Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule Extended Release 12 Hour, Oral:
Diamox Sequels: 500 mg [DSC]
Generic: 500 mg
Solution Reconstituted, Injection:
Generic: 500 mg (1 ea)
Solution Reconstituted, Injection [preservative free]:
Generic: 500 mg (1 ea)
Tablet, Oral:
Generic: 125 mg, 250 mg
Pharmacology
Mechanism of Action
Reversible inhibition of the enzyme carbonic anhydrase resulting in reduction of hydrogen ion secretion at renal tubule and an increased renal excretion of sodium, potassium, bicarbonate, and water. Decreases production of aqueous humor and inhibits carbonic anhydrase in central nervous system to retard abnormal and excessive discharge from CNS neurons.
Pharmacokinetics/Pharmacodynamics
Absorption
Appears to be dose dependent; erratic with daily doses >10 mg/kg
Distribution
Erythrocytes, kidneys; blood-brain barrier and placenta; distributes into milk (~30% of plasma concentrations)
Excretion
Urine (70% to 100% [IV, tablet], 47% [extended release capsule] as unchanged drug within 24 hours)
Onset of Action
Capsule (extended release): 2 hours; Tablet (immediate release): 1 to 1.5 hours; IV: 2 to 10 minutes
Peak effect: Capsule (extended release): 8 to 18 hours; IV: 15 minutes; Tablet: 2 to 4 hours
Time to Peak
Plasma: Capsule (extended release): 3 to 6 hours; Tablet: 1 to 4 hours; IV: 15 minutes
Duration of Action
Inhibition of aqueous humor secretion: Capsule (extended release): 18 to 24 hours; IV: 4 to 5 hours; Tablet: 8 to 12 hours
Half-Life Elimination
2.4 to 5.8 hours
Protein Binding
95%
Use: Labeled Indications
Altitude illness: Prevention or amelioration of symptoms associated with acute mountain sickness (immediate and extended release dosage forms)
Edema: Adjunctive treatment of drug-induced edema or edema due to congestive heart failure (IV and immediate release dosage forms)
Elevated intraocular pressure: Treatment of elevated intraocular pressure (IOP) in patients with chronic open-angle glaucoma or acute angle-closure glaucoma prior to surgery or as part of a 4-drug medical management regimen when a patient cannot be seen by an ophthalmologist for ≥1 hour
Epilepsy: Adjunctive treatment of centrencephalic epilepsies (IV and immediate release dosage forms)
Use: Off Label
Familial periodic paralysisc
Limited data from controlled trials and case reports suggest that acetazolamide may have some benefits in the treatment of hypokalemic and hyperkalemic periodic paralysis. Studies have shown that acetazolamide improves muscle strength in patients with hypokalemic periodic paralysis. In patients with hyperkalemic periodic paralysis, acetazolamide may decrease the steady-state potassium exchange rates and increase potassium uptake by other tissues, resulting in protection from hyperkalemic paralysis Hoskins 1974, Links 1988, Venance 2004. Further controlled studies enrolling more patients are needed to determine the role of acetazolamide in the treatment of familial periodic paralysis.
Hydrocephalus, normal-pressurec
Data from a limited number of patients in a retrospective review suggest that low-dose acetazolamide can reduce periventricular hyperintensities leading to gait improvement in patients with normal pressure hydrocephalus Alperin 2014. Additional data may be necessary to further define the role of acetazolamide in this condition.
Idiopathic intracranial hypertensionb
Data from a multicenter, randomized, double-masked, placebo-controlled study supports the use of acetazolamide (in combination with weight reduction and low sodium diet) in patients with idiopathic intracranial hypertension (III) and mild vision loss. In this study acetazolamide was associated with modest improvement in the primary endpoint of perimetric visual field function as well as secondary endpoints of papilledema grade, cerebrospinal fluid pressure, and vision-related quality of life measured at 6 months Wall 2014. Additional data may be necessary to further define the role of acetazolamide in this condition.
