Boxed Warning
Hepatotoxicity:
Hepatotoxicity has been observed in clinical trials and postmarketing experience. Hepatotoxicity may be severe, and in some cases, fatal. Monitor hepatic function and interrupt, reduce, or discontinue dosing as recommended.
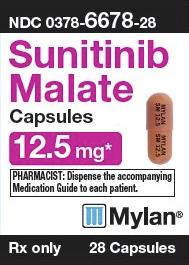
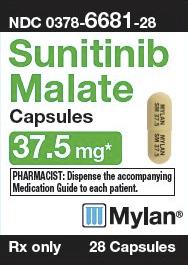
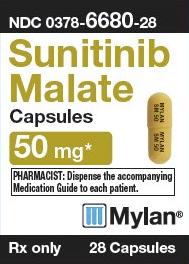
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Capsule, Oral:
Sutent: 12.5 mg, 25 mg, 37.5 mg, 50 mg
Pharmacology
Mechanism of Action
Sunitinib exhibits antitumor and antiangiogenic properties by inhibiting multiple receptor tyrosine kinases, including platelet-derived growth factors (PDGFRα and PDGFRβ), vascular endothelial growth factors (VEGFR1, VEGFR2, and VEGFR3), FMS-like tyrosine kinase-3 (FLT3), colony-stimulating factor type 1 (CSF-1R), and glial cell-line-derived neurotrophic factor receptor (RET).
Pharmacokinetics/Pharmacodynamics
Distribution
Vd/F: 2230 L
Metabolism
Hepatic; primarily metabolized by CYP3A4 to the N-desethyl metabolite SU12662 (active)
Excretion
Feces (61%); urine (16%)
Time to Peak
6 to 12 hours
Half-Life Elimination
Terminal: Sunitinib: 40 to 60 hours; SU12662: 80 to 110 hours
Protein Binding
Sunitinib: 95%; SU12662: 90%
Use in Specific Populations
Special Populations: Renal Function Impairment
Systemic exposure was 47% lower in subjects with ESRD on hemodialysis compared with patients with normal renal function.
Use: Labeled Indications
Gastrointestinal stromal tumor: Treatment of gastrointestinal stromal tumor (GIST) after disease progression on or intolerance to imatinib
Pancreatic neuroendocrine tumors, advanced: Treatment of progressive, well-differentiated pancreatic neuroendocrine tumors in patients with unresectable locally advanced or metastatic disease
Renal cell carcinoma: Adjuvant treatment of adult patients at high risk of recurrent renal cell carcinoma (RCC) following nephrectomy; treatment of advanced RCC
Use: Off Label
Thyroid cancerb
Data from two phase II studies supports the use of sunitinib for the treatment of thyroid cancer Cohen 2008, Ravaud 2008. Additional studies may be necessary to further define the role of sunitinib in this condition.
Soft tissue sarcoma (non-GIST)b
Data from an open-label, multicenter, phase II study supports the use of sunitinib for the treatment of non-GIST soft tissue sarcoma George 2009b. Additional studies may be necessary to further define the role of sunitinib in some subtypes of this condition.
Contraindications
There are no contraindications listed in the manufacturer's US labeling.
Canadian labeling: Hypersensitivity to sunitinib or any component of the formulation; pregnancy
Dosage and Administration
Dosing: Adult
Gastrointestinal stromal tumor (GIST): Oral: 50 mg once daily for 4 weeks of a 6-week treatment cycle (4 weeks on, 2 weeks off) (Demetri 2006)
GIST off-label dosing: Oral: 37.5 mg once daily, continuous daily dosing (George 2009a)
Pancreatic neuroendocrine tumors, advanced (PNET): Oral: 37.5 mg once daily, continuous daily dosing (Raymond 2011); the maximum daily dose used in clinical trials was 50 mg
Renal cell cancer, adjuvant treatment: Oral: 50 mg once daily for 4 weeks of a 6-week treatment cycle (4 weeks on, 2 weeks off) for 9 cycles (Ravaud 2016); the minimum daily dose used in clinical trials was 37.5 mg.
