarelto: 2.5 mg, 10 mg, 15 mg, 20 mg
Tablet Therapy Pack, Oral:
Xarelto Starter Pack: 15 mg (42s) and 20 mg (9s) (51 ea)
Pharmacology
Mechanism of Action
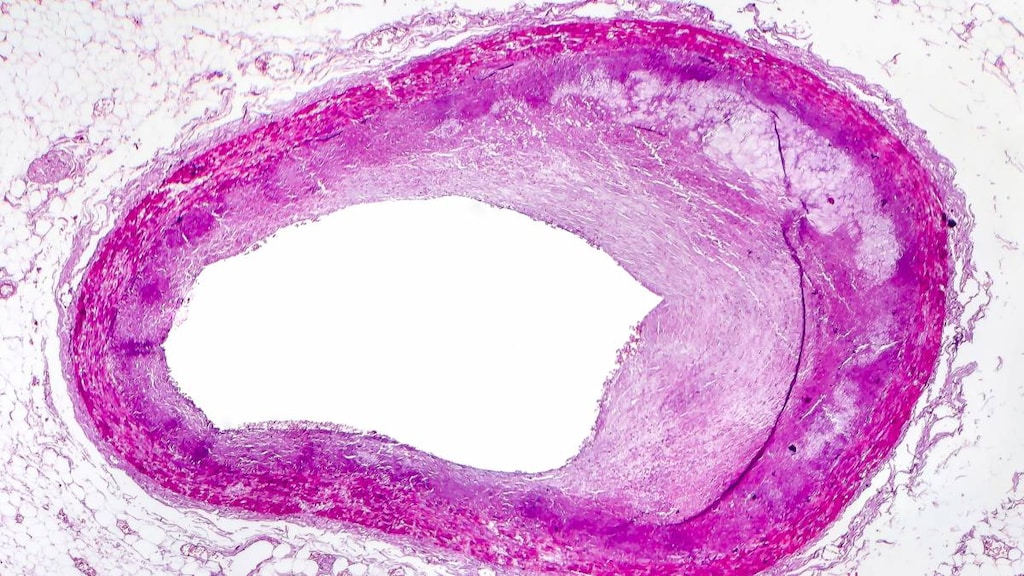
Inhibits platelet activation and fibrin clot formation via direct, selective and reversible inhibition of factor Xa (FXa) in both the intrinsic and extrinsic coagulation pathways. FXa, as part of the prothrombinase complex consisting also of factor Va, calcium ions, factor II and phospholipid, catalyzes the conversion of prothrombin to thrombin. Thrombin both activates platelets and catalyzes the conversion of fibrinogen to fibrin.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid
Distribution
Vdss: ~50 L
Metabolism
Hepatic via CYP3A4/5 and CYP2J2
Excretion
Urine (66% primarily via active tubular secretion [~36% as unchanged drug; 30% as inactive metabolites]); feces (28% [7% as unchanged drug; 21% as inactive metabolites])
Time to Peak
Plasma: 2 to 4 hours
Half-Life Elimination
Terminal: 5 to 9 hours; Elderly: 11 to 13 hours
Protein Binding
~92% to 95% (primarily to albumin)
Use in Specific Populations
Special Populations: Renal Function Impairment
Rivaroxaban exposure is increased by 44% in patients with mild impairment (CrCl 50 to 79 mL/minute) and by 52% in patients with moderate impairment (CrCl 30 to 49 mL/minute). In patients with moderate renal impairment, a 1.86-fold increase in the AUC for factor Xa inhibition and a 2.16-fold increase in PT prolongation was observed (Kubitza 2010).
Special Populations: Hepatic Function Impairment
Significant increases in rivaroxaban exposure were observed in subjects with moderate hepatic impairment (Child-Pugh class B). Increases in pharmacodynamic effects were also observed. No clinical data are available for patients with severe hepatic impairment.
Special Populations: Elderly
Elderly patients exhibit higher plasma concentrations than younger patients, with mean AUC values being ~50% higher, mainly because of reduced (apparent) total body and renal clearance.
Special Populations: Race
Healthy Japanese subjects were found to have 20% to 40% higher exposures compared with other ethnicities, including Chinese subjects.
Use: Labeled Indications
Coronary artery disease (stable) or peripheral artery disease: Reduction of risk of major cardiovascular (CV) events (CV death, myocardial infarction, and stroke) in patients with coronary artery disease (chronic) or peripheral artery disease.
Indefinite anticoagulation (reduced intensity dosing against venous thromboembolism recurrence): Reduction in the risk of recurrence of deep vein thrombosis (DVT) and pulmonary embolism (PE) in patients at continued risk of DVT and PE following at least 6 months of initial full therapeutic anticoagulant treatment for DVT and/or PE.
Nonvalvular atrial fibrillation: Prevention of stroke and systemic embolism in patients with nonvalvular atrial fibrillation.
Venous thromboembolism (deep vein thrombosis or pulmonary embolism): Treatment of DVT or PE.
Venous thromboembolism prophylaxis in acutely ill medical patients: Prophylaxis of venous thromboembolism (VTE) and VTE-related death during hospitalization and posthospital discharge in adults admitted for an acute medical illness who are at risk for thromboembolic complications due to moderate or severe restricted mobility and other risk factors for VTE and not at high risk of bleeding.
