Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Powder, Oral:
Generic: (1 g, 120 g, 454 g, 500 g, 1000 g, 2500 g, 10000 g, 12000 g, 25000 g, 45000 g)
Solution, Intravenous:
Neut: 4% (5 mL)
Generic: 4.2% (5 mL, 10 mL); 7.5% (50 mL); 8.4% (10 mL, 50 mL)
Solution, Intravenous [preservative free]:
Generic: 4.2% (5 mL); 8.4% (50 mL)
Tablet, Oral:
Generic: 325 mg, 650 mg
Pharmacology
Mechanism of Action
Dissociates to provide bicarbonate ion which neutralizes hydrogen ion concentration and raises blood and urinary pH
Neutralizing additive (dental use): Increases pH of lidocaine and epinephrine solution to improve tolerability and increase tissue uptake
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Well absorbed
Excretion
Urine (<1%)
Onset of Action
Oral: 15 minutes; IV: Rapid
Duration of Action
Oral: 1 to 3 hours; IV: 8 to 10 minutes
Use: Labeled Indications
Management of metabolic acidosis; gastric hyperacidity; alkalinization of the urine; treatment of hyperkalemia; management of overdose of certain drugs, including tricyclic antidepressants and aspirin
Neutralizing additive (dental use): Improves onset of analgesia and reduces injection site pain by adjusting lidocaine with epinephrine solution to a more physiologic pH.
Use: Off Label
Contrast-induced nephropathy (CIN) (prevention)byes
Evidence from controlled trials supports the use of isotonic sodium bicarbonate as an effective option in the prevention of contrast-induced nephropathy (CIN), demonstrating reduced incidence compared to sodium chloride Merten 2004, Ozcan 2007. However, meta-analyses have found effectiveness of sodium bicarbonate to be uncertain and noted that study heterogeneity and publication bias are substantial Brar 2009, Zoungas 2009. In addition, a double-blind, randomized trial in patients at high risk for renal complications found no benefit with IV sodium bicarbonate over IV sodium chloride Weisbord 2018.
Kidney Disease Improving Global Outcomes (KDIGO) guidelines state that in patients at increased risk of contrast-induced acute kidney injury (CI-AKI), IV volume expansion with either isotonic sodium chloride or isotonic sodium bicarbonate solutions is recommended rather than no IV volume expansion. Isotonic sodium bicarbonate is not commercially available, and thus carries a risk for compounding error during preparation. Based on the potential for harm and additional burden of preparing bicarbonate solutions, no preference is given to one solution; either agent can be used, with ease of use recognized for isotonic saline (KDIGO 2012a). European Society of Urogenital Radiology (ESUR) Contrast Media Safety Committee guidelines state that IV isotonic sodium bicarbonate appears to provide protection equal or superior to IV isotonic saline, but either regimen may be used (ESUR [Stacul 2011]).
Contraindications
Alkalosis, hypernatremia, severe pulmonary edema, hypocalcemia, unknown abdominal pain
Neutralizing additive (dental use): Not for use as a systemic alkalizer
Dosage and Administration
Dosing: Adult
Note: 1 mEq NaHCO3 is equivalent to 84 mg; each g of NaHCO3 provides ~12 mEq each of sodium and bicarbonate ions. Each oral tablet (650 mg) contains 7.7 mEq each of sodium and bicarbonate ions.
Cardiac arrest (ACLS 2010): IV: Initial: 1 mEq/kg/dose; repeat doses should be guided by arterial blood gases
Routine use of NaHCO3is not recommended. May be considered in the setting of prolonged cardiac arrest only after adequate alveolar ventilation has been established and effective cardiac compressions. Note: In some cardiac arrest situations (eg, metabolic acidosis, hyperkalemia, or tricyclic antidepressant overdose), sodium bicarbonate may be beneficial.
Metabolic acidosis in patients with chronic kidney disease: Oral (off-label): Note: KDIGO guidelines suggest oral replacement when plasma HCO3- concentrations are <22 mEq/L (KDIGO 2013).
Initial: 15.4 to 23.1 mEq/day in divided doses (eg, 650 mg tablet 2 to 3 times daily); titrate to normal serum bicarbonate concentrations (eg, 23 to 29 mEq/L) or up to 5850 mg/day; baking soda may be used as an alternative in patients who cannot take tablets (Chen 2014; KDIGO 2013; Kovesdy 2009; Raphael 2016). Avoid exceeding serum bicarbonate concentrations >32 mEq/L since this has been associated with increased mortality in patients with CKD (Navaneethan 2011).