Renal cell cancer, advanced: Oral: 50 mg once daily for 4 weeks of a 6-week treatment cycle (4 weeks on, 2 weeks off) (Motzer 2006a; Motzer 2006b; Motzer 2009)
Soft tissue sarcoma, non-GIST (off-label use): Oral: 37.5 mg once daily, continuous daily dosing (George 2009b)
Thyroid cancer, refractory (off-label use): Oral: 50 mg once daily for 4 weeks of a 6-week treatment cycle (4 weeks on, 2 weeks off) (Cohen, 2008; Ravaud, 2008)
Dosage adjustment with concurrent strong CYP3A4 inhibitor: Avoid concomitant administration with strong CYP3A4 inhibitors (eg, ketoconazole); if concomitant administration with a strong CYP3A4 inhibitor cannot be avoided, consider a dose reduction to a minimum of 37.5 mg/day (GIST, RCC) or 25 mg/day (PNET).
Dosage adjustment with concurrent CYP3A4 inducer: Avoid concomitant administration with CYP3A4 inducers (eg, rifampin); if concomitant administration with a CYP3A4 inducer cannot be avoided, consider a dosage increase (with careful monitoring for toxicity) to a maximum of 87.5 mg/day (GIST, RCC) or 62.5 mg/day (PNET).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Adjustment for Toxicity
Dosage modifications should be done in increments or decrements of 12.5 mg; individualize based on safety and tolerability.
Cardiac toxicity:
Ejection fraction <50% but >20% below baseline or below the lower limit of normal (if baseline ejection fraction is not available) without evidence of CHF: Interrupt treatment and/or reduce dose.
Clinical signs/symptoms of HF: Discontinue treatment.
Dermatologic toxicity:
Signs/symptoms of erythema multiforme (EM), Stevens-Johnson syndrome (SJS), and toxic epidermal necrolysis (TEN), including progressive skin rash, often with blisters or mucosal lesions: Discontinue sunitinib; do not restart treatment if SJS or TEN are suspected.
Necrotizing fasciitis: Discontinue sunitinib.
Hypertension, severe: Temporarily interrupt treatment until hypertension is controlled.
Nephrotic syndrome: Discontinue treatment.
Proteinuria:
Urine protein ≥3 g/24 hours: Interrupt treatment and reduce the dose.
Persistent urine protein ≥3 g/24 hours despite dose reductions: Discontinue treatment.
Reversible posterior leukoencephalopathy (RPLS): Temporarily withhold treatment; after resolution, may resume with discretion.
Thrombotic microangiopathy: Discontinue treatment.
Extemporaneously Prepared
A 10 mg/mL sunitinib oral suspension may be made with capsules and a 1:1 mixture of Ora-Sweet and Ora-Plus. Empty the contents of three 50 mg sunitinib capsules into a mortar; add small portions of vehicle and mix to a uniform paste. Mix while adding vehicle in incremental proportions to 15 mL. Transfer to amber plastic bottle and label "shake well". This suspension maintains an average concentration of 96% to 106% (of the original concentration) at room temperature or refrigerated for up to 60 days in plastic amber prescription bottles.
Navid F, Christensen R, Minkin P, et al, “Stability of Sunitinib in Oral Suspension,” Ann Pharmacother, 2008, 42(7):962-6.18577759
Administration
May be administered with or without food.
Dietary Considerations
Avoid grapefruit juice.
Storage
Store at 25°C (77°F); excursions are permitted between 15°C to 30°C (59°F to 86°F).