Venous thromboembolism prophylaxis in total hip or knee arthroplasty: Postoperative thromboprophylaxis of DVT, which may lead to PE in patients undergoing total hip arthroplasty or total knee arthroplasty.
Use: Off Label
Acute coronary syndrome (after stabilization with initial management)b
Data from a randomized, double-blind, placebo-controlled trial demonstrated that the use of rivaroxaban in addition to clopidogrel plus aspirin results in better cardiovascular outcomes (eg, reduced cardiovascular death, stroke, or MI) as compared to clopidogrel plus aspirin alone in patients with a recent acute coronary syndrome; however, major bleeding events occurred more often in patients receiving rivaroxaban Mega 2012. Caution should be employed when using rivaroxaban in this setting and should only be used in patients without high risk of bleeding Lip 2018a.
Heparin-induced thrombocytopenia (treatment)cyes
Data from case series, small prospective cohort studies, and a systematic review suggest that rivaroxaban may be used in the management of patients with heparin-induced thrombocytopenia (HIT) Linkins 2016, Kunk 2017, Sharifi 2015, Shatzel 2016, Warkentin 2017.
Based on the American Society of Hematology 2018 guidelines for management of venous thromboembolism: heparin-induced thrombocytopenia, rivaroxaban is an effective and recommended agent for heparin-induced thrombocytopenia complicated by thrombosis (HITT) or heparin-induced thrombocytopenia without thrombosis (isolated HIT).
Superficial vein thrombosis, acute symptomaticb
Data from a small phase 3b, open-label, randomized, double-blind trial support the use of rivaroxaban in the treatment of superficial vein thrombosis, particularly if there is involvement of the great saphenous vein, a ≥5 cm segment is affected, or other risk factors for venous thromboembolism are present Beyer-Westendorf 2017.
Contraindications
Severe hypersensitivity to rivaroxaban or any component of the formulation; active pathological bleeding
Canadian labeling: Additional contraindications (not in US labeling): Hepatic disease (including Child-Pugh classes B and C) associated with coagulopathy and clinically relevant bleeding risk; lesions or conditions at increased risk of clinically significant bleeding (eg, hemorrhagic or ischemic cerebral infarction, spontaneous or acquired impairment of hemostasis, active peptic ulcer disease with recent bleeding); concomitant systemic treatment with strong CYP3A4 and P-glycoprotein (P-gp) inhibitors (eg, ketoconazole, itraconazole, posaconazole, ritonavir); concomitant use with any other anticoagulant including unfractionated heparin (except at doses used to maintain central venous or arterial catheter patency), low molecular weight heparins (eg, enoxaparin, dalteparin) or heparin derivatives (eg, fondaparinux); concomitant use with warfarin, dabigatran, edoxaban, or apixaban except when switching therapy to or from rivaroxaban; pregnancy; lactation
Dosage and Administration
Dosing: Adult
Acute coronary syndrome (after stabilization with initial management) (off-label):
Note: As add-on to clopidogrel (not prasugrel or ticagrelor) and aspirin therapy in patients who are not at high risk of bleeding and do not require chronic therapeutic anticoagulation for another indication; patient preference should also be taken into consideration given the higher risk of bleeding when adding rivaroxaban to dual antiplatelet therapy (Lip 2018a).
Oral: 2.5 mg twice daily; administer in combination with low dose aspirin plus clopidogrel; continue rivaroxaban for ~1 year (Lip 2018a; Mega 2012).
Coronary artery disease (stable) or peripheral artery disease (prevention of major cardiovascular events):
Note: Some experts do not recommend substituting or adding anticoagulant therapy to aspirin for these indications due to excess risk of major bleeding (Berger 2018; Hennekens 2018). May consider rivaroxaban in carefully selected patients who are at high risk of cardiovascular events and low risk of bleeding who do not require therapeutic anticoagulation or dual antiplatelet therapy for another indication (Eikelboom 2017).
Oral: 2.5 mg twice daily; administer in combination with daily low dose aspirin.
Heparin-induced thrombocytopenia (off-label use): Note: For treatment of acute heparin-induced thrombocytopenia (HIT), either as initial therapy in selected hemodynamically stable patients or after initial therapy with a parenteral non-heparin anticoagulant (Kunk 2017; Shatzel 2016; Warkentin 2017).
HIT with or without thrombosis: Oral: 15 mg twice daily with food for 21 days or until platelet count recovery, whichever is longer, followed by 20 mg once daily with food. Note: If initially treated with a parenteral non-heparin anticoagulant, can transition to 20 mg once daily after platelet count recovery. However, if the parenteral non-heparin anticoagulant is administered for <21 days, transition to 15 mg twice daily; then, after a total of 21 days with non-heparin anticoagulation, reduce to 20 mg once daily (Coutre 2019).
Duration: Not well established:
HIT without thrombosis: Typically, 4 weeks to 3 months (ACCP [Linkins 2012]). Some experts allow for discontinuation of anticoagulation after platelet count recovery, potentially resulting in a shorter duration (ASH [Cuker 2018]).
