Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
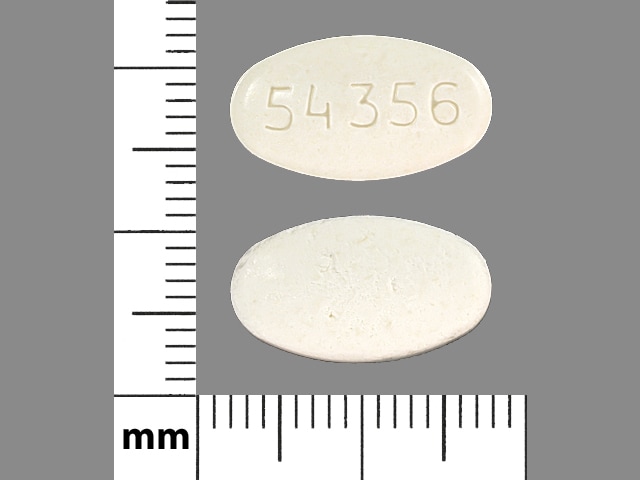
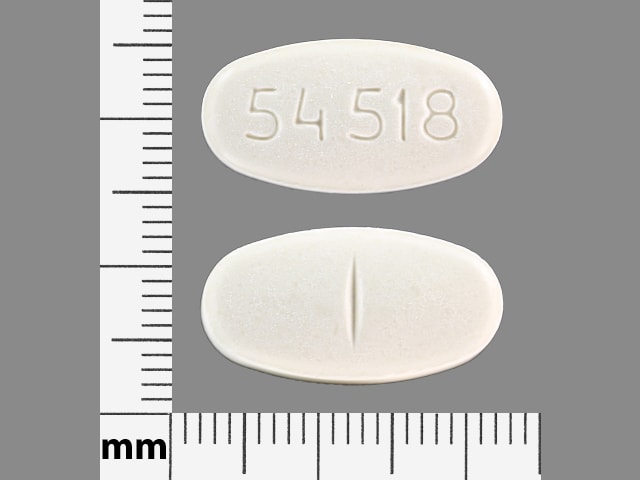
Tablet, Oral:
Valtrex: 500 mg [contains fd&c blue #2 aluminum lake]
Valtrex: 1 g [scored; contains fd&c blue #2 aluminum lake]
Generic: 500 mg, 1 g
Pharmacology
Mechanism of Action
Valacyclovir is rapidly and nearly completely converted to acyclovir by intestinal and hepatic metabolism. Acyclovir is converted to acyclovir monophosphate by virus-specific thymidine kinase then further converted to acyclovir triphosphate by other cellular enzymes. Acyclovir triphosphate inhibits DNA synthesis and viral replication by competing with deoxyguanosine triphosphate for viral DNA polymerase and being incorporated into viral DNA.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid
Distribution
Acyclovir is widely distributed throughout the body including brain, kidney, lungs, liver, spleen, muscle, uterus, vagina, and CSF
Metabolism
Hepatic; valacyclovir is rapidly and nearly completely converted to acyclovir and L-valine by first-pass effect; acyclovir is hepatically metabolized to a very small extent by aldehyde oxidase and by alcohol and aldehyde dehydrogenase (inactive metabolites)
Excretion
Urine, primarily as acyclovir (89%); Note: Following oral administration of radiolabeled valacyclovir, 46% of the label is eliminated in the feces (corresponding to nonabsorbed drug), while 47% of the radiolabel is eliminated in the urine.
Time to Peak
Children: 1.4 to 2.6 hours; Adults: 1.5 hours
Half-Life Elimination
Normal renal function: Children: 1.3 to 2.5 hours, slower clearance with increased age; Adults: 2.5 to 3.3 hours (acyclovir), ~30 minutes (valacyclovir); End-stage renal disease: 14 to 20 hours (acyclovir); During hemodialysis: 4 hours
Protein Binding
~14% to 18%
Use in Specific Populations
Special Populations: Children
Cmax ~4.2 mcg/mL in children 1 month to <12 years of age.
