Boxed Warning
Accidental exposure (buccal film, transdermal patch):
Accidental exposure to even one dose of buprenorphine, especially by children, can result in a fatal overdose of buprenorphine.
Addiction, abuse, and misuse (buccal film, immediate-release injection, transdermal patch):
Buprenorphine exposes patients and other users to the risks of opioid addiction, abuse, and misuse, which can lead to overdose and death. Assess each patient's risk prior to prescribing buprenorphine and monitor all patients regularly for the development of these behaviors or conditions.
Opioid analgesic risk evaluation and mitigation strategy (REMS):
To ensure that the benefits of opioid analgesics outweigh the risks of addiction, abuse, and misuse, the FDA has required a REMS for these products. Under the requirements of the REMS, drug companies with approved opioid analgesic products must make REMS-compliant education programs available to health care providers. Health care providers are strongly encouraged to complete a REMS-compliant education program and counsel patients and/or their caregivers, with every prescription, on safe use, serious risks, storage, and disposal of these products; emphasize to patients and their caregivers the importance of reading the Medication Guide every time it is provided by their pharmacist, and consider other tools to improve patient, household, and community safety.
Life-threatening respiratory depression (buccal film, immediate-release injection, transdermal patch):
Serious, life-threatening, or fatal respiratory depression may occur with use of buprenorphine. Monitor for respiratory depression, especially during initiation of buprenorphine or following a dose increase. Misuse or abuse of buprenorphine by chewing, swallowing, snorting, or injecting buprenorphine extracted from the buccal film or transdermal system will result in the uncontrolled delivery of buprenorphine and pose a significant risk of overdose and death.
Neonatal opioid withdrawal syndrome (buccal film, immediate-release injection, transdermal patch):
Prolonged use of buprenorphine during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated, and requires management according to protocols developed by neonatology experts. If opioid use is required for a prolonged period in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available.
Risk associated with insertion and removal (subdermal implant):
Insertion and removal of buprenorphine implant are associated with the risk of implant migration, protrusion, and expulsion resulting from the procedure. Rare but serious complications including nerve damage and migration resulting in embolism and death may result from improper insertion of drug implants inserted in the upper arm. Additional complications may include local migration, protrusion, and expulsion. Incomplete insertions or infections may lead to protrusion or expulsion.
Because of the risks associated with insertion and removal, buprenorphine implant is available only through a restricted program called the Probuphine REMS Program. All healthcare providers must successfully complete a live training program on the insertion and removal procedures and become certified, prior to performing insertions or prescribing buprenorphine implants. Patients must be monitored to ensure that the implant is removed by a healthcare provider certified to perform insertions.
Risks from concomitant use with benzodiazepines or other CNS depressants (buccal film, immediate-release injection, transdermal patch):
Concomitant use of opioids with benzodiazepines or other CNS depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing of buprenorphine and benzodiazepines or other CNS depressants for use in patients for whom alternative treatment options are inadequate. Limit dosages and durations to the minimum required. Follow patients for signs and symptoms of respiratory depression and sedation.
Risk of serious harm or death with intravenous administration (extended-release injection):
Serious harm or death could result if extended-release injection is administered intravenously. The injection forms a solid mass upon contact with body fluids and may cause occlusion, local tissue damage, and thromboembolic events, including life-threatening pulmonary emboli if administered intravenously.