HIT with thrombosis: Typically, 3 to 6 months (ACCP [Linkins 2012]; ASH [Cuker 2018]).
Nonvalvular atrial fibrillation (to prevent stroke and systemic embolism): Oral: 20 mg once daily with the evening meal.
Post-percutaneous coronary intervention with stent placement and nonvalvular atrial fibrillation (off-label): Oral: 15 mg once daily with food; administer with an appropriate antithrombotic regimen including clopidogrel (preferred P2Y12 inhibitor in this situation) with or without aspirin, depending on risk for thrombosis and bleeding (Gibson 2016; Sarafoff 2019).
Superficial vein thrombosis, acute symptomatic (off-label use):
Note: For use in patients at increased risk for thromboembolism or with recurrent superficial vein thrombosis:
Oral: 10 mg once daily for 45 days (Beyer-Westendorf 2017).
Venous thromboembolism:
Deep vein thrombosis and/or pulmonary embolism treatment:
Note: For initial therapy, without prior treatment with a parenteral anticoagulant (in hemodynamically stable patients without extensive clot burden) or as transition from a parenteral anticoagulant. May be used in patients with active cancer (eg, metastatic disease or receiving chemotherapy), but data are limited. However, in patients with GI cancer, low molecular weight heparin (LMWH) is preferred (ASCO [Key 2019]; Bauer 2020; Young 2018).
Oral: 15 mg twice daily with food for 21 days followed by 20 mg once daily with food.
Duration of therapeutic anticoagulation (first episode, general recommendations): Optimal duration of therapy is unknown and is dependent on many factors, such as whether provoking events were present, patient risk factors for recurrence and bleeding, and individual preferences:
Provoked venous thromboembolism: 3 months (provided the provoking risk factor is no longer present) (ACCP [Kearon 2016])
Unprovoked pulmonary embolism or deep vein thrombosis (proximal or isolated distal): ≥3 months depending on risk of venous thromboembolism (VTE) recurrence and bleeding. (ACCP [Kearon 2012]; ACCP [Kearon 2016]; ISTH [Baglin 2012]).
Note: All patients receiving indefinite therapeutic anticoagulation with no specified stop date should be reassessed at periodic intervals.
Indefinite anticoagulation (reduced intensity dosing for prophylaxis against venous thromboembolism recurrence): Note: For patients at elevated risk of recurrent VTE following at least 6 months of therapeutic anticoagulation. This reduced-intensity regimen is not recommended if indefinite full anticoagulation is indicated (Crowther 2017; Lip 2018b): Oral: 10 mg once daily (Weitz 2017).
Venous thromboembolism prophylaxis:
Acutely ill medical patients: Oral: 10 mg once daily for a total duration of 31 to 39 days (including hospitalization and postdischarge) (Cohen 2013; Spyropoulos 2018; manufacturer's labeling). Some experts prefer LMWH as prophylaxis during acute hospitalization and suggest not routinely extending prophylaxis beyond discharge (Pai 2019).
Total hip arthroplasty or total knee arthroplasty (alternative to LMWH): Oral: 10 mg once daily initiated at least 6 to 10 hours after surgery or when hemostasis established.
Duration: Optimal duration of prophylaxis is unknown but it is usually given for a minimum of 10 to 14 days and can be extended for up to 35 days (Eikelboom 2001; Falck-Ytter 2012); some experts suggest a duration in the lower end of the range (10 to 14 days) for total knee arthroplasty (TKA) or higher end of range (30 days) for total hip arthroplasty (THA) (Pai 2018).
Note: In carefully selected patients at low risk of VTE who are undergoing elective, unilateral THA or TKA, an alternative approach to prophylaxis is to give rivaroxaban 10 mg once daily for 5 days then switch to aspirin for an additional 30 days for THA or 9 days for TKA (Anderson 2018; Pai 2018).
Transitioning between anticoagulants: Note: This provides general guidance on transitioning between anticoagulants; also refer to local protocol for additional detail:
Transitioning from another anticoagulant to rivaroxaban:
Transitioning from LMWH or fondaparinux (therapeutic dose) to rivaroxaban:
General transition recommendation: Start rivaroxaban within 2 hours prior to the next scheduled dose of the parenteral agent.
VTE initial treatment transition (alternate recommendation): For acute VTE, some experts start rivaroxaban within 6 to 12 hours after the last dose of a twice daily LMWH regimen or within 12 to 24 hours after a once daily regimen (Hull 2018).
Transitioning from argatroban, bivalirudin, or unfractionated heparin (UFH) continuous infusion to rivaroxaban: Start rivaroxaban when the parenteral anticoagulant infusion is stopped (consult local protocol if aPTT is above the target range) (Bethea 2017; Davis 2017; Tran 2018).
Transitioning from warfarin to rivaroxaban: Discontinue warfarin and initiate rivaroxaban as soon as INR falls to <3 (US labeling) or ≤2.5 (Canadian labeling).
Transitioning from rivaroxaban to another anticoagulant:
Transitioning from rivaroxaban to UFH continuous infusion, LMWH, or fondaparinux: Start the parenteral anticoagulant when the next dose of rivaroxaban was scheduled to be given.
