What is Saxenda?
Saxenda is an injectable prescription medicine used for adults with obesity or overweight (excess weight) who also have weight related medical problems, and children aged 12 to 17 years with a body weight above 132 pounds (60 kg) and obesity to help them lose weight and keep the weight off.
- Saxenda should be used with a reduced calorie diet and increased physical activity.
- Saxenda and Victoza have the same active ingredient, liraglutide, and should not be used together or with other GLP-1 receptor agonist medicines.
- It is not known if Saxenda is safe and effective when taken with other prescription, over-the-counter medicines, or herbal weight loss products.
- It is not known if Saxenda is safe and effective in children under 12 years of age.
- It is not known if Saxenda is safe and effective in children aged 12 to 17 years with type 2 diabetes.
What is the most important information I should know about Saxenda?
Do not share your Saxenda pen with others even if the needle has been changed. You may give other people a serious infection or get a serious infection from them.
Serious side effects may happen in people who take Saxenda, including:
Possible thyroid tumors, including cancer. Tell your healthcare provider if you get a lump or swelling in your neck, hoarseness, trouble swallowing, or shortness of breath. These may be symptoms of thyroid cancer. In studies with rats and mice, Saxenda and medicines that work like Saxenda caused thyroid tumors, including thyroid cancer. It is not known if Saxenda will cause thyroid tumors or a type of thyroid cancer called medullary thyroid carcinoma (MTC) in people.
Do not use Saxenda if you or any of your family have ever had a type of thyroid cancer called medullary thyroid carcinoma (MTC), or if you have an endocrine system condition called Multiple Endocrine Neoplasia syndrome type 2 (MEN 2).
Who should not use Saxenda?
Do not use Saxenda if:
- you or any of your family have ever had a type of thyroid cancer called medullary thyroid carcinoma (MTC) or if you have an endocrine system condition called Multiple Endocrine Neoplasia syndrome type 2 (MEN 2).
- you are allergic to liraglutide or any of the ingredients in Saxenda. See the end of this Medication Guide for a complete list of ingredients in Saxenda.
- are pregnant or plan to become pregnant. Saxenda may harm your unborn baby.
What should I tell my healthcare provider before using Saxenda?
Before taking Saxenda, tell your healthcare provider about all of your medical conditions, including if you:
- are taking certain medicines called GLP-1 receptor agonists.
- have severe problems with your stomach, such as slowed emptying of your stomach (gastroparesis) or problems with digesting food.
- have or have had problems with your pancreas, kidneys or liver.
- have or have had depression or suicidal thoughts, or mental health issues.
- are breastfeeding or plan to breastfeed. It is not known if Saxenda passes into your breast milk. You and your healthcare provider should decide if you will use Saxenda or breastfeed.
Tell your healthcare provider about all the medicines you take including prescription, over-the-counter medicines, vitamins, and herbal supplements. Saxenda slows stomach emptying and can affect medicines that need to pass through the stomach quickly. Saxenda may affect the way some medicines work and some other medicines may affect the way Saxenda works.
Tell your healthcare provider if you take diabetes medicines, especially insulin and sulfonylurea medicines. Talk with your healthcare provider if you are not sure if you take any of these medicines.
How should I use Saxenda?
- Read the Instructions for Use that comes with Saxenda.
- Use Saxenda exactly as prescribed by your healthcare provider.
- Your healthcare provider should show you how to use Saxenda before you use it for the first time.
- Use Saxenda exactly as prescribed by your healthcare provider. Your dose should be increased after using Saxenda for 1 week until you reach the 3 mg dose.
- Start Saxenda with 0.6 mg per day in your first week. In your second week, increase your daily dose to 1.2 mg. In the third week, increase your daily dose to 1.8 mg. In the fourth week, increase your daily dose to 2.4 mg and in the fifth week onwards, increase your daily dose to the full dose of 3 mg. After that, do not change your dose unless your healthcare provider tells you to. Children may reduce their dose to 2.4 mg daily if the maximum dose is not tolerated.
- Saxenda is injected 1 time each day, at any time during the day.
- Inject your dose of Saxenda under the skin (subcutaneously) in your stomach area (abdomen), upper leg (thigh), or upper arm, as instructed by your healthcare provider. Do not inject into a vein or muscle.
- If you take too much Saxenda, call your healthcare provider right away. Taking too much Saxenda may cause severe nausea, severe vomiting, and low blood sugar (hypoglycemia).
