Boxed Warning
Bone marrow suppression (Campath):
Serious, including fatal, pancytopenia/marrow hypoplasia, autoimmune idiopathic thrombocytopenia, and autoimmune hemolytic anemia can occur in patients receiving alemtuzumab. Single doses of alemtuzumab >30 mg or cumulative doses >90 mg per week increase the incidence of pancytopenia.
Infusion reactions (Campath):
Alemtuzumab administration can result in serious, including fatal, infusion reactions. Carefully monitor patients during infusions and withhold alemtuzumab for Grade 3 or 4 infusion reactions. Gradually escalate alemtuzumab to the recommended dose at the initiation of therapy and after interruption of therapy for ≥7 days.
Infections (Campath):
Serious, including fatal, bacterial, viral, fungal, and protozoan infections can occur in patients receiving alemtuzumab. Administer prophylaxis against Pneumocystis jirovecii pneumonia and herpes virus infections.
Autoimmune effects (Lemtrada):
Alemtuzumab causes serious, sometimes fatal, autoimmune conditions, such as immune thrombocytopenia and anti-glomerular basement membrane disease. Monitor CBC with differential, serum creatinine levels, and urinalysis with urine cell counts at periodic intervals for 48 months after the last dose of alemtuzumab.
Infusion reactions (Lemtrada):
Alemtuzumab causes serious and life-threatening infusion reactions. Alemtuzumab must be administered in a setting with appropriate equipment and personnel to manage anaphylaxis or serious infusion reactions. Monitor patients for 2 hours after each infusion. Make patients aware that serious infusion reactions can also occur after the 2-hour monitoring period.
Malignancy (Lemtrada):
Alemtuzumab may cause an increased risk of malignancies, including thyroid cancer, melanoma, and lymphoproliferative disorders. Perform baseline and yearly skin exams.
REMS program (Lemtrada):
Because of the risk of autoimmunity, infusion reactions, and malignancies, Lemtrada is available only through restricted distribution under a Risk Evaluation Mitigation Strategy (REMS) Program. Call 1-855-676-6326 to enroll in the Lemtrada REMS program.
Stroke (Lemtrada):
Serious and life-threatening stroke (including ischemic and hemorrhagic stroke) has been reported within 3 days of alemtuzumab administration. Instruct patients to seek immediate medical attention if symptoms of stroke occur.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution, Intravenous [preservative free]:
Campath: 30 mg/mL (1 mL) [contains edetate disodium dihydrate, mouse (murine) and/or hamster protein, polysorbate 80]
Lemtrada: 12 mg/1.2 mL (1.2 mL) [contains edetate disodium dihydrate, mouse (murine) and/or hamster protein, polysorbate 80]
Pharmacology
Mechanism of Action
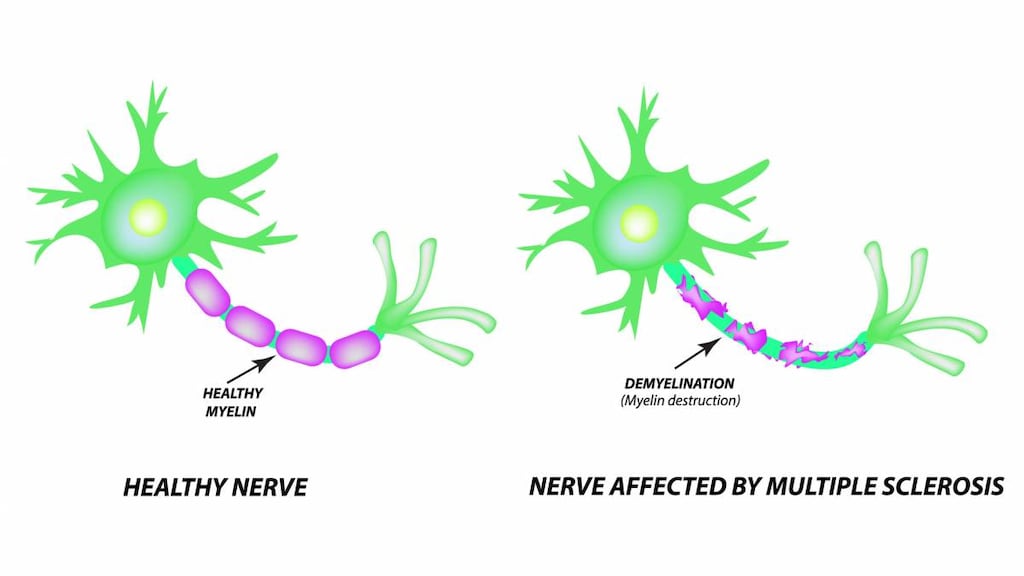
Alemtuzumab binds to CD52, a nonmodulating antigen present on the surface of B and T lymphocytes, a majority of monocytes, macrophages, NK cells, and a subpopulation of granulocytes. After binding to CD52+ cells, an antibody-dependent lysis of malignant cells occurs. In multiple sclerosis, alemtuzumab immunomodulatory effects may include alteration in the number, proportions, and properties of some lymphocyte subsets following treatment.
Pharmacokinetics/Pharmacodynamics
Distribution
Vd: IV: Campath: 0.18 L/kg (range: 0.1 to 0.4 L/kg); Lemtrada: 14.1 L
Metabolism
Campath: Clearance decreases with repeated dosing (due to loss of CD52 receptors in periphery), resulting in a sevenfold increase in AUC after 12 weeks of therapy.
Half-Life Elimination
IV: Campath: 11 hours (following first 30 mg dose; range: 2 to 32 hours); 6 days (following the last 30 mg dose; range: 1 to 14 days); Lemtrada: ~2 weeks
Use: Labeled Indications
B-cell chronic lymphocytic leukemia: Campath or MabCampath [Canadian product]: Treatment (as a single agent) of B-cell chronic lymphocytic leukemia.
Multiple sclerosis, relapsing: Lemtrada: Treatment of relapsing-remitting and active secondary progressive multiple sclerosis (MS); generally reserved for patients who have had an inadequate response to ≥2 medications indicated for the treatment of MS.
Limitations of use: Alemtuzumab is not recommended for use in patients with clinically isolated syndrome due to its safety profile.
Use: Off Label
Acute graft-versus-host disease (steroid refractory) (treatment)c
Data from a limited number of patients in two studies (one phase II and one retrospective) suggest that alemtuzumab may be beneficial for the treatment of steroid refractory acute graft-versus-host disease (aGVHD) Martinez 2009, Schnitzler 2009. Additional data may be necessary to further define the role of alemtuzumab in this condition.
Aplastic anemia, refractoryc
Data from a prospective study and a small prospective/retrospective study support the use of alemtuzumab (either as monotherapy or in combination with cyclosporine) in the management of severe refractory aplastic anemia Risitano 2009, Scheinberg 2012. Additional data may be necessary to further define the role of alemtuzumab in this condition.
Autoimmune hemolytic anemia, chronic lymphocytic leukemia (CLL)-inducedc
Data from a limited number of patients and clinical experience suggest alemtuzumab may be beneficial for the treatment of CLL-induced autoimmune hemolytic anemias Karlsson 2007, Osterborg 2009. Additional data may be necessary to further define the role of alemtuzumab in this condition.