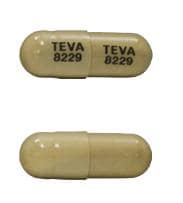
SUNItinib Images
Drug Interactions
Androgens: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Exceptions: Danazol. Monitor therapy
Antidiabetic Agents: May enhance the hypoglycemic effect of Hypoglycemia-Associated Agents. Monitor therapy
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Baricitinib: Immunosuppressants may enhance the immunosuppressive effect of Baricitinib. Management: Use of baricitinib in combination with potent immunosuppressants such as azathioprine or cyclosporine is not recommended. Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted. Consider therapy modification
BCG (Intravesical): Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Bevacizumab: SUNItinib may enhance the adverse/toxic effect of Bevacizumab. Specifically, the risk for a specific form of anemia, microangiopathic hemolytic anemia (MAHA), may be increased. Bevacizumab may enhance the hypertensive effect of SUNItinib. Avoid combination
Bisphosphonate Derivatives: Angiogenesis Inhibitors (Systemic) may enhance the adverse/toxic effect of Bisphosphonate Derivatives. Specifically, the risk for osteonecrosis of the jaw may be increased. Monitor therapy
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Cladribine: May enhance the immunosuppressive effect of Immunosuppressants. Avoid combination
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Coccidioides immitis Skin Test: Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of SUNItinib. Management: Avoid when possible. If such a combination cannot be avoided, sunitinib dose increases are recommended, and vary by indication. See full monograph for details. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of SUNItinib. Management: Avoid when possible. If such a combination cannot be avoided, sunitinib dose decreases are recommended, and vary by indication. See full monograph for details. Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Denosumab: May enhance the adverse/toxic effect of Immunosuppressants. Specifically, the risk for serious infections may be increased. Monitor therapy
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Echinacea: May diminish the therapeutic effect of Immunosuppressants. Consider therapy modification
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fingolimod: Immunosuppressants may enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). Consider therapy modification
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Grapefruit Juice: May increase the serum concentration of SUNItinib. Management: Advise patients to avoid consuming grapefruit and grapefruit juice during sunitinib treatment. Consider therapy modification
Haloperidol: QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of Haloperidol. Monitor therapy
Herbs (Hypoglycemic Properties): May enhance the hypoglycemic effect of Hypoglycemia-Associated Agents. Monitor therapy
Hypoglycemia-Associated Agents: May enhance the hypoglycemic effect of other Hypoglycemia-Associated Agents. Monitor therapy
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Itraconazole: May increase the serum concentration of SUNItinib. Management: Avoid when possible. If such a combination cannot be avoided, sunitinib dose decreases are recommended, and vary by indication. See full monograph for details. Consider therapy modification
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Leflunomide: Immunosuppressants may enhance the adverse/toxic effect of Leflunomide. Specifically, the risk for hematologic toxicity such as pancytopenia, agranulocytosis, and/or thrombocytopenia may be increased. Management: Consider not using a leflunomide loading dose in patients receiving other immunosuppressants. Patients receiving both leflunomide and another immunosuppressant should be monitored for bone marrow suppression at least monthly. Consider therapy modification
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Maitake: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Monoamine Oxidase Inhibitors: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Natalizumab: Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. Avoid combination
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
NiCARdipine: May increase the serum concentration of SUNItinib. Monitor therapy
Nivolumab: Immunosuppressants may diminish the therapeutic effect of Nivolumab. Consider therapy modification
Ocrelizumab: May enhance the immunosuppressive effect of Immunosuppressants. Monitor therapy
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Pegvisomant: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Pidotimod: Immunosuppressants may diminish the therapeutic effect of Pidotimod. Monitor therapy