Metabolic alkalosisb
Data from a randomized placebo-controlled, double blinded study in critically-ill medical patients Mazur 1999 and an open label, uncontrolled, unblinded study Marik 1991 supports the use of acetazolamide in the treatment of metabolic alkalosis. Additional trials may be necessary to further define the role of acetazolamide in this condition.
Prevention of cystine renal calculi (adjunctive therapy)c
Data from a limited number of patients in a retrospective review suggest that acetazolamide may have some benefits as adjunctive therapy for urinary alkalinization in the prevention of cystine renal calculi formation in patients who are recalcitrant to potassium citrate therapy. Additional data may be necessary to further define the role of acetazolamide in this condition.
Respiratory stimulant in stable hypercapnic COPDb
Data from a randomized, double-blind, crossover study supports the use of acetazolamide as a respiratory stimulant in the treatment of stable hypercapnic COPD Wagenaar 2003. Additional trials may be necessary to further define the role of acetazolamide in this condition.
Contraindications
Hypersensitivity to acetazolamide, sulfonamides, or any component of the formulation; marked hepatic disease or insufficiency; decreased sodium and/or potassium levels; adrenocortical insufficiency; cirrhosis; hyperchloremic acidosis; severe renal disease or dysfunction; long-term use in noncongestive angle-closure glaucoma
Note: Although the FDA approved product labeling states this medication is contraindicated with other sulfonamide-containing drug classes, the scientific basis of this statement has been challenged. See “Warnings/Precautions” for more detail.
Canadian labeling: Additional contraindications not in US labeling: Hemorrhagic glaucoma; glaucoma due to peripheral anterior synechias; metabolic acidosis.
Dosage and Administration
Dosing: Adult
Note: IM administration is not recommended because of pain secondary to the alkaline pH.
Altitude illness: Oral:
Prevention: 125 mg twice daily; beginning either the day before (preferred) or on the day of ascent; may be discontinued after staying at the same elevation for 2 to 3 days or if descent initiated (Basnyat 2006; Luks 2010). Note: In situations of rapid ascent (such as rescue or military operations), 1,000 mg/day is recommended by the manufacturer. The Wilderness Medical Society recommends consideration of using dexamethasone in addition to acetazolamide in these situations (Luks 2010).
Treatment: 250 mg twice daily. Note: With high altitude cerebral edema, dexamethasone is the primary treatment; however, acetazolamide may be used adjunctively with the same treatment dose (Luks 2010).
Manufacturer's labeling: Dosing in the prescribing information may not reflect current clinical practice. 500 to 1,000 mg/day in divided doses every 8 to 12 hours (immediate release tablets) or divided every 12 to 24 hours (extended release capsules).
Edema: Oral, IV: 250 to 375 mg once daily
Elevated intraocular pressure:
Angle-closure glaucoma, acute: Oral (immediate release) or IV: 500 mg as part of a 4-drug regimen (Pokhrel 2007; Weizer 2019). Note: Reserve medical management for emergency situations when an assessment by an ophthalmologist will be delayed by ≥1 hour (Pokhrel 2007; Weizer 2019).
Open-angle glaucoma: Oral: 250 mg 1 to 4 times/day (immediate release) or 500 mg twice daily (extended release). Note: Reserve for management of acute ocular pressure increases, including after surgery or trauma (Zhang 2017).
Epilepsy: Oral: 8 to 30 mg/kg/day in divided doses. A lower dosing range of 4 to 16 mg/kg/day in 1 to 4 divided doses has also been recommended; maximum dose: 30 mg/kg/day or 1 g/day (Oles 1989; Reiss 1996). Note: Minimal additional benefit with doses >16 mg/kg/day. Extended release capsule is not recommended for treatment of epilepsy.
Familial periodic paralysis (off-label use): Oral: 125 mg 3 times daily (Links 1988) or 250 mg once daily (Venance 2004) or 250 mg every 6 hours (Hoskins 1974). Additional data may be necessary to further define the role of acetazolamide in the treatment of this condition.
Hydrocephalous, normal pressure (off-label use): Oral: Initial: 125 mg/day; may increase dose up to 375 mg/day (Alperin 2014).
Idiopathic intracranial hypertension (off-label use): Oral: Initial: 500 mg twice daily; may increase dose as tolerated at intervals of 250 mg/week, up to 4,000 mg/day (Wall 2014).