- If you miss your daily dose of Saxenda, just take your next daily dose as usual on the following day. Do not take an extra dose of Saxenda or increase your dose on the following day to make up for your missed dose. If you miss your dose of Saxenda for 3 days or more, call your healthcare provider to talk about how to restart your treatment.
- You can take Saxenda with or without food.
- Throw away the used Saxenda pen after 30 days.
Your healthcare provider should start you on a reduced calorie diet and increased physical activity when you start taking Saxenda. Stay on this program while you are taking Saxenda.
What are the possible side effects of Saxenda?
Saxenda may cause serious side effects, including:
- See “What is the most important information I should know about Saxenda?”
- inflammation of the pancreas (pancreatitis). Stop using Saxenda and call your healthcare provider right away if you have severe pain in your stomach area (abdomen) that will not go away, with or without vomiting. You may feel the pain from your stomach area (abdomen) to your back.
- gallbladder problems. Saxenda may cause gallbladder problems including gallstones. Some gallbladder problems need surgery. Call your healthcare provider if you have any of the following symptoms:
- pain in your upper stomach (abdomen)
- fever
- yellowing of your skin or eyes (jaundice)
- clay-colored stools
- increased risk of low blood sugar (hypoglycemia) in adults with type 2 diabetes mellitus who also take medicines to treat type 2 diabetes mellitus such as sulfonylureas or insulin.
- risk of low blood sugar (hypoglycemia) in children who are 12 years of age and older without type 2 diabetes mellitus
- Signs and symptoms of low blood sugar may include:
- shakiness
- sweating
- headache
- drowsiness
- weakness
- dizziness
- confusion
- irritability
- hunger
- fast heartbeat
- feeling jittery
Talk to your healthcare provider about how to recognize and treat low blood sugar. You should check your blood sugar before you start taking Saxenda and while you take Saxenda
- increased heart rate. Saxenda can increase your heart rate while you are at rest. Your healthcare provider should check your heart rate while you take Saxenda. Tell your healthcare provider if you feel your heart racing or pounding in your chest and it lasts for several minutes.
- kidney problems (kidney failure). Saxenda may cause nausea, vomiting or diarrhea leading to loss of fluids (dehydration). Dehydration may cause kidney failure which can lead to the need for dialysis. This can happen in people who have never had kidney problems before. Drinking plenty of fluids may reduce your chance of dehydration.
Call your healthcare provider right away if you have nausea, vomiting, or diarrhea that does not go away, or if you cannot drink liquids by mouth. - serious allergic reactions. Stop using Saxenda, and get medical help right away if you have any symptoms of a serious allergic reaction including:
- swelling of your face, lips, tongue, or throat
- fainting or feeling dizzy
- very rapid heartbeat
- problems breathing or swallowing
- severe rash or itching
- depression or thoughts of suicide. You should pay attention to any mental changes, especially sudden changes, in your mood, behaviors, thoughts, or feelings. Call your healthcare provider right away if you have any mental changes that are new, worse, or worry you.
The most common side effects of Saxenda in adults* include:- nausea
- diarrhea
- constipation
- vomiting
- injection site reaction
- low blood sugar (hypoglycemia)
- headache
- upset stomach (dyspepsia)
- tiredness (fatigue)
- dizziness
- stomach pain
- change in enzyme (lipase) levels in your blood
*additional common side effects in children are fever and gastroenteritis
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of Saxenda. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Keep your Saxenda pen, pen needles, and all medicines out of the reach of children.
General information about the safe and effective use of Saxenda
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use Saxenda for a condition for which it was not prescribed. Do not give Saxenda to other people, even if they have the same symptoms that you have. It may harm them.
You can ask your pharmacist or healthcare provider for information about Saxenda that is written for health professionals.
How should I store Saxenda?
- Store your new, unused Saxenda pens in the refrigerator at 36°F to 46°F (2°C to 8°C).
- Store your pen in use for 30 days at 59ºF to 86ºF (15ºC to 30ºC) or in a refrigerator at 36°F to 46°F (2°C to 8°C).
- The Saxenda pen you are using should be thrown away after 30 days, even if it still has Saxenda left in it.
- Do not freeze Saxenda. Do not use Saxenda if it has been frozen.
- Unused Saxenda pens may be used until the expiration date printed on the label, if kept in the refrigerator.
- Keep Saxenda away from heat and out of the light.
What are the ingredients in Saxenda?