Transitioning from rivaroxaban to warfarin: Rivaroxaban can elevate the INR, complicating interpretation if overlapped with warfarin (Moore 2015). To minimize interference, check INR near the end of rivaroxaban dosing interval. Some experts suggest overlapping rivaroxaban with warfarin for ≥2 days until INR is therapeutic. An alternative is to stop rivaroxaban, start warfarin the same day, and bridge with a parenteral anticoagulant until the desired INR is reached (Leung 2019).
Transitioning between direct oral anticoagulants: Start new direct oral anticoagulants (DOACs) when the next dose of previous DOAC was scheduled to be given (Leung 2019).
Transitioning between anticoagulants in the perioperative setting: see 2017 AHA Scientific Statement, “Management of Patients on Non-Vitamin K Antagonist Oral Anticoagulants in the Acute Care and Periprocedural Setting” 2017.
Dosing adjustments with concomitant medications:
Dual P-gp and strong CYP3A inhibitors (eg, ketoconazole, ritonavir): Avoid concomitant use.
Dual P-gp and strong CYP3A inducers (eg, carbamazepine, phenytoin, rifampin, St. John's wort): Avoid concomitant use.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Obesity
In patients with a BMI >40 kg/m2 or weight >120 kg, the International Society on Thrombosis and Haemostasis (ISTH) 2016 guideline suggests avoiding the use of rivaroxaban (and other direct oral anticoagulants [DOACs]) due to the lack of clinical data in this population (ISTH [Martin 2016]). A 2017 review concluded, based on pharmacokinetic data, that for individuals with a BMI >40 kg/m2 (or weight >120 kg), rivaroxaban may be used and dosage adjustment is not necessary; however, studies were not powered to address outcomes (Moore 2017).
If used in a patient with a BMI >40 kg/m2 or weight >120 kg, ISTH suggests measuring peak and trough levels using an anti-factor Xa assay or mass spectrometry. If drug level is below the expected range, ISTH suggests changing to a vitamin K antagonist rather than adjusting the dose of rivaroxaban (ISTH [Martin 2016]).
Administration
Administer doses ≥15 mg with food; doses of 2.5 mg and 10 mg may be administered without regard to meals. For nonvalvular atrial fibrillation, administer with the evening meal. For patients who cannot swallow whole tablets, the tablets may be crushed and mixed with applesauce immediately prior to use; immediately follow administration of the 15 mg and 20 mg tablets with food (2.5 mg and 10 mg tablets may be administered without regard to food).
For nasogastric/gastric feeding tube administration, the tablets may be crushed and mixed in 50 mL of water; administer the suspension within 4 hours of preparation and follow administration of the 15 mg and 20 mg tablets immediately with enteral feeding (2.5 mg and 10 mg tablets may be administered without regard to food). Avoid administration distal to the stomach; a decrease in the AUC and Cmax (29% and 56%, respectively) was observed when rivaroxaban was delivered to the proximal small intestine; further decreases may be seen with delivery to the distal small intestine or ascending colon.
Missed doses: Patients receiving 15 mg twice daily dosing who miss a dose should take a dose immediately to ensure 30 mg of rivaroxaban is administered per day (two 15 mg tablets may be taken together); resume therapy the following day as previously taken. Patients receiving 2.5 mg twice daily who miss a dose should take a single 2.5 mg dose at the next scheduled time; then resume therapy as usual. Patients receiving once-daily dosing who miss a dose should take a dose as soon as possible on the same day; resume therapy the following day as previously taken.
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
Rivaroxaban Images
Drug Interactions
Acalabrutinib: May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Agents with Antiplatelet Properties (e.g., P2Y12 inhibitors, NSAIDs, SSRIs, etc.): May enhance the anticoagulant effect of Rivaroxaban. Management: Carefully consider risks and benefits of this combination and monitor closely; Canadian labeling recommends avoiding prasugrel or ticagrelor. Monitor therapy
Anticoagulants: May enhance the anticoagulant effect of Rivaroxaban. Refer to separate drug interaction content and to full drug monograph content regarding use of rivaroxaban with vitamin K antagonists (eg, warfarin, acenocoumarol) during anticoagulant transition and bridging periods. Exceptions: Acenocoumarol; Warfarin. Avoid combination
Antiplatelet Agents (P2Y12 Inhibitors): May enhance the adverse/toxic effect of Rivaroxaban. Specifically, the risk of bleeding may be increased. Management: Carefully consider risks and benefits of this combination and monitor closely; Canadian labeling recommends avoiding prasugrel or ticagrelor. Consider therapy modification
Apixaban: May enhance the anticoagulant effect of Anticoagulants. Refer to separate drug interaction content and to full drug monograph content regarding use of apixaban with vitamin K antagonists (eg, warfarin, acenocoumarol) during anticoagulant transition and bridging periods. Avoid combination
Aspirin: May enhance the adverse/toxic effect of Rivaroxaban. Specifically, the risk of bleeding may be increased. Management: Carefully consider risks and benefits of this combination and monitor closely. Consider therapy modification
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Bromperidol: May enhance the adverse/toxic effect of Anticoagulants. Monitor therapy
Caplacizumab: May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Clarithromycin: May increase the serum concentration of Rivaroxaban. Management: In patients with impaired renal function, clarithromycin should not be used unless the potential benefits outweigh the potential risks. This interaction is unlikely clinically significant in patients with normal renal function. Consider therapy modification
Cobicistat: May increase the serum concentration of Rivaroxaban. Avoid combination
