Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Solution Reconstituted, Intravenous, as sodium [strength expressed as base, preservative free]:
Aloprim: 500 mg (1 ea)
Generic: 500 mg (1 ea)
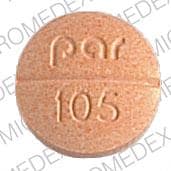
Tablet, Oral:
Zyloprim: 100 mg, 300 mg [DSC] [scored]
Zyloprim: 300 mg [scored; contains corn starch, fd&c yellow #6 aluminum lake]
Generic: 100 mg, 300 mg
Pharmacology
Mechanism of Action
Allopurinol inhibits xanthine oxidase, the enzyme responsible for the conversion of hypoxanthine to xanthine to uric acid. Allopurinol is metabolized to oxypurinol which is also an inhibitor of xanthine oxidase; allopurinol acts on purine catabolism, reducing the production of uric acid without disrupting the biosynthesis of vital purines.
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: 90% from GI tract
Distribution
Vss: IV: 0.84 to 0.87 L/kg
Metabolism
Rapidly oxidized to active metabolites, primarily oxypurinol
Excretion
Urine (76% as oxypurinol, 12% as unchanged drug); feces (~20%)
Onset of Action
Gout: Decrease in serum and urine uric acid: 2 to 3 days; peak effect: 1 week or longer; normal serum urate levels achieved typically within 1 to 3 weeks
Cancer therapy-induced hyperuricemia: Median time to plasma uric acid control: 27 hours (Cortes 2010)
Time to Peak
Plasma: Oral: Allopurinol: 1.5 hours; Oxypurinol: 4.5 hours
Half-Life Elimination
Parent drug: ~1 to 2 hours; Oxypurinol: ~15 hours
Use: Labeled Indications
Oral:
Gout, treatment: Management of primary or secondary gout (acute attack, tophi, joint destruction, uric acid lithiasis, and/or nephropathy)
Guideline recommendations: EULAR guidelines: Urate-lowering therapy (ULT) (eg, allopurinol) is indicated in all patients with recurrent flares, tophi, urate arthropathy, and/or renal stones. ULT initiation is recommended close in time to first diagnosis in patients presenting at a young age (<40 years of age) or with very high serum uric acid levels (>8 mg/dL) and/or comorbidities (eg, renal impairment, hypertension, ischemic heart disease, heart failure) (EULAR [Richette 2017]).
Nephrolithiasis, prevention of recurrent calcium stones: Management in patients with hyperuricosuria (uric acid excretion >800 mg/day in men and >750 mg/day in women)
Tumor lysis syndrome, prevention: Management of hyperuricemia associated with cancer treatment for leukemia, lymphoma, and other malignancies
Limitations of use: Allopurinol is not recommended for the treatment of asymptomatic hyperuricemia. Allopurinol reduces serum and urinary uric acid concentrations; its use should be individualized for each patient and requires an understanding of its mode of action and pharmacokinetics.
IV:
Tumor lysis syndrome, prevention: Management of hyperuricemia associated with cancer treatment for leukemia, lymphoma, or solid tumor malignancies in patients who cannot tolerate oral therapy.
Use: Off Label
Nephrolithiasis, prevention of recurrent uric acid stonesc
Clinical experience suggests the utility of allopurinol in the management of patients with recurrent nephrolithiasis due to uric acid stones Curhan 2018b, Heilberg 2016, Kenny 2010, Lipkin 2011.
Contraindications
Severe hypersensitivity reaction to allopurinol or any component of the formulation
Canadian labeling: Additional contraindications (not in the US labeling): Breastfeeding mothers and children (except those with cancer therapy-induced hyperuricemia or Lesch-Nyhan syndrome)
Note: To avoid the risk of severe cutaneous adverse reactions (SCAR), HLA-B*5801-positive patients should avoid allopurinol (Becker 2019; Saito 2016). The American College of Rheumatology recommends HLA-B*5801 screening in patients at elevated risk for SCAR, including patients of Korean descent who have CKD ≥ stage 3, as well as patients of Han Chinese or Thai descent regardless of kidney function (ACR [Khanna 2012a]). Some experts suggest screening in all patients of Korean ethnicity regardless of renal function (Becker 2019).