Because of the risk of serious harm or death that could result from intravenous self-administration, buprenorphine extended-release injection is only available through a restricted program called the Sublocade REMS Program. Healthcare settings and pharmacies that order and dispense buprenorphine extended-release injection must be certified in this program and comply with the REMS requirements.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Film, Buccal:
Belbuca: 75 mcg (1 ea, 60 ea); 150 mcg (1 ea, 60 ea); 300 mcg (1 ea, 60 ea); 450 mcg (1 ea, 60 ea); 600 mcg (1 ea, 60 ea); 750 mcg (1 ea, 60 ea); 900 mcg (1 ea, 60 ea) [contains methylparaben, propylparaben, saccharin sodium, sodium benzoate; peppermint flavor]
Implant, Subcutaneous:
Probuphine Implant Kit: 74.2 mg (4 ea)
Patch Weekly, Transdermal:
Butrans: 5 mcg/hr (4 ea); 7.5 mcg/hr (4 ea); 10 mcg/hr (4 ea); 15 mcg/hr (4 ea); 20 mcg/hr (4 ea)
Generic: 5 mcg/hr (1 ea, 4 ea); 7.5 mcg/hr (4 ea); 10 mcg/hr (1 ea, 4 ea); 15 mcg/hr (1 ea, 4 ea); 20 mcg/hr (1 ea, 4 ea)
Solution, Injection:
Buprenex: 0.3 mg/mL (1 mL)
Generic: 0.3 mg/mL (1 mL)
Solution, Injection [preservative free]:
Generic: 0.3 mg/mL (1 mL)
Solution Prefilled Syringe, Subcutaneous [preservative free]:
Sublocade: 100 mg/0.5 mL (0.5 mL); 300 mg/1.5 mL (1.5 mL)
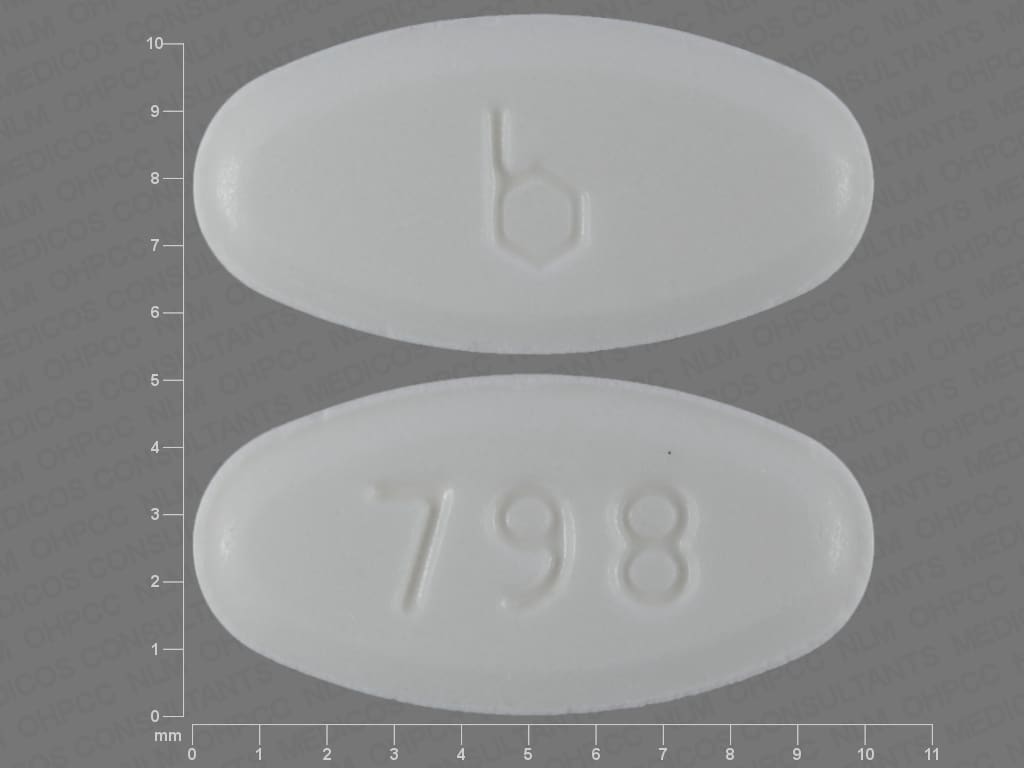
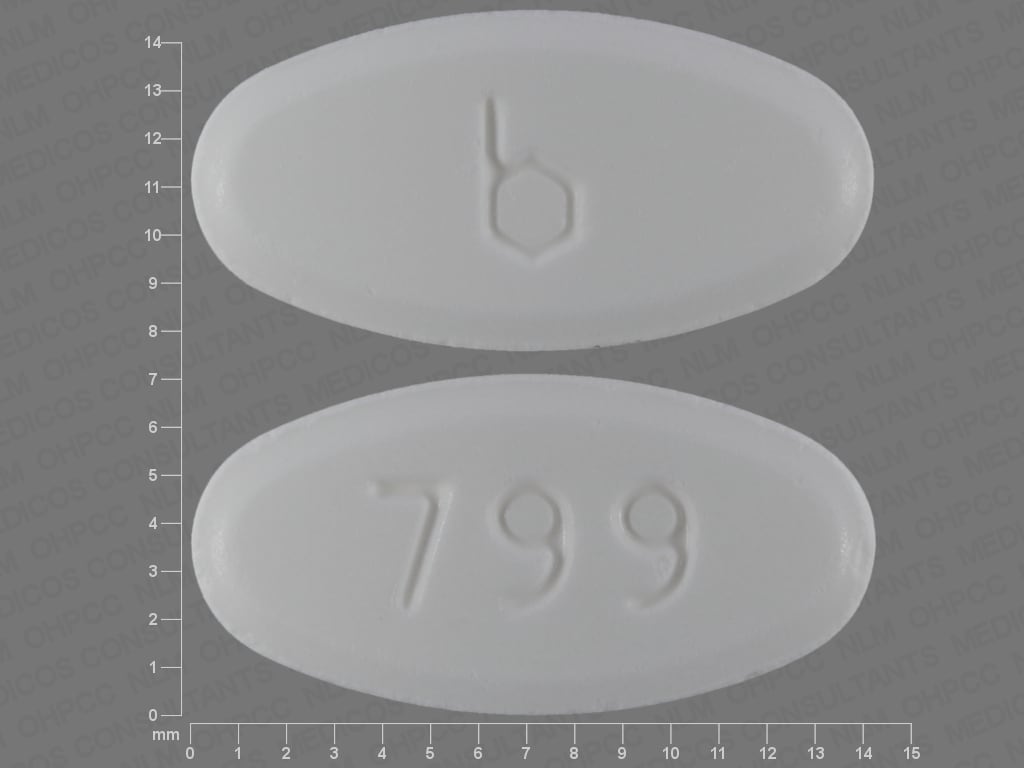
Tablet Sublingual, Sublingual:
Generic: 2 mg, 8 mg
Pharmacology
Mechanism of Action
Buprenorphine exerts its analgesic effect via high-affinity binding to mu opiate receptors in the CNS; displays partial mu agonist and weak kappa antagonist activity. Due to it being a partial mu agonist, its analgesic effects plateau at higher doses and it then behaves like an antagonist. The extended-release formulation is injected subcutaneously as a liquid; subsequent precipitation following injection results in a solid depot which will gradually release buprenorphine via diffusion and biodegradation of the depot.
Pharmacokinetics/Pharmacodynamics
Absorption
Immediate-release IM and SubQ: 30% to 40%. Application of a heating pad onto the transdermal system may increase blood concentrations of buprenorphine 26% to 55%. Ingestion of liquids decreases systemic exposure to buprenorphine from buccal film by 23% to 37%.
Distribution
CSF concentrations are ~15% to 25% of plasma concentrations
Vd:
Premature neonates (GA: 27 to 32 weeks): 6.2 ± 2.1 L/kg (Barrett 1993)
Children 4 to 7 years: 3.2 ± 2 L/kg (Olkkola 1989)
Adults: 97 to 187 L/kg
Metabolism
Primarily hepatic via N-dealkylation by CYP3A4 to norbuprenorphine (active metabolite), and to a lesser extent via glucuronidation by UGT1A1 and 2B7 to buprenorphine 3-O-glucuronide; the major metabolite, norbuprenorphine, also undergoes glucuronidation via UGT1A3; extensive first-pass effect
Excretion
Feces (~70%; 33% as unchanged drug; 5% as conjugated drug; 21% as norbuprenorphine; and 2% as conjugated norbuprenorphine); urine (27% to 30%; 1% as unchanged drug; 9.4% as conjugated drug; 2.7% as norbuprenorphine; and 11% as conjugated norbuprenorphine)
Clearance: Related to hepatic blood flow
Premature neonates (GA: 27 to 32 weeks): 0.23 ± 0.07 L/hour/kg (Barrett 1993)
Children 4 to 7 years: 3.6 ± 1.1 L/hour/kg (Olkkola 1989)
Adults: 0.78 to 1.32 L/hour/kg
Onset of Action
Analgesic: Immediate-release IM: ≥15 minutes; Peak effect: Immediate-release IM: ~1 hour
Time to Peak
Plasma: Buccal film: 2.5 to 3 hours; Extended-release SubQ: 24 hours, with steady state achieved after 4 to 6 months; Subdermal implant: 12 hours after insertion, with steady state achieved by week 4; Sublingual: 30 minutes to 1 hour (Kuhlman 1996); Transdermal patch: Steady state achieved by day 3
Duration of Action
Immediate-release IM: ≥6 hours; Extended-release SubQ: 28 days
Half-Life Elimination
Premature neonates (GA: 27 to 32 weeks): Immediate-release IV: 20 ± 8 hours (Barrett 1993)
Children 4 to 7 years: Immediate-release IV: ~1 hour (Olkkola 1989)
Adults: Immediate-release IV: 2.2 to 3 hours; Buccal film: 27.6 ± 11.2 hours; Apparent terminal half-life: Sublingual tablet: ~37 hours; Transdermal patch: ~26 hours. Note: Extended elimination half-life for sublingual administration may be due to depot effect (Kuhlman 1996)
Protein Binding
High (~96%, primarily to alpha- and beta globulin)
Use in Specific Populations
Special Populations: Hepatic Function Impairment
Because buprenorphine is extensively metabolized, plasma levels and half-life were increased in patients with moderate and severe hepatic impairment.