Pimecrolimus: May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Prothionamide: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
QT-prolonging Agents (Highest Risk): QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Quinolones: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Quinolones may diminish the therapeutic effect of Blood Glucose Lowering Agents. Specifically, if an agent is being used to treat diabetes, loss of blood sugar control may occur with quinolone use. Monitor therapy
Roflumilast: May enhance the immunosuppressive effect of Immunosuppressants. Consider therapy modification
Salicylates: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Saquinavir: May increase the serum concentration of SUNItinib. Avoid combination
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Selective Serotonin Reuptake Inhibitors: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Siponimod: Immunosuppressants may enhance the immunosuppressive effect of Siponimod. Monitor therapy
Sipuleucel-T: Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. Consider therapy modification
Smallpox and Monkeypox Vaccine (Live): Immunosuppressants may diminish the therapeutic effect of Smallpox and Monkeypox Vaccine (Live). Monitor therapy
St John's Wort: May decrease the serum concentration of SUNItinib. Avoid combination
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Tacrolimus (Topical): May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Temsirolimus: May enhance the adverse/toxic effect of SUNItinib. Avoid combination
Tertomotide: Immunosuppressants may diminish the therapeutic effect of Tertomotide. Monitor therapy
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Tofacitinib: Immunosuppressants may enhance the immunosuppressive effect of Tofacitinib. Management: Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted, and this warning seems particularly focused on more potent immunosuppressants. Consider therapy modification
Trastuzumab: May enhance the neutropenic effect of Immunosuppressants. Monitor therapy
Upadacitinib: Immunosuppressants may enhance the immunosuppressive effect of Upadacitinib. Avoid combination
Vaccines (Inactivated): Immunosuppressants may diminish the therapeutic effect of Vaccines (Inactivated). Management: Vaccine efficacy may be reduced. Complete all age-appropriate vaccinations at least 2 weeks prior to starting an immunosuppressant. If vaccinated during immunosuppressant therapy, revaccinate at least 3 months after immunosuppressant discontinuation. Consider therapy modification
Vaccines (Live): Immunosuppressants may enhance the adverse/toxic effect of Vaccines (Live). Immunosuppressants may diminish the therapeutic effect of Vaccines (Live). Management: Avoid use of live organism vaccines with immunosuppressants; live-attenuated vaccines should not be given for at least 3 months after immunosuppressants. Exceptions: Smallpox and Monkeypox Vaccine (Live). Avoid combination
Adverse Reactions
>10%:
Cardiovascular: Increased serum creatine kinase (49%), hypertension (15% to 39%), peripheral edema (≤24%), decreased left ventricular ejection fraction (11% to 16%), chest pain (13%)
Central nervous system: Fatigue (≤62%), headache (18% to 23%), insomnia (15% to 18%), chills (14%), mouth pain (6% to 14%), depression (11%), dizziness (11%)
Dermatologic: Palmar-plantar erythrodysesthesia (14% to 50%), skin discoloration (18% to 30%; yellow color), skin rash (14% to 29%), hair discoloration (7% to 29%), xeroderma (14% to 23%), alopecia (5% to 14%), erythema of skin (12%), pruritus (12%)
Endocrine & metabolic: Increased uric acid (46%), decreased serum calcium (34% to 42%), decreased serum albumin (28% to 41%), decreased serum phosphate (31% to 36%), hypothyroidism (≤24%), increased thyroid stimulating hormone level (≤24%), decreased serum potassium (12% to 21%), decreased serum sodium (20%), decreased serum magnesium (19%), weight loss (16%), increased serum calcium (13%), increased serum sodium (10% to 13%)
Gastrointestinal: Diarrhea (40% to 66%), stomatitis (29% to 61%; grades 3/4: 3% to 6%; grade 4: <1%), nausea (34% to 58%), increased serum lipase (17% to 56%), anorexia (≤48%), dysgeusia (21% to 47%), abdominal pain (25% to 39%), vomiting (19% to 39%), increased serum amylase (17% to 35%), dyspepsia (15% to 34%), constipation (12% to 23%), decreased appetite (≤19%), flatulence (14%), xerostomia (13%), gastroesophageal reflux disease (12%), glossalgia (11%)
Hematologic & oncologic: Decreased hemoglobin (26% to 79%; grades 3/4: 3% to 8%; grade 4: 2%), lymphocytopenia (38% to 68%; grades 3/4: 3% to 18%, grade 4: 2%), hemorrhage (22% to 37%; grades 3/4: ≤4%), neutropenia (grades 3/4: 13%)