B-cell chronic lymphocytic leukemia (B-CLL) (subcutaneous [off-label route])a
Data from two phase II open-label clinical trials support the subcutaneous use of alemtuzumab in the treatment of B-CLL Lundin 2002, Stilgenbauer 2009.
Hemophagocytic lymphohistiocytosis, refractoryc
Data from a small retrospective review suggest that alemtuzumab may be beneficial in the treatment of refractory hemophagocytic lymphohistiocytosis Marsh 2013. The optimal dosing and duration of alemtuzumab therapy is not known. Additional data may be necessary to further define the role of alemtuzumab in the management of this condition.
Mycosis fungoides/Sézary syndrome (advanced)c
Data from a small phase 2 study in patients with advanced mycosis fungoides/Sézary syndrome (primarily stage III or IV disease) suggest that alemtuzumab may have clinical activity in the treatment of this disease, particularly in patients with erythroderma/severe itching Lundin 2003. Additional data may be necessary to further define the role of alemtuzumab in this condition.
Solid organ transplantation: Heart transplant (induction)c
Data from a single center retrospective review suggest that alemtuzumab may be beneficial for prevention of rejection in heart transplant recipients when used in combination with decreased maintenance immunosuppression Teuteberg 2010. Additional data may be necessary to further define the role of alemtuzumab in this condition.
Solid organ transplantation: Lung transplant (induction)b
A retrospective analysis of data obtained from the United Network for Organ Sharing (UNOS) registry supports the use of alemtuzumab as induction therapy in patients receiving double lung transplants Furuya 2016. Data from other studies also support the use of alemtuzumab in the prevention of rejection in lung transplant recipients when followed by decreased maintenance immunosuppression Jaksch 2014, Shyu 2011, Whited 2015. Additional data may be necessary to further define the role of alemtuzumab in this condition.
Solid organ transplantation: Renal transplant (induction)a
Data from a large, prospective, multicenter randomized study support the use of alemtuzumab as induction therapy (followed by reduced maintenance immunosuppression) in the prevention of renal transplant rejection Haynes 2014.
Solid organ transplantation: Renal transplant (steroid-resistant cellular rejection)c
Data from small retrospective reviews support the use of alemtuzumab for treatment of acute steroid-resistant cellular rejection after renal transplant Basu 2005, van den Hoogen 2013
Stem cell transplant (allogeneic) conditioning regimen and/or graft-versus-host disease prophylaxisb
Data from two studies support the use of alemtuzumab in conditioning regimens for allogeneic stem cell transplantation to reduce the incidence of acute and/or chronic GVHD Mead 2010, Van Biesen 2009. Additional trials may be necessary to further define the role of alemtuzumab in this setting.
T-cell large granular lymphocytic leukemia (TLGLL)c
Data from a small prospective (single-arm) phase 2 study in patients with TLGLL suggest that alemtuzumab has activity (primarily in relapsed and refractory disease) in the treatment of this disease Dumitriu 2016. Additional trials may be necessary to further define the role of alemtuzumab in this setting.
T-cell prolymphocytic leukemia (T-PLL)a
Data from two studies support the use of alemtuzumab in the treatment of T-PLL Deardon 2001, Keating 2002.
Contraindications
US labeling: Lemtrada is contraindicated in patients infected with HIV (due to prolonged reduction in CD4+ lymphocytes). There are no contraindications listed in the manufacturer's Campath labeling.
Canadian labeling:
Lemtrada: Hypersensitivity to alemtuzumab or any component of the formulation; HIV infection; active or latent tuberculosis; severe active infections; active malignancies; concurrent antineoplastic or immunosuppressive therapy; history of progressive multifocal leukoencephalopathy (PML)
MabCampath: Known type 1 hypersensitivity or anaphylactic reactions to alemtuzumab or any component of the formulation; active infections; underlying immunodeficiency (eg, seropositive for HIV); active secondary malignancies; current or history of progressive multifocal leukoencephalopathy (PML)
Dosage and Administration
Dosing: Adult
Note: Alemtuzumab is associated with a moderate emetic potential in the oncology setting; antiemetics may be recommended to prevent nausea and vomiting (Hesketh 2017; Roila 2016).
B-cell chronic lymphocytic leukemia (B-CLL): Campath, MabCampath [Canadian product]: IV: Gradually escalate to a maintenance of 30 mg per dose 3 times weekly on alternate days for a total duration of therapy of up to 12 weeks (Hillmen 2007; Keating 2002)
Note: Dose escalation is required; usually accomplished in 3 to 7 days. Single doses >30 mg or cumulative doses >90 mg/week increase the incidence of pancytopenia. Pretreatment (with acetaminophen 500 to 1,000 mg and diphenhydramine 50 mg) is recommended 30 minutes prior to the first dose, with dose escalations, and as clinically indicated; IV glucocorticoids may be used for severe infusion-related reactions. Administer antiviral prophylaxis (for herpetic viral infections) and Pneumocystis jirovecii pneumonia (PCP) prophylaxis; continue for at least 2 months after completion of alemtuzumab and until CD4+ lymphocyte count is ≥200/mm3. Reinitiate with gradual dose escalation if treatment is withheld ≥7 days.
Dose escalation: Initial: 3 mg daily beginning on day 1; if tolerated (infusion reaction ≤ grade 2), increase to 10 mg daily; if tolerated (infusion reaction ≤ grade 2), may increase to maintenance of 30 mg per dose 3 times weekly (on alternate days) if required.
B-CLL (off-label route): Campath: SubQ: Initial: 3 mg on day 1; if tolerated 10 mg on day 3; if tolerated increase to 30 mg on day 5; maintenance: 30 mg per dose 3 times weekly on alternate days for a maximum of 18 weeks (Lundin 2002) or 3 mg on day 1; if tolerated 10 mg on day 2; if tolerated 30 mg on day 3, followed by 30 mg per dose 3 times weekly on alternate days for 4 to 12 weeks (Stilgenbauer 2009)
Multiple sclerosis, relapsing: Lemtrada: IV: 12 mg daily for 5 consecutive days (total 60 mg), followed 12 months later by 12 mg daily for 3 consecutive days (total 36 mg). Subsequent treatment courses of 12 mg daily for 3 consecutive days (total 36 mg) may be administered if necessary; courses should be administered no earlier than 12 months after the last dose of the prior treatment cycle.
Note: Premedicate with corticosteroids (methylprednisolone 1 g or equivalent) immediately prior to alemtuzumab for the first 3 days of each treatment course. Antihistamines and/or antipyretics may also be considered. Administer antiviral prophylaxis (for herpetic viral infections) beginning on the first day of treatment and continue for at least 2 months after completion of alemtuzumab or until CD4+ lymphocyte count is ≥200/mm3 (whichever occurs later).