Special Populations: Elderly
The pharmacokinetics are similar between younger adults and elderly, although elderly patients showed a trend toward higher plasma concentrations immediately after transdermal system removal.
Use: Labeled Indications
Opioid dependence:
Extended-release injection: Treatment of moderate to severe opioid use disorder in patients who have initiated treatment with 8 to 24 mg of a transmucosal buprenorphine-containing product, followed by dose adjustment for a minimum of 7 days.
Subdermal implant: Maintenance treatment of opioid dependence in patients who have achieved and sustained prolonged clinical stability on low to moderate doses (≤8 mg/day) of a transmucosal buprenorphine-containing product for 3 months or longer with no need for supplemental dosing or adjustments
Sublingual tablet: Treatment of opioid dependence
Limitations of use: Buprenorphine should be used as part of a complete treatment program to include counseling and psychosocial support.
Pain management:
Buccal film, transdermal patch: Management of pain severe enough to require around-the-clock, long-term opioid treatment and for which alternative treatment options are inadequate
Immediate-release injection: Management of pain severe enough to require an opioid analgesic and for which treatments are inadequate
Limitations of use: Reserve buprenorphine for use in patients for whom alternative treatment options (eg, nonopioid analgesics, opioid combination products, immediate-release opioids) are ineffective, not tolerated, or would be otherwise inadequate to provide sufficient management of pain. Buprenorphine buccal film and transdermal patch are not indicated as an as needed analgesic.
Use: Off Label
Opioid withdrawal in heroin-dependent hospitalized patients (immediate-release injection)c
Data from a limited number of patients studied who received buprenorphine parenterally for opioid withdrawal during hospitalization for an acute medical problem suggests that buprenorphine is safe when used in this setting Umbricht 2003, Welsh 2002. In a systematic review of trials evaluating the use of buprenorphine for managing opioid withdrawal, the use of buprenorphine was shown to be more effective than clonidine or lofexidine (not available in the US) and equally effective to methadone (limited data) Gowing 2017. Additional data may be necessary to further define the role of buprenorphine in the management of patients with opioid withdrawal while being hospitalized for an acute medical problem.
Perineural anesthesiac
In a metaanalysis of trials evaluating the use of buprenorphine in peripheral nerve blocks, the use of buprenorphine in this manner was shown to be safe and effective Schnabel 2017. Buprenorphine prolongs the duration of postoperative analgesia and may reduce opioid consumption when administered as a nerve block Bailard 2014, Kosel 2015, Krishnan 2016; Additional data may be necessary to further define the role of buprenorphine in the management of postoperative pain as a perineural adjunct.
Contraindications
Hypersensitivity (eg, anaphylaxis) to buprenorphine or any component of the formulation
Buccal film, immediate-release injection, transdermal patch: Additional contraindications: Significant respiratory depression; acute or severe asthma in an unmonitored setting or in the absence of resuscitative equipment; GI obstruction, including paralytic ileus (known or suspected)
Documentation of allergenic cross-reactivity for opioids is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Canadian labeling: Additional contraindications (not in US labeling): Acute respiratory depression; hypercapnia; cor pulmonale; acute alcoholism or alcohol dependence; delirium tremens; convulsive disorders; severe CNS depression; increased cerebrospinal or intracranial pressure; head injury; severe hepatic insufficiency
Buccal film, transdermal patch: Additional contraindications: Hypersensitivity to other opioids; suspected surgical abdomen (eg, acute appendicitis or pancreatitis); mild, intermittent or short duration pain that can otherwise be managed; management of acute pain, including use in outpatient or day surgeries; management of perioperative pain relief, or in other situations characterized by rapidly varying analgesic requirements; obstructive airway (other than asthma); status asthmaticus; concurrent use or use within 14 days of MAOIs; myasthenia gravis; opioid-dependent patients and for opioid withdrawal treatment; pregnancy or during labor and delivery; breastfeeding; known or suspected oral mucositis (buccal film only)
Subdermal implant: Additional contraindications: Severe respiratory insufficiency, opioid-naive patients, known or suspected GI obstruction or any condition affecting bowel transit, congenital long QT prolongation or QTc prolongation at baseline, uncorrected hypokalemia, hypomagnesemia, hypocalcemia
Dosage and Administration
Dosing: Adult
Note: Buprenorphine 8 mg sublingual tablet = buprenorphine/naloxone 8 mg/2 mg sublingual film = buprenorphine/naloxone 4.2 mg/0.7 mg buccal film = buprenorphine/naloxone 5.7 mg/1.4 mg sublingual tablet.
Acute pain (moderate to severe): Note: Long-term use is not recommended. The following recommendations are guidelines and do not represent the maximum doses that may be required in all patients. Doses should be titrated to pain relief/prevention.
Immediate-release injection:
IM: Initial: 0.3 mg every 6 to 8 hours as needed; initial dose (up to 0.3 mg) may be repeated once in 30 to 60 minutes after the initial dose if needed
Slow IV: Initial: 0.3 mg every 6 to 8 hours as needed; initial dose (up to 0.3 mg) may be repeated once in 30 to 60 minutes after the initial dose if needed
Chronic pain (moderate to severe):
Buccal film: Note: Buprenorphine buccal film doses of 600, 750, and 900 mcg are only for use following titration from lower doses (maximum dose: 900 mcg every 12 hours).
Opioid-naive patients and opioid-non-tolerant patients: Initial: 75 mcg once daily or, if tolerated, every 12 hours for at least 4 days, then increase to 150 mcg every 12 hours.
Opioid-experienced patients (conversion from other opioids to buprenorphine): Discontinue all other around-the-clock opioids when buprenorphine is initiated. Taper patient's current opioid to no more than 30 mg oral morphine sulfate equivalents daily before initiating buprenorphine. Following analgesic taper, base the initial buprenorphine dose on the patient's daily opioid dose prior to taper. Patients may require additional short-acting analgesics during the taper period.
Patients who were receiving daily dose of <30 mg of oral morphine equivalents: Initial: 75 mcg once daily or every 12 hours
Patients who were receiving daily dose of 30 to 89 mg of oral morphine equivalents: Initial: 150 mcg every 12 hours
Patients who were receiving daily dose of 90 to 160 mg of oral morphine equivalents: Initial: 300 mcg every 12 hours
Patients who were receiving daily dose of >160 mg of oral morphine equivalents: Buprenorphine buccal film may not provide adequate analgesia; consider the use of an alternate analgesic.
Conversion from methadone: Close monitoring is required when converting methadone to another opioid. Ratio between methadone and other opioid agonists varies widely according to previous dose exposure. Methadone has a long half-life and can accumulate in the plasma.