Metabolic alkalosis (off-label use): IV: 500 mg as a single dose; reassess need based upon acid-base status (Marik 1991; Mazur 1999)
Prevention of cystine renal calculi (adjunctive therapy) (off-label use): Oral: 500 mg daily at bedtime in combination with potassium citrate and captopril (Sterrett 2008)
Respiratory stimulant in stable hypercapnic COPD (off-label use): Oral: 250 mg twice daily (Wagenaar 2003)
Dosing: Geriatric
Refer to adult dosing. Oral: Initial doses should begin at the low end of the dosage range.
Dosing: Pediatric
Altitude illness, acute:
Prevention: Limited data available: Infants, Children, and Adolescents: Oral: Immediate release: 2.5 mg/kg/dose every 12 hours started either the day before (preferred) or on the day of ascent and may be discontinued after staying at the same elevation for 2 to 3 days or if descent initiated; maximum dose: 125 mg/dose (Luks 2010). Note: The International Society for Mountain Medicine does not recommend prophylaxis in children except in the rare circumstance of unavoidable rapid ascent or in children with known previous susceptibility to acute mountain sickness (Pollard 2001). Higher doses are effective up to 500 mg, but are also associated with increased adverse effects and not recommended (Luks 2010).
Treatment: Acute mountain sickness (AMS); moderate: Limited data available: Infants, Children, and Adolescents: Oral: Immediate release: 2.5 mg/kg/dose every 8 to 12 hours; maximum dose: 250 mg/dose. Note: With high altitude cerebral edema, dexamethasone is the primary treatment; however, acetazolamide may be used adjunctively with the same treatment dose (Luks 2010; Pollard 2001).
Glaucoma:
Children <12 years: Limited data available: Oral: Immediate release: 10 to 30 mg/kg/day divided every 6 to 8 hours; maximum daily dose: 1,000 mg/day (Portellos 1998; Sabri 2006).
Children ≥12 years and Adolescents: Oral:
Immediate release: Limited data available: 15 to 30 mg/kg/day in divided doses every 6 to 8 hours; maximum daily dose: 1,000 mg/day.
Extended release (Diamox sequels):
Manufacturer's labeling: 500 mg twice daily.
Alternate dosing: Weight-directed dosing: Limited data available: 15 to 30 mg/kg/day in divided doses twice daily; maximum daily dose: 1,000 mg/day (Pagliaro 2002; Sabri 2006).
Edema: Limited data available: Infants, Children, and Adolescents: Oral (immediate release), IV: 5 mg/kg/dose once daily or every other day in the morning (Park 2014).
Epilepsy, short-term management: Limited data available: Infants, Children, and Adolescents: Oral: Immediate release: Usual range: 4 to 16 mg/kg/day in 3 to 4 divided doses; may titrate; maximum daily dose: 30 mg/kg/day or 1,000 mg/day (whichever is less) (Reiss 1996); Note: Minimal additional benefit with doses >16 mg/kg/day.
Metabolic alkalosis: Limited data available; dosing regimens variable: Infants, Children, and Adolescents: IV, Oral (immediate release): 5 mg/kg/dose once daily for 3 doses been used in a prospective trial of postcardiac surgical patients (age range: 8 days to 20 months) and results showed a significant decrease in serum bicarbonate concentrations (Moffett 2007). A retrospective trial of 34 pediatric patients (mean age: 1.9 years; range: 18 days to 12 years) reported a mean effective dose of 5.4 mg/kg/dose every 6 to 8 hours; a trend showed every 6-hour dosing had a higher success rate but not statistically significant (Andrews 2013). In adults, the reported dosing is 500 mg as a single dose (Marik 1991; Moviat 2006).
Pseudotumor cerebri: Limited data available:
Children: Oral: Immediate release: Usual reported initial dose: 15 to 25 mg/kg/day in 2 to 3 divided doses; may increase if needed to a maximum daily dose: 100 mg/kg/day or 2,000 mg/day (whichever is less); therapy continued until resolution of headache, disc swelling, and visual field abnormalities; usually several months (eg, 3 to 9 months) (Distelmaier 2006; Hacifazlioglu 2012; Ko 2010; Per 2013; Rangwala 2007; Soler 1998; Spennato 2011; Standridge 2010).
