Boxed Warning
Hepatotoxicity:
Severe liver injury, including fatal liver failure, has been reported in patients treated with leflunomide, which is indicated for rheumatoid arthritis. A similar risk would be expected for teriflunomide because recommended doses of teriflunomide and leflunomide result in a similar range of plasma concentrations of teriflunomide. Concomitant use of teriflunomide with other potentially hepatotoxic drugs may increase the risk of severe liver injury. Obtain transaminase and bilirubin levels within 6 months before initiation of teriflunomide therapy. Monitor ALT levels at least monthly for 6 months after starting teriflunomide. If drug-induced liver injury is suspected, discontinue teriflunomide and start an accelerated elimination procedure with cholestyramine or charcoal. Teriflunomide is contraindicated in patients with severe hepatic impairment. Patients with preexisting liver disease may be at an increased risk of developing elevated serum transaminases when taking teriflunomide.
Embryofetal toxicity:
Teriflunomide is contraindicated for use in pregnant women and in women of reproductive potential who are not using effective contraception because of the potential for fetal harm. Teratogenicity and embryolethality occurred in animals at plasma teriflunomide exposures lower than that in humans. Exclude pregnancy before the start of treatment with teriflunomide in females of reproductive potential. Advise females of reproductive potential to use effective contraception during teriflunomide treatment and during an accelerated drug elimination procedure after teriflunomide treatment. Stop teriflunomide and use an accelerated drug elimination procedure if the patient becomes pregnant.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
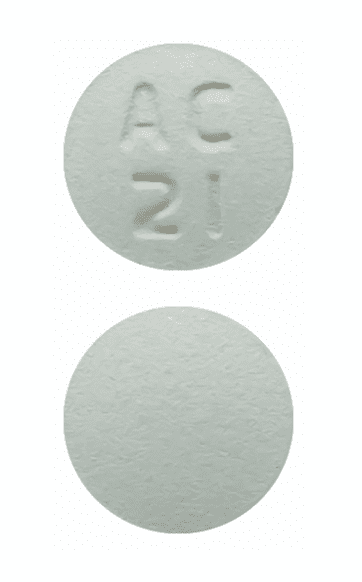
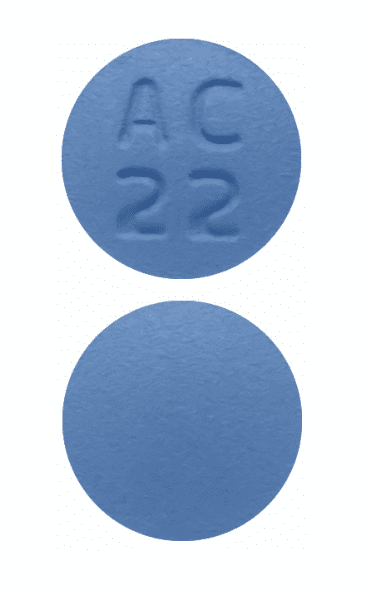
Tablet, Oral:
Aubagio: 7 mg, 14 mg [contains corn starch, fd&c blue #2 aluminum lake]
Pharmacology
Mechanism of Action
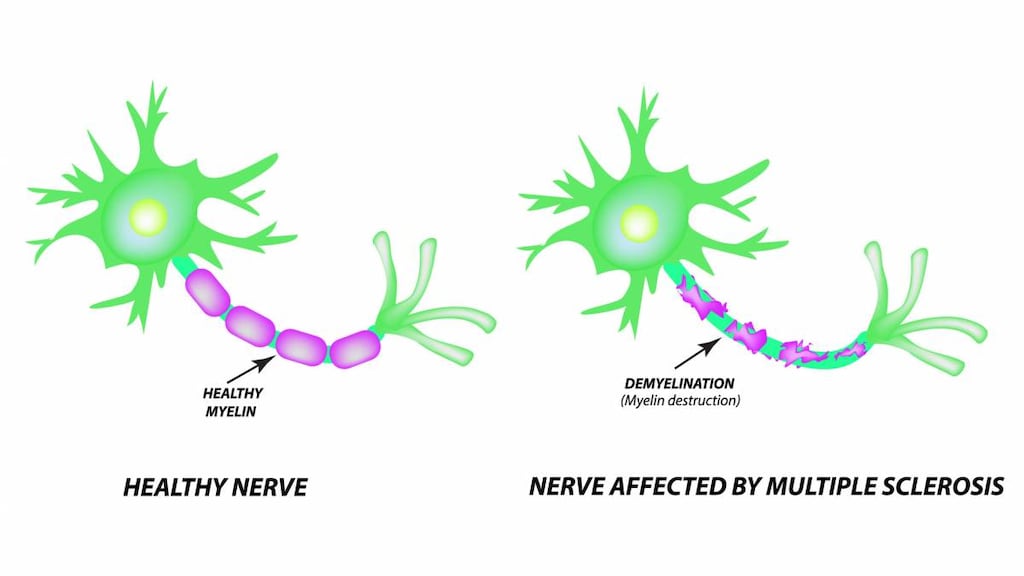
Teriflunomide is an immunomodulatory agent that inhibits pyrimidine synthesis, resulting in antiproliferative and anti-inflammatory effects. It may reduce the number of activated lymphocytes in the CNS.