Metabolic acidosis: IV: Dosage should be based on the following formula if blood gases and pH measurements are available:
HCO3-(mEq) = 0.5 x weight (kg) x [24 - serum HCO3-(mEq/L)] or HCO3-(mEq) = 0.5 x weight (kg) x [desired increase in serum HCO3-(mEq/L)]
Administer 1/2 dose initially, then remaining 1/2 dose over the next 24 hours; monitor pH, serum HCO3-, and clinical status. Note: These equations provide an estimated replacement dose. The underlying cause and degree of acidosis may result in the need for larger or smaller replacement doses. In most cases, the initial goal of therapy is to target a pH of ~7.2 and a plasma bicarbonate level of ~10 mEq/L to prevent over alkalinization. According to the ARDSNet protocol, if pH remains <7.15 after ventilator adjustments, may give NaHCO3 (Brower 2004).
If acid-base status is not available: 2 to 5 mEq/kg IV infusion over 4 to 8 hours; subsequent doses should be based on patient's acid-base status.
Hyperkalemia (ACLS 2010): IV: 50 mEq over 5 minutes (as appropriate, consider methods of enhancing potassium removal/excretion)
Renal tubular acidosis: Oral:
Distal: 0.5 to 2 mEq/kg/day in 4 to 5 divided doses
Proximal: Initial: 5 to 10 mEq/kg/day; maintenance: Increase as required to maintain serum bicarbonate in the normal range
Urine alkalinization: Oral: Initial: 48 mEq (4 g), then 12 to 24 mEq (1 to 2 g) every 4 hours; dose should be titrated to desired urinary pH; doses up to 16 g/day (200 mEq) in patients <60 years and 8 g (100 mEq) in patients >60 years. Administration of 48 mEq (4 g) every 8 hours for a total daily dose of 144 mEq (12 g) has also been shown to achieve a urinary pH of at least 7 after a period of 10 hours in one study of healthy volunteers (Cohen 2013). Note: Intravenous administration is preferred in specific overdoses (eg, salicylate) with a target urinary pH of 7.5 to 8.5 (Levine 2011; Proudfoot 2004).
Antacid: Oral: 325 mg to 2 g 1 to 4 times/day
Neutralize lidocaine with epinephrine dental anesthetic: Neutralizing additive: Mix 10 parts anesthetic (lidocaine with epinephrine) to 1 part 8.4% sodium bicarbonate
Add 0.18 mL sodium bicarbonate to 1.8 mL cartridge of lidocaine 2% with epinephrine 1:50,000 or 1:100,000
Add 2 mL sodium bicarbonate to 20 mL vial of lidocaine 2% with epinephrine 1:100,000
Add 3 mL sodium bicarbonate to 30 mL vial of lidocaine 2% with epinephrine 1:100,000
Add 5 mL sodium bicarbonate to 50 mL vial of lidocaine 2% with epinephrine 1:100,000
Prevention of contrast-induced nephropathy (off-label use): IV infusion: 154 mEq/L sodium bicarbonate in D5W solution: 3 mL/kg/hour for 1 hour immediately before contrast injection, then 1mL/kg/hour during contrast exposure and for 6 hours after procedure (Merten 2004). Some have described a prophylactic strategy based on patient risk for contrast induced nephropathy and procedure type (Goldfarb 2009). Note: In patients at high risk for renal complications, no benefit was seen with IV sodium bicarbonate over IV sodium chloride in one study; therefore, some consider IV sodium chloride as the preferred option due to lower cost and no need for compounding (Rosner 2018; Weisbord 2018).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Dose should be individualized to patient response and target parameters for condition being treated.
Antacid: Note: Chronic antacid therapy not recommended for management of GERD in pediatric patients (AAP [Lightdale 2013]; NASPGHAN/ESPGHAN [Vandenplas 2009]). Children ≥5 years and Adolescents: Oral powder: Oral: 1/2 teaspoonful/dose; may repeat up to every 2 hours not to exceed 7 doses in 24 hours, and do not use longer than 2 weeks
Cardiac arrest (PALS guidelines): Infants, Children, and Adolescents: IV, Intraosseous: 1 mEq/kg/dose; repeat doses should be guided by arterial blood gases; in infants and children <2 years of age, the 4.2% (0.5 mEq/mL) solution should be used. Note: If intraosseous route is used for administration and is subsequently used to obtain blood samples for acid-base analysis, results will be inaccurate (AHA [Kleinman 2010).