Collagenase (Systemic): Anticoagulants may enhance the adverse/toxic effect of Collagenase (Systemic). Specifically, the risk of injection site bruising and/or bleeding may be increased. Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of Rivaroxaban. Avoid combination
Dabigatran Etexilate: May enhance the anticoagulant effect of Anticoagulants. Refer to separate drug interaction content and to full drug monograph content regarding use of dabigatran etexilate with vitamin K antagonists (eg, warfarin, acenocoumarol) during anticoagulant transition and bridging periods. Avoid combination
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dasatinib: May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Deferasirox: Anticoagulants may enhance the adverse/toxic effect of Deferasirox. Specifically, the risk for GI ulceration/irritation or GI bleeding may be increased. Monitor therapy
Deoxycholic Acid: Anticoagulants may enhance the adverse/toxic effect of Deoxycholic Acid. Specifically, the risk for bleeding or bruising in the treatment area may be increased. Monitor therapy
Edoxaban: May enhance the anticoagulant effect of Anticoagulants. Refer to separate drug interaction content and to full drug monograph content regarding use of edoxaban with vitamin K antagonists (eg, warfarin, acenocoumarol) during anticoagulant transition and bridging periods. Management: Some limited combined use may be indicated during periods of transition from one anticoagulant to another. See the full edoxaban drug monograph for specific recommendations on switching anticoagulant treatment. Avoid combination
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erythromycin (Systemic): May increase the serum concentration of Rivaroxaban. Management: In patients with impaired renal function, erythromycin should not be used unless the potential benefits outweigh the potential risks. This interaction is unlikely clinically significant in patients with normal renal function. Consider therapy modification
Estrogen Derivatives: May diminish the anticoagulant effect of Anticoagulants. More specifically, the potential prothrombotic effects of some estrogens and progestin-estrogen combinations may counteract anticoagulant effects. Management: Carefully weigh the prospective benefits of estrogens against the potential increased risk of procoagulant effects and thromboembolism. Use is considered contraindicated under some circumstances. Refer to related guidelines for specific recommendations. Exceptions: Tibolone. Consider therapy modification
Factor X (Human): Anticoagulants (Inhibitors of Factor Xa) may diminish the therapeutic effect of Factor X (Human). Monitor therapy
Fat Emulsion (Fish Oil Based): May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of Rivaroxaban. Management: Consider alternatives to this combination when possible. Rivaroxaban dose adjustments may be required when used with systemic fusidic acid. Patients using this combination should be monitored extra closely. Consider therapy modification
Hemin: May enhance the anticoagulant effect of Anticoagulants. Avoid combination
Herbs (Anticoagulant/Antiplatelet Properties) (eg, Alfalfa, Anise, Bilberry): May enhance the adverse/toxic effect of Anticoagulants. Bleeding may occur. Management: Avoid such combinations when possible. If used concomitantly, increase diligence in monitoring for adverse effects (eg, bleeding, bruising, altered mental status due to CNS bleeds). Consider therapy modification
Ibritumomab Tiuxetan: Anticoagulants may enhance the adverse/toxic effect of Ibritumomab Tiuxetan. Both agents may contribute to an increased risk of bleeding. Monitor therapy
Ibrutinib: May enhance the adverse/toxic effect of Anticoagulants. Monitor therapy
Inhibitors of CYP3A4 (Moderate) and P-glycoprotein: May increase the serum concentration of Rivaroxaban. Management: No action is needed in patients with normal renal function. US labeling recommends avoidance in patients with estimated creatinine clearance 15 to 80 mL/min unless prospective benefits outweigh the risks. Other non-US labels may differ. Consider therapy modification
Inhibitors of CYP3A4 (Strong) and P-glycoprotein: May increase the serum concentration of Rivaroxaban. Exceptions: Clarithromycin. Avoid combination
Inotersen: May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Limaprost: May enhance the adverse/toxic effect of Anticoagulants. The risk for bleeding may be increased. Monitor therapy
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
MiFEPRIStone: May enhance the adverse/toxic effect of Anticoagulants. Specifically, the risk of bleeding may be increased. Avoid combination
Nevirapine: May decrease the serum concentration of Rivaroxaban. Monitor therapy
Nintedanib: Anticoagulants may enhance the adverse/toxic effect of Nintedanib. Specifically, the risk for bleeding may be increased. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective): May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents (Nonselective): May enhance the adverse/toxic effect of Rivaroxaban. Specifically, the risk of bleeding may be increased. Management: A comprehensive risk to benefit assessment should be done for all patients before any concurrent use of rivaroxaban and nonsteroidal anti-inflammatory drugs (NSAIDs). If combined, monitor patients extra closely for signs and symptoms of bleeding. Consider therapy modification
Obinutuzumab: Anticoagulants may enhance the adverse/toxic effect of Obinutuzumab. Specifically, the risk of serious bleeding-related events may be increased. Monitor therapy
Omacetaxine: Anticoagulants may enhance the adverse/toxic effect of Omacetaxine. Specifically, the risk for bleeding-related events may be increased. Management: Avoid concurrent use of anticoagulants with omacetaxine in patients with a platelet count of less than 50,000/uL. Avoid combination