Pharmacokinetics/Pharmacodynamics
Distribution
Vd: IV: 11 L
Metabolism
Primarily by hydrolysis to minor metabolites; secondary pathways include oxidation, conjugation, and N-acetylation
Excretion
Feces (~38%); urine (~23%)
Time to Peak
Plasma: 1-4 hours
Half-Life Elimination
Median: 18-19 days; enterohepatic recycling appears to contribute to the long half-life of this agent, since activated charcoal and cholestyramine substantially reduce plasma half-life
Protein Binding
>99%
Use in Specific Populations
Special Populations: Gender
There was a 23% decrease in Cl in females compared with males.
Use: Labeled Indications
Multiple sclerosis, relapsing: Treatment of relapsing forms of multiple sclerosis, including clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease in adults.
Contraindications
Hypersensitivity to teriflunomide, leflunomide, or any component of the formulation; severe hepatic impairment; coadministration with leflunomide; pregnant women; females of reproductive potential not using effective contraception.
Canadian labeling: Additional contraindications (not in US labeling): Immunodeficiency states (eg, AIDS); impaired bone marrow function or significant anemias, leucopenia, neutropenia, or thrombocytopenia; serious active infections
Dosage and Administration
Dosing: Adult
Multiple sclerosis, relapsing: Adults: Oral: 7 mg or 14 mg once daily.
Dosing: Adjustment for Toxicity
ALT elevations >3 times ULN: Discontinue teriflunomide and initiate cholestyramine or activated charcoal to enhance elimination
Drug elimination procedure: To achieve nondetectable serum concentrations (<0.02 mg/L) of teriflunomide administer either of the following:
Cholestyramine: 8 g every 8 hours for 11 days. If not tolerated, may decrease to 4 g every 8 hours for 11 days. The 11 days do not need to be consecutive unless plasma concentrations need to be lowered rapidly.
or
Activated charcoal: 50 g every 12 hours for 11 days. The 11 days do not need to be consecutive unless plasma concentrations need to be lowered rapidly.
Note: Both treatments have successfully lead to >98% decrease in teriflunomide concentrations.
Administration
Administer without regard to meals.