Note: Routine use of sodium bicarbonate (NaHCO3) is not recommended. May be considered in the setting of prolonged cardiac arrest only after adequate alveolar ventilation has been established and effective cardiac compressions. Note: In some cardiac arrest situations (eg, metabolic acidosis, hyperkalemia, or tricyclic antidepressant overdose), sodium bicarbonate may be beneficial (AHA [Kleinman 2010).
Chronic kidney disease (CKD) acidosis: Limited data available: Note: Initiate if serum bicarbonate <22 mEq/L (KDIGO 2012): Infants, Children, and Adolescents: Oral: Initial dose based on serum bicarbonate levels (see following equation); may divide dose for tolerability (Kraut 2011); adjust dose to maintain serum bicarbonate within the targeted normal range (eg, children: 22 to 23 mEq/L; adults: 24 to 25 mEq/L); undertreatment should be avoided due to negative effects of acidosis on growth (KDIGO 2012)
HCO3-(mEq) = 0.5 x weight (kg) x [desired HCO3- (mEq/L) - serum HCO3-(mEq/L)]
Hyperkalemia; adjunct: Limited data available; efficacy results variable: Infants, Children, and Adolescents: IV: 1 to 2 mEq/kg/dose has been used to redistribute extracellular potassium into cells based on physiologic understanding (Hegenbarth 2008); however, some data has shown efficacy lacking for use in acute, early treatment of hyperkalemia (ie, 60 minutes); in adult dialysis patients, while short infusions were shown to increase serum bicarbonate, they were not shown to reduce serum potassium (Ahee 2000; Blumberg 1988; Gutierrez 1991; Kim 1996; Weisberg 2008); some efficacy was observed with a long duration hypertonic bicarbonate infusion (eg, 150 mEq/L in D5W) used as rehydration fluid and/or in presence of metabolic acidosis (Weiner 1998; Weisberg 2008); serum Na should also be monitored closely
Metabolic acidosis, acute: Infants, Children, and Adolescents:
Blood-gas directed dosing (equations): IV: These equations provide an estimated replacement dose. The underlying cause and degree of acidosis may result in the need for larger or smaller replacement doses. In most cases, the initial goal of therapy is to target a pH of ~7.2 to prevent overalkalinization (Androgue 2006; Furhman 2011).
HCO3-(mEq) = 0.3 x weight (kg) x base deficit (mEq/L) or
HCO3-(mEq) = 0.5 x weight (kg) x [24 - serum HCO3-(mEq/L)]
Administer 1/2 calculated dose initially, then remaining 1/2 dose over the next 24 hours; monitor pH, serum HCO3-, and clinical status
Weight-directed dosing (if acid-base status is not available): Infants, Children, and Adolescents: IV, Intraosseous: 1 to 2 mEq/kg/dose (Hegenbarth 2008), in older Children (>2 years) and Adolescents: 2 to 5 mEq/kg IV infusion over 4 to 8 hours; subsequent doses should be based on patient's acid-base status
Neutralization local (dental) anesthetic (lidocaine with epinephrine): Neutralizing additive: Mix 10 parts anesthetic (lidocaine with epinephrine) to 1 part 8.4% sodium bicarbonate
Add 0.18 mL sodium bicarbonate to 1.8 mL cartridge of lidocaine 2% with epinephrine 1:50,000 or 1:100,000
Add 2 mL sodium bicarbonate to 20 mL vial of lidocaine 2% with epinephrine 1:100,000
Add 3 mL sodium bicarbonate to 30 mL vial of lidocaine 2% with epinephrine 1:100,000
Add 5 mL sodium bicarbonate to 50 mL vial of lidocaine 2% with epinephrine 1:100,000
Renal tubular acidosis (RTA): Limited data available: Note: Dose should be individualized based on urinary bicarbonate excretion (degree depends on type of RTA), serum bicarbonate, and possibly age-related factors; undertreatment should be avoided due to negative effects of acidosis on growth (KDIGO 2012)