Hepatic: Increased serum aspartate aminotransferase (≤72%), increased serum alanine aminotransferase (≤61%), increased serum alkaline phosphatase (24% to 46%), increased serum bilirubin (16% to 37%), increased indirect serum bilirubin (10% to 13%)
Local: Localized edema (18%)
Neuromuscular & skeletal: Asthenia (≤57%), limb pain (≤40%), arthralgia (11% to 30%), back pain (28%), myalgia (≤14%)
Renal: Increased serum creatinine (12% to 70%)
Respiratory: Cough (27%), dyspnea (26%), epistaxis (21%), nasopharyngitis (14%), oropharyngeal pain (14%), upper respiratory tract infection (11%)
Miscellaneous: Fever (12% to 22%)
1% to 10%:
Cardiovascular: Edema (≤10%), venous thromboembolism (4%), cardiac failure (3%)
Endocrine & metabolic: Hypoglycemia (2% to 10%), hyperglycemia (grades 3/4: 2%), hyperkalemia (grades 3/4: 2%)
Gastrointestinal: Hemorrhoids (10%), pancreatitis (1%)
Hematologic & oncologic: Thrombocytopenia (grades 3/4: 5%), leukopenia (grades 3/4: 3%)
Respiratory: Flu-like symptoms (5%)
Frequency not defined:
Gastrointestinal: Aphthous stomatitis, dry mucous membranes, gingival pain, gingivitis, glossitis, hematemesis, hematochezia, melena, oral discomfort, oral mucosal ulcer, tongue ulcer
Genitourinary: Abnormal uterine bleeding
Hematologic & oncologic: Hematoma
Respiratory: Hemoptysis
<1%, postmarketing, and/or case reports: Acute renal failure, angioedema, arterial thrombosis, cardiac failure, cardiomyopathy, cerebral hemorrhage, cerebral infarction, cerebrovascular accident, cholecystitis (particularly acalculous), erythema multiforme, esophagitis, fistula (sometimes associated with tumor necrosis and/or regression), necrotizing fasciitis (including of the perineum), gastrointestinal hemorrhage, gastrointestinal perforation, hemolytic-uremic syndrome, hepatic failure, hepatotoxicity, hypersensitivity reaction, hyperthyroidism, ischemic heart disease, myocardial infarction, myopathy, nephrotic syndrome, neutropenic infection, osteonecrosis of the jaw, pleural effusion, preeclampsia (like syndrome with proteinuria and reversible hypertension) (Gallucci 2013; Patel 2008), prolonged QT interval on ECG, proteinuria, pulmonary embolism, pulmonary hemorrhage, pyoderma gangrenosum (including positive dechallenges), renal insufficiency, respiratory tract hemorrhage, respiratory tract infection, reversible posterior leukoencephalopathy syndrome, rhabdomyolysis, seizure, sepsis, septic shock, serious infection, skin infection, Stevens-Johnson syndrome, thrombotic microangiopathy, thrombotic thrombocytopenic purpura, thyroiditis (Feldt 2012), torsades de pointes, toxic epidermal necrolysis, transient ischemic attacks, tumor hemorrhage, tumor lysis syndrome, urinary tract hemorrhage, urinary tract infection, ventricular arrhythmia, wound healing impairment
Warnings/Precautions
Concerns related to adverse effects:
- Cardiovascular events: Cardiovascular events (some fatal), including heart failure (HF), cardiomyopathy, myocardial ischemia and myocardial infarction (MI) have been reported. Consider left ventricular ejection fraction (LVEF) baseline evaluation prior to treatment in patients without cardiac risk factors; monitor closely for signs/symptoms of HF during sunitinib treatment; consider periodic LVEF evaluations. Discontinue with clinical signs and symptoms of HF. In patients without clinical signs/symptoms of HF, interrupt therapy and/or decrease dose with LVEF <50% but >20% from baseline or below the lower limit of normal (if baseline ejection fraction is not available). In some patients, HF may recover. Patients with cardiac events (MI [including severe/unstable angina], bypass graft, symptomatic HF, cerebrovascular accident, transient ischemic attack, and pulmonary embolism) within the previous 12 months were excluded from clinical trials and patients with prior anthracycline use or cardiac radiation were also excluded from some clinical trials; it is not known if the risk for left ventricular dysfunction is increased in patients with these conditions.
- Dermatologic toxicities: Severe cutaneous reactions, including erythema multiforme (EM), Stevens-Johnson syndrome (SJS), and toxic epidermal necrolysis (TEN) have been reported (some fatal); if signs/symptoms of EM, SJS, or TEN (progressive skin rash, often with blisters or mucosal lesions) are present, discontinue sunitinib. Do not restart treatment if SJS or TEN are suspected. Necrotizing fasciitis (with fatalities) has been reported, including perineum necrotizing fasciitis and fasciitis secondary to fistula formation. Discontinue sunitinib in patients who develop necrotizing fasciitis. Sunitinib may cause skin and/or hair depigmentation or discoloration.
- GI complications: Serious and fatal GI complications, including GI perforation, have occurred (rarely) in patients with intra-abdominal malignancies. Pancreatitis has been observed in RCC patients.
