Boxed Warning
Depression and suicidality:
Tetrabenazine can increase the risk of depression and suicidal thoughts and behavior (suicidality) in patients with Huntington disease. Anyone considering the use of tetrabenazine must balance the risks of depression and suicidality with the clinical need for control of chorea. Close observation of patients for the emergence or worsening of depression, suicidality, or unusual changes in behavior should accompany therapy. Patients, their caregivers, and families should be informed of the risk of depression and suicidality, and should be instructed to report behaviors of concern promptly to the treating physician.
Particular caution should be exercised in treating patients with a history of depression or prior suicide attempts or ideation, which are increased in frequency in Huntington disease. Tetrabenazine is contraindicated in patients who are actively suicidal, and in patients with untreated or inadequately treated depression.
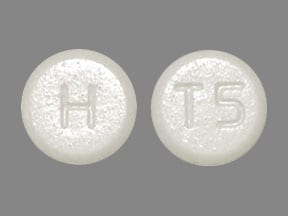
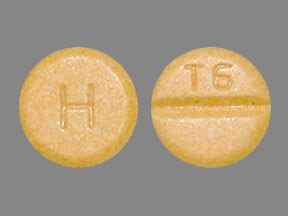
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Xenazine: 12.5 mg [contains corn starch]
Xenazine: 25 mg [scored; contains corn starch]
Generic: 12.5 mg, 25 mg
Pharmacology
Mechanism of Action
Acts as a reversible inhibitor of the human vesicular monamine transporter type 2 (VMAT-2) and thereby decreases the uptake of monoamines (including dopamine, serotonin, norepinephrine, and histamine) into synaptic vesicles and depletes the monoamine stores; hydroxytetrabenazine (HTBZ) also inhibits VMAT-2; weak binding affinity for dopamine D2 receptors.
Pharmacokinetics/Pharmacodynamics
Metabolism
Hepatic (rapid and extensive), to active metabolites: Alpha and beta hydroxytetrabenazine (HTBZ) via CYP2D6 (primary active moiety)
Excretion
Urine (~75% as metabolites, <10% as alpha and beta HTBZ); feces (~7% to 16%)
Time to Peak
Metabolites: Within 1 to 1.5 hours
Duration of Action
16 to 24 hours (at steady-state); chorea may recur within 12 to 18 hours after discontinuation
Half-Life Elimination
Alpha-HTBZ: 7 hours; 10 hours (hepatic impairment); Beta-HTBZ: 5 hours, 8 hours (hepatic impairment); Terabenazine: ~17.5 hours (hepatic impairment)
Protein Binding
82% to 85%; Metabolites: 59% to 68%
Use in Specific Populations
Special Populations: Hepatic Function Impairment
Metabolism of tetrabenazine is decreased in patients with hepatic function impairment and the Cmax is 7- to 190-fold higher compared with healthy subjects.
Use: Labeled Indications
Chorea associated with Huntington disease: Treatment of chorea associated with Huntington disease
Canadian labeling: Additional use (not in US labeling):Treatment of chronic tic disorders, including Tourette syndrome
Use: Off Label
Tardive dyskinesiacyes
Data from a limited number of patients studied suggest that tetrabenazine may decrease the frequency and severity of tardive movements in patients with tardive dyskinesia. Additional data may be necessary to further define the role of tetrabenazine in this condition.