Use: Labeled Indications
Treatment of herpes zoster (shingles) in immunocompetent patients; treatment of first-episode and recurrent genital herpes in immunocompetent patients; suppression of recurrent genital herpes and reduction of transmission of genital herpes in immunocompetent patients; suppression of genital herpes in HIV-infected individuals; treatment of herpes labialis (cold sores); treatment of chickenpox in immunocompetent children
Use: Off Label
Bell palsy, new onsetyes
Based on the American Academy of Neurology evidence-based guideline update on steroids and antivirals for Bell palsy and the American Academy of Otolaryngology–Head and Neck Surgery Foundation clinical practice guideline on Bell palsy, valacyclovir may be considered as an adjunct to oral glucocorticoids for treatment of Bell palsy in patients who present within 72 hours of symptom onset.
Cytomegalovirus, prevention in allogeneic hematopoietic cell transplant recipientsyes
Based on the American Society of Blood and Marrow Transplantation (ASBMT) and Infectious Diseases Society of American (IDSA) guidelines for preventing infectious complications among hematopoietic cell transplant recipients, the use of valacyclovir to prevent cytomegalovirus (CMV) reactivation in allogeneic hematopoietic cell transplant (HCT) patients is effective and recommended.
Herpes simplex virus, prevention in immunocompromised patientscyes
Based on the ASBMT/IDSA guidelines for preventing infectious complications among hematopoietic cell transplant recipients, valacyclovir is an effective and recommended alternative agent to prevent herpes simplex virus (HSV) reactivation (early and late) in HCT patients.
Based on the American Society of Clinical Oncology (ASCO) and IDSA guidelines for antimicrobial prophylaxis for adult patients with cancer-related immunosuppression, valacyclovir is an effective and recommended agent to prevent HSV reactivation in patients undergoing leukemia induction therapy.
Clinical experience suggests the utility of valacyclovir for prevention of HSV in seropositive solid organ transplant recipients Wilck 2013.
Herpes zoster ophthalmicusb
Data from a multicenter, randomized study support the use of valacyclovir in the management of herpes zoster ophthalmicus in immunocompetent patients Colin 2000.
Varicella zoster virus, acute retinal necrosiscyes
Data from a limited number of patients studied suggest that valacyclovir may be beneficial for the treatment of acute retinal necrosis (ARN) caused by varicella zoster virus (VZV) Aizman 2007, Aslanides 2002.
Based on the US Department of Health and Human Services (HHS) guidelines for the prevention and treatment of opportunistic infections in HIV-infected adults and adolescents, valacyclovir, after initial treatment with IV acyclovir and intravitreal ganciclovir, is an effective and recommended agent in the management of VZV ARN in HIV-infected patients.
Varicella zoster virus, prevention in immunocompromised patientsyes
Based on the ASBMT/IDSA guidelines for preventing infectious complications among hematopoietic cell transplant recipients, valacyclovir is an effective and recommended alternative agent to prevent VZV infection in seronegative HCT recipients (<24 months after HCT or >24 months and on immunosuppressive therapy or have chronic graft-vs-host disease) who cannot receive varicella-zoster immune globulin and are exposed to varicella, zoster, or a vaccinee who develops a rash; and to prevent VZV reactivation in seropositive allogeneic and autologous HCT recipients.
Clinical experience suggests the utility of valacyclovir for prevention of VZV in seropositive solid organ transplant recipients who are not already receiving CMV or HSV prophylaxis Pergam 2013.
Contraindications
Hypersensitivity to valacyclovir, acyclovir, or any component of the formulation
Dosage and Administration
Dosing: Adult
Bell palsy, new onset (adjunctive therapy) (off-label use): Oral: 1 g 3 times daily for 7 days in combination with corticosteroids; begin within 3 days of symptom onset (AAO-HNSF [Baugh 2013]; Axelsson 2003; Engström 2008). Note: Antiviral therapy alone is not recommended (AAN [Gronseth 2012]; AAO-HNSF [Baugh 2013]); some experts only recommend addition of an antiviral to steroid therapy in patients with severe Bell palsy (de Almeida 2014; Hato 2008).