Dosage and Administration
Dosing: Adult
Note: Before prescribing allopurinol, consider testing for the HLA-B*5801 allele in patients at elevated risk for developing severe cutaneous adverse reactions (SCAR) (including Korean patients with CKD ≥ stage 3 and all patients of Han Chinese or Thai descent). A negative HLA-B*5801 genetic test, however, does not entirely rule out the possibility of allopurinol-associated SCAR, so patients should still be appropriately monitored for SCAR, as well as other forms of hypersensitivity (ACR [Khanna 2012a]; Quach 2018; Saito 2016). Some experts suggest screening in all patients of Korean ethnicity regardless of renal function. Use should be avoided in any patient testing positive for the allele (Becker 2019).
Gout, treatment (chronic urate-lowering therapy): Oral: Note: Starting urate-lowering therapy (ULT) can precipitate acute gout; while typically avoided, ULT may be initiated during a flare in selected patients in conjunction with an anti-inflammatory agent. Pharmacologic prophylaxis with colchicine or an NSAID is generally recommended for the first 3 to 6 months once serum urate goal is achieved with ULT (ACR [Khanna 2012b]; Becker 2019).
Initial: 100 mg once daily (ACR [Khanna 2012a]; EULAR [Richette 2017])
Dosage adjustments: Titrate in 100 mg increments every 2 to 4 weeks to achieve the desired serum uric acid level (EULAR [Richette 2017]; Jennings 2014).
Maintenance: Doses ≥300 mg/day are usually needed to reach the desired uric acid target; doses up to 800 mg/day may be required (EULAR [Richette 2017]; Jennings 2014).
Maximum: 800 mg/day
Frequency of administration: Once daily in a single dose or in 2 or 3 divided doses. Note: The manufacturer's labeling recommends doses >300 mg be given in divided doses; however, most experts prescribe a single daily dose, regardless of total dose administered, except during a brief period (eg, when initiating or titrating therapy) when divided doses may help improve GI tolerability (Becker 2019; Currie 1978).
Nephrolithiasis, prevention of recurrent calcium or uric acid stones:
Due to calcium oxalate stones: Patients with hyperuricosuria (who continue to have active disease despite attempted dietary modification): Oral: 300 mg/day, usually given in a single daily dose but may be given in 2 or 3 divided doses, if needed, to improve GI tolerability (Curhan 2018a; Ettinger 1986; Lipkin 2011).
Due to uric acid stones (off-label use): Oral: 300 mg/day, usually given in a single daily dose but may be given in 2 or 3 divided doses, if needed, to improve GI tolerability; use is reserved for patients who continue to have active disease despite urinary alkalinization therapy and increased hydration (Curhan 2018b; Heilberg 2016; Kenny 2010; Lipkin 2011).
Tumor lysis syndrome, prevention: Patients at intermediate risk for tumor lysis syndrome (TLS) and without preexisting hyperuricemia (serum uric acid ≥8 mg/dL [476 micromol/L]):
Note: Aggressive IV hydration should always be initiated prior to cytotoxic therapy in patients at elevated risk for TLS (Coiffier 2008).
Oral: 300 mg/m2/day or 10 mg/kg/day, given in 3 divided doses every 8 hours (maximum: 800 mg/day). Begin therapy 1 to 2 days before the start of induction chemotherapy and may continue for up to 3 to 7 days after chemotherapy until normalization of laboratory evidence of TLS (eg, serum uric acid, serum LDH) (Coiffier 2008; Larson 2018).
IV: 200 to 400 mg/m2/day, given in a single daily dose or in 2 or 3 divided doses (maximum: 600 mg/day). Begin therapy 1 to 2 days before the start of induction chemotherapy and may continue for 3 to 7 days after chemotherapy until normalization of laboratory evidence of TLS (eg, serum uric acid, serum LDH) (Coiffier 2008; Larson 2018).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Dosing presenting in multiple formats (mg/m2/dose, mg/m2/day, mg/kg/day, and a fixed mg dose); take extra precautions to ensure accuracy. Before prescribing allopurinol, consider testing for the HLA-B*5801 allele in patients at elevated risk for developing severe cutaneous adverse reactions (SCAR) (including Koreans with CKD ≥ stage 3 and all patients of Han Chinese or Thai descent). A negative HLA-B*5801 genetic test, however, does not entirely rule out the possibility of allopurinol-associated SCAR, so patients should still be appropriately monitored for SCAR, as well as other forms of hypersensitivity (ACR [Khanna 2012a]; Quach 2018; Saito 2016). Some experts suggest screening in all patients of Korean ethnicity regardless of renal function. Use should be avoided in any patient testing positive for the allele (Becker 2018).