Adolescents: Oral: Immediate release: Initial: 500 mg twice daily; may increase if needed; maximum daily dose: 4,000 mg/day; usual adult dose range: 1,000 to 4,000 mg/day in 2 to 4 divided doses (Phillips 2012; Standridge 2010).
Reconstitution
Injection: Reconstitute with at least 5 mL sterile water to provide a solution containing not more than 100 mg/mL.
Extemporaneously Prepared
A 25 mg/mL oral suspension may be made with tablets and either a 1:1 mixture of Ora-Sweet® and Ora-Plus® or a 1:1 mixture of Ora-Sweet® SF and Ora-Plus®. Crush twelve 250 mg tablets in a mortar and reduce to a fine powder. Add small portions of chosen vehicle and mix to a uniform paste; mix while adding the vehicle in incremental proportions to almost 120 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 120 mL. Label “shake well” and “refrigerate”. Stable for 60 days (Allen, 1996). When diluted in 120 mL solution of cherry syrup concentrate diluted 1:4 with simple syrup, NF, it is stable 60 days refrigerated (preferred) or at room temperature (Nahata, 2004).
Allen LV Jr and Erickson MA 3rd, "Stability of Acetazolamide, Allopurinol, Azathioprine, Clonazepam, and Flucytosine in Extemporaneously Compounded Oral Liquids," Am J Health Syst Pharm, 1996, 53(16):1944-9.8862208Nahata MC, Pai VB, and Hipple TF, Pediatric Drug Formulations, 5th ed, Cincinnati, OH: Harvey Whitney Books Co, 2004.
Administration
Oral: May be administered with food. May cause an alteration in taste, especially carbonated beverages. Short-acting tablets may be crushed and suspended in cherry or chocolate syrup to disguise the bitter taste of the drug; do not use fruit juices. Alternatively, submerge tablet in 10 mL of hot water and add 10 mL honey or syrup.
IM: IM administration is painful because of the alkaline pH of the drug; use by this route is not recommended.
IV: Direct IV injection is the preferred parenteral route of administration. Specific IV push rates are not provided in the manufacturer's labeling. However, an IV push rate of up to 500 mg over 3 minutes has been reported in a clinical trial (Mazur 1999). Additionally, a study to assess cerebrovascular reserve used a rapid IV push of up to 1 g over ≤1 minute (Piepgras 1990).
Dietary Considerations
May be taken with food to decrease GI upset. May have additive effects with other folic acid antagonists. Some products may contain sodium.
Storage
Capsules, tablets: Store at controlled room temperature.
Injection: Store intact vials at 20°C to 25°C (68°F to 77°F). Store reconstituted solutions for 3 days under refrigeration at 2°C to 8°C (36°F to 46°F), or 12 hours at room temperature, 20°C to 25°C (68°F to 77°F).