Storage
Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
Teriflunomide Images
Drug Interactions
Alpelisib: BCRP/ABCG2 Inhibitors may increase the serum concentration of Alpelisib. Management: Avoid coadministration of BCRP/ABCG2 inhibitors and alpelisib due to the potential for increased alpelisib concentrations and toxicities. If coadministration cannot be avoided, closely monitor for increased alpelisib adverse reactions. Consider therapy modification
Amodiaquine: CYP2C8 Inhibitors (Moderate) may increase the serum concentration of Amodiaquine. Avoid combination
Asunaprevir: OATP1B1/1B3 (SLCO1B1/1B3) Inhibitors may increase the serum concentration of Asunaprevir. Avoid combination
Baricitinib: Immunosuppressants may enhance the immunosuppressive effect of Baricitinib. Management: Use of baricitinib in combination with potent immunosuppressants such as azathioprine or cyclosporine is not recommended. Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted. Consider therapy modification
BCG (Intravesical): Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCRP/ABCG2 Substrates: Teriflunomide may increase the serum concentration of BCRP/ABCG2 Substrates. Monitor therapy
Bendamustine: CYP1A2 Inducers (Moderate) may decrease the serum concentration of Bendamustine. Concentrations of active metabolites may be increased. Management: Consider alternatives to moderate CYP1A2 inducers during therapy with bendamustine due to the potential for decreased bendamustine plasma concentrations and reduced efficacy. Consider therapy modification
Bile Acid Sequestrants: May decrease the serum concentration of Teriflunomide. Management: Unless using this combination to intentionally enhance teriflunomide elimination, consider an alternative to the bile acid sequestrants when possible. Separating drug administration is unlikely to be effective at avoiding the interaction. Consider therapy modification
Caffeine and Caffeine Containing Products: CYP1A2 Inducers (Moderate) may decrease the serum concentration of Caffeine and Caffeine Containing Products. Monitor therapy
Charcoal, Activated: May decrease the serum concentration of Teriflunomide. Management: Unless using this combination to intentionally enhance teriflunomide elimination, consider an alternative to charcoal when possible. Separating drug administration is not likely to be effective at avoiding this interaction. Consider therapy modification
Cladribine: May enhance the immunosuppressive effect of Immunosuppressants. Avoid combination
ClomiPRAMINE: CYP1A2 Inducers (Moderate) may decrease the serum concentration of ClomiPRAMINE. Monitor therapy
CloZAPine: CYP1A2 Inducers (Moderate) may decrease the serum concentration of CloZAPine. Monitor therapy
Coccidioides immitis Skin Test: Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. Monitor therapy
Dabrafenib: CYP2C8 Inhibitors (Moderate) may increase the serum concentration of Dabrafenib. Monitor therapy
Dasabuvir: CYP2C8 Inhibitors (Moderate) may increase the serum concentration of Dasabuvir. Monitor therapy
Denosumab: May enhance the adverse/toxic effect of Immunosuppressants. Specifically, the risk for serious infections may be increased. Monitor therapy
Desloratadine: CYP2C8 Inhibitors (Moderate) may increase the serum concentration of Desloratadine. Monitor therapy
Dichlorphenamide: OAT1/3 Inhibitors may increase the serum concentration of Dichlorphenamide. Monitor therapy
DULoxetine: CYP1A2 Inducers (Moderate) may decrease the serum concentration of DULoxetine. Monitor therapy
Echinacea: May diminish the therapeutic effect of Immunosuppressants. Consider therapy modification
Elagolix: OATP1B1/1B3 (SLCO1B1/1B3) Inhibitors may increase the serum concentration of Elagolix. Avoid combination
Enzalutamide: CYP2C8 Inhibitors (Moderate) may increase the serum concentration of Enzalutamide. Monitor therapy
Erlotinib: Teriflunomide may decrease the serum concentration of Erlotinib. Management: Avoid the concomitant use of erlotinib and teriflunomide if possible. If concomitant use is unavoidable, increase the erlotinib dose by 50 mg increments at 2-week intervals to a maximum of 300 mg. Consider therapy modification
