Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Nuvigil: 50 mg, 150 mg, 200 mg, 250 mg
Generic: 50 mg, 150 mg, 200 mg, 250 mg
Pharmacology
Mechanism of Action
The exact mechanism of action of armodafinil is unknown. It is the R-enantiomer of modafinil. Armodafinil binds to the dopamine transporter and inhibits dopamine reuptake, which may result in increased extracellular dopamine levels in the brain. However, it does not appear to be a dopamine receptor agonist and also does not appear to bind to or inhibit the most common receptors or enzymes that are relevant for sleep/wake regulation.
Pharmacokinetics/Pharmacodynamics
Absorption
Readily absorbed
Distribution
Vd: 42 L
Metabolism
Hepatic, multiple pathways, including amine hydrolysis and CYP3A4/5; metabolites include R-modafinil acid and modafinil sulfone
Excretion
Urine (based on modafinil: 80% predominantly as metabolites; <10% as unchanged drug)
Time to Peak
2 hours (fasted)
Half-Life Elimination
~15 hours
Protein Binding
~60% (based on modafinil; primarily albumin)
Use in Specific Populations
Special Populations: Renal Function Impairment
Severe chronic renal failure (CrCl ≤20 mL/minute) did not influence the pharmacokinetics of modafinil, but increased exposure to modafinil acid ninefold.
Special Populations: Hepatic Function Impairment
In patients with severe hepatic impairment, clearance of modafinil was decreased by ~60% and the steady-state concentration was doubled.
Special Populations: Elderly
Systemic exposure of armodafinil was ~15% higher and clearance was ~12% lower in patients greater than 65 years of age.
Use: Labeled Indications
Narcolepsy: To improve wakefulness in patients with excessive sleepiness associated with narcolepsy.
Obstructive sleep apnea: To improve wakefulness in patients with excessive sleepiness associated with obstructive sleep apnea (OSA).
Limitations of use: In OSA, armodafinil is indicated to treat excessive sleepiness and not as treatment for the underlying obstruction. If continuous positive airway pressure (CPAP) is the treatment of choice for a patient, a maximal effort to treat with CPAP for an adequate period of time should be made prior to initiating armodafinil for excessive sleepiness.
Shift-work disorder: To improve wakefulness in patients with excessive sleepiness associated with shift-work disorder.
Contraindications
Hypersensitivity to armodafinil, modafinil, or any component of the formulation.
Dosage and Administration
Dosing: Adult
Narcolepsy: Oral: 150 to 250 mg once daily in the morning
Obstructive sleep apnea (OSA): Oral: 150 to 250 mg once daily in the morning; doses >150 mg have not been shown to have an increased benefit.
Shift-work disorder: Oral: 150 mg given once daily ~1 hour prior to work shift
Dosing: Geriatric
Refer to adult dosing. Consider lower initial dosage.