Based on
Contraindications
Hepatic impairment; patients who are actively suicidal or who have untreated or inadequately treated depression; coadministration of MAOIs or use of tetrabenazine within 2 weeks of discontinuation of MAOI therapy; coadministration with reserpine, ≥20 days should pass after discontinuing reserpine before initiating tetrabenazine therapy; coadministration with deutetrabenazine or valbenazine
Canadian labeling: Additional contraindications (not in US labeling): Hypersensitivity to tetrabenazine or any component of the formulation; history or current episode of clinical depression unless under the care of a psychiatrist who is familiar with the patient's disorder and tetrabenazine’s pharmacology
Dosage and Administration
Dosing: Adult
Dose should be individualized; titrate slowly
Chorea associated with Huntington disease: Oral:
Initial: 12.5 mg once daily in the morning, may increase to 12.5 mg twice daily after 1 week. Dosage may be increased by 12.5 mg daily at weekly intervals; daily doses >37.5 mg should be divided into 3 doses (maximum single dose: 25 mg)
Patients requiring doses >50 mg/day: Genotype for CYP2D6:
Extensive/intermediate metabolizers: Maximum: 100 mg/day; 37.5 mg/dose
Poor metabolizers: Maximum: 50 mg/day; 25 mg/dose
Concomitant use with strong CYP2D6 inhibitors (eg, fluoxetine, paroxetine, quinidine): Maximum: 50 mg/day; 25 mg/dose.
Note: If treatment is interrupted for >5 days, retitration is recommended. If treatment is interrupted for <5 days resume at previous maintenance dose.
Tardive dyskinesia (off-label use): Oral: Note: Dose is individualized based on efficacy and tolerance. Initial: 50 mg/day in divided doses; if needed, may increase daily dose by 50 mg every two weeks up to maximum of 150 mg/day in divided doses. Additional data may be necessary to further define the role of tetrabenazine in this condition (Kazamatsuri 1972; Godwin-Austen 1971; Ondo 1999).
Alternatively, an initial dose of 25 to 37.5 mg/day in 2 or 3 divided doses has been recommended with increases or decreases in increments of 12.5 mg/day at weekly intervals. Usual maximum tolerated dose: 75 mg/day in 3 divided doses; in very rare cases, doses up to 200 mg/day have been used (Nitoman Canadian product labeling 2014).
Tourette syndrome (Canadian labeling): Initial: 12.5 mg 2 to 3 times daily; may be increased by 12.5 mg daily at weekly intervals; should be increased to maximal tolerated and effective dose. Usual maximum tolerated dosage: 25 mg 3 times daily; maximum recommended dose: 200 mg/day
Dosing: Geriatric
Refer to adult dosing; use with caution.
Dosing: Pediatric
Tourette syndrome (Canadian labeling): Children and Adolescents: Oral: Administer 50% of adult dose. Initial: 6.25 mg 2 to 3 times daily; may be increased by 6.25 mg daily at weekly intervals; should be titrated slowly to maximal tolerated and effective dose (dose is individualized).
Dosing adjustment for toxicity: Children and Adolescents: For toxicity/adverse reaction, including akathisia, restlessness, parkinsonism, insomnia, depression, suicidality, anxiety, sedation (intolerable): Suspend upward dosage titration and reduce dose; consider discontinuing if adverse reaction does not resolve (may be discontinued without tapering).
Dosing: Adjustment for Toxicity
For toxicity/adverse reaction, including akathisia, restlessness, parkinsonism, insomnia, depression, suicidality, anxiety, sedation (intolerable): Suspend upward dosage titration and reduce dose; consider discontinuing if adverse reaction does not resolve (may be discontinued without tapering).
Administration
Oral: May administer without regard to meals.