Active ingredient: liraglutide
Inactive ingredients: disodium phosphate dihydrate, propylene glycol, phenol and water for injection
For information about Saxenda go to www.SAXENDA.com or contact: Novo Nordisk Inc 1-844-363-4448
Instructions for use for Saxenda
- Read these instructions carefully before using your Saxenda pen.
- Do not use your pen without proper training from your healthcare provider. Make sure that you know how to give yourself an injection with the pen before you start your treatment.
- Warning - If you are blind or have poor eyesight and cannot read the dose counter on the pen, do not use this pen without help. Get help from a person with good eyesight who is trained to use the Saxenda pen.
- You can refresh your training at any time by watching the online training video at WWW.SAXENDA.COM.
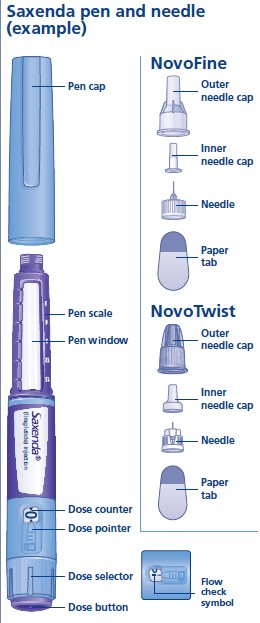
- Start by checking your pen to make sure that it contains Saxenda, then look at the pictures below to get to know the different parts of your pen and needle.
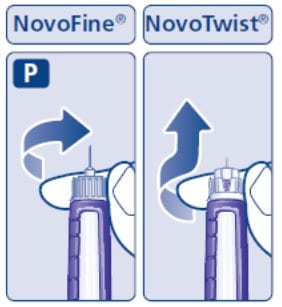
Your pen is a prefilled, dial-a-dose, single-patient-use pen. It contains 18 mg of liraglutide, and you can select doses of 0.6 mg, 1.2 mg, 1.8 mg, 2.4 mg and 3 mg. Your pen is made to be used with NovoFine or NovoTwist disposable needles up to a length of 8 mm. Pen needles are not included with your Saxenda pen.
Step 1. Prepare your pen with a new needle
- Wash your hands with soap and water.
- Check the name and colored label of your pen, to make sure that it contains Saxenda. This is especially important if you take more than 1 type of medicine.
- Pull off the pen cap.
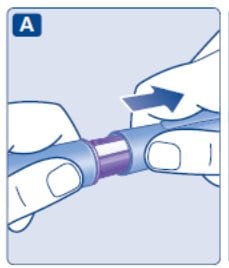
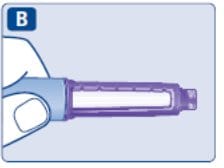
- Check that Saxenda in your pen is clear and colorless.
Look through the pen window. If Saxenda looks cloudy, do not use the pen.
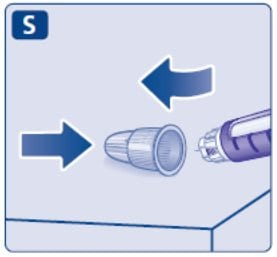
- Take a new needle, and tear off the paper tab.
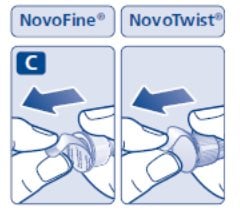
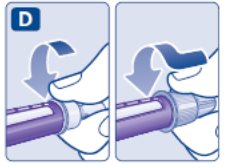
- Push the needle straight onto the pen. Turn until it is on tight.
- Pull off the outer needle cap. Do not throw it away.
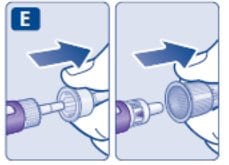
- Pull off the inner needle cap and throw it away.
A drop of Saxenda may appear at the needle tip. This is normal, but you must still check the Saxenda flow, if you use a new pen for the first time.
Warning. Always use a new needle for each injection.
This will prevent contamination, infection, leakage of Saxenda, and blocked needles leading to the wrong dose.
Never use a bent or damaged needle.
Do not attach a new needle to your pen until you are ready to take your injection.
Step 2. Check the Saxenda flow with each new pen.
- Check the Saxenda flow before your first injection with each new pen.
If your Saxenda pen is already in use, go to Step 3 “Select your dose”. - Turn the dose selector until the dose counter shows the flow check symbol.

- Hold the pen with the needle pointing up.