Hyperuricemia associated with chemotherapy management: Maintain adequate hydration; begin allopurinol 1 to 2 days before initiation of induction chemotherapy; may continue for 3 to 7 days after chemotherapy (Coiffier 2008); daily doses >300 mg should be administered in divided doses:
Oral:
Manufacturer's labeling:
Children <6 years: 150 mg daily
Children 6 to 10 years: 300 mg daily
Children >10 years and Adolescents: 600 to 800 mg daily for 2 to 3 days in 2 to 3 divided doses
Alternate dosing: Tumor lysis syndrome; intermediate-risk: Limited data available (Coiffier 2008): Infants, Children, and Adolescents:
Weight-directed dosing: 10 mg/kg/day divided every 8 hours; maximum daily dose: 800 mg/day
BSA-directed dosing: 50 to 100 mg/m2/dose every 8 hours; maximum daily dose: 300 mg/m2/day
IV: For patients unable to tolerate oral therapy (BSA-directed dosing):
Manufacturer's labeling: Children and Adolescents: Initial: 200 mg/m2/day administered once daily or in equally divided doses at 6-, 8-, or 12-hour intervals
Alternate dosing: Tumor lysis syndrome; intermediate-risk: Limited data available: Infants, Children, and Adolescents: 200 to 400 mg/m2/day in 1 to 3 divided doses; maximum daily dose: 600 mg/day (Coiffier 2008)
Hyperuricemia associated with inborn errors of purine metabolism (Lesch-Nyhan syndrome): Limited data available: Oral: Infants, Children, and Adolescents: Initial: 5 to 10 mg/kg/day; adjust dose to maintain a high-normal serum uric acid concentration and a urinary uric acid/creatinine ratio <1; reported range: 3.7 to 9.7 mg/kg/day; usual maximum daily dose: 600 mg/day (Torres 2007a; Torres 2007b).
Recurrent calcium oxalate renal stones (including glycogen storage disease): Limited data available: Oral: Children and Adolescents: 4 to 10 mg/kg/day in divided doses 3 to 4 times daily; maximum daily dose: 300 mg/day (Copelvitch 2012; Santos-Victoriano 1998)
Reconstitution
Reconstitute powder for injection with 25 mL SWFI. Further dilute with NS or D5W to a final concentration of ≤6 mg/mL.
Extemporaneously Prepared
A 20 mg/mL oral suspension may be made with tablets and either a 1:1 mixture of Ora-Sweet® and Ora-Plus® or a 1:1 mixture of Ora-Sweet® SF and Ora-Plus® or a 1:4 mixture of cherry syrup concentrate and simple syrup, NF. Crush eight 300 mg tablets in a mortar and reduce to a fine powder. Add small portions of chosen vehicle and mix to a uniform paste; mix while adding the vehicle in incremental proportions to almost 120 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 120 mL. Label “shake well”. Stable for 60 days refrigerated or at room temperature (Allen 1996; Nahata 2004).
Allen LV Jr and Erickson MA 3rd, "Stability of Acetazolamide, Allopurinol, Azathioprine, Clonazepam, and Flucytosine in Extemporaneously Compounded Oral Liquids," Am J Health Syst Pharm, 1996, 53(16):1944-9.8862208Nahata MC, Pai VB, and Hipple TF, Pediatric Drug Formulations, 5th ed, Cincinnati, OH: Harvey Whitney Books Co, 2004.
Administration
Oral: Administer after meals.
IV: The rate of infusion depends on the volume of the infusion; infuse maximum single daily doses (600 mg/day) over ≥30 minutes. IV daily dose can be administered as a single infusion or in equally divided doses at 6-, 8-, or 12-hour intervals (manufacturer's labeling).
Tumor lysis syndrome prevention: Administer aggressive fluids sufficient to maintain adequate hydration and urinary output; whenever possible, allopurinol therapy should be initiated 24 to 48 hours before the start of chemotherapy (and other treatments) known to cause tumor lysis (Coiffier 2008).
Other indications: Administer fluids sufficient to yield daily urinary output of at least 2 L and to maintain a neutral or, preferably, slightly alkaline urine.
Dietary Considerations
For tumor lysis syndrome prevention, administer aggressive fluids sufficient to maintain adequate hydration and urinary output (Coiffier 2008). For other indications, fluid intake should be administered to yield neutral or slightly alkaline urine and an output of ~2 L (in adults).
Storage
Powder for injection: Store at 20°C to 25°C (68°F to 77°F). Following preparation, intravenous solutions in NS or D5W should be stored at 20°C to 25°C (68°F to 77°F). Do not refrigerate reconstituted and/or diluted product. Must be administered within 10 hours of solution preparation.