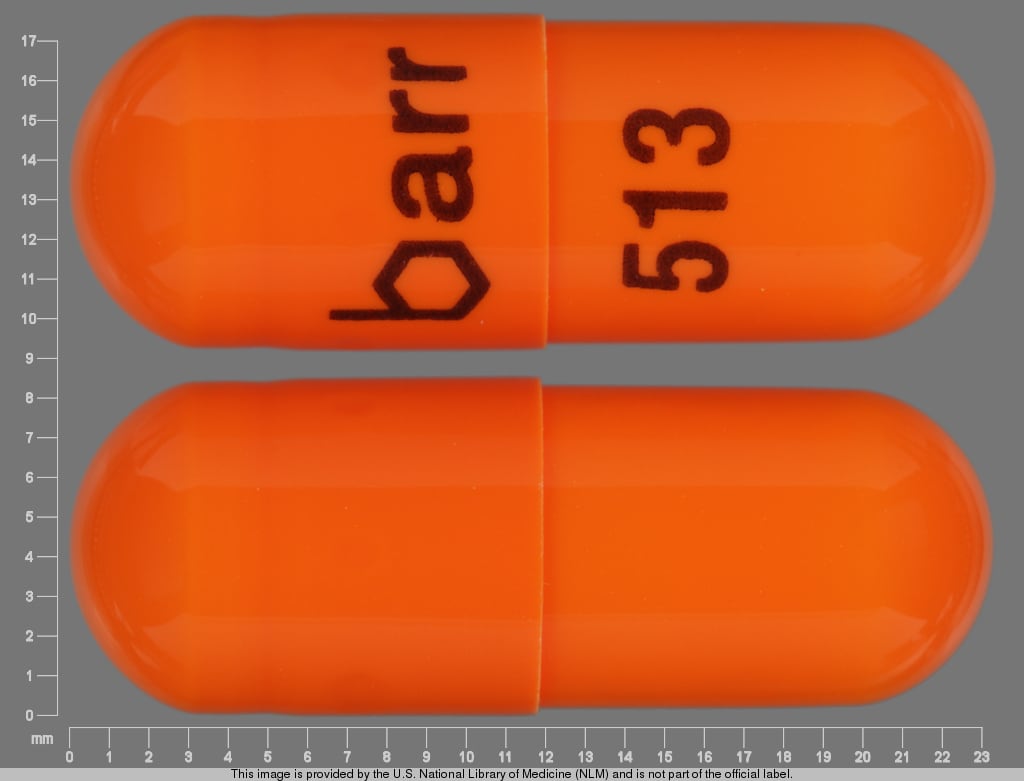
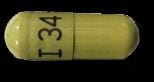
AcetaZOLAMIDE Images
Drug Interactions
Ajmaline: Sulfonamides may enhance the adverse/toxic effect of Ajmaline. Specifically, the risk for cholestasis may be increased. Monitor therapy
Alpha-/Beta-Agonists (Indirect-Acting): Carbonic Anhydrase Inhibitors may increase the serum concentration of Alpha-/Beta-Agonists (Indirect-Acting). Monitor therapy
Amantadine: Carbonic Anhydrase Inhibitors may increase the serum concentration of Amantadine. Monitor therapy
Amphetamines: Carbonic Anhydrase Inhibitors may decrease the excretion of Amphetamines. Monitor therapy
CarBAMazepine: Carbonic Anhydrase Inhibitors may increase the serum concentration of CarBAMazepine. Monitor therapy
Carbonic Anhydrase Inhibitors: May enhance the adverse/toxic effect of other Carbonic Anhydrase Inhibitors. The development of acid-base disorders with concurrent use of ophthalmic and oral carbonic anhydrase inhibitors has been reported. Management: Avoid concurrent use of different carbonic anhydrase inhibitors if possible. Monitor patients closely for the occurrence of kidney stones and with regards to severity of metabolic acidosis. Avoid combination
CycloSPORINE (Systemic): AcetaZOLAMIDE may increase the serum concentration of CycloSPORINE (Systemic). Monitor therapy
Dexketoprofen: May enhance the adverse/toxic effect of Sulfonamides. Monitor therapy
Diacerein: May enhance the therapeutic effect of Diuretics. Specifically, the risk for dehydration or hypokalemia may be increased. Monitor therapy
Flecainide: Carbonic Anhydrase Inhibitors may increase the serum concentration of Flecainide. Monitor therapy
Fosphenytoin-Phenytoin: Carbonic Anhydrase Inhibitors may enhance the adverse/toxic effect of Fosphenytoin-Phenytoin. Specifically, the risk for osteomalacia or rickets may be increased. Monitor therapy
Lithium: Carbonic Anhydrase Inhibitors may decrease the serum concentration of Lithium. Monitor therapy
Mecamylamine: Sulfonamides may enhance the adverse/toxic effect of Mecamylamine. Avoid combination
Mefloquine: May diminish the therapeutic effect of Anticonvulsants. Mefloquine may decrease the serum concentration of Anticonvulsants. Management: Mefloquine is contraindicated for malaria prophylaxis in persons with a history of convulsions. Monitor anticonvulsant concentrations and treatment response closely with concurrent use. Consider therapy modification
Memantine: Carbonic Anhydrase Inhibitors may increase the serum concentration of Memantine. Monitor therapy
MetFORMIN: Carbonic Anhydrase Inhibitors may enhance the adverse/toxic effect of MetFORMIN. Specifically, the risk of developing lactic acidosis may be increased. Monitor therapy
Methenamine: Carbonic Anhydrase Inhibitors may diminish the therapeutic effect of Methenamine. Management: Consider avoiding this combination. Monitor for decreased therapeutic effects of methenamine if used concomitant with a carbonic anhydrase inhibitor. Consider therapy modification
Mianserin: May diminish the therapeutic effect of Anticonvulsants. Monitor therapy