Fingolimod: Immunosuppressants may enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). Consider therapy modification
Grazoprevir: OATP1B1/1B3 (SLCO1B1/1B3) Inhibitors may increase the serum concentration of Grazoprevir. Avoid combination
Leflunomide: May enhance the adverse/toxic effect of Teriflunomide. Leflunomide may increase the serum concentration of Teriflunomide. Avoid combination
Lidocaine (Systemic): CYP1A2 Inducers (Moderate) may decrease the serum concentration of Lidocaine (Systemic). Monitor therapy
Melatonin: CYP1A2 Inducers (Moderate) may decrease the serum concentration of Melatonin. Monitor therapy
Mexiletine: CYP1A2 Inducers (Moderate) may decrease the serum concentration of Mexiletine. Monitor therapy
Natalizumab: Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. Avoid combination
Nivolumab: Immunosuppressants may diminish the therapeutic effect of Nivolumab. Consider therapy modification
OAT1/3 Substrates: Teriflunomide may increase the serum concentration of OAT1/3 Substrates. Monitor therapy
OATP1B1/1B3 (SLCO1B1/1B3) Substrates: Teriflunomide may increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. Monitor therapy
Ocrelizumab: May enhance the immunosuppressive effect of Immunosuppressants. Monitor therapy
OLANZapine: CYP1A2 Inducers (Moderate) may decrease the serum concentration of OLANZapine. Monitor therapy
Ombitasvir, Paritaprevir, Ritonavir, and Dasabuvir: CYP2C8 Inhibitors (Moderate) may increase the serum concentration of Ombitasvir, Paritaprevir, Ritonavir, and Dasabuvir. Specifically, the concentrations of the dasabuvir component may be increased. Monitor therapy
PACLitaxel (Conventional): CYP2C8 Inhibitors (Moderate) may increase the serum concentration of PACLitaxel (Conventional). Monitor therapy
PACLitaxel (Protein Bound): CYP2C8 Inhibitors (Moderate) may increase the serum concentration of PACLitaxel (Protein Bound). Monitor therapy
PAZOPanib: BCRP/ABCG2 Inhibitors may increase the serum concentration of PAZOPanib. Avoid combination
Pidotimod: Immunosuppressants may diminish the therapeutic effect of Pidotimod. Monitor therapy
Pimecrolimus: May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Pioglitazone: CYP2C8 Inhibitors (Moderate) may increase the serum concentration of Pioglitazone. Monitor therapy
Pirfenidone: CYP1A2 Inducers (Moderate) may decrease the serum concentration of Pirfenidone. Monitor therapy
Pomalidomide: CYP1A2 Inducers (Moderate) may decrease the serum concentration of Pomalidomide. Monitor therapy
Propranolol: CYP1A2 Inducers (Moderate) may decrease the serum concentration of Propranolol. Monitor therapy
Repaglinide: CYP2C8 Inhibitors (Moderate) may increase the serum concentration of Repaglinide. Monitor therapy
Revefenacin: OATP1B1/1B3 (SLCO1B1/1B3) Inhibitors may increase serum concentrations of the active metabolite(s) of Revefenacin. Avoid combination
Riluzole: CYP1A2 Inducers (Moderate) may decrease the serum concentration of Riluzole. Monitor therapy
Roflumilast: May enhance the immunosuppressive effect of Immunosuppressants. Consider therapy modification
ROPINIRole: CYP1A2 Inducers (Moderate) may decrease the serum concentration of ROPINIRole. Monitor therapy
Rosuvastatin: Teriflunomide may increase the serum concentration of Rosuvastatin. Management: Limit the maximum adult rosuvastatin dose to 10 mg/day in patients receiving teriflunomide, and monitor for evidence of rosuvastatin toxicity (eg, muscle toxicity, elevated transaminase concentrations). Consider therapy modification
Selexipag: CYP2C8 Inhibitors (Moderate) may increase serum concentrations of the active metabolite(s) of Selexipag. Management: Reduce the selexipag dose to once daily when combined with moderate CYP2C8 inhibitors. Revert back to twice daily selexipag dosing upon stopping the moderate CYP2C8 inhibitor. Consider therapy modification
Siponimod: Immunosuppressants may enhance the immunosuppressive effect of Siponimod. Monitor therapy
Sipuleucel-T: Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. Consider therapy modification
