Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
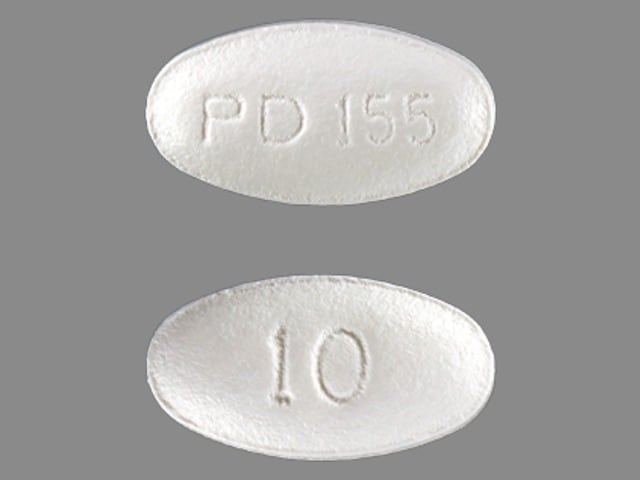
Lipitor: 10 mg, 20 mg, 40 mg, 80 mg
Generic: 10 mg, 20 mg, 40 mg, 80 mg
Pharmacology
Mechanism of Action
Inhibitor of 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase, the rate-limiting enzyme in cholesterol synthesis (reduces the production of mevalonic acid from HMG-CoA); this then results in a compensatory increase in the expression of LDL receptors on hepatocyte membranes and a stimulation of LDL catabolism. In addition to the ability of HMG-CoA reductase inhibitors to decrease levels of high-sensitivity C-reactive protein (hsCRP), they also possess pleiotropic properties including improved endothelial function, reduced inflammation at the site of the coronary plaque, inhibition of platelet aggregation, and anticoagulant effects (de Denus 2002; Ray 2005).
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Rapidly absorbed; extensive first-pass metabolism in GI mucosa and liver
Distribution
Vd: ~381 L
Metabolism
Hepatic via CYP3A4; forms active ortho- and parahydroxylated derivatives and an inactive beta-oxidation product; plasma concentrations are elevated in patients with chronic alcoholic liver disease and Child-Pugh class A and B liver disease
Excretion
Bile (following hepatic and/or extra-hepatic metabolism; does not appear to undergo enterohepatic recirculation); urine (<2% as unchanged drug)
Onset of Action
Initial changes: 3 to 5 days; Maximal reduction in plasma cholesterol and triglycerides: 2 to 4 weeks; LDL reduction: 10 mg/day: 39% (for each doubling of this dose, LDL is lowered approximately 6%)
Time to Peak
Serum: 1 to 2 hours
Half-Life Elimination
Parent drug: ~14 hours; Equipotent metabolites: 20 to 30 hours
Protein Binding
≥98%
Use in Specific Populations
Special Populations: Hepatic Function Impairment
Cmax and AUC are each 4-fold greater in patients with Child-Pugh class A disease; Cmax and AUC are ~16-fold and 11-fold increased, respectively, in patients with Child-Pugh class B disease.
Special Populations: Elderly
Plasma concentrations are higher (~40% for Cmax and 30% for AUC).
Special Populations: Gender
Plasma concentrations in women differ from those in men (~ 20% higher for Cmax and 10% lower for AUC)
Use: Labeled Indications
Heterozygous familial hypercholesterolemia: To reduce elevated total cholesterol (total-C), LDL cholesterol (LDL-C), apolipoprotein B (apo B), and triglyceride levels, and to increase HDL cholesterol in patients with primary hypercholesterolemia.
Heterozygous familial hypercholesterolemia (pediatrics): To reduce total-C, LDL-C, and apo B levels in pediatric patients 10 to 17 years of age with heterozygous familial hypercholesterolemia with LDL-C ≥190 mg/dL, LDL-C ≥160 mg/dL with positive family history of premature cardiovascular disease (CVD), or LDL-C ≥160 mg/dL with 2 or more other CVD risk factors.
Homozygous familial hypercholesterolemia: To reduce total-C and LDL-C in patients with homozygous familial hypercholesterolemia as an adjunct to other lipid-lowering treatments (eg, LDL apheresis) or if such treatments are unavailable.
Prevention of atherosclerotic cardiovascular disease:
Primary prevention of atherosclerotic cardiovascular disease (ASCVD): To reduce the risk of myocardial infarction (MI), stroke, revascularization procedures, and angina in adult patients without a history of coronary heart disease (CHD) but who have multiple CHD risk factors.
Secondary prevention in patients with established ASCVD: To reduce the risk of MI, stroke, revascularization procedures, and angina in patients with a history of CHD.
Use: Off Label
Transplantation, post heart or post kidneyyes
Based on the 2010 International Society of Heart and Lung Transplantation guidelines for the care of heart transplant recipients, atorvastatin is effective and recommended following heart transplant, regardless of cholesterol levels, to reduce cardiac allograft vasculopathy and improve long-term outcomes.
Based on the 2013 Kidney Disease: Improving Global Outcomes clinical practice guideline for lipid management in chronic kidney disease, atorvastatin is suggested following kidney transplant to reduce cardiovascular events (eg, myocardial infarction, stroke, cardiovascular death).