- Hand-foot skin reaction: Hand-foot skin reaction (HFSR) observed with tyrosine kinase inhibitors (TKIs), including sunitinib, and is distinct from hand-foot syndrome (palmar-plantar erythrodysesthesia) associated with traditional chemotherapy agents; HFSR due to TKIs is localized with defined hyperkeratotic lesions; symptoms include burning, dysesthesia, paresthesia, or tingling on the palms/soles, and generally occur within the first 2 to 4 weeks of treatment; pressure and flexor areas may develop blisters (callus-like), dry/cracked skin, edema, erythema, desquamation, or hyperkeratosis (Appleby 2011). The following treatments may be used in addition to the recommended dosage modifications (Lacouture 2008). Prior to treatment initiation, a pedicure is recommended to remove hyperkeratotic areas/calluses, which may predispose to HFSR; avoid vigorous exercise/activities that may stress hands or feet. During therapy, patients should reduce exposure to hot water (may exacerbate hand-foot symptoms); avoid constrictive footwear and excessive skin friction. Patients may also wear thick cotton gloves or socks and should wear shoes with padded insoles. Grade 1 HFSR may be relieved with moisturizing creams, cotton gloves and socks (at night) and/or keratolytic creams such as urea (20% to 40%) or salicylic acid (6%). Apply topical steroid (eg, clobetasol ointment) twice daily to erythematous areas of grade 2 HFSR; topical anesthetics (eg, lidocaine 2%) and then systemic analgesics (if appropriate) may be used for pain control. Resolution of acute erythema may result in keratotic areas which may be softened with keratolytic agents.
- Hemorrhage: Hemorrhagic events (some fatal) have been reported through postmarketing surveillance. Events (including grades 3 and 4 toxicity) have included GI, respiratory, tumor, urinary tract, and brain hemorrhages. Epistaxis was the most commonly observed hemorrhagic event, while GI hemorrhage was the most common ≥ grade 3 event. Tumor-related hemorrhage has been reported, and may occur suddenly. In patients with pulmonary tumors, severe and life-threatening hemoptysis or pulmonary hemorrhage may occur; cases of pulmonary hemorrhage with some fatalities have been reported. Monitor for signs/symptoms of bleeding/hemorrhage and obtain complete blood counts as clinically necessary.
- Hepatotoxicity: [US Boxed Warning]: Hepatotoxicity, which may be severe and/or fatal, has been observed in clinical trials and in postmarketing surveillance. Monitor hepatic function and interrupt, reduce, or discontinue dosing as recommended. Signs of liver failure include jaundice, elevated transaminases, and/or hyperbilirubinemia, in conjunction with encephalopathy, coagulopathy and/or renal failure. Monitor liver function tests at baseline, with each treatment cycle and if clinically indicated. Withhold treatment for grade 3 or 4 hepatotoxicity; discontinue if hepatotoxicity does not resolve. Do not reinitiate in patients with severe changes in liver function tests or other signs/symptoms of liver failure. Sunitinib has not been studied in patients with ALT or AST >2.5 times ULN (or >5 times ULN if due to liver metastases).
- Hypertension: Sunitinib may cause hypertension; for severe hypertension, interrupt therapy until hypertension is controlled. Monitor blood pressure routinely during sunitinib treatment; if indicated, initiate appropriate antihypertensive treatment to reduce the risk for cardiotoxicity (Armenian 2017).
- Hypoglycemia: Symptomatic hypoglycemia has been associated with sunitinib; may result in loss of consciousness or require hospitalization. Hypoglycemia occurred infrequently in patients with renal cell cancer and gastrointestinal stromal tumors (GIST); however, the incidence is higher (~10%) in patients with pancreatic neuroendocrine tumors (PNET); preexisting glucose homeostasis abnormalities were not always present in hypoglycemic patients with PNET. Blood glucose decreases may be worse in patients with diabetes. Monitor blood glucose levels regularly during and following discontinuation of treatment. Dose modifications of antidiabetic medications may be necessary to minimize the risk of hypoglycemia.