Omega-3 Fatty Acids: May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Oritavancin: May diminish the therapeutic effect of Anticoagulants. Specifically, oritavancin may artificially increase the results of laboratory tests commonly used to monitor anticoagulant effectiveness, which could lead to incorrect decisions to decrease anticoagulant doses. Monitor therapy
OXcarbazepine: May decrease the serum concentration of Rivaroxaban. Monitor therapy
Pentosan Polysulfate Sodium: May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Progestins: May diminish the therapeutic effect of Anticoagulants. More specifically, the potential prothrombotic effects of some progestins and progestin-estrogen combinations may counteract anticoagulant effects. Management: Carefully weigh the prospective benefits of progestins against the potential increased risk of procoagulant effects and thromboembolism. Use is considered contraindicated under some circumstances. Refer to related guidelines for specific recommendations. Consider therapy modification
Prostacyclin Analogues: May enhance the adverse/toxic effect of Anticoagulants. Specifically, the antiplatelet effects of these agents may lead to an increased risk of bleeding with the combination. Monitor therapy
Salicylates: May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
St John's Wort: May decrease the serum concentration of Rivaroxaban. Avoid combination
Sugammadex: May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Sulodexide: May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Telavancin: May diminish the therapeutic effect of Anticoagulants. Specifically, telavancin may artificially increase the results of laboratory tests commonly used to monitor anticoagulant effectiveness, which could lead to incorrect decisions to decrease anticoagulant doses. Monitor therapy
Thrombolytic Agents: May enhance the anticoagulant effect of Anticoagulants. Management: See full drug monograph for guidelines for the use of alteplase for acute ischemic stroke during treatment with oral anticoagulants. Monitor therapy
Tibolone: May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Tipranavir: May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Urokinase: May enhance the anticoagulant effect of Anticoagulants. Avoid combination
Vitamin E (Systemic): May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Anticoagulants may enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Vorapaxar: May enhance the adverse/toxic effect of Anticoagulants. More specifically, this combination is expected to increase the risk of bleeding. Avoid combination
Zanubrutinib: May enhance the adverse/toxic effect of Anticoagulants. Monitor therapy
Test Interactions
Prolongs activated partial thromboplastin time (aPTT), HepTest, and Russell viper venom time
Adverse Reactions
>10%: Hematologic & oncologic: Hemorrhage (5% to 28%)
1% to 10%:
Central nervous system: Dizziness (2%), insomnia (2%), anxiety (1%), depression (1%), fatigue (1%), syncope (1%)
Dermatologic: Wound secretion (3%), pruritus (2%), skin blister (1%)
Gastrointestinal: Abdominal pain (3%)
Hematologic & oncologic: Major hemorrhage (≤4%)
Hepatic: Increased serum transaminases (>3 x ULN: 2% [Watkins 2011])
Neuromuscular & skeletal: Back pain (3%), limb pain (2%), muscle spasm (1%)
Frequency not defined: Respiratory: Bronchiectasis, pulmonary hemorrhage
<1%, postmarketing, and/or case reports: Agranulocytosis, anaphylactic shock, anaphylaxis, angioedema, cerebral hemorrhage, cholestasis, decreased hemoglobin, DRESS syndrome, hematoma at injection site, hemiparesis, hemophthalmos, hepatitis, hepatic injury, hypersensitivity reaction, intracranial hemorrhage, jaundice, retroperitoneal hemorrhage, spinal hematoma, Stevens-Johnson syndrome, subdural hematoma, thrombocytopenia
Warnings/Precautions
Concerns related to adverse effects:
- Bleeding: The most common complication is bleeding; major hemorrhages (eg, intracranial, GI, retinal, epidural hematoma, adrenal bleeding) have been reported. Certain patients are at increased risk of bleeding; risk factors include bacterial endocarditis, congenital or acquired bleeding disorders, vascular retinopathy, thrombocytopenia, recent puncture of large vessels or organ biopsy, stroke, intracerebral surgery, or other neuraxial procedure, severe uncontrolled hypertension, renal impairment, recent major surgery, recent major bleeding (intracranial, GI, intraocular, or pulmonary), concomitant use of drugs that affect hemostasis, and advanced age. When used for venous thromboembolism (VTE) prophylaxis in acutely ill medical patients, rivaroxaban is not recommended for use in patients at an increased risk of bleeding, including patients with a history of bronchiectasis, pulmonary cavitation, or pulmonary hemorrhage, active cancer, gastroduodenal ulcer in the past 3 months, history of bleeding in the past 3 months, or dual antiplatelet therapy. Monitor for signs and symptoms of bleeding (weakness, dizziness, unexplained edema). Prompt clinical evaluation is warranted with any unexplained decrease in hemoglobin or blood pressure. Andexanet alfa is available for reversal of rivaroxaban in patients experiencing life-threatening or uncontrolled bleeding. Rivaroxaban is highly protein-bound, therefore, hemodialysis is ineffective. Protamine sulfate and vitamin K are not expected to affect the anticoagulant activity of rivaroxaban. Depending on the bleeding severity, activated oral charcoal should be considered if ingestion occurred within 1 to 2 hours of presentation. The following alternative options may also be considered depending on specific clinical scenario: 4-factor unactivated prothrombin concentrate (eg, Kcentra) or 4-factor activated prothrombin complex concentrate (eg, FEIBA). Some studies and case reports have shown moderate success in correcting coagulation tests with some of these agents; however, correction of coagulation tests does not imply reversal of the anticoagulation effect of the medication (AHA/ASA [Hemphill 2015; EHRA [Heidbuchel 2015]; NCS/SCCM [Frontera 2016]).