Distal; type 1: Dose requirements may vary with age; some data suggests infants and children <6 years require higher daily dose than older children (Rodriguez-Soriano 1982); daily dose should replace urinary excretion and endogenous production (McSherry 1972, Rodriguez-Soriano 1982)
Infants: Oral: Usual range: 5 to 8 mEq/kg/day (Rodriguez-Soriano 2002); reported range: 3.9 to 10 mEq/kg/day (Rodriguez-Soriano 1982)
Children and Adolescents: Oral: Initial: At least 3 mEq/kg/day; usual initial range: 3 to 4 mEq/kg/day; titrate as necessary (Rodriguez-Soriano 1982, Rodriguez-Soriano 2002, Santos 1986)
Proximal, type 2: Infants, Children, and Adolescents: Oral: Initial: 5 to 10 mEq/kg/day in divided doses; usual range: 10 to 20 mEq/kg/day; titrate as necessary to target serum bicarbonate (Chan 2001; Rodriguez-Soriano 2002)
Skin protectant; relief of minor irritation: Note: Notify physician if no symptom resolution within 7 days, or if symptoms reappear after an initial resolution. Children ≥2 years and Adolescents: Topical: Oral powder (baking soda):
Bath soak: Dissolve 1 to 2 cups in tub of warm water, soak for 10 to 30 minutes; pat skin dry
Compress or wet dressing: Mix powder with water; soak clean soft cloth with mixture, apply cloth loosely to affected area for 15 to 30 minutes; may repeat as needed or as directed by physician.
Paste: Mix powder with water to form a paste, apply to the affected area of skin as needed
Tricyclic antidepressant (TCA, Na channel blocker), overdose: Limited data available: Infants, Children, and Adolescents: IV, Intraosseous: 1 to 2 mEq/kg/dose; titrate to maintain serum pH 7.45 to 7.55, follow with 150 mEq NaHCO3/L infusion to maintain targeted pH (Hegenbarth 2008)
Reconstitution
Prevention of contrast-induced nephropathy (off-label use): Remove 154 mL from 1000 mL bag of D5W; replace with 154 mL of 8.4% sodium bicarbonate; resultant concentration is 154 mEq/L (Merten 2004); more practically, institutions may remove 150 mL from 1000 mL bag of D5W and replace with 150 mL of 8.4% sodium bicarbonate; resultant concentration is 150 mEq/L
Neutralizing additive (dental use): Add specified volume of 8.4% sodium bicarbonate directly with lidocaine and epinephrine injection and mix; use immediately after mixing.
Administration
IV: For direct IV infusion in emergencies, administer slowly; for infusion, dilute to a maximum concentration of 0.5 mEq/mL in dextrose solution and infuse over at least 2 hours (maximum rate of administration: 1 mEq/kg/hour).
Vesicant (at concentrations ≥8.4%); ensure proper needle or catheter placement prior to and during IV infusion. Avoid extravasation.
Extravasation management: If extravasation occurs, stop infusion immediately and disconnect (leave needle/cannula in place); gently aspirate extravasated solution (do NOT flush the line); initiate hyaluronidase antidote; remove needle/cannula; apply dry cold compresses (Hurst 2004; Reynolds 2014); elevate extremity.
Hyaluronidase: Intradermal or SubQ: Inject a total of 1 to 1.7 mL (15 units/mL) as five separate 0.2 to 0.3 mL injections (using a 25-gauge needle) into area of extravasation at the leading edge in a clockwise manner (Reynolds 2014).
Oral product should be administered 1 to 3 hours after meals.
Infiltration (dental use; Onpharma): Add specified volume of 8.4% sodium bicarbonate directly with lidocaine and epinephrine injection and mix; use immediately after mixing.
Dietary Considerations
Some products may contain sodium. Oral product should be taken 1 to 3 hours after meals.
Storage
Store injection at room temperature. Protect from heat and from freezing. Use only clear solutions.
Neutralizing additive (dental use): Store at 20°C to 25°C (68°F to 77°F).