Contraindications
Hypersensitivity to atorvastatin or any component of the formulation; active liver disease; unexplained persistent elevations of serum transaminases; pregnancy; breastfeeding
Canadian labeling: Additional contraindications (not in US labeling): Concurrent therapy with cyclosporine or glecaprevir/pibrentasvir
Dosage and Administration
Dosing: Adult
Note: Use in conjunction with lifestyle modification (eg, diet and exercise). When choosing to initiate therapy and selecting dose intensity, consider the following: Age, baseline LDL cholesterol (LDL-C), 10-year atherosclerotic cardiovascular disease (ASCVD) risk, risk-enhancing factors, potential adverse effects, and drug interactions. High-intensity statin therapy (atorvastatin 40 to 80 mg/day) generally reduces LDL-C by ≥50%. Moderate-intensity statin therapy (atorvastatin 10 to 20 mg/day) generally reduces LDL-C by ~30% to 49%. Assess response ~1 to 3 months after initiation of therapy or dose adjustment and every 3 to 12 months thereafter (ACC/AHA [Grundy 2019]; ACC/AHA [Stone 2014]).
Heterozygous familial hypercholesterolemia:
Note: Multiple lipid-lowering therapies may be needed if statin monotherapy is not effective. Referral to a lipid specialist should be considered if treatment goals are not met (ACC/AHA [Grundy 2019]; Rosenson 2019a; Smilde 2001; Stein 2003).
High-intensity therapy: Oral: Initial: 40 or 80 mg once daily; if 40 mg once daily is initiated and tolerated, increase to 80 mg once daily.
Homozygous familial hypercholesterolemia:
Note: Multiple lipid-lowering therapies are usually needed to achieve treatment goals; treatment should be guided by an experienced lipid specialist (Rosenson 2019a).
High-intensity therapy: Oral: 80 mg once daily (Rosenson 2019a).
Prevention of atherosclerotic cardiovascular disease:
Note: If LDL-C goal (eg, percent reduction or absolute goal) is not met with the initial dose, may consider up-titration based on estimated 10-year ASCVD risk (see ACC/AHA ASCVD Risk Estimator online), LDL-C response, and tolerability. If LDL-C goal is not met with maximally tolerated dose, additional lipid-lowering therapy may be warranted (ACC/AHA [Grundy 2019]; ACC/AHA [Stone 2014]).
Primary prevention:
Patients without diabetes, age 40 to 75 years, and LDL-C 70 to 189 mg/dL:
ASCVD 10-year risk 5% to <7.5%:
Note: Depending on baseline LDL-C and presence of risk-enhancing factors, consider statin therapy after shared decision-making with patient. Some experts suggest shared decision-making if ASCVD 10-year risk is 5% to 10%; however, in patients with a baseline LDL-C ≥160 mg/dL, statin therapy is usually recommended (Pignone 2019).
Moderate-intensity therapy: Oral: 10 to 20 mg once daily to reduce LDL-C by 30% to 49% (ACC/AHA [Grundy 2019]; ACC/AHA [Stone 2014]).
ASCVD 10-year risk ≥7.5% to <20%:
Note: Depending on baseline LDL-C and presence of risk-enhancing factors, consider statin therapy after shared decision-making with patient. Some experts suggest initiating moderate-intensity statin therapy in most patients if ASCVD 10-year risk is >10% to <20% and an LDL-C >100 mg/dL (Pignone 2019).
Moderate-intensity therapy: Oral: 10 to 20 mg once daily to reduce LDL-C by 30% to 49%; higher risk patients with multiple risk-enhancing factors may benefit from higher doses to reduce LDL-C by ≥50% (ACC/AHA [Grundy 2019]).
ASCVD 10-year risk ≥20%: High-intensity therapy: Oral: 80 mg once daily to reduce LDL-C by ≥50%; if unable to tolerate due to adverse effects, may reduce dose to 40 mg once daily (ACC/AHA [Grundy 2019]; ACC/AHA [Stone 2014]. Alternatively, start 40 mg once daily and titrate to 80 mg once daily if LDL-C remains above target (Pignone 2019).
Patients with diabetes:
Age 40 to 75 years without additional ASCVD risk factors: Moderate-intensity therapy: Oral: 10 to 20 mg once daily to reduce LDL-C by 30% to 49% (ACC/AHA [Grundy 2019]; ACC/AHA [Stone 2014]).
ASCVD risk >20% or multiple ASCVD risk factors: High-intensity therapy: Oral: 80 mg once daily to reduce LDL-C by ≥50%; if unable to tolerate due to adverse effects, may reduce dose to 40 mg once daily (ACC/AHA [Grundy 2019]; ACC/AHA [Stone 2014]).
LDL-C ≥190 mg/dL and age 20 to 75 years: High-intensity therapy: Oral: 80 mg once daily to reduce LDL-C by ≥50%; if unable to tolerate due to adverse effects, may reduce dose to 40 mg once daily. Note: Consider familial hypercholesterolemia, which is preferably managed by an experienced lipid specialist (ACC/AHA [Grundy 2019]; ACC/AHA [Stone 2014]).