- Thromboembolic events: [US Boxed Warning]: As with any oral anticoagulant in the absence of adequate alternative anticoagulation, an increased risk of thrombotic events (including stroke) may occur with premature discontinuation of rivaroxaban. Consider the addition of alternative anticoagulant therapy when discontinuing rivaroxaban for reasons other than pathological bleeding or completion of a course of therapy. An increased rate of stroke was observed during the transition from rivaroxaban to warfarin in clinical trials in atrial fibrillation (AF) patients. In a post-hoc analysis of the ROCKET AF trial, patients who temporarily (>3 days) or permanently discontinued anticoagulation, the risk of stroke or non-CNS embolism was similar with rivaroxaban as compared to warfarin (Patel 2013). In patients with nonvalvular AF who had an acute ischemic stroke while receiving a direct-acting oral anticoagulant (DOAC) (eg, rivaroxaban), guidelines generally support withholding oral anticoagulation until 4 to 14 days after the onset of neurological symptoms (time frame may vary with shorter times for transient ischemic attack or small, nondisabling stroke and longer times for moderate to severe stroke) (AHA/ASA [Kernan 2014]; AHA/ASA [Powers 2018]).
Disease-related concerns:
- Antiphospholipid syndrome: Use not recommended in patients with triple-positive antiphospholipid syndrome; safety and efficacy have not been established. Patients positive for all 3 antiphospholipid antibodies (lupus anticoagulant, anticardiolipin, and anti-beta 2-glycoprotein I) may have increased rates of recurrent thrombotic events compared with vitamin K antagonist therapy.
- Bariatric surgery:
– Altered absorption: Evaluate the risk versus benefit of possible decreased drug absorption against the consideration of alternative anticoagulants; efficacy may be decreased after gastric bypass or sleeve gastrectomy. Apixaban’s absorption appears to occur primarily in the small intestine. Peak apixaban concentrations and total AUC are reduced by 60% when released in the distal small intestine and further reduced to 90% and 84%, respectively, when released in the ascending colon (Frost 2013).
– Rivaroxaban: Peak concentrations and AUC were reduced by 56% and 29%, respectively, when released into the proximal small intestine and further reduced in the distal small intestine or colon (manufacturer labeling 2019). Patients with significantly altered GI tracts are represented by small series and case reports (Hakeam 2017). The available data are conflicting for absorption alterations, derived from small populations, and underrepresent individual direct oral anticoagulants and surgeries (Kroll 2017; Kroll 2018; Lee 2013; Rottenstreich 2018).
- Hepatic impairment: Avoid use in patients with moderate to severe hepatic impairment (Child-Pugh classes B and C) or in patients with any hepatic disease associated with coagulopathy.
- Renal impairment: Use with caution in patients with moderate renal impairment (CrCl 30 to 50 mL/minute), including patients receiving concomitant drug therapy that may increase rivaroxaban systemic exposure and those with deteriorating renal function. Monitor for any signs or symptoms of blood loss. Avoid use in patients with CrCl <15 to 30 mL/minute depending on the indication. Avoid use in patients with end-stage kidney disease requiring hemodialysis (Dager 2018). Discontinue use in patients who develop acute renal failure.
- Valvular disease: Use is not recommended in patients with prosthetic heart valves or significant rheumatic heart disease. Avoid use of DOACs in patients with mechanical valves or with moderate to severe mitral stenosis (AHA/ACC/HRS [January 2019]). However, a DOAC may be used in patients with AF and native aortic valve disease, tricuspid valve disease, or mitral regurgitation when anticoagulation is required (AHA/ACC/HRS [January 2014, 2019]; AHA/ACC [Nishimura 2017]).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Use with caution in the elderly. Elderly patients exhibit higher rivaroxaban concentrations compared to younger patients due primarily to reduced clearance. Overall, efficacy of rivaroxaban in the elderly (≥65 years of age) was similar to that of patients <65 years of age. Both thrombotic and bleeding events were higher in the elderly; however, the risk to benefit profile was favorable among all age groups.
Dosage form specific issues:
- Lactose intolerance: May contains lactose; use is not recommended in patients with lactose or galactose intolerance (eg, Lapp lactase deficiency, glucose-galactose malabsorption).