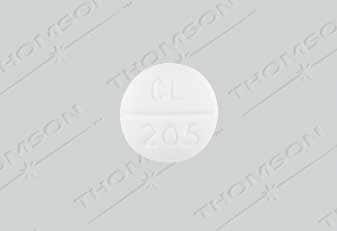
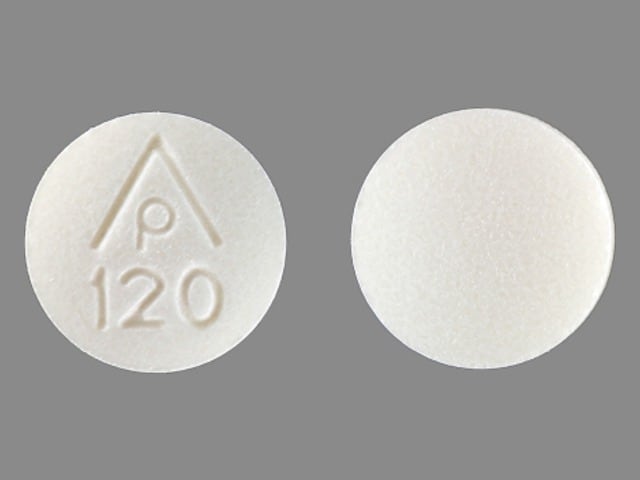
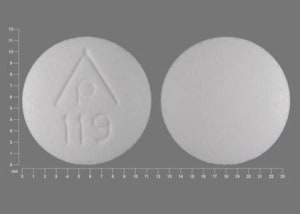
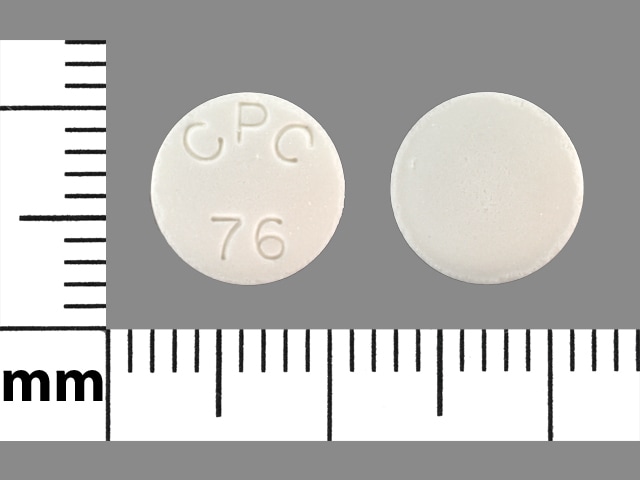
Sodium Bicarbonate Images
Drug Interactions
Acalabrutinib: Antacids may decrease the serum concentration of Acalabrutinib. Management: Separate administration of acalabrutinib from the administration of any antacids by at least 2 hours in order to minimize the potential for a significant interaction. Consider therapy modification
AcetaZOLAMIDE: May enhance the adverse/toxic effect of Sodium Bicarbonate. Specifically, the risk of renal calculus formation may be increased. Monitor therapy
Alpha-/Beta-Agonists (Indirect-Acting): Alkalinizing Agents may increase the serum concentration of Alpha-/Beta-Agonists (Indirect-Acting). Monitor therapy
Amantadine: Alkalinizing Agents may increase the serum concentration of Amantadine. Monitor therapy
Amphetamines: Alkalinizing Agents may decrease the excretion of Amphetamines. Management: Consider alternatives to using amphetamines and alkalinizing agents in combination. If these agents must be used together, patients should be monitored closely for excessive amphetamine effects. Consider therapy modification
Antipsychotic Agents (Phenothiazines): Antacids may decrease the absorption of Antipsychotic Agents (Phenothiazines). Monitor therapy
Atazanavir: Antacids may decrease the absorption of Atazanavir. Consider therapy modification
Bisacodyl: Antacids may diminish the therapeutic effect of Bisacodyl. Antacids may cause the delayed-release bisacodyl tablets to release drug prior to reaching the large intestine. Gastric irritation and/or cramps may occur. Consider therapy modification
Bismuth Subcitrate: Antacids may diminish the therapeutic effect of Bismuth Subcitrate. Management: Avoid administration of antacids within 30 minutes of bismuth subcitrate (tripotassium bismuth dicitrate) administration. Consider therapy modification
Bosutinib: Antacids may decrease the serum concentration of Bosutinib. Management: Administer antacids more than 2 hours before or after bosutinib. Consider therapy modification
Bromperidol: Antacids may decrease the absorption of Bromperidol. Monitor therapy
Calcium Polystyrene Sulfonate: Antacids may enhance the adverse/toxic effect of Calcium Polystyrene Sulfonate. The combined use of these two agents may result in metabolic alkalosis and/or loss of efficacy of the cation exchange resin. Management: To minimize this interaction, consider: a)separating doses by 2 or more hours; b)rectal administration of the exchange resin; or c)alternatives to antacids. Monitor for metabolic alkalosis and attenuation of CPS effects. Avoid magnesium hydroxide. Consider therapy modification
Captopril: Antacids may decrease the serum concentration of Captopril. Monitor therapy
Cefditoren: Antacids may decrease the serum concentration of Cefditoren. Management: Concomitant use of cefditoren with antacids is not recommended. Consider alternative methods to control acid reflux (eg, diet modification) or alternative antimicrobial therapy. If antacid therapy can not be avoided, separate dosing by several hours. Consider therapy modification
Cefpodoxime: Antacids may decrease the serum concentration of Cefpodoxime. Monitor therapy
Cefuroxime: Antacids may decrease the serum concentration of Cefuroxime. Management: Administer cefuroxime axetil at least 1 hour before or 2 hours after the administration of short-acting antacids. Consider therapy modification
Chloroquine: Antacids may decrease the serum concentration of Chloroquine. Management: Separate administration of antacids and chloroquine by at least 4 hours to minimize any potential negative impact of antacids on chloroquine bioavailability. Consider therapy modification
Corticosteroids (Oral): Antacids may decrease the bioavailability of Corticosteroids (Oral). Management: Consider separating doses by 2 or more hours. Budesonide enteric coated tablets could dissolve prematurely if given with drugs that lower gastric acid, with unknown impact on budesonide therapeutic effects. Consider therapy modification