Secondary prevention in patients with established atherosclerotic cardiovascular disease (eg, coronary heart disease, cerebrovascular disease [ischemic stroke or transient ischemic attack], peripheral arterial disease):
Note: Patients with high-risk ASCVD may require additional therapies to achieve LDL-C goal (eg, <70 mg/dL or <50 mg/dL if very high risk).
High-intensity therapy: Oral: 80 mg once daily to reduce LDL-C by ≥50%; if unable to tolerate 80 mg once daily, may reduce dose to 40 mg once daily; if unable to tolerate 40 mg once daily, may reduce dose to 10 to 20 mg once daily (ACC/AHA [Grundy 2019]; ACC/AHA [Stone 2014]).
Transplantation, post heart or post kidney (off-label use):
Note: Initiate after transplant regardless of baseline cholesterol levels. Certain immunosuppressive drugs can induce or exacerbate hypercholesterolemia; significant drug interactions between statins and immunosuppressant drugs are frequent; many interactions can increase statin serum concentrations and risk of toxicity (eg, myopathy) (Brennan 2019; Costanzo 2010; KDIGO 2013; Wiggins 2016). Consult drug interactions database for more detailed information.
Oral: Initial: 10 mg once daily starting 1 to 2 weeks after transplant; increase dose based on response and tolerability up to 20 mg once daily (Brennan 2019; Costanzo 2010; Wiggins 2016).
Dosing: Geriatric
Prevention of atherosclerotic cardiovascular disease:
Note: If LDL cholesterol (LDL-C) goal (eg, percent reduction or absolute goal) is not met with the initial dose, may consider up-titration based on estimated 10-year atherosclerotic cardiovascular disease (ASCVD) risk (see ACC/AHA ASCVD Risk Estimator online), LDL-C response, and tolerability. If LDL-C goal is not met with maximally tolerated dose, additional lipid-lowering therapy may be warranted (ACC/AHA [Grundy 2019]; ACC/AHA [Stone 2014]).
Primary prevention:
Age >75 years: Note: Assess ASCVD risk, life expectancy, and likelihood for adverse effects. Consider moderate-intensity therapy after shared decision-making with patient:
Oral: 10 to 20 mg once daily (ACC/AHA [Grundy 2019]; ACC/AHA [Stone 2014]; ADA 2019).
Secondary prevention in patients with established atherosclerotic cardiovascular disease (eg, coronary heart disease, cerebrovascular disease [ischemic stroke or transient ischemic attack], peripheral arterial disease):
Note: Patients with high-risk ASCVD may require additional therapies to achieve LDL-C goal (eg, <70 mg/dL or <50 mg/dL if very high risk).
Age >75 years: Moderate- to high-intensity therapy: Oral: 10 to 80 mg once daily (ACC/AHA [Grundy 2019]); if a moderate-intensity dose (10 to 20 mg once daily) is started and tolerated, increase to a high-intensity dose (40 to 80 mg once daily) within 3 months (Rosenson 2019b).
Refer to adult dosing for other indications.
Dosing: Pediatric
Dosage should be individualized according to the baseline LDL-C level, the recommended goal of therapy, and patient response; adjustments should be made at intervals of 4 weeks.
Heterozygous familial and nonfamilial hypercholesterolemia:
Note: Begin treatment if after adequate trial (6 to 12 months) of intensive lifestyle modification emphasizing body weight normalization and diet, the following are present (AACE [Jellinger 2017]):
LDL-C ≥190 mg/dL or
LDL-C remains ≥160 mg/dL and 2 or more cardiovascular risk factors: family history of premature atherosclerotic cardiovascular disease (<55 years of age); overweight; obesity; or other elements of insulin resistance syndrome or
LDL-C ≥130 mg/dL and diabetes mellitus (Daniels 2008; NHLBI 2011).
Children 6 to <10 years of age (Tanner stage I): Limited data available: Oral: Initial: 5 mg once daily; if target LDL-C not achieved after 4 weeks, may increase incrementally by doubling dose (10 mg/day, 20 mg/day) at monthly intervals until target LDL-C; usual maximum daily dose: 40 mg/day; however, in some cases doses up to 80 mg/day have been used; dosing based on a long-term trial (3 years) of 272 patients (age range: 6 to 15 years); doses of 80 mg/day were used in 12 patients <10 years of age; over the 3 year study duration, similar efficacy was observed without growth or maturation impairment (Langslet 2016).
Children and Adolescents 10 to 17 years: Oral: Initial: 10 mg once daily; if target LDL-C not achieved after 4 weeks, may increase incrementally by doubling dose (20 mg/day, 40 mg/day) at monthly intervals until target LDL-C up to a maximum daily dose: 80 mg/day (Langslet 2016).
Hyperlipidemia: Limited data available: Children and Adolescents 10 to 17 years (males and postmenarchal females): Oral: Initial: 10 mg once daily; if LDL-C target not achieved after 1 to 3 months, may increase to meet target LDL-C; in pediatric patients with heterozygous familial hypercholesterolemia, a maximum titrated dose based upon LDL response: 80 mg/day was used (Langslet 2016; McCrindle 2007; NHLBI 2011).