Smallpox and Monkeypox Vaccine (Live): Immunosuppressants may diminish the therapeutic effect of Smallpox and Monkeypox Vaccine (Live). Monitor therapy
Tacrolimus (Topical): May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Talazoparib: BCRP/ABCG2 Inhibitors may increase the serum concentration of Talazoparib. Monitor therapy
Tasimelteon: CYP1A2 Inducers (Moderate) may decrease the serum concentration of Tasimelteon. Monitor therapy
Tertomotide: Immunosuppressants may diminish the therapeutic effect of Tertomotide. Monitor therapy
Theophylline Derivatives: CYP1A2 Inducers (Moderate) may decrease the serum concentration of Theophylline Derivatives. Exceptions: Dyphylline. Monitor therapy
TiZANidine: CYP1A2 Inducers (Moderate) may decrease the serum concentration of TiZANidine. Monitor therapy
Tofacitinib: Immunosuppressants may enhance the immunosuppressive effect of Tofacitinib. Management: Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted, and this warning seems particularly focused on more potent immunosuppressants. Consider therapy modification
Topotecan: BCRP/ABCG2 Inhibitors may increase the serum concentration of Topotecan. Avoid combination
Trastuzumab: May enhance the neutropenic effect of Immunosuppressants. Monitor therapy
Treprostinil: CYP2C8 Inhibitors (Moderate) may increase the serum concentration of Treprostinil. Monitor therapy
Ubrogepant: BCRP/ABCG2 Inhibitors may increase the serum concentration of Ubrogepant. Management: Use an initial ubrogepant dose of 50 mg and second dose (if needed) of 50 mg when used with a BCRP inhibitor. Consider therapy modification
Vaccines (Inactivated): Immunosuppressants may diminish the therapeutic effect of Vaccines (Inactivated). Management: Vaccine efficacy may be reduced. Complete all age-appropriate vaccinations at least 2 weeks prior to starting an immunosuppressant. If vaccinated during immunosuppressant therapy, revaccinate at least 3 months after immunosuppressant discontinuation. Consider therapy modification
Vaccines (Live): Immunosuppressants may enhance the adverse/toxic effect of Vaccines (Live). Immunosuppressants may diminish the therapeutic effect of Vaccines (Live). Management: Avoid use of live organism vaccines with immunosuppressants; live-attenuated vaccines should not be given for at least 3 months after immunosuppressants. Exceptions: Smallpox and Monkeypox Vaccine (Live). Avoid combination
Voxilaprevir: OATP1B1/1B3 (SLCO1B1/1B3) Inhibitors may increase the serum concentration of Voxilaprevir. Avoid combination
Warfarin: Teriflunomide may decrease the serum concentration of Warfarin. Monitor therapy
Adverse Reactions
>10%:
Central nervous system: Headache (16% to 18%)
Dermatologic: Alopecia (10% to 13%)
Endocrine & metabolic: Hypophosphatemia (18%)
Gastrointestinal: Diarrhea (13% to 14%), nausea (8% to 11%)
Hematologic & oncologic: Lymphocytopenia (10% to 12%)
Hepatic: Increased serum alanine aminotransferase (13% to 15%)
1% to 10%:
Cardiovascular: Hypertension (3% to 4%)
Central nervous system: Paresthesia (8% to 9%)
Hematologic & oncologic: Neutropenia (4% to 6%)
Neuromuscular & skeletal: Arthralgia (6% to 8%), peripheral neuropathy (including carpal tunnel syndrome; 1% to 2%)
<1%, postmarketing, and/or case reports: Anaphylaxis, angioedema, cytomegalovirus disease (reactivation), hypersensitivity reaction, increased serum creatinine, interstitial pulmonary disease, jaundice, pancreatitis, Stevens-Johnson syndrome, thrombocytopenia, toxic epidermal necrolysis, uric acid nephropathy
Warnings/Precautions
Concerns related to adverse effects:
- Dermatologic reactions: Cases of serious skin reactions, including cases of Stevens-Johnson syndrome and fatal toxic epidermal necrolysis have been reported with teriflunomide; very rare cases of drug reaction with eosinophilia and systemic symptoms have been reported with leflunomide. Discontinue if evidence of severe dermatologic reactions occurs and begin an accelerated drug elimination procedure (eg, cholestyramine, activated charcoal) immediately; in such cases, patients should not be re-exposed to teriflunomide.