Aplastic anemia, refractory (off-label use): Campath:
IV: 10 mg daily for 10 days (as monotherapy); patients received a 1 mg test dose initially (Scheinberg 2012) or
SubQ: 3 mg day 1, 10 mg day 2, then 30 mg/day days 3, 4, and 5 (total dose: 103 mg over 5 consecutive days; in combination with cyclosporine) (Risitano 2009)
Autoimmune cytopenias, CLL-induced, refractory (off-label use): Campath: IV, SubQ: Gradually escalate to a maintenance of 10 to 30 mg per dose 3 times weekly for 4 to 12 weeks (Karlsson 2007; Osterborg 2009)
Graft versus host disease (GVHD), acute, steroid refractory, treatment (off-label use): Campath: IV: 10 mg daily for 5 consecutive days, then 10 mg weekly on days 8, 15, and 22 if CR not achieved (Martinez 2009) or 10 mg weekly until symptom resolution (Schnitzler 2009)
Hemophagocytic lymphohistiocytosis, refractory (off-label use): Campath: IV, SubQ: Note: The optimal dose and duration of therapy is not known. Median dose: 1 mg/kg (range 0.1 to 8.9 mg/kg; maximum initial dose: 3 mg) divided over a median of 4 days (range 2 to 10 days); refer to article for further information (Marsh 2013)
Mycosis fungoides/Sézary syndrome, advanced (off-label use): Campath: IV: Initial: 3 mg, increase to 10 mg and then to 30 mg as soon as infusion-related reactions were tolerated; Maintenance: 30 mg 3 times weekly for up to 12 weeks, or until complete remission is achieved or disease progression is noted; for dosing interruptions >7 days due to toxicity, reinitiate at 3 or 10 mg (Lundin 2003).
Solid organ transplantation: Campath:
Heart transplant, induction (off-label use): IV: 30 mg once intra-operatively at the time of transplant followed by minimized maintenance immunosuppression (Teuteberg 2010). Additional data may be necessary to further define the role of alemtuzumab in this condition.
Lung transplant, induction (off-label use): IV, SubQ: 30 mg once either immediately before allograft reperfusion or immediately following transplant; followed by minimized maintenance immunosuppression (Jaksch 2014; Shyu 2011; Whited 2015). Additional data may be necessary to further define the role of alemtuzumab in this condition.
Renal transplant, induction (off-label use): IV: 30 mg as a single dose at the time of transplant (immediately following reperfusion) followed by a second 30 mg dose 24 hours later (the second dose was omitted in patients >60 years of age); followed by minimized maintenance immunosuppression (Haynes 2014).
Renal transplant, steroid resistant cellular rejection (off-label use): IV, SubQ: 15 to 30 mg/dose SubQ on 2 subsequent days (van den Hoogen 2013) or 30 mg/dose IV over 2 to 4 hours for 1 to 2 doses (Basu 2005). Additional data may be necessary to further define the role of alemtuzumab in this condition.
Stem cell transplant (allogeneic) conditioning regimen (off-label use): Campath: IV: 20 mg daily for 5 days (in combination with fludarabine and melphalan) beginning 8 days prior to transplant (Mead 2010) or beginning 7 days prior to transplant (Van Besien 2009)
T-cell large granular lymphocytic leukemia (off-label use): Campath: IV: 10 mg daily for 10 days; patients received a 1 mg test dose initially (Dumitriu 2016)
T-cell prolymphocytic leukemia (T-PLL; off-label use): Campath: IV: Initial test dose 3 mg or 10 mg, followed by dose escalation to 30 mg per dose 3 times weekly as tolerated until maximum response (Dearden 2001) or Initial dose: 3 mg day 1, if tolerated increase to 10 mg day 2, if tolerated increase to 30 mg on day 3 (days 1, 2, and 3 are consecutive days), followed by 30 mg per dose every Monday, Wednesday, Friday for a total of 4 to 12 weeks (Keating 2002)
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Aplastic anemia, refractory (off-label use): Campath:
Children ≥2 years of age and Adolescents (<50 kg): IV: 0.2 mg/kg/dose (maximum: 10 mg/dose) for 10 days (as monotherapy); patients received a 1 mg test dose initially (Scheinberg 2012)
Children ≥2 years of age and Adolescents (≥50 kg): IV: 10 mg daily for 10 days (as monotherapy); patients received a 1 mg test dose initially (Scheinberg 2012)
Hemophagocytic lymphohistiocytosis, refractory (off-label use): Infants, Children, and Adolescents: Campath: IV, SubQ: Note: The optimal dose and duration of therapy is not known. Median dose: 1 mg/kg (range 0.1 to 8.9 mg/kg; maximum initial dose: 3 mg) divided over a median of 4 days (range 2 to 10 days); refer to article for further information (Marsh 2013)
Dosing adjustment for toxicity: There are no pediatric-specific recommendations; the presented dosing adjustments are based on experience in adult patients. Refer to specific protocol for management in pediatric patients if available.
Nonhematologic toxicity:
Treatment of B-CLL: Campath, MabCampath [Canadian product]:
Note: If treatment is withheld ≥7 days, reinitiate at 3 mg with re-escalation to 10 mg and then 30 mg.
Grade 3 or 4 infusion reaction: Withhold infusion
Serious infection or other serious adverse reaction: Withhold alemtuzumab until resolution
Autoimmune anemia or autoimmune thrombocytopenia: Discontinue alemtuzumab
Hematologic toxicity (severe neutropenia or thrombocytopenia, not autoimmune): Treatment of B-CLL: Campath, MabCampath [Canadian product]:
Note: If treatment is withheld ≥7 days, reinitiate at 3 mg with re-escalation to 10 mg and then 30 mg.
ANC <250/mm3 and/or platelet count ≤25,000/mm3:
First occurrence: Withhold treatment; resume at 30 mg per dose when ANC ≥500/mm3 and platelet count ≥50,000/mm3
Second occurrence: Withhold treatment; resume at 10 mg per dose when ANC ≥500/mm3 and platelet count ≥50,000/mm3
Third occurrence: Discontinue alemtuzumab.
Patients with a baseline ANC ≤250/mm3 and/or a baseline platelet count ≤25,000/mm3 at initiation of therapy: If ANC and/or platelet counts decrease by ≥50% of the baseline value:
First occurrence: Withhold treatment; resume at 30 mg per dose upon return to baseline values
Second occurrence: Withhold treatment; resume at 10 mg per dose upon return to baseline values
Third occurrence: Discontinue alemtuzumab.
Dosing: Adjustment for Toxicity
Dosage adjustment for nonhematologic toxicity:
Treatment of B-CLL: Campath, MabCampath [Canadian product]:
Note: If treatment is withheld ≥7 days, reinitiate at 3 mg with re-escalation to 10 mg and then 30 mg.
Grade 3 or 4 infusion reaction: Withhold infusion
Serious infection or other serious adverse reaction: Withhold alemtuzumab until resolution
Autoimmune anemia or autoimmune thrombocytopenia: Discontinue alemtuzumab
Treatment of MS: Lemtrada: Serious infusion reaction: Consider immediate discontinuation
Dosage adjustment for hematologic toxicity (severe neutropenia or thrombocytopenia, not autoimmune): Treatment of B-CLL: Campath, MabCampath [Canadian product]:
Note: If treatment is withheld ≥7 days, reinitiate at 3 mg with re-escalation to 10 mg and then 30 mg.