- Osteonecrosis of the jaw: Osteonecrosis of the jaw (ONJ), also referred to as medication-related osteonecrosis of the jaw (MRONJ), has been reported with sunitinib. Concurrent bisphosphonate use or dental disease may increase the risk for ONJ. According to a position paper by the American Association of Maxillofacial Surgeons (AAOMS), MRONJ has been associated with bisphosphonates and other antiresorptive agents (denosumab), and antiangiogenic agents (eg, bevacizumab, sunitinib) used for the treatment of osteoporosis or malignancy. Antiangiogenic agents, when given concomitantly with antiresorptive agents, are associated with an increased risk of ONJ. Other risk factors for MRONJ include dentoalveolar surgery (eg, tooth extraction, dental implants), preexisting inflammatory dental disease, and concomitant corticosteroid use. Consider a dental examination and preventive dentistry prior to initiation of sunitinib (and during therapy); if possible, avoid invasive dental procedures in patients with current or prior bisphosphonate use (particularly IV bisphosphonate use). The AAOMS suggests that if medically permissible, initiation of antiangiogenic agents for cancer therapy should be delayed until optimal dental health is attained (if extractions are required, antiangiogenesis therapy should delayed until the extraction site has mucosalized or until after adequate osseous healing). Once antiangiogenic therapy for oncologic disease is initiated, procedures that involve direct osseous injury and placement of dental implants should be avoided. Patients developing ONJ during therapy should receive care by an oral surgeon (AAOMS [Ruggiero 2014]).
- Proteinuria/nephrotic syndrome: Proteinuria and nephrotic syndrome have been reported; some cases have led to renal failure and fatal outcomes. Monitor for new onset or worsening proteinuria with baseline and periodic urinalysis and follow up with 24-hour urine protein if clinically indicated. If urine protein is ≥3 g/24 hours, interrupt treatment and reduce the dose. Discontinue treatment in patients with nephrotic syndrome or persistent urine protein ≥3 g/24 hours despite dose reductions. The safety of continuing treatment with sunitinib in patients with moderate to severe proteinuria has not been evaluated.
- QTc prolongation: QTc prolongation and torsade de pointes have been observed (dose dependent); use caution in patients with a history of QTc prolongation, with medications known to increase sunitinib levels or prolong the QT interval, or patients with preexisting (relevant) cardiac disease, bradycardia, or electrolyte imbalance. Consider baseline and periodic 12-lead ECGs; correct electrolyte abnormalities prior to treatment and monitor and correct potassium, calcium, and magnesium levels during therapy.
- Reversible posterior leukoencephalopathy syndrome: Reversible posterior leukoencephalopathy syndrome (RPLS) has been reported rarely (some fatal). Symptoms of RPLS include confusion, headache, hypertension, lethargy, seizure, blindness and/or other vision, or neurologic disturbances; interrupt treatment and begin medical management, including management of hypertension.
- Thyroid disorders: Thyroid dysfunction (eg, hypothyroidism, hyperthyroidism, thyroiditis) may occur. Hyperthyroidism, sometimes followed by hypothyroidism, has also been reported. Monitor thyroid function at baseline and monitor for signs/symptoms of thyroid dysfunction during treatment. Patients not receiving thyroid hormone replacement therapy at sunitinib initiation should be monitored (TSH) every 4 weeks for 4 months and then every 2 to 3 months; those patients already receiving levothyroxine prior to initiating sunitinib should have TSH monitored every 4 weeks until levels and levothyroxine dose are stable, then monitor every 2 months (Hamnvik 2011).
- Thrombotic microangiopathy: Thrombotic microangiopathy (including thrombotic thrombocytopenic purpura and hemolytic uremic syndrome), sometimes leading to renal failure or fatality, has been reported with sunitinib, both as monotherapy and in combination with bevacizumab. Discontinue sunitinib if thrombotic microangiopathy develops; effects may be reversible after discontinuation.
- Tumor lysis syndrome: Tumor lysis syndrome (TLS), including fatalities, has been reported, predominantly in patients with RCC or GIST. Risk for TLS is higher in patients with a high tumor burden prior to treatment; monitor closely. Correct clinically significant dehydration and treat high uric acid levels prior to initiation of treatment.
- Wound healing complications: Impaired wound healing has been reported with sunitinib; temporarily withhold treatment for patients undergoing major surgical procedures. The optimal time to resume treatment after a procedure has not been determined; the decision to resume sunitinib following a major surgical procedure should be based on clinical judgement of recovery from surgery.
Disease-related concerns:
- Renal insufficiency: An increased incidence of fatigue, thyroid dysfunction and treatment-induced hypertension was reported in patients with renal insufficiency (CrCl ≤60 mL/minute) who received sunitinib for the treatment of renal cell cancer (Gupta 2011).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Administration: Dosing schedules vary by indication; some treatment regimens are continuous daily dosing; other treatment schedules are daily dosing for 4 weeks of a 6-week cycle (4 weeks on, 2 weeks off).