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
Tetrabenazine Images
Drug Interactions
Abiraterone Acetate: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of abiraterone with CYP2D6 substrates that have a narrow therapeutic index whenever possible. When concurrent use is not avoidable, monitor patients closely for signs/symptoms of toxicity. Consider therapy modification
Ajmaline: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Alcohol (Ethyl): CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Antipsychotic Agents: Tetrabenazine may enhance the adverse/toxic effect of Antipsychotic Agents. Monitor therapy
Asunaprevir: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Consider therapy modification
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the adverse/toxic effect of Tetrabenazine. Avoid combination
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
CloBAZam: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
Cobicistat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CYP2D6 Inhibitors (Moderate): May decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CYP2D6 Inhibitors (Strong): May increase the serum concentration of Tetrabenazine. Specifically, concentrations of the active alpha- and beta-dihydrotetrabenazine metabolites may be increased. Management: Tetrabenazine adult dose should be reduced by 50% when starting a strong CYP2D6 inhibitor. Maximum tetrabenazine adult dose is 50 mg/day when used with a strong CYP2D6 inhibitor. Consider therapy modification
Dacomitinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of dacomitinib with CYP2D6 subtrates that have a narrow therapeutic index. Consider therapy modification
Darunavir: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Deutetrabenazine: May enhance the adverse/toxic effect of Tetrabenazine. Avoid combination
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
Haloperidol: QT-prolonging Agents (Indeterminate Risk - Avoid) may enhance the QTc-prolonging effect of Haloperidol. Monitor therapy
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Imatinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Lumefantrine: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
Metoclopramide: May enhance the adverse/toxic effect of Tetrabenazine. Avoid combination
MetyroSINE: May enhance the adverse/toxic effect of Tetrabenazine. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Monoamine Oxidase Inhibitors: Tetrabenazine may enhance the adverse/toxic effect of Monoamine Oxidase Inhibitors. Avoid combination
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Panobinostat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Peginterferon Alfa-2b: May decrease the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Peginterferon Alfa-2b may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Perhexiline: CYP2D6 Substrates (High risk with Inhibitors) may increase the serum concentration of Perhexiline. Perhexiline may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Piribedil: May diminish the therapeutic effect of Tetrabenazine. Tetrabenazine may diminish the therapeutic effect of Piribedil. Avoid combination
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
QT-prolonging Agents (Highest Risk): QT-prolonging Agents (Indeterminate Risk - Avoid) may enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QuiNINE: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Reserpine: May enhance the adverse/toxic effect of Tetrabenazine. Avoid combination
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Valbenazine: Tetrabenazine may enhance the adverse/toxic effect of Valbenazine. Avoid combination
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Adverse Reactions
Note: Many adverse effects are dose-related and may resolve at lower dosages. Adverse effects reported for adults with chorea associated with Huntington disease.
>10%:
Central nervous system: Drowsiness (≤17% to ≤57%), sedation (≤17% to ≤57%), depression (19% to 35%), extrapyramidal reaction (15% to 33%), fatigue (22%), insomnia (22%), akathisia (19% to 20%), anxiety (15%), falling (15%)
Gastrointestinal: Nausea (13%)
Respiratory: Upper respiratory tract infection (11%)
1% to 10%:
Central nervous system: Drug-induced Parkinson's disease (3% to 10%), equilibrium disturbance (9%), irritability (9%), abnormal gait (4%), dizziness (4%), dysarthria (4%), headache (4%), obsessive rumination (4%)
Gastrointestinal: Dysphagia (4% to 10%), vomiting (6%), decreased appetite (4%), diarrhea (2%)
Genitourinary: Dysuria (4%)
Hematologic & oncologic: Bruise (6%)
Neuromuscular & skeletal: Bradykinesia (9%)
Respiratory: Bronchitis (4%), dyspnea (4%)
Miscellaneous: Laceration (6%, head)
<1%, postmarketing, and/or case reports: Aggressive behavior (worsening), aspiration pneumonia, confusion, hyperhidrosis, hyperprolactinemia, increased serum transaminases, orthostatic dizziness, orthostatic hypotension, neuroleptic malignant syndrome, pneumonia, prolonged QT interval on ECG, restlessness, skin rash, suicidal ideation, syncope, tremor
Warnings/Precautions
Concerns related to adverse effects:
- Akathisia: Use has been associated with akathisia; monitor for signs and symptoms of restlessness and agitation. Dosage reduction or discontinuation may be necessary.
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery or driving).
- Depression/suicidal ideation: [US Boxed Warning]: Use can increase risk for depression and suicidal thoughts and behavior in patients with Huntington disease; closely monitor for emergence or worsening of depression, suicidality, or unusual behavioral changes. Use with caution in patients with a history of depression or prior suicide attempts or ideation; monitor patients closely for new or worsening signs or symptoms of depression. Use is contraindicated in patients who are actively suicidal, and in patients with untreated or inadequately treated depression. Consider discontinuing use if depression/suicidal ideation does not resolve.