Press and hold in the dose button until the dose counter shows 0. The 0 must line up with the dose pointer.
A drop of Saxenda will appear at the needle tip. - If no drop appears, repeat Step 2 above as shown in Figures G and H up to 6 times. If there is still no drop, change the needle and repeat Step 2 as shown in Figures G and H 1 more time.
Do not use the pen if a drop of Saxenda still does not appear. Contact Novo Nordisk at 1-844-363-4448.
Always make sure that a drop appears at the needle tip before you use a new pen for the first time. This makes sure that Saxenda flows.
If no drop appears, you will not inject any Saxenda, even though the dose counter may move. This may mean that there is a blocked or damaged needle.
A small drop may remain at the needle tip, but it will not be injected.
Only check the Saxenda flow before your first injection with each new pen.

Step 3. Select your dose
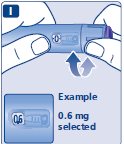
- Turn the dose selector until the dose counter shows your dose (0.6 mg, 1.2 mg, 1.8 mg, 2.4 mg or 3 mg).
Make sure you know the dose of Saxenda you should use.
If you select the wrong dose, you can turn the dose selector forward or backwards to the correct dose.
Always use the dose counter and the dose pointer to see how many mg you select.
You will hear a “click” every time you turn the dose selector. Do not set the dose by counting the number of clicks you hear.
Do not use the pen scale to set the dose. It does not show exactly how much Saxenda is left in your pen.
Only doses of 0.6 mg, 1.2 mg, 1.8 mg, 2.4 mg or 3 mg can be selected with the dose selector. The selected dose must line up exactly with the dose pointer to make sure that you get a correct dose.
The dose selector changes the dose. Only the dose counter and dose pointer will show how many mg you select for each dose.
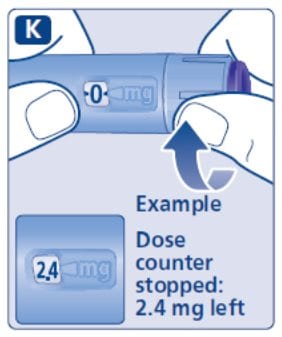
You can select up to 3 mg each dose. When your pen contains less than 3 mg the dose counter stops before 3 mg is shown.
The dose selector clicks differently when turned forward, backwards or past the number of mg left. Do not count the pen clicks.
 How much Saxenda is left?
How much Saxenda is left?
- The pen scale shows you about how much Saxenda is left in your pen.
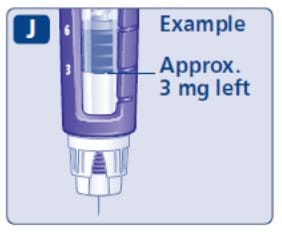
- To see how much Saxenda is left, use the dose counter:
Turn the dose selector until the dose counter stops.
If it shows 3, at least 3 mg are left in your pen. If the dose counter stops before 3 mg, there is not enough Saxenda left for a full dose of 3 mg.
If you need more Saxenda than what is left in your pen:
Only if trained or told by your healthcare provider, you may split your dose between your current pen and a new pen. Use a calculator to plan the doses as instructed by your healthcare provider.
Be very careful to calculate correctly.
If you are not sure how to split your dose using 2 pens, then select and inject the dose you need with a new pen.
Step 4. Inject your dose
- Insert the needle into your skin as your healthcare provider has shown you.
- Make sure you can see the dose counter. Do not cover it with your fingers. This could stop the injection.
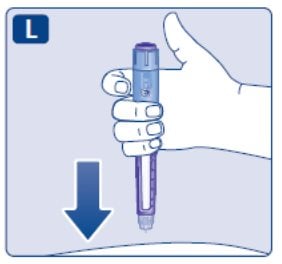
- Press and hold down the dose button until the dose counter shows 0. The 0 must line up with the dose pointer. You may then hear or feel a click.

- Keep the needle in your skin after the dose counter has returned to 0 and count slowly to 6.
- If the needle is removed earlier, you may see a stream of Saxenda coming from the needle tip. If this happens, the full dose will not be delivered.

- Remove the needle from your skin.
If blood appears at the injection site, press lightly. Do not rub the area.
Always watch the dose counter to know how many mg you inject. Hold the dose button down until the dose counter shows 0.
How to identify a blocked or damaged needle?
- If 0 does not appear in the dose counter after continuously pressing the dose button, you may have used a blocked or damaged needle.