Prevention of graft coronary artery disease: Limited data available: Children and Adolescents: Oral: 0.2 mg/kg/day rounded to nearest 2.5 mg increment; not to exceed age-appropriate doses (Chin 2002; Chin 2008).
Dosing adjustment for toxicity: Muscle symptoms (potential myopathy): Children ≥10 years and Adolescents: Discontinue use until symptoms can be evaluated; check CPK level; based on experience in adult patients, also evaluate patient for conditions that may increase the risk for muscle symptoms (eg, hypothyroidism, reduced renal or hepatic function, rheumatologic disorders such as polymyalgia rheumatica, steroid myopathy, vitamin D deficiency, or primary muscle diseases). Upon resolution (symptoms and any associated CPK abnormalities), resume the original or consider a lower dose of atorvastatin and retitrate. If muscle symptoms recur, discontinue atorvastatin use. After muscle symptom resolution, may reinitiate a different statin at an initial low dose; gradually increase if tolerated. Based on experience in adult patients, if muscle symptoms or elevated CPK persists for 2 months in the absence of continued statin use, consider other causes of muscle symptoms. If determined to be due to another condition aside from statin use, may resume statin therapy at the original dose (NHLBI 2011; Stone 2014).
Dosing: Adjustment for Toxicity
Severe muscle symptoms or fatigue: Promptly discontinue use; evaluate CPK, creatinine, and urinalysis for myoglobinuria (ACC/AHA [Stone 2014]).
Mild to moderate muscle symptoms: Discontinue use until symptoms can be evaluated; evaluate patient for conditions that may increase the risk for muscle symptoms (eg, hypothyroidism, reduced renal or hepatic function, rheumatologic disorders such as polymyalgia rheumatica, steroid myopathy, vitamin D deficiency, or primary muscle diseases). Upon resolution, resume the original or lower dose of atorvastatin. If muscle symptoms recur, discontinue atorvastatin use. After muscle symptom resolution, may use a low dose of a different statin; gradually increase if tolerated. In the absence of continued statin use, if muscle symptoms or elevated CPK continues after 2 months, consider other causes of muscle symptoms. If determined to be due to another condition aside from statin use, may resume statin therapy at the original dose (ACC/AHA [Stone 2014]).
Administration
Oral: Administer with or without food; may take without regard to time of day. The manufacturer's labeling states tablets should not be broken; however, available data do not indicate any safety or efficacy concerns with this practice.
Dietary Considerations
Before initiation of therapy, patients should be placed on a standard cholesterol-lowering diet for 3 to 6 months and the diet should be continued during drug therapy. Atorvastatin serum concentration may be increased when taken with grapefruit juice; avoid concurrent intake of large quantities (>1 quart/day).
Red yeast rice contains variable amounts of several compounds that are structurally similar to HMG-CoA reductase inhibitors, primarily monacolin K (or mevinolin) which is structurally identical to lovastatin; concurrent use of red yeast rice with HMG-CoA reductase inhibitors may increase the incidence of adverse and toxic effects (Lapi 2008; Smith 2003).
Storage
Store at 20°C to 25°C (68°F to 77°F).
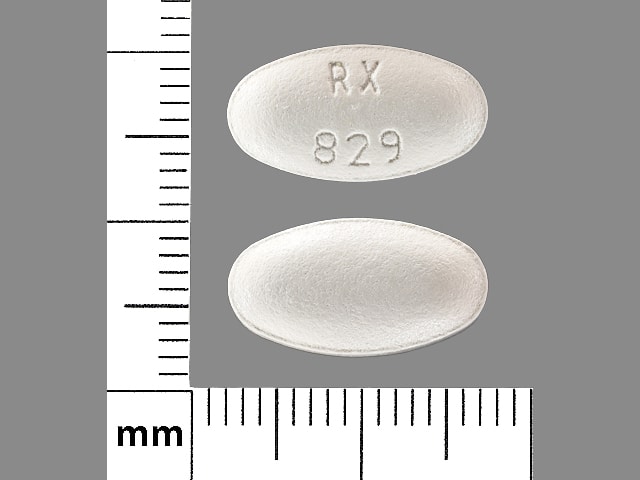
AtorvaSTATin Images
Drug Interactions
Acipimox: May enhance the myopathic (rhabdomyolysis) effect of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Aliskiren: AtorvaSTATin may increase the serum concentration of Aliskiren. Monitor therapy
Amiodarone: May increase the serum concentration of AtorvaSTATin. Monitor therapy
Antihepaciviral Combination Products: May increase the serum concentration of AtorvaSTATin. Avoid combination
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Asunaprevir: May increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Azithromycin (Systemic): May enhance the myopathic (rhabdomyolysis) effect of AtorvaSTATin. Monitor therapy
Bexarotene (Systemic): May decrease the serum concentration of AtorvaSTATin. Monitor therapy
Bezafibrate: May enhance the myopathic (rhabdomyolysis) effect of HMG-CoA Reductase Inhibitors (Statins). Bezafibrate may increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). More specifically, bezafibrate may increase the serum concentration of fluvastatin Management: Monitor patients closely for myopathy with concomitant use of bezafibrate and HMG-CoA reductase inhibitors. Concomitant use is contraindicated in patients predisposed to myopathy and alternative therapy should be considered. Consider therapy modification
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Cimetidine: AtorvaSTATin may enhance the adverse/toxic effect of Cimetidine. Specifically, there is a theoretical potential for enhanced effects on reducing endogenous steroid activity. Monitor therapy
Ciprofibrate: May enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Management: Avoid the use of HMG-CoA reductase inhibitors and ciprofibrate if possible. If concomitant therapy is considered, benefits should be carefully weighed against the risks, and patients should be monitored closely for signs/symptoms of muscle toxicity. Consider therapy modification