ANC <250/mm3 and/or platelet count ≤25,000/mm3:
First occurrence: Withhold treatment; resume at 30 mg per dose when ANC ≥500/mm3 and platelet count ≥50,000/mm3
Second occurrence: Withhold treatment; resume at 10 mg per dose when ANC ≥500/mm3 and platelet count ≥50,000/mm3
Third occurrence: Discontinue alemtuzumab.
Patients with a baseline ANC ≤250/mm3 and/or a baseline platelet count ≤25,000/mm3 at initiation of therapy: If ANC and/or platelet counts decrease by ≥50% of the baseline value:
First occurrence: Withhold treatment; resume at 30 mg per dose upon return to baseline values
Second occurrence: Withhold treatment; resume at 10 mg per dose upon return to baseline values
Third occurrence: Discontinue alemtuzumab.
Dosing: Obesity
American Society for Blood and Marrow Transplantation (ASBMT) practice guideline committee position statement on chemotherapy dosing in obesity: Utilize a flat dose based on the regimen selected for hematopoietic stem cell transplant conditioning in adults (Bubalo 2014).
Reconstitution
Campath, MabCampath [Canadian product]: Dilute appropriate dose for infusion in 100 mL NS or D5W. Compatible in polyvinylchloride (PVC) bags. Gently invert the bag to mix the solution. Do not shake prior to use.
Lemtrada: Withdraw 12 mg (1.2 mL) from vial and add to 100 mL bag of NS or D5W. Gently invert the bag to mix the solution.
Administration
IV: Campath or MabCampath [Canadian product]: Administer by IV infusion over 2 hours. Premedicate with diphenhydramine 50 mg and acetaminophen 500 to 1,000 mg 30 minutes before each infusion. IV glucocorticoids have been effective in decreasing severe infusion-related events. Start anti-infective prophylaxis. Other drugs should not be added to or simultaneously infused through the same IV line. Do not give IV push or bolus. Compatible in polyvinylchloride (PVC) or polyethylene lined administration sets or low protein binding filters. May be given through peripheral IV.
Infusion times may have varied in studies for off-label uses; refer to specific reference citations.
Lemtrada: Administer by IV infusion over 4 hours (beginning within 8 hours after dilution); do not administer by IV push or IV bolus. May extend the infusion duration if clinically indicated. Do not infuse other medications through the same IV line. Premedicate with corticosteroids (methylprednisolone 1,000 mg or equivalent) for first 3 days of each treatment course. Administer in a setting with personnel and equipment appropriate to manage infusion reactions. Monitor vital signs prior to and periodically during the infusion. Infusion reactions should be managed symptomatically; consider discontinuing immediately for severe infusion reaction. Observe for at least 2 hours after each infusion, longer if clinically indicated.
SubQ: Campath: SubQ (off-label route): SubQ administration has been studied (Lundin 2002; Stilgenbauer 2009); an increased rate of injection site reactions has been observed, with only rare incidences of chills or infusion-like reactions typically observed with IV infusion. A longer dose escalation time (1 to 2 weeks) may be needed due to injection site reactions (Lundin 2002). Premedicate with diphenhydramine 50 mg and acetaminophen 500 to 1,000 mg 30 minutes before dose. The subQ route should NOT be used for the treatment of T-PLL (Deardon 2011).
Alemtuzumab is associated with a moderate emetic potential in adults in the oncology setting; antiemetics may be recommended to prevent nausea and vomiting (Hesketh 2017; Roila 2016).
Storage
Campath: Prior to dilution in NS or D5W, store intact (30 mg/1 mL) vials at 2°C to 8°C (36°F to 46°F); do not freeze (if accidentally frozen, thaw in refrigerator prior to administration). Do not shake; protect from light. Following dilution, store at room temperature or refrigerate; protect from light; use within 8 hours. Discard unused portion in the vial.
Lemtrada: Prior to dilution in NS or D5W, store intact vials at 2°C to 8°C (36°F to 46°F). Do not freeze. Do not shake; protect from light. Following dilution, store at room temperature or refrigerate; use within 8 hours.
MabCampath [Canadian product]: Prior to dilution in NS or D5W, store vials at 2°C to 8°C (36°F to 46°F). Do not freeze (discard vial if frozen). Do not shake. Protect from light. Following dilution, store at room temperature or refrigerate; use within 8 hours.
Drug Interactions
Baricitinib: Immunosuppressants may enhance the immunosuppressive effect of Baricitinib. Management: Use of baricitinib in combination with potent immunosuppressants such as azathioprine or cyclosporine is not recommended. Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted. Consider therapy modification
BCG (Intravesical): Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG (Intravesical): Myelosuppressive Agents may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Chloramphenicol (Ophthalmic): May enhance the adverse/toxic effect of Myelosuppressive Agents. Monitor therapy
Cladribine: May enhance the immunosuppressive effect of Immunosuppressants. Avoid combination
Cladribine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Avoid combination
CloZAPine: Myelosuppressive Agents may enhance the adverse/toxic effect of CloZAPine. Specifically, the risk for neutropenia may be increased. Monitor therapy
Coccidioides immitis Skin Test: Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. Monitor therapy
Deferiprone: Myelosuppressive Agents may enhance the neutropenic effect of Deferiprone. Management: Avoid the concomitant use of deferiprone and myelosuppressive agents whenever possible. If this combination cannot be avoided, monitor the absolute neutrophil count more closely. Consider therapy modification
Denosumab: May enhance the adverse/toxic effect of Immunosuppressants. Specifically, the risk for serious infections may be increased. Monitor therapy
Dipyrone: May enhance the adverse/toxic effect of Myelosuppressive Agents. Specifically, the risk for agranulocytosis and pancytopenia may be increased Avoid combination
Echinacea: May diminish the therapeutic effect of Immunosuppressants. Consider therapy modification
Fingolimod: Immunosuppressants may enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). Consider therapy modification
Leflunomide: Immunosuppressants may enhance the adverse/toxic effect of Leflunomide. Specifically, the risk for hematologic toxicity such as pancytopenia, agranulocytosis, and/or thrombocytopenia may be increased. Management: Consider not using a leflunomide loading dose in patients receiving other immunosuppressants. Patients receiving both leflunomide and another immunosuppressant should be monitored for bone marrow suppression at least monthly. Consider therapy modification
Mesalamine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Natalizumab: Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. Avoid combination
Nivolumab: Immunosuppressants may diminish the therapeutic effect of Nivolumab. Consider therapy modification
Ocrelizumab: May enhance the immunosuppressive effect of Immunosuppressants. Monitor therapy
Pidotimod: Immunosuppressants may diminish the therapeutic effect of Pidotimod. Monitor therapy
Pimecrolimus: May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Promazine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Roflumilast: May enhance the immunosuppressive effect of Immunosuppressants. Consider therapy modification
Siponimod: Immunosuppressants may enhance the immunosuppressive effect of Siponimod. Monitor therapy
Sipuleucel-T: Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. Consider therapy modification
Smallpox and Monkeypox Vaccine (Live): Immunosuppressants may diminish the therapeutic effect of Smallpox and Monkeypox Vaccine (Live). Monitor therapy
Tacrolimus (Topical): May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Tertomotide: Immunosuppressants may diminish the therapeutic effect of Tertomotide. Monitor therapy
Tofacitinib: Immunosuppressants may enhance the immunosuppressive effect of Tofacitinib. Management: Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted, and this warning seems particularly focused on more potent immunosuppressants. Consider therapy modification
Trastuzumab: May enhance the neutropenic effect of Immunosuppressants. Monitor therapy
Upadacitinib: Immunosuppressants may enhance the immunosuppressive effect of Upadacitinib. Avoid combination
Vaccines (Inactivated): Immunosuppressants may diminish the therapeutic effect of Vaccines (Inactivated). Management: Vaccine efficacy may be reduced. Complete all age-appropriate vaccinations at least 2 weeks prior to starting an immunosuppressant. If vaccinated during immunosuppressant therapy, revaccinate at least 3 months after immunosuppressant discontinuation. Consider therapy modification
Vaccines (Live): Immunosuppressants may enhance the adverse/toxic effect of Vaccines (Live). Immunosuppressants may diminish the therapeutic effect of Vaccines (Live). Management: Avoid use of live organism vaccines with immunosuppressants; live-attenuated vaccines should not be given for at least 3 months after immunosuppressants. Exceptions: Smallpox and Monkeypox Vaccine (Live). Avoid combination
Test Interactions
May interfere with diagnostic serum tests that utilize antibodies.