Dose titration (opioid-naive or opioid-experienced patients): Individually titrate in increments of 150 mcg every 12 hours, no more frequently than every 4 days, to a dose that provides adequate analgesia and minimizes adverse reactions (maximum dose: 900 mcg every 12 hours; doses up to 450 mcg every 12 hours were studied in opioid naive patients). Patients may require additional short-acting analgesics during titration.
Discontinuation of therapy: When discontinuing buccal film, use a gradual downward titration, such as decreasing the dose by no more than 10% to 25% in a physically dependent patient and continue downward titration every 2 to 4 weeks. If patient displays withdrawal symptoms, temporarily interrupt the taper or increase dose to previous level and then reduce dose more slowly by increasing interval between dose reductions, decreasing amount of daily dose reduction, or both.
Patients with oral mucositis: Reduce the starting dose and titration incremental dose by 50%.
Transdermal patch:
Opioid-naive patients: Initial: 5 mcg/hour applied once every 7 days
Opioid-experienced patients (conversion from other opioids to buprenorphine): Discontinue all other around-the-clock opioid drugs when buprenorphine therapy is initiated. Short-acting analgesics as needed may be continued until analgesia with transdermal buprenorphine is attained. There is a potential for buprenorphine to precipitate withdrawal in patients already receiving opioids.
Patients who were receiving daily dose of <30 mg of oral morphine equivalents: Initial: 5 mcg/hour applied once every 7 days
Patients who were receiving daily dose of 30 to 80 mg of oral morphine equivalents: Taper the current around-the-clock opioid for up to 7 days to ≤30 mg/day of oral morphine or equivalent before initiating therapy. Initial: 10 mcg/hour applied once every 7 days
Patients who were receiving daily dose of >80 mg of oral morphine equivalents: Buprenorphine transdermal patch, even at the maximum dose of 20 mcg/hour applied once every 7 days, may not provide adequate analgesia; consider the use of an alternate analgesic.
Dose titration (opioid-naive or opioid-experienced patients): May increase dose in 5 mcg/hour, 7.5 mcg/hour, or 10 mcg/hour increments (using no more than two patches), based on patient's supplemental short-acting analgesic requirements, with a minimum titration interval of 72 hours (maximum dose: 20 mcg/hour applied once every 7 days; risk for QTc prolongation increases with doses >20 mcg/hour patch).
Discontinuation of therapy: When discontinuing transdermal patch, use a gradual downward titration, such as decreasing the dose by no more than 10% to 25% in a physically dependent patient and continue downward titration every 2 to 4 weeks. If patient displays withdrawal symptoms, temporarily interrupt the taper or increase dose to previous level and then reduce dose more slowly by increasing interval between dose reductions, decreasing amount of daily dose reduction, or both.
Opioid withdrawal in heroin-dependent hospitalized patients (off-label use): Immediate-release injection: IV infusion: 0.3 to 0.9 mg (diluted in 50 to 100 mL of NS) over 20 to 30 minutes every 6 to 12 hours (Welsh 2002)
Opioid dependence:
Extended-release injection: SubQ: Initial: 300 mg monthly for the first 2 months, after treatment has been inducted and adjusted with 8 to 24 mg of a transmucosal buprenorphine-containing product for a minimum of 7 days. Maintenance: 100 mg monthly, increasing to 300 mg monthly for patients who tolerate the 100 mg dose but do not demonstrate a satisfactory clinical response (as evidenced by self-reported illicit opioid use or urine drug screens positive for illicit opioid use). Note: Administer doses at least 26 days apart.
Subdermal implant: Insert 4 implants subdermally in the inner side of the upper arm. Remove no later than 6 months after the date of insertion; if continued treatment is desired, insert 4 new implants subdermally in the inner side of the contralateral arm. After one insertion in each arm, discontinue treatment with subdermal implants.
Converting back to sublingual tablet: On day of implant removal, resume buprenorphine treatment at previous sublingual dose.
Sublingual tablet: Note: The combination product, buprenorphine and naloxone, is preferred therapy over buprenorphine monotherapy for induction treatment (and stabilization/maintenance treatment) for short-acting opioid dependence (US Department of Health and Human Services 2005).
Induction: 2 to 4 mg; if no signs of precipitated withdrawal after 60 to 90 minutes, may increase in increments of 2 to 4 mg. Once initial dose is tolerated, may increase to a dose that is clinically effective and provides 24 hours of stabilization. Buprenorphine treatment initiation should begin after mild to moderate opioid withdrawal signs appear (to avoid precipitated withdrawal), which is generally at least 6 to 12 hours after last use of short-acting opioids (eg, heroin, oxycodone) and 24 to 72 hours after last use of long-acting opioids (methadone) (Kampman [ASAM 2015]).
After induction and titration, daily dose usually ≥8 mg/day. In patients continuing to use opioids, consider increasing the dose by 4 to 8 mg to a daily dose of ≥12 to 16 mg/day (Kampman [ASAM 2015]).
Manufacturer's labeling: Dosing in the prescribing information may not reflect current clinical practice.
Induction: Day 1: 8 mg; Day 2 and subsequent induction days: Induction usually accomplished over 3 to 4 days. Dosing on the first day may be given in 2 to 4 mg increments.
Maintenance: Target dose: 16 mg/day; doses higher than 24 mg/day have not been demonstrated to provide any clinical advantage.
Perineural anesthesia (off-label use): Immediate-release perineural injection: 200 to 300 mcg added to local anesthetic (eg, bupivacaine, mepivacaine, tetracaine) with or without epinephrine and administered as a single injection (Kosel 2015; Krishnan 2016).
Dosing: Geriatric
Acute pain (moderate to severe): Immediate-release injection: IM, slow IV: Refer to adult dosing; use with caution.
Chronic pain (moderate to severe): Buccal film, transdermal patch: No specific dosage adjustments required; use caution and titrate slowly due to potential for increased risk of adverse events.
Opioid dependence: Extended-release injection, subdermal implant: No specific dosage adjustments required; use caution due to potential for increased risk of adverse events and inability to adjust dosage.
Dosing: Pediatric
Acute pain (moderate to severe): Dose should be titrated to appropriate effect. The following recommendations are guidelines and do not represent the maximum doses that may be required in all patients.
Children 2 to 12 years: IM, slow IV injection: Initial: Opioid-naive: 2 to 6 mcg/kg/dose every 4 to 6 hours (APS 2016); Note: Not all children have faster clearance rates than adults; some children may require dosing intervals of every 6 to 8 hours; observe clinical effects to establish the proper dosing interval.