Administration
May be administered without regard to food.
Storage
Store at 20°C to 25°C (68°F to 77°F).
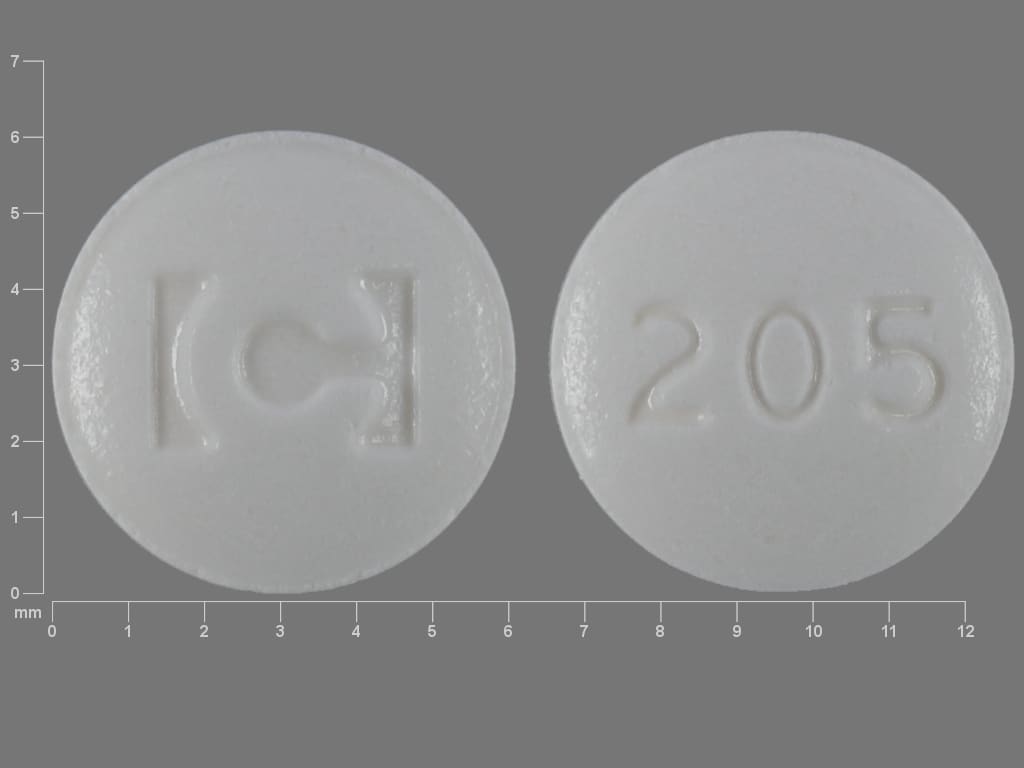
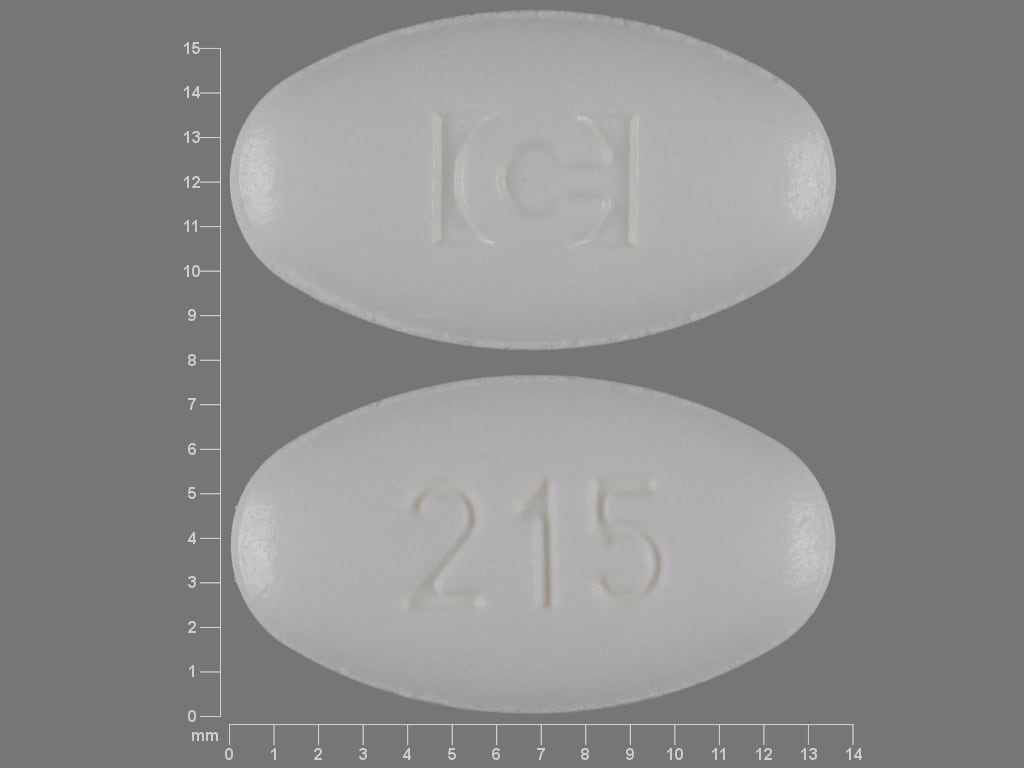
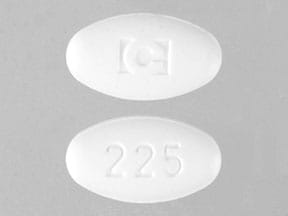
Armodafinil Images
Drug Interactions
Acebrophylline: May enhance the stimulatory effect of CNS Stimulants. Avoid combination
Alcohol (Ethyl): May diminish the therapeutic effect of Armodafinil. Avoid combination
ARIPiprazole: Armodafinil may decrease the serum concentration of ARIPiprazole. Monitor therapy
AtoMOXetine: May enhance the hypertensive effect of Sympathomimetics. AtoMOXetine may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Cannabinoid-Containing Products: May enhance the tachycardic effect of Sympathomimetics. Exceptions: Cannabidiol. Monitor therapy
CloZAPine: CYP3A4 Inducers (Weak) may decrease the serum concentration of CloZAPine. Monitor therapy
Cocaine (Topical): May enhance the hypertensive effect of Sympathomimetics. Management: Consider alternatives to use of this combination when possible. Monitor closely for substantially increased blood pressure or heart rate and for any evidence of myocardial ischemia with concurrent use. Consider therapy modification
CycloSPORINE (Systemic): Armodafinil may decrease the serum concentration of CycloSPORINE (Systemic). Monitor therapy
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Doxofylline: Sympathomimetics may enhance the adverse/toxic effect of Doxofylline. Monitor therapy
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Esketamine: May enhance the hypertensive effect of CNS Stimulants. Monitor therapy
Estrogen Derivatives (Contraceptive): Armodafinil may decrease the serum concentration of Estrogen Derivatives (Contraceptive). Management: Use alternative or concomitant methods of contraception in patients taking armodafinil and for one month after armodafinil discontinuation. Consider therapy modification
Guanethidine: May enhance the arrhythmogenic effect of Sympathomimetics. Guanethidine may enhance the hypertensive effect of Sympathomimetics. Monitor therapy
Iobenguane Radiopharmaceutical Products: CNS Stimulants may diminish the therapeutic effect of Iobenguane Radiopharmaceutical Products. Management: Discontinue all drugs that may inhibit or interfere with catecholamine transport or uptake for at least 5 biological half-lives before iobenguane administration. Do not administer these drugs until at least 7 days after each iobenguane dose. Avoid combination
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Linezolid: May enhance the hypertensive effect of Sympathomimetics. Management: Reduce initial doses of sympathomimetic agents, and closely monitor for enhanced pressor response, in patients receiving linezolid. Specific dose adjustment recommendations are not presently available. Consider therapy modification