Opioid Agonists: May enhance the adverse/toxic effect of Diuretics. Opioid Agonists may diminish the therapeutic effect of Diuretics. Monitor therapy
Orlistat: May decrease the serum concentration of Anticonvulsants. Monitor therapy
Primidone: Carbonic Anhydrase Inhibitors may enhance the adverse/toxic effect of Primidone. Specifically, osteomalacia and rickets. Carbonic Anhydrase Inhibitors may decrease the serum concentration of Primidone. Monitor therapy
QuiNIDine: Carbonic Anhydrase Inhibitors may decrease the excretion of QuiNIDine. Monitor therapy
Salicylates: May enhance the adverse/toxic effect of Carbonic Anhydrase Inhibitors. Salicylate toxicity might be enhanced by this same combination. Management: Avoid these combinations when possible.Dichlorphenamide use with high-dose aspirin as contraindicated. If another combination is used, monitor patients closely for adverse effects. Tachypnea, anorexia, lethargy, and coma have been reported. Consider therapy modification
Sodium Bicarbonate: AcetaZOLAMIDE may enhance the adverse/toxic effect of Sodium Bicarbonate. Specifically, the risk of renal calculus formation may be increased. Monitor therapy
Sodium Phosphates: Diuretics may enhance the nephrotoxic effect of Sodium Phosphates. Specifically, the risk of acute phosphate nephropathy may be enhanced. Management: Consider avoiding this combination by temporarily suspending treatment with diuretics, or seeking alternatives to oral sodium phosphate bowel preparation. If the combination cannot be avoided, hydrate adequately and monitor fluid and renal status. Consider therapy modification
Trientine: Carbonic Anhydrase Inhibitor Diuretics may decrease the serum concentration of Trientine. Monitor therapy
Test Interactions
May cause false-positive results for urinary protein with Albustix®, Labstix®, Albutest®, Bumintest®; interferes with HPLC theophylline assay and serum uric acid levels; may lead to false-negative aldosterone/renin ratio (ARR) (Funder 2016)
Adverse Reactions
Frequency not defined.
Cardiovascular: Flushing
Central nervous system: Ataxia, confusion, convulsions, depression, dizziness, drowsiness, excitement, fatigue, flaccid paralysis, headache, malaise, paresthesia
Dermatologic: Allergic skin reaction, skin photosensitivity, Stevens-Johnson syndrome, toxic epidermal necrolysis, urticaria
Endocrine & metabolic: Electrolyte imbalance, growth retardation (children), hyperglycemia, hypoglycemia, hypokalemia, hyponatremia, metabolic acidosis
Gastrointestinal: Decreased appetite, diarrhea, dysgeusia, glycosuria, melena, nausea, vomiting
Genitourinary: Crystalluria, hematuria
Hematologic and oncologic: Agranulocytosis, aplastic anemia, leukopenia, thrombocytopenia, thrombocytopenic purpura
Hepatic: Abnormal hepatic function tests, cholestatic jaundice, fulminant hepatic necrosis, hepatic insufficiency
Hypersensitivity: Anaphylaxis
Local: Pain at injection site
Ophthalmic: Myopia
Otic: Auditory disturbance, tinnitus
Renal: Polyuria, renal failure
Miscellaneous: Fever
Warnings/Precautions
Concerns related to adverse effects:
- CNS effects: Impairment of mental alertness and/or physical coordination may occur.