Adverse Reactions
Multiple sclerosis:
>10%:
Central nervous system: Headache (52%), fatigue (18%), insomnia (16%), paresthesia (10%)
Dermatologic: Skin rash (53%), urticaria (16%), pruritus (14%)
Endocrine & metabolic: Thyroid disease (13% to 37%)
Gastrointestinal: Nausea (21%), diarrhea (12%)
Genitourinary: Urinary tract infection (19%)
Hematologic & oncologic: Lymphocytopenia (100%)
Immunologic: Antibody development (neutralizing: 5% to 94%; anti-alemtuzumab: 2% to 83%; no effect on drug efficacy)
Infection: Infection (71%), herpes virus infection (16%), fungal infection (12% to 13%; including oral candidiasis, vulvovaginal candidiasis)
Local: Infusion-related reaction (92%)
Neuromuscular & skeletal: Arthralgia (12%), back pain (12%), limb pain (12%)
Respiratory: Nasopharyngitis (25%), upper respiratory tract infection (16%), oropharyngeal pain (11%), sinusitis (11%)
Miscellaneous: Fever (29%)
1% to 10%:
Cardiovascular: Flushing (10%), tachycardia (8%), chest discomfort (7%), peripheral edema (5%), atrial fibrillation (≤3%), bradycardia (≤3%), chest pain (≤3%), hypertension (≤3%), hypotension (≤3%)
Central nervous system: Dizziness (10%), chills (9%), anxiety (7%), neurological signs and symptoms (≤3%; transient)
Dermatologic: Dermatitis (8%), erythema of skin (5%)
Gastrointestinal: Abdominal pain (10%), vomiting (10%), oral herpes simplex infection (9%), dysgeusia (8%), dyspepsia (8%), appendicitis (≤3%), gastroenteritis (≤3%), tooth infection (≤3%)
Genitourinary: Microscopic hematuria (8%), uterine hemorrhage (5%), genital herpes simplex (1%)
Hematologic & oncologic: Decreased CD-4 cell count (6%), decreased CD-8 cell counts (6%), decreased T cell lymphocytes (5%), immune thrombocytopenia (2%), hematoma (1%), petechia (1%)
Hypersensitivity: Angioedema (≤3%)
Infection: Influenza (8%), herpes zoster infection (4%), herpes simplex infection (2%), human papilloma virus infection (2%)
Neuromuscular & skeletal: Myasthenia (7%), muscle spasm (6%), myalgia (6%), neck pain (5%), asthenia (5%)
Ophthalmic: Graves’ ophthalmopathy (1%)
Respiratory: Cough (9%), dyspnea (8%), bronchitis (7%), epistaxis (5%), bronchospasm (≤3%), pneumonia (≤3%)
Frequency not defined:
Central nervous system: Pain
Respiratory: Hypersensitivity pneumonitis, pneumonitis (with fibrosis), pulmonary infiltrates
B-cell chronic lymphocytic leukemia:
>10%:
Cardiovascular: Hypotension (16%), cardiac arrhythmia (14%), hypertension (14%)
Central nervous system: Chills (53%), headache (14%)
Dermatologic: Urticaria (16%), skin rash (13%)
Hematologic & oncologic: Lymphocytopenia (97%; grades 3/4: 97%), neutropenia (77%; grades 3/4: 42% to 64%), anemia (76%; grades 3/4: 12% to 38%), thrombocytopenia (71%; grades 3/4: 13% to 52%)
Infection: Infection (50% to 74%), CMV viremia (55%), cytomegalovirus disease (6% to 16%)
Respiratory: Dyspnea (14%)
Miscellaneous: Fever (69%)
1% to 10%:
Cardiovascular: Tachycardia (10%)
Central nervous system: Insomnia (10%), anxiety (8%), dysesthesia (>5%), fatigue (>5%)
Dermatologic: Erythema of skin (4%)
Gastrointestinal: Diarrhea (10%), anorexia (>5%), nausea (>5%), stomatitis (>5%), vomiting (>5%)
Hematologic & oncologic: Febrile neutropenia (grades ≥3: 5% to 10%), autoimmune thrombocytopenia (2%)
Immunologic: Antibody development (2% to 8%; neutralizing: 2%)
Infection: Sepsis (grades ≥3: 3% to 10%)
Neuromuscular & skeletal: Musculoskeletal pain (>5%), tremor (3%)
Respiratory: Bronchospasm (>5%)
<1%, postmarketing, and/or case reports (any indication): Anaphylactic shock, anaphylaxis, anemia, anti-GBM disease, aplastic anemia, autoimmune hemolytic anemia, autoimmune hepatitis, bone marrow aplasia, bone marrow depression, cardiac failure, cardiomyopathy, cerebrovascular accident, cholecystitis, chronic inflammatory demyelinating polyneuropathy, connective tissue disease (undifferentiated), Epstein-Barr-associated lymphoproliferative disorder, Epstein-Barr infection, goiter, Goodpasture’s syndrome, graft versus host disease (transfusion associated), Graves’ disease, Guillain-Barre syndrome, hemolytic anemia, hemophilia A (acquired [anti-Factor VIII antibodies]), hemorrhagic stroke, hyperthyroidism, hypothyroidism, immunological signs and symptoms (hemophagocytic lymphohistiocytosis), ischemic stroke, listeriosis (including gastroenteritis, encephalitis, sepsis), lymphoproliferative disorder, malignant lymphoma, malignant melanoma, malignant neoplasm of thyroid, membranous glomerulonephritis, meningitis due to listeria monocytogenes, meningitis (herpes), neutropenia, opportunistic infection, optic neuropathy, pancytopenia, pneumonitis, progressive multifocal leukoencephalopathy, pulmonary alveolar hemorrhage, pure red cell aplasia, reactivation of disease, reduced ejection fraction, retinal pigment changes (epitheliopathy), rheumatoid arthritis, serum sickness, suicidal ideation, suicidal tendencies, syncope, thyroiditis, tuberculosis, tumor lysis syndrome, type 1 diabetes mellitus, vasculitis, vitiligo
Warnings/Precautions
Concerns related to adverse effects:
- Autoimmune effects: [US Boxed Warning (Lemtrada)]: Alemtuzumab causes serious, sometimes fatal, autoimmune conditions, such as immune thrombocytopenia and antiglomerular basement membrane (anti-GBM) disease, in patients receiving alemtuzumab for the treatment of multiple sclerosis (MS). Monitor CBC with differential, serum creatinine levels, and urinalysis with urine cell counts at periodic intervals for 48 months after the last dose of alemtuzumab. Monitor for symptoms of immune thrombocytopenia (easy bruising, petechiae, spontaneous mucocutaneous bleeding, heavy menstrual bleeding) in patients receiving alemtuzumab for MS. Glomerular nephropathies, including anti-GBM disease, have been reported up to 40 months after the last dose. Monitor for nephropathy symptoms (dyspnea, edema, elevated serum creatinine, change in urine color, decreased urine output, fatigue, hematuria, hemoptysis, proteinuria). Glomerular nephropathies require urgent evaluation; may lead to end-stage renal disease requiring dialysis or renal transplantation if not treated. Urine dipstick results of ≥1+ protein warrant assessment of urine protein to creatinine ratio. Perform further evaluation for nephropathies if urine protein to creatinine ratio >200 mg/g, increase in serum creatinine >30%, or unexplained hematuria. Alveolar hemorrhage manifesting as hemoptysis has been reported with anti-GBM disease. Prompt intervention is necessary for increased serum creatinine with hematuria, signs of pulmonary involvement of anti-GBM disease (eg, hemoptysis, exertional dyspnea), or autoimmune cytopenias. Immune thrombocytopenia (formerly known as idiopathic thrombocytopenic purpura), thyroid disorders, autoimmune hemolytic anemia, autoimmune hepatitis, autoimmune pancytopenia, undifferentiated connective tissue disorders, acquired hemophilia A, rheumatoid arthritis, type 1 diabetes, vasculitis, vitiligo, and retinal pigment epitheliopathy have been reported in patients receiving alemtuzumab for MS. Guillain-Barre syndrome and chronic inflammatory demyelinating polyradiculoneuropathy have been reported in patients receiving alemtuzumab for other uses. Alemtuzumab may increase the risk for other autoimmune conditions.