Clarithromycin: May increase the serum concentration of AtorvaSTATin. Management: Limit atorvastatin to a maximum dose of 20 mg/day (for adults) when used with clarithromycin. If this combination is used, monitor patients more closely for evidence of atorvastatin toxicity. Consider therapy modification
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Cobicistat: May increase the serum concentration of AtorvaSTATin. Management: Avoid the combined use of atorvastatin with atazanavir/cobicistat. Atorvastatin dose should not exceed 20 mg daily when combined with other cobicistat-containing regimens. Consider therapy modification
Colchicine: May enhance the myopathic (rhabdomyolysis) effect of HMG-CoA Reductase Inhibitors (Statins). Colchicine may increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Consider therapy modification
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CycloSPORINE (Systemic): May increase the serum concentration of AtorvaSTATin. Avoid combination
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Consider therapy modification
Cyproterone: May increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Management: Avoid use of statins metabolized by CYP3A4 (eg, simvastatin) and consider avoiding fluvastatin as well in patients receiving high dose cyproterone (300 mg/day). Consider use of pravastatin, rosuvastatin, or pitavastatin if statin therapy is needed. Consider therapy modification
Dabigatran Etexilate: AtorvaSTATin may decrease the serum concentration of Dabigatran Etexilate. Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Daclatasvir: May increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Danazol: May increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Management: Concurrent use of simvastatin with danazol is contraindicated. Do not exceed 20 mg per day of lovastatin if combined with danazol. Fluvastatin, pravastatin, and rosuvastatin may pose lower risk. Consider therapy modification
DAPTOmycin: HMG-CoA Reductase Inhibitors (Statins) may enhance the adverse/toxic effect of DAPTOmycin. Specifically, the risk of skeletal muscle toxicity may be increased. Management: Consider temporarily stopping HMG-CoA reductase inhibitor therapy prior to daptomycin. If used together, regular (i.e., at least weekly) monitoring of CPK concentrations is recommended. Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Digoxin: AtorvaSTATin may increase the serum concentration of Digoxin. Monitor therapy
DilTIAZem: AtorvaSTATin may increase the serum concentration of DilTIAZem. DilTIAZem may increase the serum concentration of AtorvaSTATin. Management: Consider using lower atorvastatin doses when used together with diltiazem. Consider therapy modification
Dronedarone: May increase the serum concentration of AtorvaSTATin. Monitor therapy
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Efavirenz: May decrease the serum concentration of AtorvaSTATin. Monitor therapy
Elbasvir: May increase the serum concentration of AtorvaSTATin. Management: Limit the dose of atorvastatin to a maximum of 20 mg/day when used together with elbasvir and grazoprevir. Monitor closely for evidence of statin-related toxicities such as myalgia or myopathy. Consider therapy modification
Eltrombopag: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. Monitor therapy
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Erythromycin (Systemic): May increase the serum concentration of AtorvaSTATin. Monitor therapy
Etravirine: May decrease the serum concentration of HMG-CoA Reductase Inhibitors (Statins). This applies to atorvastatin, lovastatin and simvastatin. Monitor therapy
Fenofibrate and Derivatives: May enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Fluconazole: May increase the serum concentration of AtorvaSTATin. Monitor therapy
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosphenytoin: May decrease the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Consider therapy modification
Fusidic Acid (Systemic): May enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Specifically, the risk for muscle toxicities, including rhabdomyolysis may be significantly increased. Management: Avoid concurrent use whenever possible. Use is listed as contraindicated in product characteristic summaries in several countries, although UK labeling suggests that use could be considered under exceptional circumstances and with close supervision. Avoid combination
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Gemfibrozil: May enhance the myopathic (rhabdomyolysis) effect of AtorvaSTATin. Gemfibrozil may increase the serum concentration of AtorvaSTATin. Avoid combination
Glecaprevir and Pibrentasvir: May increase the serum concentration of AtorvaSTATin. Avoid combination
Grapefruit Juice: May increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Management: Avoid concurrent use of GFJ with lovastatin or simvastatin. Avoid high quantities of GFJ with atorvastatin. Consider using a lower statin dose or a statin that is less likely to interact when possible. Consider therapy modification
Grazoprevir: May increase the serum concentration of AtorvaSTATin. Management: Limit the dose of atorvastatin to a maximum of 20 mg/day when used together with elbasvir and grazoprevir. Monitor closely for evidence of statin-related toxicities such as myalgia or myopathy. Consider therapy modification
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Istradefylline: May increase the serum concentration of AtorvaSTATin. Monitor therapy