Cysteamine (Systemic): Antacids may diminish the therapeutic effect of Cysteamine (Systemic). Monitor therapy
Dabigatran Etexilate: Antacids may decrease the serum concentration of Dabigatran Etexilate. Management: Dabigatran etexilate Canadian product labeling recommends avoiding concomitant use with antacids for 24 hours after surgery. In other situations, administer dabigatran etexilate 2 hours prior to antacids. Monitor clinical response to dabigatran therapy. Consider therapy modification
Dasatinib: Antacids may decrease the serum concentration of Dasatinib. Management: Simultaneous administration of dasatinib and antacids should be avoided. Administer antacids 2 hours before or 2 hours after dasatinib. Consider therapy modification
Delavirdine: Antacids may decrease the serum concentration of Delavirdine. Management: Separate doses of delavirdine and antacids by at least 1 hour. Monitor for decreased delavirdine therapeutic effects with this combination. Consider therapy modification
Dexmethylphenidate: Antacids may increase the absorption of Dexmethylphenidate. Specifically, antacids may interfere with the normal release of drug from the extended-release capsules (Focalin XR brand), which could result in both increased absorption (early) and decreased delayed absorption. Monitor therapy
Elvitegravir: Antacids may decrease the serum concentration of Elvitegravir. Management: Separate administration of antacids and elvitegravir-containing products by at least 2 hours in order to minimize the risk for an interaction. Consider therapy modification
Erlotinib: Antacids may decrease the serum concentration of Erlotinib. Management: Separate the administration of erlotinib and any antacid by several hours in order to minimize the risk of a significant interaction. Consider therapy modification
Flecainide: Sodium Bicarbonate may diminish the arrhythmogenic effect of Flecainide. Sodium Bicarbonate may increase the serum concentration of Flecainide. Monitor therapy
Fosinopril: Antacids may decrease the serum concentration of Fosinopril. Management: The US and Canadian fosinopril manufacturer labels recommend separating the doses of antacids and fosinopril by 2 hours. Consider therapy modification
Gefitinib: Antacids may decrease the serum concentration of Gefitinib. Management: Administer gefitinib at least 6 hours before or after administration of an antacid, and closely monitor clinical response to gefitinib. Consider therapy modification
Hyoscyamine: Antacids may decrease the serum concentration of Hyoscyamine. Management: Administer immediate release hyoscyamine before meals and antacids after meals when these agents are given in combination. Consider therapy modification
Iron Preparations: Antacids may decrease the absorption of Iron Preparations. Management: Separate dosing of oral iron preparations and antacids as much as possible to avoid decreased efficacy of iron preparation. If coadministered with antacids, monitor for decreased therapeutic effects of iron preparations. Exceptions: Ferric Carboxymaltose; Ferric Citrate; Ferric Derisomaltose; Ferric Gluconate; Ferric Hydroxide Polymaltose Complex; Ferric Pyrophosphate Citrate; Ferumoxytol; Iron Dextran Complex; Iron Sucrose. Consider therapy modification
Itraconazole: Antacids may decrease the serum concentration of Itraconazole. Antacids may increase the serum concentration of Itraconazole. Management: Administer Sporanox brand itraconazole at least 2 hours before or 2 hours after administration of any antacids. Exposure to Tolsura brand itraconazole may be increased by antacids; consider itraconazole dose reduction. Consider therapy modification
Ketoconazole (Systemic): Antacids may decrease the serum concentration of Ketoconazole (Systemic). Management: Administer oral ketoconazole at least 2 hours prior to use of any antacid product. Monitor patients closely for signs of inadequate clinical response to ketoconazole. Consider therapy modification