- Bone marrow suppression: [US Boxed Warning (Campath)]: Serious and fatal cytopenias (including pancytopenia, bone marrow hypoplasia, autoimmune hemolytic anemia, and autoimmune idiopathic thrombocytopenia) have occurred. Single doses >30 mg or cumulative weekly doses >90 mg are associated with an increased incidence of pancytopenia. Severe prolonged myelosuppression, hemolytic anemia, pure red cell aplasia, bone marrow aplasia, and bone marrow hypoplasia have also been reported with use at the normal dose for the treatment of B-cell chronic lymphocytic leukemia (B-CLL). Discontinue for serious hematologic or other serious toxicity (except lymphopenia) until the event resolves. Permanently discontinue if autoimmune anemia or autoimmune thrombocytopenia occurs. Patients receiving blood products should only receive irradiated blood products due to the potential for transfusion-associated graft-versus-host disease during lymphopenia.
- Cholecystitis: In a clinical trial of MS patients, an increased risk of acute acalculous cholecystitis was observed in patients receiving alemtuzumab versus interferon beta-1a; additional postmarketing cases have also been reported. Symptom onset ranged from <24 hours to 2 months after alemtuzumab infusion. Some patients recovered without surgical intervention (and received antibiotics); some patients underwent cholecystectomy. Monitor closely (acute acalculous cholecystitis is associated with high morbidity and mortality); symptoms may include abdominal pain/tenderness, fever, nausea, vomiting, leukocytosis, and abnormal liver enzymes. Evaluate and treat promptly if acute acalculous cholecystitis is suspected or diagnosed.
- GI toxicity: Alemtuzumab is associated with a moderate emetic potential in adults in the oncology setting; antiemetics may be recommended to prevent nausea and vomiting (Hesketh 2017; Roila 2016).
- Hepatitis: Autoimmune hepatitis causing clinically significant liver injury, including acute liver failure requiring transplant, has been reported; monitor serum transaminases and total bilirubin prior to initiation of therapy, then periodically until 48 months after the last infusion or at any time during therapy. Monitor for clinical signs/symptoms of hepatic dysfunction (unexplained nausea, vomiting, abdominal pain, anorexia, fatigue, jaundice, and/or dark urine); if reported, promptly obtain serum transaminases and total bilirubin; may require treatment interruption or discontinuation.
- Infections: [US Boxed Warning (Campath)]: Serious and potentially fatal infections (bacterial, viral, fungal, and protozoan) have been reported. Administer prophylactic medications against Pneumocystis jirovecii pneumonia (PCP) and herpes viral infections during treatment and for at least 2 months following last dose or until CD4+ counts are ≥200 cells/mm3 (whichever is later). Severe and prolonged lymphopenia may occur; CD4+ counts usually return to ≥200 cells/mm3 within 2 to 6 months; however, CD4+ and CD8+ lymphocyte counts may not return to baseline levels for more than 1 year. Withhold treatment during serious infections; may be reinitiated upon resolution of infection. Monitor for cytomegalovirus (CMV) infection (during and for at least 2 months after completion of therapy); initiate appropriate antiviral treatment and withhold alemtuzumab for CMV infection or confirmed CMV viremia (withhold alemtuzumab during CMV antiviral treatment). For patients being treated for MS, initiate antiviral prophylaxis (for herpetic viral infections) beginning on the first day of treatment and continue for at least 2 months or until CD4+ lymphocyte count is ≥200/mm3. In clinical trials for MS, infections seen more commonly in alemtuzumab-treated patients included nasopharyngitis, urinary tract infection, upper respiratory tract infection, sinusitis, herpetic infections, influenza, and bronchitis; serious cases of appendicitis, gastroenteritis, pneumonia, herpes zoster, and tooth infection also occurred. Serious (sometimes fatal) opportunistic infections have been reported, including aspergillosis, coccidioidomycosis, histoplasmosis, PCP, nocardiosis, and CMV. Listeria monocytogenes infections (encephalitis, gastroenteritis, meningitis, sepsis), including fatal cases of Listeria meningoencephalitis have been reported; Listeria infections have developed as early as 3 days post treatment and up to 8 months after the last dose for MS. The duration of increased risk for Listeria infections after treatment is unknown. Patients should initiate Listeria precautions prior to starting treatment, which include avoiding or adequately heating foods that may potentially carry this bacteria (eg, deli meat, dairy products made with unpasteurized milk, soft cheeses, or undercooked meat, seafood, or poultry). The incubation period for Listeria monocytogenes ranges from 3 to 70 days; signs/symptoms of invasive listeriosis generally start within 1 month of exposure. Symptoms of Listeria infection include fever, chills, diarrhea, nausea, vomiting, headache, pains in joints and muscles, neck stiffness, difficulty walking, mental status changes, coma, and other neurologic changes. Treatment (eg, with anti-infectives) may not adequately prevent Listeria infection-related morbidity/mortality. Consider delaying treatment in patients with any active infection until infection is controlled. Screen for tuberculosis (per local guidelines). Patients should be screened for human papilloma virus as clinically necessary.
