Boxed Warning
Cardiovascular risk:
Nonsteroidal anti-inflammatory drugs (NSAIDs) may cause an increased risk of serious cardiovascular thrombotic events, myocardial infarction (MI), and stroke, which can be fatal. This risk may increase with duration of use. Patients with cardiovascular disease or risk factors for cardiovascular disease may be at greater risk.
Salsalate is contraindicated for the treatment of perioperative pain in the setting of coronary artery bypass graft (CABG) surgery.
Gastrointestinal risk:
NSAIDs cause an increased risk of serious gastrointestinal (GI) adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients are at greater risk for serious GI events.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
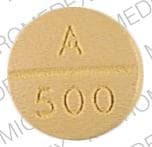
Tablet, Oral:
Disalcid: 500 mg [DSC], 750 mg [DSC]
Generic: 500 mg, 750 mg
Pharmacology
Mechanism of Action
Salsalate inhibits prostaglandin synthesis providing, anti-inflammatory effects with less inhibition of platelet aggregation than aspirin
Pharmacokinetics/Pharmacodynamics
Absorption
Complete, from small intestine; food slows absorption
Metabolism
Salsalate is partially hydrolyzed in the intestine to two moles of salicylic acid (active) and metabolites; salicylates are further metabolized in the liver
Excretion
Primarily urine
Onset of Action
Therapeutic: 3 to 4 days of continuous dosing
Half-Life Elimination
Salsalate: ~1 hour; Salicylic acid 3.5 to ≥16 hours (due to capacity limited biotransformation)
Use: Labeled Indications
Rheumatic disorders: Treatment of signs and symptoms of osteoarthritis, rheumatoid arthritis, and related rheumatic disorders
Contraindications
Hypersensitivity to salsalate or any component of the formulation; asthma, urticaria, or allergic reaction to aspirin or NSAIDs; perioperative pain in the setting of coronary artery bypass graft (CABG) surgery.
Documentation of allergenic cross-reactivity for salicylates is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Dosage and Administration
Dosing: Adult
Rheumatic disorders: Oral: Note: Use the lowest effective dose for the shortest duration; after observing the response to initial therapy, adjust dose as needed. Usual dose: 3 g per day in 2 to 3 divided doses
Dosing: Geriatric
Refer to adult dosing. May require lower dosage.
Administration
Administer with food to decrease GI distress.
Dietary Considerations
May be taken with food to decrease GI distress.
Storage
Store at 15°C to 30°C (59°F to 86°F).
Salsalate Images
Drug Interactions
Agents with Antiplatelet Properties (e.g., P2Y12 inhibitors, NSAIDs, SSRIs, etc.): May enhance the adverse/toxic effect of Salicylates. Increased risk of bleeding may result. Monitor therapy
Ajmaline: Salicylates may enhance the adverse/toxic effect of Ajmaline. Specifically, the risk for cholestasis may be increased. Monitor therapy
Ammonium Chloride: May increase the serum concentration of Salicylates. Monitor therapy
Angiotensin-Converting Enzyme Inhibitors: Salicylates may enhance the nephrotoxic effect of Angiotensin-Converting Enzyme Inhibitors. Salicylates may diminish the therapeutic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Anticoagulants: Salicylates may enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Benzbromarone: Salicylates may diminish the therapeutic effect of Benzbromarone. Monitor therapy
Blood Glucose Lowering Agents: Salicylates may enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Carbonic Anhydrase Inhibitors: Salicylates may enhance the adverse/toxic effect of Carbonic Anhydrase Inhibitors. Salicylate toxicity might be enhanced by this same combination. Management: Avoid these combinations when possible.Dichlorphenamide use with high-dose aspirin as contraindicated. If another combination is used, monitor patients closely for adverse effects. Tachypnea, anorexia, lethargy, and coma have been reported. Exceptions: Brinzolamide; Dorzolamide. Consider therapy modification
Corticosteroids (Systemic): Salicylates may enhance the adverse/toxic effect of Corticosteroids (Systemic). These specifically include gastrointestinal ulceration and bleeding. Corticosteroids (Systemic) may decrease the serum concentration of Salicylates. Withdrawal of corticosteroids may result in salicylate toxicity. Monitor therapy
Dexketoprofen: Salicylates may enhance the adverse/toxic effect of Dexketoprofen. Dexketoprofen may diminish the therapeutic effect of Salicylates. Salicylates may decrease the serum concentration of Dexketoprofen. Management: The use of high-dose salicylates (3 g/day or more in adults) together with dexketoprofen is inadvisable. Consider administering dexketoprofen 30-120 min after or at least 8 hrs before cardioprotective doses of aspirin to minimize any possible interaction. Avoid combination