Itraconazole: May increase the serum concentration of AtorvaSTATin. Management: Limit atorvastatin to a maximum adult dose of 20 mg/day in patients receiving itraconazole. Assess clinical response to ensure that the lowest necessary dose of atorvastatin is used. Consider use of fluva-, rosuva-, pitava-, or pravastatin when possible. Consider therapy modification
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Ketoconazole (Systemic): AtorvaSTATin may enhance the adverse/toxic effect of Ketoconazole (Systemic). Specifically, there is a theoretical potential for additive effects on reducing endogenous steroid concentrations. Ketoconazole (Systemic) may increase the serum concentration of AtorvaSTATin. Management: Administer ketoconazole with atorvastatin cautiously, and monitor for toxic effects of atorvastatin (e.g., myalgia, rhabdomyolysis, liver function test abnormalities). Consider use of fluva-, rosuva-, pitava-, or pravastatin when possible. Consider therapy modification
Lanthanum: HMG-CoA Reductase Inhibitors (Statins) may decrease the serum concentration of Lanthanum. Management: Administer HMG-CoA reductase inhibitors at least two hours before or after lanthanum. Consider therapy modification
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Ledipasvir: May enhance the adverse/toxic effect of AtorvaSTATin. Monitor therapy
Letermovir: May increase the serum concentration of AtorvaSTATin. Management: Limit the atorvastatin dose to 20 mg daily when combined with letermovir. When letermovir is coadministered with cyclosporine, the use of atorvastatin (at any dose) is not recommended. Consider therapy modification
Lomitapide: May increase the serum concentration of AtorvaSTATin. AtorvaSTATin may increase the serum concentration of Lomitapide. Management: When the lomitapide dose is 10 mg daily or greater, reduce the lomitapide dose by 50% when combined with atorvastatin. No dose adjustment is required when the lomitapide dose is 5 mg daily. Consider therapy modification
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Midazolam: AtorvaSTATin may increase the serum concentration of Midazolam. Monitor therapy
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Niacin: May enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Niacinamide: May enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Phenytoin: May decrease the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Consider therapy modification
Posaconazole: May increase the serum concentration of AtorvaSTATin. Avoid combination
Protease Inhibitors: May increase the serum concentration of AtorvaSTATin. Management: See full monograph for recommended dose limits. Avoid atorvastatin with tipranavir/ritonavir. Consider therapy modification
QuiNINE: May increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Raltegravir: May enhance the myopathic (rhabdomyolysis) effect of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Ranolazine: May increase the serum concentration of AtorvaSTATin. Monitor therapy
Red Yeast Rice: May enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Avoid combination
Repaglinide: HMG-CoA Reductase Inhibitors (Statins) may increase the serum concentration of Repaglinide. Monitor therapy
Rifamycin Derivatives: May decrease the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Management: Consider use of noninteracting antilipemic agents (note: pitavastatin concentrations may increase with rifamycin treatment). Monitor for altered HMG-CoA reductase inhibitor effects. Rifabutin and fluvastatin, or possibly pravastatin, may pose lower risk. Consider therapy modification
Rupatadine: May enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Specifically, the risk for increased CPK and/or other muscle toxicities may be increased. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of AtorvaSTATin. Management: The maximum atorvastatin dose should not exceed 40 mg/day with concurrent use of simeprevir, and use of the lowest necessary atorvastatin dose is recommended. Consider therapy modification
Spironolactone: AtorvaSTATin may enhance the adverse/toxic effect of Spironolactone. Specifically, there is a theoretical potential for enhanced effects on reducing endogenous steroid activity. Monitor therapy
St John's Wort: May increase the metabolism of HMG-CoA Reductase Inhibitors (Statins). Management: Consider avoiding the concomitant administration of St Johns Wort with interacting HMG-CoA reductase inhibitors in order to avoid the potential for decreased antilipemic effects. Monitor for decreased effects during concomitant therapy. Consider therapy modification
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Telithromycin: May increase the serum concentration of AtorvaSTATin. Management: Consider limiting atorvastatin to a max (adult) dose of 20 mg/day when used with telithromycin. Although not a specific recommendation in atorvastatin labeling, this is consistent with dosing for other strong CYP3A4 inhibitors, including clarithromycin. Consider therapy modification
Teriflunomide: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. Monitor therapy
Ticagrelor: May increase the serum concentration of AtorvaSTATin. Monitor therapy
Tipranavir: May increase the serum concentration of AtorvaSTATin. Avoid combination