Adolescents: IM, slow IV injection: Initial: Opioid-naive: 0.3 mg every 6 to 8 hours as needed; initial dose may be repeated once in 30 to 60 minutes if clinically needed
Chronic pain (moderate to severe): Adolescents ≥18 years: Transdermal patch:
Opioid-naive patients: Initial: 5 mcg/hour applied once every 7 days
Opioid-experienced patients (conversion from other opioids to buprenorphine patch): Discontinue all other around-the-clock opioid drugs when buprenorphine therapy is initiated. Short-acting analgesics as needed may be continued until analgesia with transdermal buprenorphine is attained. There is a potential for buprenorphine to precipitate withdrawal in patients already receiving opioids.
Patients who were receiving daily dose of <30 mg of oral morphine equivalents: Initial: 5 mcg/hour applied once every 7 days
Patients who were receiving daily dose of 30 to 80 mg of oral morphine equivalents: Taper the current around-the-clock opioid for up to 7 days to ≤30 mg/day of oral morphine or equivalent before initiating therapy. Initial: 10 mcg/hour applied once every 7 days.
Patients who were receiving daily dose of >80 mg of oral morphine equivalents: Buprenorphine transdermal patch, even at the maximum dose of 20 mcg/hour applied once every 7 days, may not provide adequate analgesia; consider the use of an alternate analgesic.
Dose titration (opioid-naive or opioid-experienced patients): May increase dose in 5 mcg/hour, 7.5 mcg/hour, or 10 mcg/hour increments (using no more than two 5 mcg/hour patches); titrate no more frequently than every 72 hours; maximum dose: 20 mcg/hour applied once every 7 days due to risk of QTc prolongation associated with higher doses.
Discontinuation of therapy: Taper dose gradually every 7 days to prevent withdrawal in the physically dependent patient; consider initiating immediate-release opioids, if needed for signs and symptoms of withdrawal.
Opioid dependence: Note: Do not start induction with buprenorphine until objective and clear signs of withdrawal are apparent (otherwise withdrawal may be precipitated).
Sublingual tablet: Note: The combination product, buprenorphine and naloxone, is preferred therapy over buprenorphine monotherapy for induction treatment (and stabilization/maintenance treatment) for short-acting opioid dependence (US Department of Health and Human Services 2005)
American Society of Addiction Medicine Guidelines (Kampman [ASAM 2015]): Limited data available: Adolescents: Sublingual tablet:
Note: Buprenorphine treatment initiation should begin after mild to moderate opioid withdrawal signs appear (to avoid precipitated withdrawal), which is generally at least 6 to 12 hours after last use of short-acting opioids (eg, heroin, oxycodone) and 24 to 72 hours after last use of long-acting opioids (methadone).
Induction: Initial: 2 to 4 mg; if no signs of precipitated withdrawal after 60 to 90 minutes, may increase in increments of 2 to 4 mg. Once initial dose is tolerated, may increase to a dose that is clinically effective and provides 24 hours of stabilization.
After induction and titration, daily dose usually ≥8 mg/day are necessary. In patients continuing to use opioids, consider increasing the dose by 4 to 8 mg to a daily dose of ≥12 to 16 mg/day. Maximum daily dose 24 mg/day.
Manufacturer's labeling: Adolescents ≥16 years:
Induction: Day 1: 8 mg/day divided in 2 to 4 mg increments; day 2 and subsequent induction days dose dependent upon patient response. In 1 study, patients received 8 mg on day 1, followed by 16 mg on day 2; induction usually accomplished over 3 to 4 days. Treatment should begin only when objective and clear signs of moderate opioid withdrawal appear, and not less than 4 hours after last use of heroin or other short-acting opioids or not less than 24 hours after last use of methadone or other long-acting opioids. Titrating dose to clinical effectiveness should be done as rapidly as possible to prevent undue withdrawal symptoms and patient drop-out during the induction period.
Maintenance: Target dose: 16 mg/day; reported range: 4 to 24 mg/day; doses higher than 24 mg/day have not been demonstrated to provide any clinical advantage; patients should be switched to the buprenorphine/naloxone combination product for maintenance and unsupervised therapy
Subdermal implant: Adolescents ≥16 years: Insert 4 implants subdermally in the inner side of the upper arm. Remove no later than 6 months after the date of insertion; if continued treatment is desired, insert 4 new implants subdermally in the inner side of the contralateral arm. After 1 insertion in each arm, discontinue treatment with subdermal implants.
To convert back to sublingual tablet: On day of implant removal, resume buprenorphine treatment at previous sublingual dose
Reconstitution
Extended-release injection: Use only the syringe and safety needle included with product. Remove product from refrigerator and bring to room temperature over at least 15 minutes. Do not open the foil pouch or attach the needle until immediately prior to injection.
Extemporaneously Prepared
A 0.075 mg/mL solution can be made using the 0.3 mg/mL injection, 95% ethanol, and simple syrup. Add 1.26 mL of 95% ethanol to 0.3 mg buprenorphine obtained from an 0.3 mg/1 mL ampule, mix well, and add quantity of simple syrup sufficient to obtain 4 mL (final volume). Solution is stable under refrigeration and at room temperature for 30 days when stored in amber glass bottles and for 7 days when stored in oral syringes (Anagnostis 2011; Anagnostis 2013).
Anagnostis EA, Sadaka RE, Sailor LA, et al, "Formulation of Buprenorphine for Sublingual Use in Neonates," J Pediatr Pharmacol Ther, 2011, 16(4):281-4.22768012Anagnostis EA, personal communication, March 2013.
Administration
IM: Administer immediate-release injection via deep IM injection.
IV: Administer immediate-release injection slowly, over at least 2 minutes. Administration over 20 to 30 minutes preferred when managing opioid withdrawal in heroin-dependent hospitalized patients (Welsh 2002).
Oral:
Buccal film: Prior to placing the film, moisten inside of cheek with tongue or water. Apply film with a dry finger immediately after removing it from packaging. Place yellow side of film against the inside of the moistened cheek; press and hold the film in place for 5 seconds with finger (film should stay in place after this period). Keep film in place until it dissolves completely (usually within 30 minutes of application). Do not chew, swallow, touch, or move film after placement. Avoid eating or drinking until film dissolves. Do not cut or tear the film. Avoid application to areas of the mouth with any open sores or lesions. To dispose of film; remove foil overwrap from any unused, unneeded films and dispose by flushing down the toilet.
Sublingual tablet: Tablet should be placed under the tongue until dissolved; should not be chewed or swallowed (swallowing tablets before dissolved reduces bioavailability). If two or more tablets are needed per dose, all may be placed under the tongue at once, or two at a time. To ensure consistent bioavailability, subsequent doses should always be taken the same way.
Subcutaneous injection: Administer extended-release injection as an abdominal subcutaneous injection only, using only the syringe and safety needle included with product. Do not administer IV or IM. Inject between the transpyloric and transtubercular planes in an area with adequate subcutaneous tissue that is free of skin conditions (eg, nodules, lesions, excessive pigment.) Rotate the injection site between injections. Subsequent precipitation following injection results in a solid depot which will gradually release buprenorphine. The patient may have a lump for several weeks that will decrease over time; advise not to rub or massage the injection site. In the event the depot from an extended-release injection must be removed, it can be surgically excised under local anesthesia within 14 days of injection. See prescribing information for details. For insertion by health care providers trained in the injection technique and certified through the REMS program.