- Hepatotoxicity: [US Boxed Warning]: Use of leflunomide has been associated with reports of hepatotoxicity, hepatic failure, and death, therefore, a similar risk is expected with teriflunomide. Patients with preexisting liver disease (acute or chronic liver disease or ALT >2 x ULN) may be at an increased risk of developing elevated transaminases during therapy; use is contraindicated in patients with severe impairment. Use in patients with concurrent exposure to potentially hepatotoxic drugs may increase the risk of hepatotoxicity. Obtain transaminase and bilirubin levels within 6 months prior to initiation of treatment. Monitor ALT levels at least monthly for first 6 months during therapy; if hepatotoxicity is likely teriflunomide-induced, start drug elimination procedures (eg, cholestyramine, activated charcoal) and monitor liver function tests weekly until normalized. Discontinuation of therapy may be considered if transaminases increase >3 x ULN.
- Hypersensitivity reactions: Anaphylaxis and severe allergic reactions may occur; discontinue if any signs or symptoms of hypersensitivity reaction occur and begin an accelerated drug elimination procedure (eg, cholestyramine, activated charcoal) immediately; in such cases, patients should not be re-exposed to teriflunomide.
- Hypertension: Increases in blood pressure have been reported; monitor at initiation of therapy and periodically thereafter.
- Infections: May increase susceptibility to infection, including opportunistic pathogens. Severe infections, sepsis, and fatalities have been reported with leflunomide. One case of fatal sepsis has been reported with teriflunomide. Not recommended in patients with severe immunodeficiency, bone marrow dysplasia, or severe, uncontrolled infections. Caution should be exercised when considering the use in patients with a history of new/recurrent infections, with conditions that predispose them to infections, or with chronic, latent, or localized infections. Patients who develop a new infection while undergoing treatment should be monitored closely; consider suspension or discontinuation of therapy and drug elimination procedures (eg, cholestyramine, activated charcoal) if infection is serious.
- Interstitial lung disease: Interstitial lung disease, including acute interstitial pneumonitis, has been reported; may be fatal and occur at any time during therapy. Consider treatment discontinuation in patients who develop new onset or worsening of pulmonary symptoms. Drug elimination procedures (eg, cholestyramine, activated charcoal) should be considered if evidence of interstitial lung disease.
- Malignancy: Use may affect defenses against malignancies; impact on the development and course of malignancies is not fully defined. As compared to the general population, an increased risk of lymphoma has been noted in clinical trials with use of some immunosuppressive medications.
- Pancreatitis: Very rare cases of pancreatitis have been reported (Aubagio Canadian product monograph 2015); discontinue therapy in patients with symptoms of acute pancreatitis suspected to be drug-induced and begin drug elimination procedures (eg, cholestyramine, activated charcoal).
- Peripheral neuropathy: Cases of peripheral neuropathy (including polyneuropathy and mononeuropathy) have been reported; use with caution in patients >60 years, receiving concomitant neurotoxic medications or patients with diabetes; discontinue if evidence of peripheral neuropathy occurs and begin drug elimination procedures (eg, cholestyramine, activated charcoal).
- Renal effects: Transient acute renal failure, most likely due to acute uric acid nephropathy, has been reported.
Disease-related concerns:
- Hematologic disorders: Use with caution in patients with a prior history of significant hematologic abnormalities; avoid use with bone marrow dysplasia. Neutropenia, leukopenia, and thrombocytopenia (including rare cases of platelet counts <50,000/mm3) have been reported in clinical trials. Use of leflunomide has been associated with rare pancytopenia, agranulocytosis, and thrombocytopenia, therefore, a similar risk may be expected with teriflunomide. Monitoring of hematologic function is required.
- Tuberculosis: Safety has not been established in patients with latent tuberculosis infection. Patients should be screened for tuberculosis and if necessary, treated prior to initiating therapy.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Pregnancy/women of childbearing potential: [US Boxed Warning]: Teriflunomide is contraindicated in pregnant women or women of childbearing potential who are not using effective contraception. Pregnancy must be excluded prior to initiating treatment in females of reproductive potential.