- If this happens you have not received any Saxenda even though the dose counter has moved from the original dose that you have set.
How to handle a blocked needle?
Change the needle as described in Step 5, and repeat all steps starting with Step 1: “Prepare your pen with a new needle”.
Make sure you select the full dose you need.
Never touch the dose counter when you inject. This can stop the injection.
You may see a drop of Saxenda at the needle tip after injecting. This is normal and does not affect your dose.
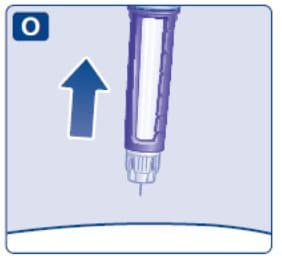
Step 5. After your injection
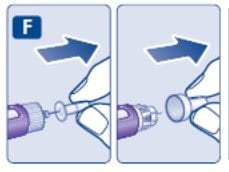
- Carefully remove the needle from the pen. Do not put the needle caps back on the needle, to avoid needle sticks.
- Place the needle in a sharps container right away to reduce the risk of needle sticks.

- Put the pen cap on your pen after each use to protect Saxenda from light.
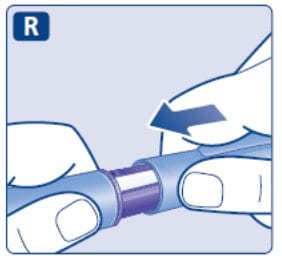
If you do not have a sharps container, follow a 1-handed needle recapping method. Carefully slip the needle into the outer needle cap. Dispose of the needle in a sharps container as soon as possible.
Never try to put the inner needle cap back on the needle. You may stick yourself with the needle.
Always remove the needle from your pen. This prevents contamination, infection, leakage of Saxenda, and blocked needles leading to the wrong dose. If the needle is blocked, you will not inject any Saxenda.
Always dispose of the needle after each injection.
- Do not throw away in the household trash. Put the needle and any empty Saxenda pen or any pen used for 30 days still containing Saxenda in a FDA-cleared sharps disposal container right away after use.
- If you do not have a FDA-cleared sharps disposal container, you may use a household container that is:
- made of a heavy-duty plastic
- can be closed with a tight-fitting, puncture-resistant lid, without sharps being able to come out upright and stable during use
- leak-resistant
- properly labeled to warn of hazardous waste inside the container
- When your sharps disposal container is almost full, you will need to follow your community guidelines for the right way to dispose of your sharps disposal container. There may be state or local laws about how you should throw away used needles and syringes. For more information about the safe sharps disposal, and for specific information about sharps disposal in the state that you live in, go to the FDA’s website at: HTTP://WWW.FDA.GOV/SAFESHARPSDISPOSAL
- Do not dispose of your used sharps disposal container in your household trash unless your community guidelines permit this. Do not recycle your used sharps disposal container.
- Safely dispose of Saxenda that is out of date or no longer needed.
 Important
Important
- Caregivers must be very careful when handling used needles to prevent needle sticks and cross infection.
- Never use a syringe to withdraw Saxenda from your pen.
- Always carry an extra pen and new needles with you, in case of loss or damage.
- Always keep your pen and needles out of reach of others, especially children.
- Do not share your Saxenda pen or needles with anyone else. You may give an infection to them or get an infection from them.
- Always keep your pen with you. Do not leave it in a car or other place where it can get too hot or too cold.
Caring for your pen
- Do not drop your pen or knock it against hard surfaces. If you drop it or suspect a problem, attach a new needle and check the Saxenda flow before you inject.
- Do not try to repair your pen or pull it apart.
- Do not expose your pen to dust, dirt or liquid.
- Do not wash, soak, or lubricate your pen. If necessary, clean it with mild detergent on a moistened cloth.
How should I store my Saxenda pen?
- Store your new, unused Saxenda pens in the refrigerator at 36°F to 46°F (2°C to 8°C).
- Store your pen in use for 30 days at 59ºF to 86ºF (15ºC to 30ºC) or in a refrigerator at 36°F to 46°F (2°C to 8°C).
- The Saxenda pen you are using should be thrown away after 30 days, even if it still has Saxenda left in it.
- Do not freeze Saxenda. Do not use Saxenda if it has been frozen.
- Unused Saxenda pens may be used until the expiration date printed on the label, if kept in the refrigerator.
- Keep Saxenda away from heat and out of the light.