Lanthanum: Antacids may diminish the therapeutic effect of Lanthanum. Consider therapy modification
Ledipasvir: Antacids may decrease the serum concentration of Ledipasvir. Management: Separate the administration of ledipasvir and antacids by 4 hours. Consider therapy modification
Lithium: Sodium Bicarbonate may increase the excretion of Lithium. Monitor therapy
Mecamylamine: Alkalinizing Agents may increase the serum concentration of Mecamylamine. Monitor therapy
Memantine: Alkalinizing Agents may increase the serum concentration of Memantine. Monitor therapy
Mesalamine: Antacids may diminish the therapeutic effect of Mesalamine. Antacid-mediated increases in gastrointestinal pH may cause the premature release of mesalamine from specific sustained-release mesalamine products. Management: Avoid concurrent administration of antacids with sustained-release mesalamine products. Separating antacid and mesalamine administration, and/or using lower antacid doses may be adequate means of avoiding this interaction. Consider therapy modification
Methenamine: Antacids may diminish the therapeutic effect of Methenamine. Consider therapy modification
Methylphenidate: Antacids may increase the absorption of Methylphenidate. Specifically, antacids may interfere with the normal release of drug from the extended-release capsules (Ritalin LA brand), which could result in both increased absorption (early) and decreased delayed absorption. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): Antacids may decrease the serum concentration of Multivitamins/Minerals (with ADEK, Folate, Iron). Specifically, antacids may decrease the absorption of orally administered iron. Management: Separate dosing of oral iron-containing multivitamin preparations and antacids by as much time as possible in order to minimize impact on therapeutic efficacy of the iron preparation. Consider therapy modification
Neratinib: Antacids may decrease the serum concentration of Neratinib. Specifically, antacids may reduce neratinib absorption. Management: Separate the administration of neratinib and antacids by giving neratinib at least 3 hours after the antacid. Consider therapy modification
Nilotinib: Antacids may decrease the serum concentration of Nilotinib. Management: Separate the administration of nilotinib and any antacid by at least 2 hours whenever possible in order to minimize the risk of a significant interaction. Consider therapy modification
PAZOPanib: Antacids may decrease the serum concentration of PAZOPanib. Management: Avoid the use of antacids in combination with pazopanib whenever possible. Separate doses by several hours if antacid treatment is considered necessary. The impact of dose separation has not been investigated. Consider therapy modification
Pexidartinib: Antacids may decrease the serum concentration of Pexidartinib. Management: Administer pexidartinib 2 hours before or after antacids. Consider therapy modification
Phosphate Supplements: Antacids may decrease the absorption of Phosphate Supplements. Management: This applies only to oral phosphate administration. Separating administer of oral phosphate supplements from antacid administration by as long as possible may minimize the interaction. Exceptions: Sodium Glycerophosphate Pentahydrate. Consider therapy modification
Potassium Phosphate: Antacids may decrease the serum concentration of Potassium Phosphate. Management: Consider separating administration of antacids and oral potassium phosphate by at least 2 hours to decrease risk of a significant interaction. Consider therapy modification
QuiNIDine: Antacids may decrease the excretion of QuiNIDine. Monitor therapy
QuiNINE: Alkalinizing Agents may increase the serum concentration of QuiNINE. Monitor therapy
Rilpivirine: Antacids may decrease the serum concentration of Rilpivirine. Management: Administer antacids at least 2 hours before or 4 hours after rilpivirine. Administer antacids at least 6 hours before or 4 hours after the rilpivirine/dolutegravir combination product. Consider therapy modification