Subdermal implant: For insertion under local anesthesia by health care providers trained in the insertion and removal procedure through the REMS program. See prescribing information for details.
Transdermal patch: Apply patch to intact, nonirritated skin only. Apply to a hairless or nearly hairless skin site. If hairless site is not available, do not shave skin; hair at application site should be clipped. Prior to application, if the site must be cleaned, clean with clear water and allow to dry completely; do not use soaps, alcohol, oils, lotions, or abrasives due to potential for increased skin absorption. Do not use any patch that has been damaged, cut or manipulated in any way. Remove patch from protective pouch immediately before application. Remove the protective backing, and apply the sticky side of the patch to one of eight possible application sites (upper outer arm, upper chest, upper back or the side of the chest [each site on either side of the body]). Up to 2 patches may be applied at the same time adjacent to one another at the same application site. Firmly press patch in place and hold for ~15 seconds. Change patch every 7 days. Rotate patch application sites whenever a patch is replaced or added; wait ≥21 days before reapplying another patch to the same skin site. Avoid exposing application site to external heat sources (eg, heating pad, electric blanket, heat lamp, hot tub). Incidental exposure to water while bathing or showering is acceptable based on experience during clinical studies. If there is difficulty with patch adhesion, the edges of the system may be taped in place with first-aid tape. If ineffective, the system may be covered with waterproof or semipermeable adhesive dressings suitable for 7 days of wear. If the patch falls off during the 7-day dosing interval, dispose of the patch and apply a new patch to a different skin site. Dispose of patches using the Patch-Disposal Unit or by folding the adhesive sides of the patch together and then flushing down the toilet. In Canada, disposal via a pharmacy take back program is recommended; trash disposal is not advised.
Storage
Extended-release injection: Store refrigerated at 2°C to 8°C (36°F to 46°F). Discard if left at room temperature (15°C to 30°C [59°F to 86°F]) for more than 7 days.
Immediate-release injection: Store at 20°C to 25°C (68°F to 77°F); excursions permitted between 15°C to 30°C (59°F to 86°F). Protect from prolonged exposure to light.
Buccal film, transdermal patch, sublingual tablet: Store at 25°C (77°F); excursions permitted between 15°C to 30°C (59°F to 86°F).
Subdermal implant: Store at 20°C to 25°C (68°F to 77°F); excursions permitted between 15°C to 30°C (59°F to 86°F).
Buprenorphine Images
Drug Interactions
Alcohol (Ethyl): May enhance the CNS depressant effect of Buprenorphine. Management: Advise patients receiving buprenorphine about the increased risk of CNS depression if they consume alcohol. Consider alternatives to buprenorphine for opioid addiction treatment in patients who are dependent on alcohol. Consider therapy modification
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Alvimopan: Opioid Agonists may enhance the adverse/toxic effect of Alvimopan. This is most notable for patients receiving long-term (i.e., more than 7 days) opiates prior to alvimopan initiation. Management: Alvimopan is contraindicated in patients receiving therapeutic doses of opioids for more than 7 consecutive days immediately prior to alvimopan initiation. Consider therapy modification
Amphetamines: May enhance the analgesic effect of Opioid Agonists. Monitor therapy
Anticholinergic Agents: May enhance the adverse/toxic effect of Opioid Agonists. Specifically, the risk for constipation and urinary retention may be increased with this combination. Monitor therapy
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Atazanavir: Buprenorphine may decrease the serum concentration of Atazanavir. Atazanavir may increase the serum concentration of Buprenorphine. Management: Avoid this combination in patients un-boosted atazanavir due to possible decreased atazanavir concentrations. This combination is not contraindicated in patients also receiving ritonavir, but monitoring for buprenorphine toxicity is recommended. Avoid combination
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CNS Depressants: May enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
Cobicistat: May increase the serum concentration of Buprenorphine. Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of Buprenorphine. Monitor therapy
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Buprenorphine. Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Daclatasvir: May increase the serum concentration of Buprenorphine. Monitor therapy
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Desmopressin: Opioid Agonists may enhance the adverse/toxic effect of Desmopressin. Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Diuretics: Opioid Agonists may enhance the adverse/toxic effect of Diuretics. Opioid Agonists may diminish the therapeutic effect of Diuretics. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Efavirenz: May decrease serum concentrations of the active metabolite(s) of Buprenorphine. Efavirenz may decrease the serum concentration of Buprenorphine. Monitor therapy
Eluxadoline: Opioid Agonists may enhance the constipating effect of Eluxadoline. Avoid combination
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Etravirine: May decrease the serum concentration of Buprenorphine. Monitor therapy
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Gastrointestinal Agents (Prokinetic): Opioid Agonists may diminish the therapeutic effect of Gastrointestinal Agents (Prokinetic). Monitor therapy
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Monoamine Oxidase Inhibitors: Buprenorphine may enhance the adverse/toxic effect of Monoamine Oxidase Inhibitors. Avoid combination
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Nalmefene: May diminish the therapeutic effect of Opioid Agonists. Management: Avoid the concomitant use of nalmefene and opioid agonists. Discontinue nalmefene 1 week prior to any anticipated use of opioid agonistss. If combined, larger doses of opioid agonists will likely be required. Consider therapy modification
Naltrexone: May diminish the therapeutic effect of Opioid Agonists. Management: Seek therapeutic alternatives to opioids. See full drug interaction monograph for detailed recommendations. Consider therapy modification
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Ombitasvir, Paritaprevir, and Ritonavir: May increase the serum concentration of Buprenorphine. Monitor therapy
Ombitasvir, Paritaprevir, Ritonavir, and Dasabuvir: May increase the serum concentration of Buprenorphine. Monitor therapy