Other warnings/precautions:
- Drug elimination procedure: Due to variations in clearance, it may take up to 2 years to reach low levels of teriflunomide metabolite serum concentrations. A drug elimination procedure using cholestyramine or activated charcoal is recommended when a more rapid elimination is needed. If a response to teriflunomide had already been observed, the use of a rapid elimination procedure may result in the return of disease activity.
- Immunizations: Patients should be brought up to date with all immunizations before initiating therapy. Live vaccines should not be given concurrently; there are no data available concerning secondary transmission of live vaccines in patients receiving therapy.
Monitoring Parameters
CBC within 6 months of initiation and periodically thereafter based on signs/symptoms of infection; serum creatinine; serum transaminase and bilirubin within 6 months of initiation of therapy and monthly during the initial 6 months of treatment. In addition, monitor for signs/symptoms of severe infection, abnormalities in hepatic function tests, symptoms of hepatotoxicity, hypophosphatemia, and blood pressure (baseline and periodically thereafter). Monitor hepatic function tests weekly until normalized in patients with suspected teriflunomide-induced hepatotoxicity. Screen for tuberculosis prior to therapy. Evaluate pregnancy status in females of reproductive potential before treatment initiation.
Pregnancy
Pregnancy Considerations
[US Boxed Warning]: Teriflunomide is contraindicated in pregnant women and in females of reproductive potential who are not using effective contraception because of the potential for fetal harm. Teratogenicity and embryolethality occurred in animals at plasma teriflunomide exposures lower than that in humans. Stop teriflunomide and use an accelerated drug elimination procedure if the patient becomes pregnant. Pregnancy outcome information following maternal use during pregnancy or following use in male patients who fathered a child are limited (Andersen 2018; Kieseier 2014).
[US Boxed Warning]: Exclude pregnancy before the start of treatment with teriflunomide in females of reproductive potential. Women of childbearing potential should not receive therapy until pregnancy has been excluded, they have been counseled concerning fetal risk, and reliable contraceptive measures have been confirmed.
[US Boxed Warning]: Advise females of reproductive potential to use effective contraception during teriflunomide treatment and during an accelerated drug elimination procedure after teriflunomide treatment. Women who wish to become pregnant, as well as all females of reproductive potential, should undergo the accelerated drug elimination procedure when teriflunomide is discontinued. Pregnancy should be avoided until undetectable serum concentrations (<0.02 mg/L) are verified.
Teriflunomide is found in semen. Males and their female partners should use reliable contraception during therapy. Males who wish to father a child should discontinue teriflunomide and undergo the accelerated drug elimination procedure or wait until plasma teriflunomide concentrations are <0.02 mg/L.
In general, disease-modifying therapies for multiple sclerosis (MS) are stopped prior to a planned pregnancy, and not initiated during pregnancy, except in females at high risk of MS activity (AAN [Rae-Grant 2018]). Consider use of agents other than teriflunomide for females at high risk of disease reactivation who are planning a pregnancy. Delaying pregnancy is recommended for females with persistent high disease activity; when disease-modifying therapy is needed in these patients, other agents are preferred (ECTRIMS/EAN [Montalban 2018]).
Data collection to monitor pregnancy and infant outcomes following exposure to teriflunomide is ongoing. Health care providers are encouraged to enroll females exposed to teriflunomide during pregnancy in the pregnancy registry (800-745-4447, option 2).
Patient Education
What is this drug used for?
- It is used to treat MS (multiple sclerosis).
Frequently reported side effects of this drug
- Nausea
- Diarrhea
- Hair thinning or loss
- Joint pain
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Severe headache
- Severe dizziness
- Passing out
- Vision changes
- Bruising
- Bleeding
- Severe loss of strength and energy
- Swollen glands
- Burning or numbness feeling
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes.
- Severe pulmonary disorder like lung or breathing problems like difficulty breathing, shortness of breath, or a cough that is new or worse.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.
Patient Education
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for health care professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience, and judgment in diagnosing, treating, and advising patients.