Tablet: Store at 15°C to 25°C (59°F to 77°F). Store in a dry place. Protect from light.
Allopurinol Images
Drug Interactions
Amoxicillin: Allopurinol may enhance the potential for allergic or hypersensitivity reactions to Amoxicillin. Monitor therapy
Ampicillin: Allopurinol may enhance the potential for allergic or hypersensitivity reactions to Ampicillin. Monitor therapy
Angiotensin-Converting Enzyme Inhibitors: May enhance the potential for allergic or hypersensitivity reactions to Allopurinol. Consider therapy modification
Antacids: May decrease the absorption of Allopurinol. Exceptions: Sodium Bicarbonate. Consider therapy modification
AzaTHIOprine: Allopurinol may increase serum concentrations of the active metabolite(s) of AzaTHIOprine. More specifically, allopurinol may increase mercaptopurine serum concentrations and promote formation of active thioguanine nucleotides. Management: Reduce the azathioprine dose to one third to one quarter of the usual dose if used concomitantly with allopurinol, and monitor closely for systemic toxicity (particularly hematologic toxicity, nausea, and vomiting). Consider therapy modification
Bacampicillin: Allopurinol may enhance the potential for allergic or hypersensitivity reactions to Bacampicillin. Monitor therapy
Bendamustine: Allopurinol may enhance the adverse/toxic effect of Bendamustine. Specifically, the risk of severe skin reactions may be enhanced. Monitor therapy
Capecitabine: Allopurinol may decrease serum concentrations of the active metabolite(s) of Capecitabine. Avoid combination
CarBAMazepine: Allopurinol may increase the serum concentration of CarBAMazepine. Monitor therapy
Cyclophosphamide: Allopurinol may enhance the adverse/toxic effect of Cyclophosphamide. Specifically, bone marrow suppression. Monitor therapy
CycloSPORINE (Systemic): Allopurinol may increase the serum concentration of CycloSPORINE (Systemic). Monitor therapy
Didanosine: Allopurinol may increase the serum concentration of Didanosine. Avoid combination
Doxofylline: Allopurinol may increase the serum concentration of Doxofylline. Monitor therapy
Loop Diuretics: May enhance the adverse/toxic effect of Allopurinol. Loop Diuretics may increase the serum concentration of Allopurinol. Specifically, Loop Diuretics may increase the concentration of Oxypurinol, an active metabolite of Allopurinol. Monitor therapy
Mercaptopurine: Allopurinol may increase the serum concentration of Mercaptopurine. Allopurinol may also promote formation of active thioguanine nucleotides. Management: Reduce the mercaptopurine dose to one third to one quarter of the usual dose if used with allopurinol, and monitor closely for systemic toxicity. US labeling for mercaptopurine oral suspension (Purixan brand) recommends avoiding allopurinol. Consider therapy modification
Pegloticase: Allopurinol may enhance the adverse/toxic effect of Pegloticase. Specifically, Allopurinol may blunt increases in serum urate that would signal an increased risk of anaphylaxis and infusion reactions. Avoid combination
Riluzole: Allopurinol may enhance the adverse/toxic effect of Riluzole. Specifically, the risk of hepatotoxicity may be increased. Management: Consider alternatives to allopurinol in patients receiving treatment with riluzole due to the potential for additive hepatotoxicity. Consider therapy modification
Tegafur: Allopurinol may diminish the therapeutic effect of Tegafur. Avoid combination
Theophylline Derivatives: Allopurinol may increase the serum concentration of Theophylline Derivatives. Exceptions: Dyphylline. Monitor therapy
Thiazide and Thiazide-Like Diuretics: May enhance the potential for allergic or hypersensitivity reactions to Allopurinol. Thiazide and Thiazide-Like Diuretics may increase the serum concentration of Allopurinol. Specifically, Thiazide Diuretics may increase the concentration of Oxypurinol, an active metabolite of Allopurinol. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Allopurinol may enhance the anticoagulant effect of Vitamin K Antagonists. Consider therapy modification
Adverse Reactions
1% to 10%:
Dermatologic: Maculopapular rash (≤3%; pruritic), skin rash (≤2%)
Endocrine & metabolic: Gout (≤6%; acute)
Gastrointestinal: Nausea (1%), vomiting (≤1%)
Renal: Renal failure syndrome (≤1%), renal insufficiency (≤1%)
Frequency not defined:
Gastrointestinal: Diarrhea
Hepatic: Increased serum alanine aminotransferase, increased serum alkaline phosphatase, increased serum aspartate aminotransferase