Opioid Agonists: Opioids (Mixed Agonist / Antagonist) may diminish the analgesic effect of Opioid Agonists. Management: Seek alternatives to mixed agonist/antagonist opioids in patients receiving pure opioid agonists, and monitor for symptoms of therapeutic failure/high dose requirements (or withdrawal in opioid-dependent patients) if patients receive these combinations. Exceptions: Buprenorphine; Butorphanol; Meptazinol; Nalbuphine; Pentazocine. Avoid combination
Opioids (Mixed Agonist / Antagonist): May diminish the therapeutic effect of Buprenorphine. This combination may also induce opioid withdrawal. Avoid combination
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Pegvisomant: Opioid Agonists may diminish the therapeutic effect of Pegvisomant. Monitor therapy
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
PHENobarbital: May enhance the CNS depressant effect of Buprenorphine. PHENobarbital may decrease the serum concentration of Buprenorphine. Management: Avoid use of buprenorphine and phenobarbital when possible. Monitor for respiratory depression/sedation. Because phenobarbital is also a strong CYP3A4 inducer, monitor for decreased buprenorphine efficacy and withdrawal if combined. Consider therapy modification
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
Primidone: May enhance the CNS depressant effect of Buprenorphine. Primidone may decrease the serum concentration of Buprenorphine. Management: Avoid use of buprenorphine and primidone when possible. Monitor for respiratory depression/sedation. Because primidone is also a strong CYP3A4 inducer, monitor for decreased buprenorphine efficacy and withdrawal if combined. Consider therapy modification
QT-prolonging Agents (Highest Risk): QT-prolonging Agents (Indeterminate Risk - Avoid) may enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Ramosetron: Opioid Agonists may enhance the constipating effect of Ramosetron. Monitor therapy
Rifabutin: May decrease the serum concentration of Buprenorphine. Monitor therapy
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Serotonergic Agents (High Risk): Opioid Agonists may enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Sincalide: Drugs that Affect Gallbladder Function may diminish the therapeutic effect of Sincalide. Management: Consider discontinuing drugs that may affect gallbladder motility prior to the use of sincalide to stimulate gallbladder contraction. Consider therapy modification
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Succinylcholine: May enhance the bradycardic effect of Opioid Agonists. Monitor therapy
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Adverse Reactions
Buccal film:
1% to 10%:
Cardiovascular: Hypertension (1% to <5%), peripheral edema (1% to <5%)
Central nervous system: Fatigue (≥5%), headache (4% to ≥5%), dizziness (2% to ≥5%), drowsiness (1% to ≥5%), anxiety (1% to <5%), depression (1% to <5%), falling (1% to <5%), insomnia (1% to <5%), opioid withdrawal syndrome (1% to <5%)
Dermatologic: Hyperhidrosis (1% to <5%), pruritus (1% to <5%), skin rash (1% to <5%)
Endocrine & metabolic: Hot flash (1% to <5%)
Gastrointestinal: Nausea (9% to 10%), diarrhea (≥5%), xerostomia (≥5%), vomiting (4% to ≥5%), constipation (3% to ≥5%), abdominal pain (1% to <5%), decreased appetite (1% to <5%), gastroenteritis (1% to <5%)
Genitourinary: Urinary tract infection (1% to <5%)
Hematologic & oncologic: Anemia (1% to <5%), bruise (1% to <5%)
Neuromuscular & skeletal: Back pain (1% to <5%), muscle spasm (1% to <5%)
Respiratory: Upper respiratory tract infection (≥5%), bronchitis (1% to <5%), nasopharyngitis (1% to <5%), oropharyngeal pain (1% to <5%), paranasal sinus congestion (1% to <5%), sinusitis (1% to <5%)
Miscellaneous: Fever (1% to <5%)
Implant:
>10%:
Central nervous system: Headache (13%)
Local: Local pain (13%; at implant site), local pruritus (12%; at implant site)
1% to 10%:
Cardiovascular: Chest pain (1%)
Central nervous system: Depression (6%), dizziness (4%), pain (4%), drowsiness (3%), fatigue (3%), chills (2%), migraine (2%), paresthesia (1%), sedation (1%), sensation of cold (1%)
Dermatologic: Localized erythema (10%; at implant site), skin rash (2%), excoriation (1% to 2%; including scratch), skin lesion (1%)
Gastrointestinal: Constipation (6%), nausea (6%), vomiting (6%), toothache (5%), upper abdominal pain (3%), flatulence (1%)
Hematologic & oncologic: Local hemorrhage (7%; at implant site)
Local: Localized edema (5%; at implant site), local swelling (1%)
Neuromuscular & skeletal: Back pain (6%), limb pain (3%), asthenia (2%)
Respiratory: Oropharyngeal pain (5%), cough (3%), dyspnea (1%)
Miscellaneous: Fever (3%), laceration (3%)
Injection:
>10%: Central nervous system: Sedation (≤66%)
1% to 10%:
Cardiovascular: Hypotension (1% to 5%)
Central nervous system: Vertigo (5% to 10%), dizziness (2% to 10%), headache (1% to 9%), fatigue (4% to 6%), drowsiness (2% to 5%)
Dermatologic: Injection site pruritus (6% to 10%), diaphoresis (1% to 5%)
Endocrine & metabolic: Increased gamma-glutamyl transferase (3% to 4%)
Gastrointestinal: Nausea (5% to 10%), constipation (8% to 9%), vomiting (1% to 9%)
Hepatic: Increased serum aspartate aminotransferase (3% to 5%), increased serum alanine aminotransferase (1% to 5%)
Local: Pain at injection site (5% to 6%), erythema at injection site (3% to 4%), bruising at injection site (1%), induration at injection site (1%), swelling at injection site (≤1%)
Neuromuscular & skeletal: Increased creatine phosphokinase (3% to 5%)
Ophthalmic: Miosis (1% to 5%)
Respiratory: Hypoventilation (1% to 5%)
Sublingual tablet:
>10%:
Central nervous system: Headache (29%), insomnia (21%)
Dermatologic: Diaphoresis (13%)
Gastrointestinal: Nausea (14%), abdominal pain (12%)
Infection: Infection (12%)
1% to 10%: Gastrointestinal: Constipation (8%), vomiting (8%)
Transdermal patch:
>10%:
Central nervous system: Dizziness (2% to 15%), headache (3% to 14%), drowsiness (2% to 13%)
Gastrointestinal: Nausea (6% to 21%), constipation (3% to 13%)
Local: Application-site pruritus (5% to 15%)
1% to 10%:
Cardiovascular: Chest pain (<5%), hypertension (<5%), peripheral edema (1% to <5%)
Central nervous system: Fatigue (≤5%), insomnia (<5%), anxiety (1% to <5%), depression (1% to <5%), falling (1% to <5%), hypoesthesia (1% to <5%), migraine (1% to <5%), pain (1% to <5%), paresthesia (1% to <5%)
Dermatologic: Pruritus (1% to 5%), hyperhidrosis (1% to <5%), skin rash (1% to <5%)
Gastrointestinal: Vomiting (≤9%), xerostomia (≥5% to 6%), anorexia (1% to <5%), diarrhea (1% to <5%), dyspepsia (1% to <5%), upper abdominal pain (1% to <5%), stomach discomfort (2%)
Genitourinary: Urinary tract infection (1% to <5%)
Infection: Influenza (1% to <5%)
Local: Application site erythema (5% to 10%), application site rash (5% to 8%), application site irritation (1% to 6%)
Neuromuscular & skeletal: Arthralgia (1% to <5%), asthenia (1% to <5%), back pain (1% to <5%), joint swelling (1% to <5%), limb pain (1% to <5%), muscle spasm (1% to <5%), musculoskeletal pain (1% to <5%), myalgia (1% to <5%), neck pain (1% to <5%), tremor (1% to <5%)