- Infusion reactions: [US Boxed Warning]: Serious and potentially fatal infusion-related reactions may occur; monitor for infusion reaction; carefully monitor during infusion; withhold treatment for serious or grade 3 or 4 infusion reactions. For B-CLL, gradual escalation to the recommended maintenance dose is required at initiation and with treatment interruptions (for ≥7 days) to minimize infusion-related reactions. For MS, must be administered in a setting with appropriate equipment and personnel to manage anaphylaxis or serious infusion reaction; monitor for 2 hours after each infusion; inform patients that serious infusion reactions may also occur within 48 hours after the last infusion. In patients treated for B-CLL, infusion reaction symptoms may include acute respiratory distress syndrome, anaphylactic/anaphylactoid shock, angioedema, bronchospasm, cardiac arrest, cardiac arrhythmias, chills, dyspnea, fever, hypotension, myocardial infarction, pulmonary infiltrates, rash, rigors, syncope, or urticaria. The incidence of infusion reaction is highest during the first week of B-CLL treatment. Premedicate with acetaminophen and an oral antihistamine. Medications for the treatment of reactions should be available for immediate use. Use caution and carefully monitor blood pressure in patients with ischemic heart disease and patients on antihypertensive therapy. For B-CLL, reinitiate with gradual dose escalation if treatment is withheld ≥7 days. Similar infusion reactions, as well as pulmonary alveolar hemorrhage and life-threatening stroke (including ischemic and hemorrhagic stroke), have been observed with use in the treatment of multiple sclerosis. Cases of severe (including fatal) neutropenia have also been reported within 2 months of infusion; may resolve with granulocyte colony-stimulating factor treatment. Mild to moderate decreases in platelet counts at infusion initiation have been reported; may resolve without treatment. Premedication with corticosteroids for initial 3 days of each treatment course is recommended. Antihistamines and/or antipyretics may also be considered. Consider additional monitoring in patients with existing cardiovascular or respiratory compromise. Observe for infusion-related reactions; advise patients to monitor for signs/symptoms of infusion reaction, particularly during the 48 hours following infusion.
- Malignancy: [US Boxed Warning (Lemtrada)]: Alemtuzumab may cause an increased risk of malignancies, including thyroid cancer, melanoma, and lymphoproliferative disorders. Perform baseline and yearly skin exams. Other malignant neoplasm (breast cancer or basal cell carcinoma) has been observed (rarely) in patients receiving treatment for MS. Use caution if initiating treatment in patients with preexisting or ongoing malignancies.
- Pneumonitis: Pneumonitis (hypersensitivity or fibrosis) has been reported. Monitor for symptoms (dyspnea, cough, wheezing, hemoptysis, chest pain/tightness).
- Progressive multifocal leukoencephalopathy: Progressive multifocal leukoencephalopathy (PML) was diagnosed in a patient 2 months after the second alemtuzumab course for the treatment of MS. PML is an opportunistic viral infection of the brain caused by the John Cunningham (JC) virus and usually leads to death or severe disability. PML typically only occurs in patients who are immunocompromised; however, the patient who developed PML while taking alemtuzumab had no identifiable systemic medical condition resulting in immunosuppression, had not received other MS medications for >1 year, was not taking any concomitant immunomodulatory or immunosuppressant medications, and had not previously been treated with natalizumab. At the first sign or symptom suggestive of PML, perform a diagnostic evaluation and withhold therapy; symptoms progress over days to weeks and may include progressive weakness on one side of the body or clumsiness of limbs, vision disturbances, and mental status changes. Cases of PML have been diagnosed based on MRI findings and the detection of JC virus DNA in the cerebrospinal fluid without specific PML signs/symptoms. Monitoring with brain MRI for signs that may be consistent with PML may be beneficial and allow for an early diagnosis of PML.
- Stroke and cervicocephalic arterial dissection (Lemtrada): [US Boxed Warning (Lemtrada)]: Serious and life-threatening stroke (including ischemic and hemorrhagic stroke) has been reported within 3 days of Lemtrada administration. Instruct patients to seek immediate medical attention if symptoms of a stroke occur. Most cases of stroke occurred within 1 day of administration; cases of cervicocephalic (eg, vertebral, carotid) arterial dissection involving multiple arteries occurred within 3 days. Educate patients to seek immediate medical care if symptoms of stroke and cervicocephalic arterial dissection occur.
- Thyroid disorders: Autoimmune thyroid disorders occurred in over one-third of patients receiving alemtuzumab for MS. In a trial evaluating alemtuzumab versus interferon beta-1a in patients with MS, thyroid dysfunction occurred more frequently in patients taking alemtuzumab (34% versus 6.5%) (Daniels 2014). The incidence of the first episode of thyroid dysfunction increased annually the first 3 years (year 1: 4.6%; year 2: 13.3%; year 3: 16.1%) then gradually decreased thereafter. Among patients with alemtuzumab-related thyroid dysfunction, Graves hyperthyroidism occurred most commonly (23%), followed by hypothyroidism and subacute thyroiditis (7% and 4%, respectively). Thyroid dysfunction (thyroiditis, Graves disease, goiter) has also been reported with alemtuzumab use for the treatment of other conditions. For B-CLL treatment, thyroid-stimulating hormone (TSH) monitoring is recommended; monitor TSH at baseline and every 2 to 3 months during alemtuzumab treatment (Hamnvik 2011). For MS, monitor TSH at baseline and every 3 months until 48 months after last infusion or longer or at any time during therapy if clinically indicated.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Hepatitis B virus or hepatitis C virus infected patients: Alemtuzumab has not been studied in MS patients infected with hepatitis B virus (HBV) or hepatitis C virus (HCV); consider screening patients at increased risk of infection prior to initiating treatment. Use with caution in HBV or HCV carriers; patients may be at risk for viral reactivation.
Dosage form specific issues:
- Polysorbate 80: Some dosage forms may contain polysorbate 80 (also known as Tweens). Hypersensitivity reactions, usually a delayed reaction, have been reported following exposure to pharmaceutical products containing polysorbate 80 in certain individuals (Isaksson 2002; Lucente 2000; Shelley 1995). Thrombocytopenia, ascites, pulmonary deterioration, and renal and hepatic failure have been reported in premature neonates after receiving parenteral products containing polysorbate 80 (Alade 1986; CDC 1984). See manufacturer's labeling.
Other warnings/precautions:
- Appropriate use: Alemtuzumab is not recommended for use in MS patients with inactive disease or who are stable on other treatment. Patients should commit to at least 48 months of follow-up after the last infusion.
- Duplicate therapy: If considering Lemtrada treatment for use in a patient who has previously received Campath/MabCampath, consider the additive and long-lasting immune system effects.