Monitoring Parameters
CBC with differential and platelets (prior to each treatment cycle and if indicated during treatment), liver function tests (baseline, with each cycle and if clinically indicated), serum chemistries including magnesium, phosphate, calcium, and potassium (prior to each treatment cycle), blood glucose levels (regularly during and following discontinuation of treatment), urinalysis (for proteinuria development or worsening); pregnancy test (prior to treatment in females of reproductive potential); LVEF at baseline (and periodic with cardiac risk factors), consider ECG (12-lead; baseline and periodic), monitor blood pressure routinely (Armenian 2017); monitor for signs/symptoms of HF during treatment; consider periodic LVEF evaluations; consider dental exam prior to treatment initiation; monitor for symptoms of hypothyroidism, hyperthyroidism, or thyroiditis; signs/symptoms of bleeding/hemorrhage, hypoglycemia, dermatologic toxicity. Monitor adherence.
Thyroid function testing (Hamnvik, 2011):
Preexisting levothyroxine therapy: Obtain baseline TSH levels, then monitor every 4 weeks until levels and levothyroxine dose are stable, then monitor every 2 months
Without preexisting thyroid hormone replacement: TSH at baseline, then every 4 weeks for 4 months, then every 2-3 months
Pregnancy
Pregnancy Considerations
Based on animal reproduction studies and its mechanism of action, sunitinib may cause fetal harm if administered to a pregnant woman. Because sunitinib inhibits angiogenesis, a critical component of fetal development, adverse effects on pregnancy would be expected. Obtain a pregnancy test prior to treatment initiation in women of reproductive potential; effective contraception should be used during treatment and for at least 4 weeks after the last sunitinib dose. Male patients with female partners of reproductive potential should use effective contraception during treatment and for 7 weeks after the last sunitinib dose. Male and female fertility may be affected.
Patient Education
What is this drug used for?
- It is used to treat cancer.
Frequently reported side effects of this drug
- Loss of strength and energy
- Nausea
- Vomiting
- Lack of appetite
- Weight loss
- Abdominal pain
- Constipation
- Diarrhea
- Hair discoloration
- Skin discoloration
- Hair loss
- Dry skin
- Itching
- Trouble sleeping
- Change in taste
- Mouth irritation
- Mouth sores
- Back pain
- Sore throat
- Stuffy nose
- Dry mouth
- Passing gas
- Muscle pain
- Joint pain
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Low blood sugar like dizziness, headache, fatigue, feeling weak, shaking, fast heartbeat, confusion, increased hunger, or sweating.
- High blood sugar like confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit.
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding.
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain.
- Thyroid problems like change in weight without trying, anxiety, agitation, feeling very weak, hair thinning, depression, neck swelling, difficulty focusing, inability handling heat or cold, menstrual changes, tremors, or sweating.
- Electrolyte problems like mood changes, confusion, muscle pain or weakness, abnormal heartbeat, seizures, lack of appetite, or severe nausea or vomiting,
- Jaw pain
- Redness or irritation of palms or soles of feet
- Depression
- Dizziness
- Passing out
- Flu-like signs
- Abnormal heartbeat
- Chest pain
- Headache
- Heart problems like cough or shortness of breath that is new or worse, swelling of the ankles or legs, abnormal heartbeat, weight gain of more than five pounds in 24 hours, dizziness, or passing out.
- Thrombotic thrombocytopenic purpura/hemolytic uremic syndrome like bruising or bleeding; loss of strength and energy; dark urine or yellow skin; pale skin; change in amount of urine passed; vision changes; change in strength on one side is greater than the other, trouble speaking or thinking, or change in balance; or fever.
- Tumor lysis syndrome like fast heartbeat or abnormal heartbeat; any passing out; unable to pass urine; muscle weakness or cramps; nausea, vomiting, diarrhea or lack of appetite; or feeling sluggish.
- Posterior reversible encephalopathy syndrome like confusion, not alert, vision changes, seizures, or severe headache.
- Necrotizing fasciitis like warm skin with red or purple areas of swelling that spread quickly; ulcers, blisters, black spots on the skin; or any other skin changes.
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.