Cytomegalovirus (CMV), prevention in allogeneic hematopoietic cell transplant (HCT) recipients (alternative agent) (off-label use): High-risk patients (CMV-seropositive HCT recipients and CMV-seronegative HCT recipients with a CMV-seropositive donor): Oral: 2 g 3 to 4 times daily, beginning at engraftment and continued to day 100 (ASBMT/IDSA [Tomblyn 2009]) or 2 g 3 times daily, started after initial therapy with IV ganciclovir from day −8 to day −2 prior to transplant, and continued until engraftment or longer in patients on glucocorticoids (Milano 2001; Wingard 2018). Note: Both strategies should be combined with screening for CMV reactivation (ASBMT/IDSA [Tomblyn 2009]; Wingard 2018).
Herpes simplex virus (HSV), mucocutaneous infection:
Genital:
Immunocompetent patients:
Treatment, initial episode: Oral: 1 g twice daily for 7 to 10 days; extend duration if lesion has not healed completely after 10 days (CDC [Workowski 2015]).
Treatment, recurrent episode: Oral: 500 mg twice daily for 3 days or 1 g once daily for 5 days. Note: Treatment is most effective when initiated during the prodrome or within 1 day of lesion onset (CDC [Workowski 2015]).
Suppressive therapy (eg, for severe and/or frequent recurrences): Oral: 500 mg or 1 g once daily. Note: Reassess need periodically (eg, annually). The 500 mg daily dose may be less effective in patients who experience very frequent (≥10) recurrences per year (CDC [Workowski 2015]).
Immunocompromised patients (including HIV-infected):
Treatment, initial or recurrent episode: Oral: 1 g twice daily for 5 to 10 days; extend treatment duration if lesions have not healed completely after 10 days. Note: Severe disease should be treated with IV acyclovir for the first 2 to 7 days; may switch to valacyclovir when lesions begin to regress and continue for at least 10 days total and until lesions have resolved completely (CDC [Workowski 2015]; HHS [OI adult 2018]).
Suppressive therapy (eg, for severe and/or frequent recurrences): Oral: 500 mg twice daily. Note: Reassess need periodically (eg, annually) (CDC [Workowski 2015]; HHS [OI adult 2018]).
Pregnant females:
Treatment, initial episode (alternative agent): Oral: 1 g twice daily for 7 to 10 days; extend duration if lesion has not healed completely after 10 days (ACOG 2007; Riley 2018).
Treatment, recurrent episode (symptomatic) (alternative agent): Oral: 500 mg twice daily for 3 days or 1 g once daily for 5 days (ACOG 2007). Note: Some experts reserve treatment of recurrent episodes for patients with severe and/or frequent symptoms (Riley 2018).
Suppressive therapy, for patients with a genital HSV lesion anytime during pregnancy (alternative agent): Oral: 500 mg twice daily, beginning at 36 weeks' gestation and continued until onset of labor (ACOG 2007; CDC [Workowski 2015]; Riley 2018). Note: Some experts offer suppressive therapy earlier than 36 weeks' gestation for women who have a first-episode lesion during the third trimester (Riley 2018).
Orolabial:Note: Initiate therapy at earliest symptom.
Immunocompetent patients:
Cold sores (herpes labialis): Oral: 2 g twice daily for 1 day (manufacturer's labeling)
Primary infection (eg, gingivostomatitis): Oral: 1 g twice daily for 7 to 10 days (Klein 2018)
Suppressive therapy (eg, for severe and/or frequent recurrences): Oral: 500 mg or 1 g once daily (Baker 2003; Gilbert 2007). Note: Reassess need periodically (eg, annually) (HHS [OI adult 2018]).
Immunocompromised patients (including HIV-infected):
Treatment, initial or recurrent episode: Oral: 1 g twice daily for 5 to 10 days and until complete lesion resolution (HHS [OI adult 2018])
Suppressive therapy (eg, for severe and/or frequent recurrences): Oral: 500 mg twice daily. Note: Reassess need periodically (eg, annually) (HHS [OI adult 2018]).
Herpes simplex virus, prevention in immunocompromised patients (off-label use):
Seropositive HCT recipients (allogeneic or autologous) or seropositive patients undergoing leukemia induction chemotherapy: Oral: 500 mg twice daily (ASBMT/IDSA [Tomblyn 2009]; Wingard 2018). Initiate with the chemotherapeutic or conditioning regimen and continue until recovery of WBC count and resolution of mucositis; duration may be extended in patients with frequent recurrences or graft-vs-host disease (GVHD) (ASBMT/IDSA [Tomblyn 2009]; ASCO/IDSA [Taplitz 2018]).