- Esophageal dysmotility/aspiration: Use has been associated with esophageal dysmotility, dysphagia, and aspiration; use with caution in patients at risk of aspiration pneumonia.
- Neuroleptic malignant syndrome (NMS): Use may be associated with NMS; monitor for mental status changes, fever, muscle rigidity and/or autonomic instability. Discontinue with confirmed NMS; may recur with reintroduction of treatment; monitor carefully.
- Ophthalmic effects: Binds to melanin-containing tissues in animal studies; may result in accumulation and toxicity with extended use and long-term ophthalmic effects. Clinical relevance and monitoring recommendations are unknown.
- Orthostatic hypotension: May cause orthostatic hypotension; monitor patients at risk closely.
- Parkinsonism: May cause parkinsonism symptoms (ie, bradykinesia, hypertonia, rigidity). Dose reduction or discontinuation of therapy may be necessary.
- QT prolongation: Has been shown to prolong the QT interval alone (minimal) and with other drugs with comparable effects on the QT interval (additive). Avoid use in patients with congenital QT prolongation, a history of cardiac arrhythmias, or concomitant drugs known to cause QT prolongation.
- Tardive dyskinesia: May cause dyskinetic movements; discontinue use if signs and symptoms of tardive dyskinesia occur.
Disease-related concerns:
- Prolactin-dependent tumors: Elevates prolactin levels; use with caution in patients with breast cancer or other prolactin; dose discontinuation may be considered.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- CYP2D6 poor metabolizers: CYP2D6 poor metabolizers have increased levels of primary drug metabolites. Patients should be tested for the CYP2D6 gene prior to initiating doses >50 mg/day; maximum dosage should not exceed 50 mg/day in poor metabolizers.
- Huntington disease: May worsen mood, cognition, rigidity, and functional capacity in patients with Huntington disease, which can be difficult to differentiate from progression of the underlying disease. Underlying chorea may improve over time in some patients, thereby decreasing the need for therapy. Re-evaluate patients need for treatment by periodically assessing the effect on chorea and possible adverse effects. Dose reduction or discontinuation of therapy may be necessary.
Other warnings/precautions:
- Appropriate use: Should not be used to treat levodopa-induced dyskinesia.
Monitoring Parameters
Improvement in movement disorder; signs and/or symptoms of depression or suicide ideation; signs and/or symptoms of NMS; orthostatic blood pressure. Due to the possibility of comorbid psychiatric disorders, and potential psychiatric adverse effects, patients should be carefully monitored for potential changes in psychiatric status during therapy. CYP2D6 genotyping for evaluation of metabolizer status (for patients requiring >50 mg/day).
Pregnancy
Pregnancy Considerations
Adverse events were observed in some animal reproduction studies. Limited information related to the use of tetrabenazine in pregnancy has been located (Lubbe 1983).
Patient Education
What is this drug used for?
- It is used to treat disabling involuntary movements in Huntington's chorea.
Frequently reported side effects of this drug
- Loss of strength or energy
- Common cold symptoms
- Anxiety
- Nausea
- Vomiting
- Trouble sleeping
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Depression like thoughts of suicide, anxiety, emotional instability, confusion.
- Mood changes
- Agitation
- Panic attacks
- Behavioral changes
- Abnormal movements
- Change in balance
- Tremors
- Trouble moving
- Stiffness
- Falls
- Severe fatigue
- Restlessness
- Fast heartbeat
- Abnormal heartbeat
- Dizziness
- Passing out
- Trouble swallowing
- No menstrual periods
- Sexual dysfunction
- Confusion
- Vision changes
- Nipple discharge
- Enlarged breasts
- Neuroleptic malignant syndrome like fever, muscle cramps or stiffness, dizziness, severe headache, confusion, change in thinking, fast heartbeat, abnormal heartbeat, or sweating a lot.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.