Ginkgo Biloba: May enhance the anticoagulant effect of Salicylates. Management: Consider alternatives to this combination of agents. Monitor for signs and symptoms of bleeding (especially intracranial bleeding) if salicylates are used in combination with ginkgo biloba. Consider therapy modification
Herbs (Anticoagulant/Antiplatelet Properties) (eg, Alfalfa, Anise, Bilberry): May enhance the adverse/toxic effect of Salicylates. Bleeding may occur. Consider therapy modification
Hyaluronidase: Salicylates may diminish the therapeutic effect of Hyaluronidase. Management: Patients receiving salicylates (particularly at larger doses) may not experience the desired clinical response to standard doses of hyaluronidase. Larger doses of hyaluronidase may be required. Consider therapy modification
Influenza Virus Vaccine (Live/Attenuated): May enhance the adverse/toxic effect of Salicylates. Specifically, Reye's syndrome may develop. Avoid combination
Loop Diuretics: Salicylates may diminish the diuretic effect of Loop Diuretics. Loop Diuretics may increase the serum concentration of Salicylates. Monitor therapy
Methotrexate: Salicylates may increase the serum concentration of Methotrexate. Salicylate doses used for prophylaxis of cardiovascular events are not likely to be of concern. Consider therapy modification
Nonsteroidal Anti-Inflammatory Agents (Nonselective): May enhance the adverse/toxic effect of Salicylates. An increased risk of bleeding may be associated with use of this combination. Nonsteroidal Anti-Inflammatory Agents (Nonselective) may diminish the cardioprotective effect of Salicylates. Salicylates may decrease the serum concentration of Nonsteroidal Anti-Inflammatory Agents (Nonselective). Consider therapy modification
Potassium Phosphate: May increase the serum concentration of Salicylates. Monitor therapy
PRALAtrexate: Salicylates may increase the serum concentration of PRALAtrexate. Salicylate doses used for prophylaxis of cardiovascular events are unlikely to be of concern. Consider therapy modification
Probenecid: Salicylates may diminish the therapeutic effect of Probenecid. Monitor therapy
Salicylates: May enhance the anticoagulant effect of other Salicylates. Monitor therapy
Sulfinpyrazone: Salicylates may decrease the serum concentration of Sulfinpyrazone. Avoid combination
Thrombolytic Agents: Salicylates may enhance the adverse/toxic effect of Thrombolytic Agents. An increased risk of bleeding may occur. Monitor therapy
Valproate Products: Salicylates may increase the serum concentration of Valproate Products. Monitor therapy
Varicella Virus-Containing Vaccines: Salicylates may enhance the adverse/toxic effect of Varicella Virus-Containing Vaccines. Specifically, the risk for Reye's syndrome may increase. Avoid combination
Test Interactions
False results for plasma T4; salsalate is metabolized to salicylic acid; consider test interactions for salicylic acid.
Adverse Reactions
Frequency not defined.
Cardiovascular: Hypotension
Central nervous system: Vertigo
Dermatologic: Skin rash, Stevens-Johnson syndrome, toxic epidermal necrolysis, urticaria
Gastrointestinal: Abdominal pain, diarrhea, gastrointestinal hemorrhage, gastrointestinal perforation, gastrointestinal ulcer, nausea
Hematologic & oncologic: Anemia
Hepatic: Abnormal hepatic function tests, hepatitis
Hypersensitivity: Anaphylactic shock, angioedema
Otic: Auditory impairment, tinnitus
Renal: Decreased creatinine clearance, nephritis
Respiratory: Bronchospasm
Warnings/Precautions
Concerns related to adverse effects:
- Anaphylactoid reactions: Even in patients without prior exposure to salsalate, anaphylactoid reactions may occur; patients with "aspirin triad" (bronchial asthma, aspirin intolerance, rhinitis) may be at increased risk. Do not use in patients who experience bronchospasm, asthma, rhinitis, or urticaria with NSAID or aspirin therapy.
- Cardiovascular events: [U.S. Boxed Warning]: NSAIDs are associated with an increased risk of adverse cardiovascular thrombotic events, including MI and stroke. Risk may be increased with duration of use or pre-existing cardiovascular risk factors or disease. Carefully evaluate individual cardiovascular risk profiles prior to prescribing. Use caution with fluid retention or heart failure. Concurrent administration of salsalate, and potentially other nonselective NSAIDs, may interfere with aspirin’s cardioprotective effect. Use the lowest effective dose for the shortest duration of time, consistent with individual patient goals, to reduce risk of cardiovascular events; alternate therapies should be considered for patients at high risk.