Riociguat: Antacids may decrease the serum concentration of Riociguat. Management: Separate the administration of antacids and riociguat by at least 1 hour in order to minimize any potential interaction. Consider therapy modification
Rosuvastatin: Antacids may decrease the serum concentration of Rosuvastatin. Monitor therapy
Sotalol: Antacids may decrease the serum concentration of Sotalol. Management: Avoid simultaneous administration of sotalol and antacids. Administer antacids 2 hours after sotalol. Consider therapy modification
Sulpiride: Antacids may decrease the serum concentration of Sulpiride. Management: Separate administration of antacids and sulpiride by at least 2 hours in order to minimize the impact of antacids on sulpiride absorption. Consider therapy modification
Tetracyclines: Antacids may decrease the absorption of Tetracyclines. Management: Separate administration of antacids and oral tetracycline derivatives by several hours when possible to minimize the extent of this potential interaction. Exceptions: Eravacycline. Consider therapy modification
Velpatasvir: Antacids may decrease the serum concentration of Velpatasvir. Management: Separate administration of velpatasvir and antacids by at least 4 hours. Consider therapy modification
Adverse Reactions
Frequency not defined.
Cardiovascular: Cardiac failure (exacerbation), edema
Central nervous system: Cerebral hemorrhage
Endocrine & metabolic: Acidosis (intracranial), hypernatremia, hypocalcemia, hypokalemia, metabolic alkalosis, milk-alkali syndrome (especially with renal dysfunction)
Gastrointestinal: Abdominal distention, eructation, flatulence (oral administration)
Neuromuscular & skeletal: Tetany
Respiratory: Pulmonary edema
Warnings/Precautions
Concerns related to adverse effects:
- Extravasation: Vesicant (at concentrations ≥8.4%); ensure proper catheter or needle position prior to and during infusion. Avoid extravasation (tissue necrosis may occur due to hypertonicity.
Disease-related concerns:
- Cirrhosis: Use with caution in patients with cirrhosis.
- Edema: Use with caution in patients with edema.
- Heart failure: Use with caution in patients with heart failure.
- Peptic ulcer disease: Not to be used in treatment of peptic ulcer disease.
- Renal impairment: Use with caution in patients with renal impairment; may cause sodium retention.
Special populations:
- Elderly: Not the antacid of choice for the elderly because of sodium content and potential for systemic alkalosis.
- Pediatric: Rapid administration in neonates, infants, and children <2 years of age has led to hypernatremia, decreased CSF pressure, and intracranial hemorrhage.
Dosage form specific issues:
- Injection: Use of IV NaHCO3should be reserved for documented metabolic acidosis and for hyperkalemia-induced cardiac arrest. Routine use in cardiac arrest is not recommended.
Pregnancy
Pregnancy Considerations
Animal reproduction studies have not been conducted. Medications used for the treatment of cardiac arrest in pregnancy are the same as in the non-pregnant woman. Doses and indications should follow current Advanced Cardiovascular Life Support guidelines. Appropriate medications should not be withheld due to concerns of fetal teratogenicity (Campbell 2009; Jeejeebhoy [AHA] 2015). Antacids containing sodium bicarbonate should not be used during pregnancy due to their potential to cause metabolic alkalosis and fluid overload (Mahadevan 2007).
Patient Education
What is this drug used for?
Tablets:
- It is used to treat heartburn and upset stomach.
Injection:
- It is used to treat high acid levels in the blood.
- It is used to lower acid levels in the urine.
- It is used to replace bicarbonate loss caused by severe diarrhea.
All products:
- It may be given to you for other reasons. Talk with the doctor.
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Twitching
- Stiff muscles
- Muscle spasms
- Irritability
- Shortness of breath
- Excessive weight gain
- Swelling of arms or legs
- Severe injection site pain, burning, redness, edema, blistering, or irritation
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.