Other warnings/precautions:
- Spinal or epidural hematoma: [US Boxed Warning]: Spinal or epidural hematomas may occur with neuraxial anesthesia (epidural or spinal anesthesia) or spinal puncture in patients who are anticoagulated; may result in long-term or permanent paralysis. The risk of spinal/epidural hematoma is increased with the use of indwelling epidural catheters, concomitant administration of other drugs that affect hemostasis (eg, nonsteroidal anti-inflammatory drugs, platelet inhibitors, other anticoagulants), in patients with a history of traumatic or repeated epidural or spinal punctures, or a history of spinal deformity or spinal surgery. Monitor for signs of neurologic impairment (eg, midline back pain, numbness/weakness of legs, bowel/bladder dysfunction); prompt diagnosis and treatment are necessary. In patients who are anticoagulated or pharmacologic thromboprophylaxis is anticipated, assess risks versus benefits prior to neuraxial interventions. The optimal timing between the administration of rivaroxaban and neuraxial procedures is not known. Placement or removal of an epidural catheter or lumbar puncture is best performed when the anticoagulant effect of rivaroxaban is low. European guidelines recommend waiting at least 22 to 26 hours following the last rivaroxaban dose when using prophylactic dosing (eg, 10 mg once daily) before catheter placement or lumbar puncture (Gogarten 2010). When higher doses are used (eg, 20 mg once daily), some suggest avoidance of neuraxial procedures for at least 48 hours (Rosencher 2013). In patients who have received neuraxial anesthesia concurrently with rivaroxaban (usually in patients undergoing knee or hip arthroplasty), avoid removal of epidural catheter for at least 18 hours following the last rivaroxaban dose; avoid rivaroxaban administration for at least 6 hours following epidural catheter removal; if traumatic puncture occurs, avoid rivaroxaban administration for at least 24 hours. In addition to these and other clinical variables, consider renal function and the age of the patient (elderly patients exhibit a prolonged rivaroxaban half-life [11 to 13 hours]) (Kubitza 2010; Rosencher 2013). The Canadian labeling recommends avoiding doses >10 mg in patients with a postoperative indwelling epidural catheter.
Monitoring Parameters
Renal function and CBC prior to initiation, when clinically indicated, and at least annually in all patients (AHA [Raval 2017]); hepatic function; signs of bleeding.
Routine coagulation testing is not required or necessary for direct oral anticoagulants (DOACs). There are currently no FDA-approved assays or calibration reagents available.
In clinical situations when assessment of the anticoagulant effect is useful (eg, acute care, periprocedural settings, absorption), evaluating a recent creatinine clearance and time since the last dose was ingested is usually sufficient for guiding clinical decisions. Most commonly used coagulation tests (PT, INR, aPTT) cannot definitively exclude the presence of clinically relevant serum concentrations. A prolonged PT suggests clinically relevant serum concentrations are present, but normal PT and aPTT values using standard reagents cannot rule out the presence of rivaroxaban. Highly sensitive reagents for PT testing may be able to exclude the presence of rivaroxaban.
If available, the preferred test to rule out clinically significant serum concentrations and quantify anticoagulant effect is anti-factor Xa activity calibrated specifically for rivaroxaban (undetectable anti-Xa activity likely excludes clinically relevant drug concentrations). An anti-factor Xa assay calibrated for low molecular weight heparin can rule out clinically relevant drug concentrations, but is not useful for quantification (ACC [Tomaselli 2017]; AHA [Raval 2017]; Leung 2019).
Pregnancy
Pregnancy Considerations
Based on ex vivo data, rivaroxaban crosses the placenta (Bapat 2015).
Information related to the use of rivaroxaban during pregnancy (Beyer-Westendorf 2016; Hoeltzenbein 2015; Königsbrügge 2014; Lameijer 2018; Myers 2016) and postpartum (Rudd 2015) is limited. Use of direct acting oral anticoagulants increases the risk of bleeding in all patients. When used in pregnancy, there is also the potential for fetal bleeding or subclinical placental bleeding which may increase the risk of miscarriage, preterm delivery, fetal compromise, or stillbirth (Cohen 2016).
Data are insufficient to evaluate the safety of direct acting oral anticoagulants during pregnancy (Bates 2012) and use in pregnant females is not recommended (Regitz-Zagrosek [ESC 2018]). Agents other than rivaroxaban are preferred for the treatment of AF or VTE in pregnant patients (Kearon 2016; Lip 2018; Regitz-Zagrosek [ESC 2018]). Patients should be switched to an alternative anticoagulant if pregnancy occurs during therapy. Fetal monitoring that includes evaluations for fetal bleeding and assessments for risk of preterm delivery are recommended if the direct acting oral anticoagulant is continued (Cohen 2016).
Until safety data are available, adequate contraception is recommended during therapy for females of childbearing potential. Females planning a pregnancy should be switched to alternative anticoagulants prior to conception (Cohen 2016).
Patient Education
What is this drug used for?
- It is used to thin the blood so that clots will not form.
- It is used to treat blood clots.
- It is used to lower the chance of heart attack, stroke, and death in some people.
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding
- Back pain
- Burning or numbness feeling
- Muscle weakness
- Paralysis
- Bladder incontinence
- Bowel incontinence
- Severe cerebrovascular disease like change in strength on one side is greater than the other, difficulty speaking or thinking, change in balance, or vision changes.
- Severe dizziness
- Passing out
- Severe loss of strength and energy
- A fall hitting head
- Severe headache
- Wound site pain
- Edema
- New drainage
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.