Solid organ transplant recipients (HSV-seropositive patients who do not require CMV prophylaxis): Oral: 500 mg twice daily for at least 1 month (Wilck 2013); some experts recommend continuing for 3 to 6 months after transplantation and during periods of lymphodepletion associated with treatment of rejection (Fishman 2018).
Herpes zoster (shingles), treatment:
Immunocompetent patients: Oral: 1 g 3 times daily for 7 days. Initiate at earliest sign or symptom; treatment is most effective when initiated ≤72 hours after rash onset, but may initiate treatment >72 hours after rash onset if new lesions are continuing to appear (Cohen 1999).
Immunocompromised patients (including HIV-infected):
Acute localized dermatomal: Oral: 1 g 3 times daily for 7 to 10 days; consider longer duration if lesions resolve slowly (HHS [OI adult 2018]; Pergam 2013).
Extensive cutaneous lesions or visceral involvement: Oral: 1 g 3 times daily to complete a 10- to 14-day course. Note: Patients should receive initial treatment with IV acyclovir; when formation of new lesions has ceased and signs/symptoms of visceral infection are improving, may then switch to valacyclovir (HHS [OI adult 2018]; Pergam 2013).
Herpes zoster ophthalmicus (off-label use): Immunocompetent patients: Oral: 1 g 3 times daily for 7 days (Colin 2000). Note: Immunocompromised patients and patients who require hospitalization for sight-threatening disease should receive IV acyclovir (Albrecht 2018b).
Varicella (chickenpox), uncomplicated, treatment (off-label): Oral: 1 g 3 times daily. Note: Ideally initiate therapy within 24 hours of symptom onset, but may start later if patient still has active skin lesions; continue treatment for at least 5 to 7 days and until all lesions have crusted. Immunocompromised patients generally require IV acyclovir; however, for patients with uncomplicated or mild disease (<50 lesions), some experts treat with valacyclovir (Albrecht 2018a; HHS [OI adult 2018]).
Varicella zoster virus (VZV), acute retinal necrosis (off-label use): Oral: 1 g 3 times daily for approximately 6 weeks (following initial treatment with IV acyclovir) (Aizman 2007; Albrecht 2018b; Aslanides 2002; HHS [OI adult 2018]); in HIV-infected patients, intravitreal ganciclovir should be added (HHS [OI adult 2018]).
Varicella zoster virus, prevention in immunocompromised patients (off-label use):
HCT recipients (allogeneic and autologous):
Postexposure prophylaxis: Oral: 1 g 3 times daily; initiate within 96 hours (preferably within 48 hours) of exposure and continue until 22 days after exposure. Note: Indicated following exposure if varicella-zoster immune globulin is unavailable in seronegative HCT recipients who are <24 months after HCT or >24 months after HCT and on immunosuppressive therapy or have chronic GVHD (ASBMT/IDSA [Tomblyn 2009]).
Prevention of VZV reactivation in seropositive patients: Oral: 500 mg twice daily for 1 year following transplantation; may extend duration in patients requiring ongoing immunosuppression (some experts continue prophylaxis in these patients until 6 months after discontinuation of all systemic immunosuppression) (ASBMT/IDSA [Tomblyn 2009]).