- Immunizations: Patients should not be immunized with live, viral vaccines during or recently after treatment. The ability to respond to any vaccine following therapy is unknown. Testing for antibodies to varicella zoster virus (VZV) is recommended prior to initiation of Lemtrada if history of chickenpox or VZV vaccination status is unknown. When using for the treatment of MS, complete necessary immunizations at least 6 weeks prior to initiating alemtuzumab. Determine if patient has a history varicella or vaccination for VZV; if not, test for VZV antibodies and consider vaccinations for antibody-negative patients; postpone alemtuzumab treatment for 6 weeks following VZV vaccination.
- REMS Program: [US Boxed Warning (Lemtrada)]: Due to the risk of autoimmunity, infusion reactions, and malignancies, alemtuzumab is available only through restricted distribution under a Risk Evaluation Mitigation Strategy (REMS) Program when used for the treatment of MS. Contact 1-855-676-6326 to enroll in the Lemtrada REMS program. Prescribers and pharmacies must be certified with the REMS program, and patients and healthcare facilities must be enrolled and comply with ongoing monitoring.
Monitoring Parameters
Campath: CBC with differential and platelets (weekly, more frequent if worsening); signs and symptoms of infection; CD4+ lymphocyte counts (after treatment until recovery); cytomegalovirus antigen (routinely during and for 2 months after treatment); consider thyroid-stimulating hormone (TSH) at baseline and then every 2 to 3 months during alemtuzumab treatment (Hamnvik 2011). Monitor closely for infusion reactions (including hypotension, rigors, fever, shortness of breath, bronchospasm, chills, and/or rash); vital signs (prior to and during infusion); carefully monitor BP, especially in patients with ischemic heart disease or on antihypertensive medications.
Lemtrada: CBC with differential prior to initiation then monthly until 48 months after last infusion; serum creatinine prior to initiation then monthly until 48 months after last infusion or at any time during therapy if clinically indicated; serum transaminases and total bilirubin prior to initiation then periodically until 48 months after the last infusion or at any time during therapy if clinically indicated; urinalysis with urine cell counts prior to initiation then monthly until 48 months after last infusion (urine dipstick results of ≥1+ protein warrant assessment of urine protein to creatinine ratio); urine protein to creatinine ratio at baseline and then as clinically indicated (evaluate further for nephropathies if urine protein to creatinine ratio >200 mg/g, increase in serum creatinine >30%, or unexplained hematuria); TSH at baseline and every 3 months until 48 months after last infusion or longer or at any time during therapy if clinically indicated. Observe for at least 2 hours after each infusion, longer if clinically indicated. Monitor for signs/symptoms of infection; annual human papillomavirus screening; tuberculosis screening; signs/symptoms of progressive multifocal leukoencephalopathy; baseline and annual skin exams (for melanoma).
Pregnancy
Pregnancy Considerations
Alemtuzumab is a humanized monoclonal antibody (IgG1). Potential placental transfer of human IgG is dependent upon the IgG subclass and gestational age, generally increasing as pregnancy progresses. The lowest exposure would be expected during the period of organogenesis (Palmeira 2012; Pentsuk 2009). Based on animal studies, alemtuzumab may cause fetal B- and T-lymphocyte depletion.
Information related to the use of alemtuzumab in pregnant females with multiple sclerosis is limited (Alroughani 2016; Tuohy 2015). Alemtuzumab induces persistent thyroid disorders which may cause adverse maternal and fetal events. In a patient who developed Graves disease during alemtuzumab therapy, neonatal Graves disease with thyroid storm developed in her infant exposed in utero 1 year following maternal treatment.
In general, disease-modifying therapies for multiple sclerosis are stopped prior to a planned pregnancy and not initiated during pregnancy, except in females at high risk of multiple sclerosis activity (AAN [Rae-Grant 2018]). Consider use of agents other than alemtuzumab for females at high risk of disease reactivation who are planning a pregnancy. Delaying pregnancy is recommended for females with persistent high disease activity; however, use of alemtuzumab may be an alternative option in these patients if the last infusion is at least 4 months prior to conception (ECTRIMS/EAN [Montalban 2018]).
Females and males of reproductive potential should use effective contraception during therapy and for at least 6 months after the last dose of Campath. Females of reproductive potential should use effective contraception during therapy and for 4 months after the last dose of Lemtrada.
Data collection to monitor pregnancy and infant outcomes following exposure to alemtuzumab is ongoing. Health care providers are encouraged to enroll females exposed to alemtuzumab during pregnancy in the pregnancy exposure registry (1-866-758-2990).
Patient Education
What is this drug used for?
- It is used to treat a type of leukemia.
- It is used to treat MS (multiple sclerosis).
- It may be given for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Anxiety
- Back pain
- Painful extremities
- Flushing
- Nausea
- Vomiting
- Diarrhea
- Muscle pain
- Joint pain
- Abdominal pain
- Stuffy nose
- Sore throat
- Lack of appetite
- Muscle spasms
- Muscle weakness
- Change in taste
- Trouble sleeping
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Gallbladder problems like pain in the upper right abdominal area, right shoulder area, or between the shoulder blades; yellow skin; or fever with chills; bloating; or severe nausea or vomiting
- Infusion reactions like chest pain, passing out, slow heartbeat, fast heartbeat, abnormal heartbeat, fever, hives, itching, rash, trouble breathing, shortness of breath, severe headache, dizziness, swelling of face or mouth, chest tightness, hoarseness, or wheezing
- Infection
- Progressive multifocal leukoencephalopathy like confusion, depression, trouble with memory, behavioral changes, change in strength on one side is greater than the other, trouble speaking, change in balance, or vision changes
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding
- Severe pulmonary disorder like lung or breathing problems like trouble breathing, shortness of breath, or a cough that is new or worse
- Kidney problems like not able to pass urine, blood in the urine, change in amount of urine passed, or weight gain
- Severe cerebrovascular disease like change in strength on one side is greater than the other, trouble speaking or thinking, change in balance, or vision changes
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
- Tumor lysis syndrome like fast heartbeat or abnormal heartbeat; any passing out; not able to pass urine; muscle weakness or cramps; nausea, vomiting, diarrhea or lack of appetite; or feeling sluggish
- Thyroid problems like change in weight without trying, anxiety, feeling restless, feeling very weak, hair thinning, depression, neck swelling, trouble focusing, inability handling heat or cold, menstrual changes, tremors, or sweating
- Thyroid cancer like new lump or swelling in the neck, pain in the front of the neck, persistent cough, persistent change in voice like hoarseness, or trouble swallowing or breathing
- Shortness of breath
- Severe loss of strength and energy
- Swollen glands
- Dizziness
- Passing out
- Thrush
- Severe headache
- Neck pain
- Slow heartbeat
- Chest pain
- Fast heartbeat
- Burning or numbness feeling
- Vision changes
- Abnormal heartbeat
- Abnormal sweating
- Mole changes
- Depression
- Night sweats
- Thoughts of suicide
- Swelling of arms or legs
- Neck rigidity
- Abnormal gait
- Confusion
- Skin growths
- Vaginal pain, itching, and discharge
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.