- Gastrointestinal events: [U.S. Boxed Warning]: NSAIDs may increase risk of gastrointestinal irritation, inflammation, ulceration, bleeding, and perforation. These events may occur at any time during therapy and without warning. Use caution with a history of GI disease (bleeding and/or ulcers), concurrent therapy with aspirin, anticoagulants and/or corticosteroids, smoking, use of alcohol, the elderly or debilitated patients. Use the lowest effective dose for the shortest duration of time, consistent with individual patient goals, to reduce risk of GI adverse events; alternate therapies should be considered for patients at high risk. When used concomitantly with ≤325 mg of aspirin, a substantial increase in the risk of gastrointestinal complications (eg, ulcer) occurs; concomitant gastroprotective therapy (eg, proton pump inhibitors) is recommended (Bhatt, 2008).
- Hematologic effects: Platelet adhesion and aggregation may be decreased; may prolong bleeding time; patients with coagulation disorders or who are receiving anticoagulants should be monitored closely. Anemia may occur; patients on long-term NSAID therapy should be monitored for anemia.
- Hepatic effects: Severe hepatic reactions (eg, fulminant hepatitis, liver failure) have occurred with NSAID use, rarely (may be fatal); elevations of ALT or AST may occur; discontinue if signs or symptoms of liver disease develop, or if systemic manifestations occur.
- Salicylate sensitivity: Patients with sensitivity to tartrazine dyes, nasal polyps, and asthma may have an increased risk of salicylate sensitivity. Previous nonreaction does not guarantee future safe taking of medication.
- Skin reactions: NSAIDs may cause serious skin adverse events including exfoliative dermatitis, Stevens-Johnson syndrome (SJS), and toxic epidermal necrolysis (TEN); may be fatal; discontinue use at first sign of skin rash or hypersensitivity.
Disease-related concerns:
- Asthma: Do not administer to patients with aspirin-sensitive asthma; severe bronchospasm may occur. Use caution in patients with other forms of asthma.
- Coronary artery bypass graft surgery: [U.S. Boxed Warning]: Use is contraindicated for treatment of perioperative pain in the setting of coronary artery bypass graft (CABG) surgery. Risk of MI and stroke may be increased with use following CABG surgery.
- Hepatic impairment: Use with caution in patients with decreased hepatic function. Closely monitor patients with any abnormal LFT.
- Hypertension: Use with caution; may cause new-onset hypertension or worsening of existing hypertension. Response to ACE inhibitors, thiazides, or loop diuretics may be impaired with concurrent use of NSAIDs.
- Renal impairment: NSAID use may compromise existing renal function; dose-dependent decreases in prostaglandin synthesis may result from NSAID use, reducing renal blood flow which may cause renal decompensation. Patients with impaired renal function, dehydration, heart failure, liver dysfunction, those taking diuretics, and ACE inhibitors, and the elderly are at greater risk of renal toxicity. Rehydrate patient before starting therapy; monitor renal function closely. Not recommended for use in patients with advanced renal disease. Long-term NSAID use may result in renal papillary necrosis.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Pediatric: Children and teenagers who have or are recovering from chickenpox or flu-like symptoms should not use this product.
Monitoring Parameters
Signs and symptoms of GI bleeding; BP; renal function; urinary pH; plasma salicylate, CBC, and chemistry profile periodically during long term therapy.
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Adverse events have not been observed in animal reproduction studies. Due to the known effects of salicylates (closure of ductus arteriosus), use during late pregnancy should be avoided.
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience nausea. Have patient report immediately to prescriber signs of abdominal ulcers (severe abdominal or back pain; black, tarry, or bloody stools; vomiting blood or vomit that looks like coffee grounds; or weight gain or abnormal swelling), signs of bleeding (vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding), signs of kidney problems (unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain), signs of high potassium (abnormal heartbeat, confusion, dizziness, passing out, weakness, shortness of breath, numbness or tingling feeling), signs of severe cerebrovascular disease (change in strength on one side is greater than the other, difficulty speaking or thinking, change in balance, or vision changes), shortness of breath, excessive weight gain, swelling of arms or legs, chest pain, fast heartbeat, severe headache, noise or ringing in the ears, hearing loss, severe abdominal pain, severe loss of strength and energy, severe dizziness, passing out, vision changes, signs of Stevens-Johnson syndrome/toxic epidermal necrolysis (red, swollen, blistered, or peeling skin [with or without fever]; red or irritated eyes; or sores in mouth, throat, nose, or eyes), or signs of liver problems (dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin) (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for health care professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience, and judgment in diagnosing, treating, and advising patients.