Solid organ transplant recipients (VZV-seropositive patients who do not require CMV prophylaxis): Oral: 500 mg twice daily for 3 to 6 months after transplantation and during periods of lymphodepletion associated with treatment of rejection (Fishman 2018; Pergam 2013).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Herpes labialis (cold sores), treatment:
Immunocompetent: Children ≥12 years and Adolescents: Oral: 2,000 mg every 12 hours for 1 day (2 doses); initiate at earliest symptom onset
HIV-exposed/-positive: Adolescents: Oral: 1,000 mg twice daily for 5 to 10 days (HHS [adult OI 2017])
Herpes simplex virus (HSV), genital infection; immuncompetent patients: Limited data available:
First episode; treatment: Children and Adolescents: Oral: 20 mg/kg/dose twice daily, maximum dose: 1,000 mg/dose; for 7 to 10 days (Bradley 2017; CDC [Workowski 2015])
Recurrent episodes; treatment: Begin with onset of symptoms (prodrome) or lesion appearance (CDC [Workowski 2015]): Children and Adolescents:
Patient weight <50 kg: Oral: 20 mg/kg/dose twice daily; maximum dose: 1,000 mg/dose; for 5 days (Bradley 2017)
Patient weight ≥50 kg: Oral: 1,000 mg once daily for 5 days (CDC [Workowski 2015])
Suppressive therapy: Children and Adolescents: Oral: 20 mg/kg/dose once daily; maximum dose: 1,000 mg/dose (Bradley 2017; CDC [Workowski 2015])
Herpes simplex virus (HSV), prophylaxis in immunocompromised patients (eg, HSCT or leukopenic oncology patients): Limited data available (Erard 2007; IDSA [Tomblyn 2009]): Children and Adolescents: Oral:
Early reactivation prevention: Begin at initiation of conditioning and continue until engraftment or resolution of mucositis (IDSA [Tomblyn 2009)
Patient weight <40 kg: 250 mg twice daily
Patient weight ≥40 kg: 500 mg once or twice daily; twice daily dosing should be considered in patients who are highly suppressed
Late reactivation prevention: Continue throughout the first year following HSCT (Erard 2007; IDSA [Tomblyn 2009])
Patient weight <40 kg: 250 mg twice daily
Patient weight ≥40 kg: 500 mg once or twice daily; twice daily dosing should be considered in patients who are highly suppressed
Herpes simplex virus (HSV), treatment of acute retinal disease; step-down therapy: Limited data available: Children ≥50 kg or Adolescents: Oral: 1,000 mg 3 times daily for 4 to 6 weeks; begin after completion of a 10 to 14 day intravenous acyclovir course (HHS [adult OI 2017, pediatric OI 2016])
Herpes simplex virus (HSV), treatment of mucocutaneous infection or gingivostomatitis; immunocompetent patients: Limited data available: Infants ≥3 months, Children, and Adolescents: Oral: 20 mg/kg/dose twice daily for 5 to 7 days; maximum dose: 1,000 mg/dose (Bradley 2017; Kimberlin 2010)
Mononucleosis (Epstein-Barr virus [EBV]); treatment: Limited data available; efficacy results variable: Adolescents: 1,000 mg 3 times daily; a small trial in college-aged students (age ≥18 years) showed a 14-day course of valacyclovir reduced EBV oral excretion (Balfour 2007; Bradley 2017)
Varicella (chickenpox), prophylaxis in immunocompromised patients (eg, HSCT or leukopenic oncology): Limited data available: Children and Adolescents:
Weight-directed: Oral: 15 to 30 mg/kg/dose 3 times daily (Bomgaars 2008; Nadal 2002)
Fixed dosing:
Patient weight <40 kg: Oral: 250 or 500 mg twice daily (Erard 2007; IDSA [Tomblyn 2009])
Patient weight ≥40 kg: Oral: 500 mg twice daily (Erard 2007; IDSA [Tomblyn 2009])
Postexposure prophylaxis (IDSA [Tomblyn 2009]): Note: Continue for 22 days postexposure.
Patient weight <40 kg: Oral: 500 mg 3 times daily
Patient weight ≥40 kg: Oral: 1,000 mg 3 times daily
Varicella (chickenpox), treatment in immunocompetent patients: Note: Routine use in otherwise healthy children not generally recommended; treatment of varicella may be considered in individuals at high risk for a possible moderate-severe course (eg, unvaccinated adolescents, individuals with chronic cutaneous or pulmonary conditions, patients on long-term salicylate therapy or receiving short, intermittent, or aerosolized corticosteroids (Red Book [AAP 2015]): Infants ≥3 months, Children, and Adolescents <18 years: Limited data available in patients <2 years of age: Oral: 20 mg/kg/dose 3 times daily for 5 days; maximum dose: 1,000 mg/dose; initiate within 24 hours of rash onset (Bradley 2017; Red Book [AAP 2015]
Extemporaneously Prepared
50 mg/mL Oral Suspension (ASHP Standard Concentration) (ASHP 2017)
A 50 mg/mL oral suspension may be made with tablets, Ora-Plus, and either Ora-Sweet or Ora-Sweet SF. Crush eighteen 500 mg tablets in a mortar and reduce to a fine powder. Add 5 mL portions of Ora-Plus (40 mL total) and mix to a uniform paste; transfer to a 180 mL calibrated amber glass bottle, rinse mortar with 10 mL of Ora-Plus 5 times, then add quantity of syrup (Ora-Sweet or Ora-Sweet SF) sufficient to make 180 mL. Label "shake well" and "refrigerate." Stable for 21 days refrigerated.