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Lumateperone: Armodafinil may decrease the serum concentration of Lumateperone. Monitor therapy
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
NiMODipine: CYP3A4 Inducers (Weak) may decrease the serum concentration of NiMODipine. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Solriamfetol: Sympathomimetics may enhance the hypertensive effect of Solriamfetol. Monitor therapy
Solriamfetol: CNS Stimulants may enhance the hypertensive effect of Solriamfetol. Monitor therapy
Sympathomimetics: May enhance the adverse/toxic effect of other Sympathomimetics. Monitor therapy
Tedizolid: May enhance the hypertensive effect of Sympathomimetics. Tedizolid may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Ubrogepant: CYP3A4 Inducers (Weak) may decrease the serum concentration of Ubrogepant. Management: Use an initial ubrogepant dose of 100 mg and second dose (if needed) of 100 mg when used with a weak CYP3A4 inducer. Consider therapy modification
Adverse Reactions
>10%: Central nervous system: Headache (14% to 23%; dose related)
1% to 10%:
Cardiovascular: Palpitations (2%), increased heart rate (1%)
Central nervous system: Insomnia (4% to 6%; dose related), dizziness (5%), anxiety (4%), depression (1% to 3%; dose related), fatigue (2%), agitation (1%), depressed mood (1%), lack of concentration (1%), migraine (1%), nervousness (1%), pain (1%), paresthesia (1%)
Dermatologic: Skin rash (1% to 4%; dose related), contact dermatitis (1%), diaphoresis (1%)
Endocrine & metabolic: Increased gamma-glutamyl transferase (1%), increased thirst (1%)
Gastrointestinal: Nausea (6% to 9%; dose related), xerostomia (2% to 7%; dose related), diarrhea (4%), dyspepsia (2%), upper abdominal pain (2%), anorexia (1%), constipation (1%), decreased appetite (1%), loose stools (1%), vomiting (1%)
Hypersensitivity: Seasonal allergy (1%)
Neuromuscular & skeletal: Tremor (1%)
Renal: Polyuria (1%)
Respiratory: Dyspnea (1%), flu-like symptoms (1%)
Miscellaneous: Fever (1%)
<1%, postmarketing, and/or case reports: Anaphylaxis, angioedema, DRESS syndrome, hypersensitivity reaction (including bronchospasm, dysphagia), hypouricemia, increased liver enzymes, increased serum alkaline phosphatase, irritability, multi-organ hypersensitivity, oral mucosa changes (including blistering, sores, ulceration), pancytopenia, skin changes (including blistering, sores, ulceration), Stevens-Johnson syndrome, suicidal ideation, systolic hypertension, toxic epidermal necrolysis
Warnings/Precautions
Concerns related to adverse effects:
- CNS effects: May impair the ability to engage in potentially hazardous activities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery, driving).