- Sulfonamide (“sulfa”) allergy: The FDA-approved product labeling for many medications containing a sulfonamide chemical group includes a broad contraindication in patients with a prior allergic reaction to sulfonamides. There is a potential for cross-reactivity between members of a specific class (eg, two antibiotic sulfonamides). However, concerns for cross-reactivity have previously extended to all compounds containing the sulfonamide structure (SO2NH2). An expanded understanding of allergic mechanisms indicates cross-reactivity between antibiotic sulfonamides and nonantibiotic sulfonamides may not occur or at the very least this potential is extremely low (Brackett 2004; Johnson 2005; Slatore 2004; Tornero 2004). In particular, mechanisms of cross-reaction due to antibody production (anaphylaxis) are unlikely to occur with nonantibiotic sulfonamides. T-cell-mediated (type IV) reactions (eg, maculopapular rash) are less well understood and it is not possible to completely exclude this potential based on current insights. In cases where prior reactions were severe (Stevens-Johnson syndrome/TEN), some clinicians choose to avoid exposure to these classes.
Disease-related concerns:
- Diabetes: Use with caution in patients with prediabetes or diabetes mellitus; may see a change in glucose control.
- Hepatic impairment: Use with caution in patients with hepatic dysfunction; in cirrhosis, avoid electrolyte and acid/base imbalances that might lead to hepatic encephalopathy.
- Respiratory acidosis: Use with caution in patients with respiratory acidosis; may worsen acidosis.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Use with caution in the elderly; may be more sensitive to side effects.
Other warnings/precautions:
- Appropriate use: Increasing the dose does not increase diuresis and may increase the incidence of drowsiness and/or paresthesia; often results in a reduction of diuresis.
- IM administration: Painful because of the alkaline pH of the drug; use by this route is not recommended.
Monitoring Parameters
Intraocular pressure (30 to 60 minutes after administration for acute angle-closure glaucoma (Pokhrel 2007; Weizer 2019); serum electrolytes; periodic CBC with differential; monitor growth in pediatric patients
Pregnancy
Pregnancy Considerations
Limited data is available following the use of acetazolamide in pregnant women for the treatment of idiopathic intracranial hypertension (Falardeau 2013; Kesler 2013).
Pregnant women exposed to acetazolamide during pregnancy for the treatment of seizure disorders are encouraged to enroll themselves into the AED Pregnancy Registry by calling 1-888-233-2334. Additional information is available at aedpregnancyregistry.org
Patient Education
What is this drug used for?
- It is used to get rid of extra fluid.
- It is used to treat or prevent altitude sickness.
- It is used to help control certain kinds of seizures.
- It is used to treat glaucoma
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Nausea
- Vomiting
- Change in taste
- Diarrhea
- Lack of appetite
- Blurred vision
- Fatigue
- Loss of strength and energy
- Injection site pain
- Flushing
- Anxiety
- Dizziness
- Headache
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Acidosis like confusion, fast breathing, fast heartbeat, abnormal heartbeat, severe abdominal pain, nausea, vomiting, fatigue, shortness of breath, or loss of strength and energy.
- Electrolyte problems like mood changes, confusion, muscle pain or weakness, abnormal heartbeat, seizures, lack of appetite, or severe nausea or vomiting.
- High blood sugar like confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit.
- Low blood sugar like dizziness, headache, fatigue, feeling weak, shaking, fast heartbeat, confusion, increased hunger, or sweating.
- Vision changes
- Trouble hearing
- Noise or ringing in the ears
- Burning or numbness feeling
- Painful urination
- Blood in the urine
- Unable to pass urine
- Change in amount of urine passed
- Muscle weakness
- Change in balance
- Abnormal gait
- Depression
- Confusion
- Seizures
- Severe sulfonamide reaction like rash; red, swollen, blistered, or peeling skin; red or irritated eyes; mouth, throat, nose, or eye sores; fever, chills, or sore throat; cough that is new or worse; loss of strength and energy; any bruising or bleeding; or signs of liver problems like dark urine, fatigue, lack of appetite, upset stomach or stomach pain, light-colored stools, throwing up, or yellow skin.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.