Fish DN, Vidaurri VA, and Deeter RG, "Stability of Valacyclovir Hydrochloride in Extemporaneously Prepared Oral Liquids," Am J Health Syst Pharm, 1999, 56(19):1957-60.10554914
Administration
If GI upset occurs, administer with meals.
Storage
Store at 15°C to 25°C (59°F to 77°F).
ValACYclovir Images
Drug Interactions
Cladribine: Agents that Undergo Intracellular Phosphorylation may diminish the therapeutic effect of Cladribine. Avoid combination
CloZAPine: CYP1A2 Inhibitors (Weak) may increase the serum concentration of CloZAPine. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Foscarnet: May enhance the nephrotoxic effect of Acyclovir-Valacyclovir. Avoid combination
Mycophenolate: Acyclovir-Valacyclovir may increase the serum concentration of Mycophenolate. Mycophenolate may increase the serum concentration of Acyclovir-Valacyclovir. Monitor therapy
Talimogene Laherparepvec: Antiherpetic Antivirals may diminish the therapeutic effect of Talimogene Laherparepvec. Monitor therapy
Tenofovir Products: Acyclovir-Valacyclovir may increase the serum concentration of Tenofovir Products. Tenofovir Products may increase the serum concentration of Acyclovir-Valacyclovir. Monitor therapy
Theophylline Derivatives: CYP1A2 Inhibitors (Weak) may increase the serum concentration of Theophylline Derivatives. Exceptions: Dyphylline. Monitor therapy
TiZANidine: CYP1A2 Inhibitors (Weak) may increase the serum concentration of TiZANidine. Management: Avoid these combinations when possible. If combined use is necessary, initiate tizanidine at an adult dose of 2 mg and increase in 2 to 4 mg increments based on patient response. Monitor for increased effects of tizanidine, including adverse reactions. Consider therapy modification
Varicella Virus Vaccine: Acyclovir-Valacyclovir may diminish the therapeutic effect of Varicella Virus Vaccine. Management: When possible, avoid use of acyclovir or valacyclovir within the 24 hours prior to administration of the varicella vaccine, and avoid use of these antiviral agents for 14 days after vaccination. Avoid combination
Zidovudine: Acyclovir-Valacyclovir may enhance the CNS depressant effect of Zidovudine. Monitor therapy
Zoster Vaccine (Live/Attenuated): Acyclovir-Valacyclovir may diminish the therapeutic effect of Zoster Vaccine (Live/Attenuated). Management: When possible, discontinue antiviral agents with anti-zoster activity (i.e., acyclovir, valacyclovir, famciclovir) for at least 24 hours prior to and 14 days after receiving a live attenuated zoster vaccine. Avoid combination
Adverse Reactions
>10%:
Central nervous system: Headache (13% to 38%)
Gastrointestinal: Nausea (5% to 15%), abdominal pain (1% to 11%)
Hepatic: Increased serum AST (2% to 16%), increased serum ALT (≤14%)
Respiratory: Nasopharyngitis (≤16%)
1% to 10%:
Central nervous system: Fatigue (≤8%), depression (≤7%), dizziness (2% to 4%)
Dermatologic: Skin rash (≤8%)
Endocrine & metabolic: Dehydration (children: 2%)
Gastrointestinal: Vomiting (≤6%), diarrhea (children: 5%; adults: <1%)
Genitourinary: Dysmenorrhea (≤8%)
Hematologic & oncologic: Thrombocytopenia (≤3%), leukopenia (≤1%; mild)
Hepatic: Increased serum alkaline phosphatase (≤4%)
Infection: Herpes simplex infection (children: 2%)
Neuromuscular & skeletal: Arthralgia (≤6%)
Respiratory: Rhinorrhea (children: 2%)
Miscellaneous: Fever (children: 4%)
<1%, postmarketing, and/or case reports: Aggressive behavior, agitation, alopecia, anemia, aplastic anemia, ataxia, brain disease, coma, confusion, delirium, dysarthria, erythema multiforme, facial edema, hallucination (auditory and visual), hemolytic-uremic syndrome, hepatitis, hypersensitivity reaction (acute; includes anaphylaxis, angioedema, dyspnea, pruritus, skin rash, urticaria), hypertension, hypersensitivity angiitis, increased serum creatinine, loss of consciousness, mania, psychosis, renal failure, renal pain, seizure, skin photosensitivity, tachycardia, thrombotic thrombocytopenic purpura, tremor, urinary urgency, visual disturbance
Warnings/Precautions
Concerns related to adverse effects:
- CNS effects: CNS adverse effects (including agitation, hallucinations, confusion, delirium, seizures, and encephalopathy) have been reported in both adult and pediatric patients with or without renal dysfunction. Elderly patients are more likely to experience CNS adverse effects.