- Dermatologic effects (severe): Serious and life-threatening rashes including Stevens-Johnson syndrome and toxic epidermal necrolysis have been reported. In modafinil clinical trials, rashes were more likely to occur in children; serious, postmarketing reactions have occurred with modafinil and armodafinil in adults and children. Most cases have been reported within the first 8 weeks of initiating therapy; however, rare cases have occurred after prolonged therapy. No risk factors have been identified to predict occurrence or severity of these reactions. Patients should be advised to discontinue use at first sign of rash, skin or mouth sores or blistering or ulceration (unless the rash is clearly not drug-related).
- Hypersensitivity reactions: Rare cases of drug reaction with eosinophilia and system symptoms (DRESS), also known as multiorgan hypersensitivity, and cases of angioedema and anaphylactoid reactions have been reported. Signs and symptoms of DRESS are diverse. Patients typically present with fever and rash associated with other organ system involvement. Patients should be advised to discontinue therapy and promptly report any signs or symptoms related to these adverse effects.
Disease-related concerns:
- Cardiovascular disease: Use is not recommended in patients with a history of left ventricular hypertrophy or patients with mitral valve prolapse who have developed mitral valve prolapse syndrome with previous CNS stimulant use. Patients with these conditions may also experience chest pain, palpitations, dyspnea, and transient ischemic T-wave changes on ECG. Due to limited experience use caution in patients with history of myocardial infarction (MI) or angina. Increased blood pressure monitoring may be required, and new or additional antihypertensive therapy may be needed.
- Hepatic impairment: Use with caution in patients with hepatic impairment; dosage reduction is recommended with severe dysfunction.
- Psychiatric disorders: Use caution in patients with a history of psychosis, depression, or mania. Armodafinil has been shown to worsen the symptoms of these diseases (eg, mania, hallucinations, suicidal thoughts). Discontinue therapy if psychiatric symptoms develop.
- Sleep disorders: Appropriate use: For use following complete evaluation of sleepiness and in conjunction with other standard treatments (eg, CPAP). The degree of sleepiness should be reassessed frequently; some patients may not return to a normal level of wakefulness. Patients with excessive sleepiness should be advised to avoid driving or any other potentially dangerous activity. Use >12 weeks has not been studied; patient should be reevaluated to determine effectiveness if use exceeds 12 weeks.
- Tourette syndrome/tics: Use with caution in patients with Tourette syndrome and other tic disorders. Stimulants may exacerbate tics (motor and phonic) and Tourette syndrome; however, evidence demonstrating increased tics is limited. Evaluate for tics and Tourette syndrome prior to therapy initiation (AACAP [Murphy 2013]; Pliszka 2007).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Use reduced doses in elderly patients; concentrations of armodafinil are significantly higher in patients >65 years of age.
Other warnings/precautions:
- Abuse potential: Use with caution in patients with a history of drug abuse; potential for drug dependency exists.
Monitoring Parameters
Signs of hypersensitivity, rash, psychiatric symptoms, levels of sleepiness, blood pressure, and drug abuse
Pregnancy
Pregnancy Considerations
Preliminary data from the Nuvigil/Provigil pregnancy registry suggest an increased risk of major fetal congenital malformations, including congenital cardiac anomalies (Alertec Canadian product monograph 2019). Intrauterine growth restriction and spontaneous abortion have been reported in association with armodafinil.
Efficacy of steroidal contraceptives (including depot and implantable contraceptives) may be decreased; alternate means of effective contraception or the addition of a barrier method should be used during armodafinil therapy and for 1 month after armodafinil is discontinued.
A pregnancy registry has been established for patients exposed to armodafinil; healthcare providers are encouraged to register pregnant patients or pregnant females may register themselves by calling 1-866-404-4106.
Patient Education
What is this drug used for?
- It is used to treat a lot of sleepiness that may happen with sleep apnea, narcolepsy, or shift work problems.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Trouble sleeping
- Nausea
- Dry mouth
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Depression like thoughts of suicide, anxiety, emotional instability, or confusion.
- Swollen glands
- Sensing things that seem real but are not
- Behavioral changes
- Chest pain
- Fast heartbeat
- Confusion
- Severe headache
- Dizziness
- Passing out
- Vision changes
- Anxiety
- Abnormal heartbeat
- Dark urine
- Yellow skin
- Unable to pass urine
- Change in amount of urine passed
- Chills
- Shortness of breath
- Swelling of arms or legs
- Bruising
- Bleeding
- Severe loss of strength and energy
- Muscle pain
- Joint pain
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.