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Tolvaptan: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. Consider therapy modification
Trabectedin: HMG-CoA Reductase Inhibitors (Statins) may enhance the myopathic (rhabdomyolysis) effect of Trabectedin. Monitor therapy
Velpatasvir: May increase the serum concentration of AtorvaSTATin. Monitor therapy
Verapamil: AtorvaSTATin may increase the serum concentration of Verapamil. Verapamil may increase the serum concentration of AtorvaSTATin. Management: Consider using lower atorvastatin doses when used together with verapamil. Consider therapy modification
Voriconazole: May increase the serum concentration of AtorvaSTATin. Management: Monitor for toxic effects of atorvastatin (e.g., myalgia, rhabdomyolysis, liver function test abnormalities) during concomitant treatment, and reduce atorvastatin dose when possible. Consider use of fluva-, rosuva-, pitava-, or pravastatin when possible. Consider therapy modification
Voxilaprevir: May increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Management: Use the lowest statin dose possible if combined with voxilaprevir and monitor patients for increased statin effects/toxicities. Avoid concomitant use of voxilaprevir with rosuvastatin or pitavastatin, and limit pravastatin doses to 40 mg daily. Consider therapy modification
Adverse Reactions
>10%:
Gastrointestinal: Diarrhea (7% to 14%)
Neuromuscular & skeletal: Arthralgia (9% to 12%)
Respiratory: Nasopharyngitis (13%)
1% to 10%:
Cardiovascular: Hemorrhagic stroke (2%)
Central nervous system: Insomnia (5%), malaise (<2%), nightmares (<2%)
Dermatologic: Urticaria (<2%)
Endocrine & metabolic: Diabetes mellitus (6%), hyperglycemia (<2%)
Gastrointestinal: Nausea (7%), dyspepsia (6%), abdominal distress (<2%), cholestasis (<2%), eructation (<2%), flatulence (<2%)
Genitourinary: Urinary tract infection (7% to 8%), urine abnormality (white blood cells positive in urine: <2%)
Hepatic: Increased serum transaminases (≤2%), abnormal hepatic function tests (<2%), hepatitis (<2%), increased serum alkaline phosphatase (<2%)
Neuromuscular & skeletal: Limb pain (9%), myalgia (4% to 8%), musculoskeletal pain (5%), muscle spasm (4% to 5%), increased creatine phosphokinase (<2%), joint swelling (<2%), muscle fatigue (<2%), neck pain (<2%)
Ophthalmic: Blurred vision (<2%)
Otic: Tinnitus (<2%)
Respiratory: Pharyngolaryngeal pain (3% to 4%), epistaxis (<2%)
Miscellaneous: Fever (<2%)
Frequency not defined: Central nervous system: Myasthenia
<1%, postmarketing, and/or case reports: Abdominal pain, alopecia, amnesia (reversible), anaphylaxis, anemia, angioedema, anorexia, back pain, bullous rash, chest pain, cognitive dysfunction (reversible), confusion (reversible), cystitis (interstitial; Huang 2015), depression, dizziness, dysgeusia, elevated glycosylated hemoglobin (HbA1c), erythema multiforme, fatigue, gynecomastia, hepatic failure, hypoesthesia, increased serum glucose, interstitial pulmonary disease, jaundice, memory impairment (reversible), myopathy, myositis, pancreatitis, paresthesia, peripheral edema, peripheral neuropathy, pruritus, rhabdomyolysis, rupture of tendon, Stevens-Johnson syndrome, thrombocytopenia, toxic epidermal necrolysis, vomiting, weight gain
Warnings/Precautions
Concerns related to adverse effects:
- Diabetes mellitus: Increases in HbA1c and fasting blood glucose have been reported.
- Hepatotoxicity: Persistent elevations in serum transaminases have been reported; upon dose reduction, drug interruption, or discontinuation, transaminase levels returned to or near pretreatment levels. Postmarketing reports of fatal and nonfatal hepatic failure have been reported and are rare. If serious hepatotoxicity with clinical symptoms and/or hyperbilirubinemia or jaundice occurs during treatment, interrupt therapy promptly. If an alternate etiology is not identified, do not restart atorvastatin. Liver enzyme tests should be obtained at baseline and as clinically indicated and if signs/symptoms of liver injury occur. Ethanol may enhance the potential of adverse hepatic effects; instruct patients to avoid excessive ethanol consumption.
- Myopathy/rhabdomyolysis: Rhabdomyolysis with acute renal failure secondary to myoglobinuria and/or myopathy has been reported; patients should be monitored closely. This risk is dose-related and is increased with concurrent use of strong CYP3A4 inhibitors; if concurrent use is warranted, consider lower starting and maintenance doses of atorvastatin. Use caution in patients with inadequately treated hypothyroidism, and those taking other drugs associated with myopathy (eg, colchicine); these patients are predisposed to myopathy. Immune-mediated necrotizing myopathy (IMNM) associated with HMG-CoA reductase inhibitors use has also been reported. Patients should be instructed to report unexplained muscle pain, tenderness, weakness, or brown urine, particularly if accompanied by malaise or fever. Discontinue therapy if markedly elevated CPK levels occur or myopathy is diagnosed/suspected.
Disease-related concerns:
- Hepatic impairment and/or ethanol use: Use with caution in patients who consume large amounts of ethanol or have a history of liver disease; use is contraindicated in patients with active liver disease or unexplained persistent elevations of serum transaminases.
- Renal impairment: Use with caution in patients with renal impairment; these patients are predisposed to myopathy.