<1%, postmarketing, and/or case reports: Abdominal pain, acute respiratory distress syndrome, ageusia, agitation, agranulocytosis, albuminuria, alopecia, amblyopia, amnesia, anemia, anorexia, aplastic anemia, apnea, arthralgia, asthenia, asthma, bone marrow aplasia, bone marrow suppression, bradycardia, bronchospasm, cardiac disorder, cardiac failure, cataract, cellulitis, cerebral infarction, cerebrovascular accident, chills, cholestatic jaundice, chronic myelocytic leukemia (blast crisis), coma, confusion, conjunctivitis, constipation, decreased libido, depression, diaphoresis, disseminated intravascular coagulation, dizziness, drowsiness, dysgeusia, dyspepsia, dystonia, ecchymoses, ECG abnormality, eczema, edema, electrolyte disorder, enlargement of abdomen, enlargement of salivary glands, eosinophilia, eosinophilic fibrohistiocytic bone marrow lesion, epistaxis, exfoliative dermatitis, facial edema, fever, flatulence, flushing, foot-drop, furunculosis, gastritis, gastrointestinal hemorrhage, glycosuria, granulomatous hepatitis, gynecomastia, headache, hematuria, hemolytic anemia, hemorrhage, hemorrhagic pancreatitis, hepatic failure, hepatic necrosis, hepatomegaly, hepatotoxicity, hyperbilirubinemia, hypercalcemia, hyperglycemia, hyperkalemia, hyperlipidemia, hypernatremia, hyperphosphatemia, hypersensitivity angiitis, hypersensitivity reaction, hypertension, hyperuricemia, hypervolemia, hypocalcemia, hypokalemia, hypomagnesemia, hyponatremia, hypoprothrombinemia, hypotension, hypotonia, impotence, increased serum creatinine, infection, injection site reaction, insomnia, intestinal obstruction, iritis, jaundice, lactic acidosis, leukocytosis, leukopenia, lichen planus, low cardiac output, lymphadenopathy, lymphocytosis, macular retinitis, malaise, male infertility, mental status changes, metabolic acidosis, mucositis, myalgia, myoclonus, myopathy, necrotizing angiitis, nephritis, neuritis, neutropenia, oliguria, onycholysis, optic neuritis, pain, pancytopenia, paralysis, paresthesia, pericarditis, peripheral neuropathy, peripheral vascular disease, pharyngitis, proctitis, pruritus, pulmonary embolism, purpuric rash, respiratory failure, respiratory insufficiency, reticulocytosis, rhinitis, seizure, sepsis, septic shock, skin edema, splenomegaly, status epilepticus, Stevens-Johnson syndrome, stomatitis, tachypnea, thrombocytopenia, thrombophlebitis, tinnitus, tongue edema, toxic epidermal necrolysis, tremor, tumor lysis syndrome, twitching, uremia, urinary tract infection, urticaria, vasculitis, vasodilation, ventricular fibrillation, vertigo, vesicobullous dermatitis, water intoxication
Warnings/Precautions
Concerns related to adverse effects:
- Bone marrow suppression: Bone marrow suppression has been reported in patients receiving allopurinol, most of whom received concomitant medications with a potential for hematologic toxicity. The onset occurs between 6 weeks to 6 years after allopurinol initiation. Varying degrees of bone marrow depression affecting one or more cell lines may occur (rare) in patients receiving allopurinol alone.
- CNS effects: May occasionally cause drowsiness; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery or driving).
- Hepatotoxicity: Cases of hepatotoxicity (reversible) have been reported. Asymptomatic elevations of serum alkaline phosphatase or serum transaminases have been observed. Monitor for signs/symptoms of hepatotoxicity and evaluate liver function if they occur. Periodic liver function tests are recommended during the early stages of therapy in patients with preexisting hepatic impairment.
- Hypersensitivity: Use has been associated with a variety of hypersensitivity reactions, ranging from mild with maculopapular eruption (MPE) to severe cutaneous adverse reactions (SCAR), including Stevens-Johnson syndrome/toxic epidermal necrolysis (SJS/TEN), drug reaction with eosinophilia and systemic symptoms (DRESS), and the potentially life-threatening systemic manifestation, allopurinol hypersensitivity syndrome (AHS) (Stamp 2016). In some instances, a skin rash may be followed by more severe hypersensitivity reactions; discontinue at first sign of skin rash or other signs indicative of allergic reaction. Consider HLA-B*5801 testing prior to initiation of therapy in patients at elevated risk for SCAR (including Korean patients with CKD ≥ stage 3 and all patients of Han Chinese and Thai descent regardless of renal function) (ACR [Khanna 2012a]). Some experts suggest screening in patients of Korean ethnicity regardless of renal function. Avoid allopurinol in any patient testing positive for the allele (Becker 2019).