- Thrombotic microangiopathy: Has occurred in immunocompromised patients (at doses of 8 g/day).
Disease-related concerns:
- Renal impairment: Use caution in patients with renal impairment, the elderly, and/or those receiving nephrotoxic agents. Acute renal failure and CNS effects have been observed in patients with renal dysfunction; dose adjustment may be required. Precipitation in renal tubules may occur; maintain adequate hydration.
Special populations:
- Elderly: Use with caution in the elderly; CNS effects have been reported.
- Immunocompromised patients: Advanced HIV (CD4 <100 cells/mm3): Safety and efficacy have not been established for treatment/suppression of recurrent genital herpes or disseminated herpes in patients with profound immunosuppression.
Other warnings/precautions:
- Appropriate use: For cold sores, treatment should begin at the earliest symptom (tingling, itching, burning). For genital herpes, treatment should begin as soon as possible after the first signs and symptoms (within 72 hours of onset of first diagnosis or within 24 hours of onset of recurrent episodes). For herpes zoster, treatment should begin within 72 hours of onset of rash. For chickenpox, treatment should begin with earliest sign or symptom.
Monitoring Parameters
Urinalysis, BUN, serum creatinine, liver enzymes, and CBC
Pregnancy
Pregnancy Considerations
Valacyclovir is metabolized to acyclovir. In a pharmacokinetic study, maternal acyclovir serum concentrations were higher in pregnant females receiving valacyclovir than those given acyclovir for the suppression of recurrent herpes simplex virus (HSV) infection late in pregnancy. Amniotic fluid concentrations were also higher; however, there was no evidence that fetal exposure differed between the groups (Kimberlin 1998).
Data from an acyclovir pregnancy registry have shown no increased rate of birth defects than that of the general population; however, there are insufficient data regarding miscarriage or adverse maternal or fetal outcomes.
Untreated herpes simplex during pregnancy increases the risk for fetal complications, including (but not limited to) neonatal chorioretinitis, microcephaly, and skin lesions. Rarely, transplacental transmission resulting in congenital infection may occur. In addition, maternal coinfection with HSV increases the risk for perinatal HIV transmission.
Because more data is available for acyclovir, that agent is preferred for the treatment of genital herpes in pregnant females (CDC [Workowski 2015]); however, valacyclovir may be considered for use due to its simplified dosing schedule (HHS [OI adult 2018]). Pregnant females who have a history of genital herpes recurrence, suppressive therapy is recommended starting at 36 weeks' gestation (HHS [OI adult 2018]).
Patient Education
What is this drug used for?
- It is used to treat herpes infections.
- It is used to treat shingles.
- It is used to treat cold sores.
- It is used to treat chickenpox.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Headache
- Nausea
- Vomiting
- Dizziness
- Fatigue
- Abdominal pain
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Kidney problems like unable to pass urine, blood in urine, change in amount of urine passed, or weight gain.
- Confusion
- Behavioral changes
- Mood changes
- Sensing things that seem real but are not
- Tremors
- Difficulty moving
- Rigidity
- Thrombotic thrombocytopenic purpura/hemolytic uremic syndrome like bruising or bleeding; feeling very tired or weak; dark urine or yellow skin or eyes; pale skin; change in the amount of urine passed; vision changes; change in strength on one side is greater than the other, trouble speaking or thinking, change in balance; or fever
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.