- Stroke: Patients with recent stroke or TIA receiving long-term therapy with high-dose (ie, 80 mg/day) atorvastatin may be at increased risk for hemorrhagic stroke (SPARCL Investigators [Amarenco 2006]). A subsequent post-hoc analysis demonstrated that patients with lacunar or hemorrhagic stroke may be at higher risk of hemorrhagic stroke; however, this finding was determined to be hypothesis generating. The overall benefit of treatment with atorvastatin (ie, reduced risk of stroke and cardiovascular events) in this population seems to outweigh the increased risk of hemorrhagic stroke if one truly exists (Goldstein 2008).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Use with caution in patients with advanced age, these patients are predisposed to myopathy.
- Surgical patients: The manufacturer recommends temporary discontinuation for elective major surgery, acute medical or surgical conditions, or in any patient experiencing an acute, serious condition suggestive of a myopathy or having a risk factor predisposing to the development of renal failure secondary to rhabdomyolysis (eg, sepsis, hypotension, trauma, uncontrolled seizures, severe metabolic, endocrine, or electrolyte disorders). Based on current research and clinical guidelines, HMG-CoA reductase inhibitors should be continued in the perioperative period for noncardiac and cardiac surgery (ACC/AHA [Fleisher 2014]; ACC/AHA [Hillis 2011]). Perioperative discontinuation of statin therapy is associated with an increased risk of cardiac morbidity and mortality.
Dosage form specific issues:
- Polysorbate 80: Some dosage forms may contain polysorbate 80 (also known as Tweens). Hypersensitivity reactions, usually a delayed reaction, have been reported following exposure to pharmaceutical products containing polysorbate 80 in certain individuals (Isaksson 2002; Lucente 2000; Shelley 1995).
Other warnings/precautions:
- Appropriate use: Secondary causes of hyperlipidemia should be ruled out prior to therapy.
Monitoring Parameters
ACC/AHA Blood Cholesterol Guideline recommendations (ACC/AHA [Grundy 2019]; ACC/AHA [Stone 2014]):
Lipid panel (total cholesterol, HDL, LDL, triglycerides): Lipid profile (fasting or nonfasting) before initiating treatment. Fasting lipid profile should be rechecked 4 to 12 weeks after starting therapy and every 3 to 12 months thereafter. If 2 consecutive LDL levels are <40 mg/dL, consider decreasing the dose.
Hepatic transaminase levels: Baseline measurement of hepatic transaminase levels (AST and ALT); measure AST, ALT, total bilirubin, and alkaline phosphatase if symptoms suggest hepatotoxicity (eg, unusual fatigue or weakness, loss of appetite, abdominal pain, dark-colored urine or yellowing of skin or sclera) during therapy.
CPK: CPK should not be routinely measured. Baseline CPK measurement is reasonable for some individuals (eg, family history of statin intolerance or muscle disease, clinical presentation, concomitant drug therapy that may increase risk of myopathy). May measure CPK in any patient with symptoms suggestive of myopathy (pain, tenderness, stiffness, cramping, weakness, or generalized fatigue).
Evaluate for new-onset diabetes mellitus during therapy; if diabetes develops, continue statin therapy and encourage adherence to a heart-healthy diet, physical activity, a healthy body weight, and tobacco cessation.
If patient develops a confusional state or memory impairment, may evaluate patient for nonstatin causes (eg, exposure to other drugs), systemic and neuropsychiatric causes, and the possibility of adverse effects associated with statin therapy.
Pregnancy
Pregnancy Considerations
Atorvastatin is contraindicated in pregnant females or those who may become pregnant.
There are reports of congenital anomalies following maternal use of HMG-CoA reductase inhibitors in pregnancy; however, maternal disease, differences in specific agents used, and the low rates of exposure limit the interpretation of the available data (Godfrey 2012; Lecarpentier 2012). Cholesterol biosynthesis may be important in fetal development; serum cholesterol and triglycerides increase normally during pregnancy. The discontinuation of lipid-lowering medications temporarily during pregnancy is not expected to have significant impact on the long-term outcomes of primary hypercholesterolemia treatment.
Atorvastatin should be discontinued immediately if an unplanned pregnancy occurs during treatment.
Adequate contraception is recommended if an HMG-CoA reductase inhibitor is required in females of reproductive potential. Females planning a pregnancy should discontinue the HMG-CoA reductase inhibitor 1 to 2 months prior to attempting to conceive (AHA/ACC [Grundy 2019]).
Patient Education
What is this drug used for?
- It is used to lower bad cholesterol and raise good cholesterol (HDL).
- It is used to lower triglycerides.
- It is used in some people to lower the chance of heart attack, stroke, and certain heart procedures.
- It is used to slow the progress of heart disease.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Diarrhea
- Joint pain
- Nausea
- Trouble sleeping
- Stuffy nose
- Sore throat
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Urinary tract infection like blood in the urine, burning or painful urination, passing a lot of urine, fever, lower abdominal pain, or pelvic pain.
- Severe cerebrovascular disease like change in strength on one side is greater than the other, difficulty speaking or thinking, change in balance, or vision changes.
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Unable to pass urine
- Change in amount of urine passed
- Severe loss of strength and energy
- Confusion
- Memory problems or loss
- Severe muscle pain
- Severe muscle tenderness
- Severe muscle weakness
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.