Disease-related concerns:
- Acute gout attacks: Even when normal or subnormal serum uric acid levels have been attained, an increase in acute gout attacks has been reported during the early stages of allopurinol administration. When allopurinol is initiated, maintenance colchicine doses should generally be administered as prophylaxis. Additionally, it is recommended to initiate with a low allopurinol dose (100 mg daily) and increase at weekly intervals by 100 mg until a serum uric acid level of 6 mg/dL or less is attained (do not exceed the maximum recommended dose of 800 mg/day). In some cases, colchicine or anti-inflammatory agents may be required to suppress gouty attacks. After several months of therapy, attacks usually decrease in duration and severity. These episodes may be due to mobilization of urates from tissue deposits, causing fluctuations in the serum uric acid levels. Even with adequate allopurinol therapy, several months may be required to deplete the uric acid pool enough to achieve control of the acute attacks.
- Renal impairment: Dose reductions are recommended in patients with renal impairment; monitor closely. Patients with reduced renal function receiving thiazide diuretics in combination with allopurinol may be at increased risk for hypersensitivity reactions. Some patients with preexisting renal disease or poor urate clearance have shown a rise in BUN with allopurinol. Patients with renal impairment should be carefully monitored during the early stages of allopurinol treatment; reduce the dose or withdraw therapy if increased renal function abnormalities appear and persist. Renal failure associated with allopurinol has been observed in patients with hyperuricemia secondary to neoplastic diseases. Concurrent conditions including multiple myeloma and congestive myocardial disease were present among patients whose renal dysfunction increased after allopurinol was begun. Renal failure is also frequently associated with gouty nephropathy and rarely with hypersensitivity reactions associated with allopurinol. Albuminuria has been observed among patients who developed clinical gout following chronic glomerulonephritis and chronic pyelonephritis.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant drug interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
- Concomitant medications: Concomitant use of allopurinol (at doses of 300 to 600 mg/day) with mercaptopurine or azathioprine will require a reduction in the mercaptopurine or azathioprine dose to approximately one-third to one-fourth of the usual dose. Subsequent dose adjustments may be necessary based on therapeutic response and toxicity.
Other warnings/precautions:
- Hydration: For tumor lysis syndrome prevention, administer aggressive fluids sufficient to maintain adequate hydration and urinary output (Coiffier 2008). For other indications, fluid intake sufficient to yield a daily urinary output of at least 2 L and maintenance of a neutral or (preferably) a slightly alkaline urine are desirable in order to avoid possible formation of xanthine calculi due to allopurinol therapy and to help prevent renal urate precipitation in patients receiving concomitant uricosuric agents.
Monitoring Parameters
CBC, serum uric acid levels every 2 to 5 weeks during dose titration until desired level is achieved and every 6 months thereafter (ACR [Khanna 2012a]), liver function tests (periodically in patients with preexisting hepatic disease), renal function (BUN, serum creatinine, or creatinine clearance [prior to initiation and periodically]), prothrombin time (periodically in patients receiving warfarin). Monitor hydration status, signs/symptoms of hepatotoxicity, and signs/symptoms of hypersensitivity reactions, including SCAR. Consider HLA-B*5801 testing prior to initiation of therapy in patients at elevated risk for SCAR.
Pregnancy
Pregnancy Considerations
Allopurinol crosses the placenta (Torrance 2009).
Information related to allopurinol in pregnancy is limited. Based on available information, an increased risk of adverse fetal events has not been observed (Hoeltzenbein 2013).
Patient Education
What is this drug used for?
- It is used to lower uric acid in the blood.
- It is used to prevent high uric acid levels during chemo.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Diarrhea
- Nausea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain.
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Infection
- Kidney stone like back pain, abdominal pain, or blood in the urine.
- Painful urination
- Eye irritation
- Vision changes
- Joint pain
- Swollen glands
- Shortness of breath
- Excessive weight gain
- Swelling of arms or legs
- Chest pain
- Bruising
- Bleeding
- Severe loss of strength and energy
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.