Respiratory: Bronchitis (1% to <5%), cough (1% to <5%), dyspnea (1% to <5%), nasopharyngitis (1% to <5%), pharyngolaryngeal pain (1% to <5%), sinusitis (1% to <5%), upper respiratory tract infection (1% to <5%)
Miscellaneous: Fever (1% to <5%)
<1%, postmarketing, and/or case reports: Abdominal distention, abdominal distress, abdominal pain, abnormal dreams, abnormal gait, abnormal hepatic function tests, accidental injury, acute sinusitis, agitation, amblyopia, anaphylactic shock, angina pectoris, angioedema, apathy, apnea, application site burning, application site dermatitis, application site discharge, application site reaction, application site vesicles, asthenia, ataxia, atrial fibrillation, blurred vision, bone fracture, bradycardia, bronchospasm, cellulitis, cellulitis at injection site, cerebrovascular accident, changes in respiration, chest pain, chills, cholecystitis, coma, confusion, conjunctivitis, contact dermatitis, coronary artery disease, cough, cyanosis, decreased libido, decreased mental acuity, decreased plasma testosterone, dehydration, depersonalization, depressed mood, depression, diarrhea, diplopia, disorientation, disturbance in attention, diverticulitis of the gastrointestinal tract, drug dependence (physical dependence), dysarthria, dysgeusia, dyspepsia, dysphagia, dysphoria, dyspnea, emotional lability, euphoria, exacerbation of asthma, excoriation, facial edema, flatulence, flushing, gallbladder disease (intracholedochal pressure), glossalgia, glossitis, hallucination, hepatic encephalopathy, hepatic failure, hepatic necrosis, hepatitis (including cytolytic), hepatorenal syndrome, hiccups, hot flash, hypersensitivity reaction, hyperventilation, hypoesthesia, hypogonadism (Brennan 2013; Debono 2011), hypotension, hypoventilation, increased blood pressure, increased serum alanine aminotransferase, increased serum aspartate aminotransferase, increased serum transaminases, injection site reaction, intestinal obstruction, jaundice, laceration, lethargy, local discomfort, localized warm feeling, loss of consciousness, malaise, memory impairment, mental status changes, migraine, miosis, musculoskeletal pain, myasthenia, nasal congestion, neck pain, nervousness, nightmares, noncardiac chest pain, opioid withdrawal syndrome, oral hypoesthesia, oral mucosa erythema, orthostatic hypotension, osteoarthritis, pallor, palpitations, pneumonia, prolonged Q-T interval on ECG, pruritus, psychosis, respiratory depression, respiratory distress, respiratory failure, restlessness, rhinitis, rhinorrhea, sedation, seizure, sensation of cold, sexual disorder, skin rash, slurred speech, stomatitis, syncope, tachycardia, tinnitus, tooth abscess, toothache, transient ischemic attacks, tremor, urinary hesitancy, urinary incontinence, urinary retention, urticaria, vasodilation, vertigo, visual disturbance, weight loss, Wenckebach period on ECG, wheezing, xeroderma, xerophthalmia, xerostomia
Warnings/Precautions
Concerns related to adverse effects:
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery, driving).
- Hepatic events: Hepatitis has been reported; hepatic events ranged from transient, asymptomatic transaminase elevations to hepatic failure; in many cases, patients had preexisting hepatic impairment. Monitor liver function tests in patients at increased risk for hepatotoxicity (eg, history of alcohol abuse, preexisting hepatic dysfunction, IV drug abusers) prior to and during therapy. Remove buprenorphine subdermal implant if signs and symptoms of buprenorphine toxicity develop concurrent with hepatic impairment. If signs and symptoms of toxicity or overdose occur within 2 weeks of extended-release injection, removal of the depot may be required.
- Hypersensitivity reactions: Hypersensitivity, including bronchospasm, angioneurotic edema, and anaphylactic shock, have been reported. The most common symptoms include rash, hives, and pruritus.
- Hypotension: May cause severe hypotension (including orthostatic hypotension and syncope); use with caution in patients with hypovolemia, cardiovascular disease (including acute MI), or drugs that may exaggerate hypotensive effects (including phenothiazines or general anesthetics). Monitor for symptoms of hypotension following initiation or dose titration. Avoid use in patients with circulatory shock.
- Infection: Subdermal implant: Infection may occur at site of insertion or removal, with excessive palpation shortly after insertion and improper removal increasing the risk. Examine the insertion site 1 week following insertion for signs of infection or problems with wound healing.
- QT prolongation: Buprenorphine has been observed to cause QTc prolongation. Do not exceed a dose of 900 mcg every 12 hours buccal film or one 20 mcg/hour transdermal patch. Avoid using in patients with a personal or family history of long QT syndrome or in patients taking concurrent class IA or III antiarrhythmics or other medications that prolong the QT interval. Use with caution in patients with hypokalemia, hypomagnesemia, or clinically unstable cardiac disease, including unstable heart failure, unstable atrial fibrillation, symptomatic bradycardia, or active MI.
- Respiratory depression: Buccal film, extended-release and immediate-release injection, transdermal patch: [US Boxed Warning]: Serious, life-threatening, or fatal respiratory depression may occur. Monitor closely for respiratory depression, especially during initiation or dose escalation. Misuse or abuse by chewing, swallowing, snorting, or injecting buprenorphine extracted from the buccal film or transdermal system will result in the uncontrolled delivery of buprenorphine and pose a significant risk of overdose and death. Misuse by self-injection of buprenorphine or the concomitant use of buprenorphine and benzodiazepines (or other CNS depressants, including alcohol) may result in coma or death. Carbon dioxide retention from opioid-induced respiratory depression can exacerbate the sedating effects of opioids. If the extended-release injection is discontinued due to respiratory depression, monitor the patient for ongoing respiratory depression for several months due to its extended-release characteristics. Use with caution in patients with compromised respiratory function (eg, chronic obstructive pulmonary disease, cor pulmonale, decreased respiratory reserve, hypoxia, hypercapnia, or preexisting respiratory depression).
Disease-related concerns:
- Abdominal conditions: May obscure diagnosis or clinical course of patients with acute abdominal conditions.
- Adrenocortical insufficiency: Use with caution in patients with adrenal insufficiency, including Addison disease. Long-term opioid use may cause adrenal insufficiency (nausea, vomiting, anorexia, fatigue, weakness, dizziness and low blood pressure) or secondary hypogonadism, which may lead to sexual dysfunction, infertility, mood disorders, and osteoporosis (Brennan 2013).
- Biliary tract impairment: Use with caution in patients with biliary tract dysfunction, including acute pancreatitis; opioids may cause constriction of sphincter of Oddi.
- Bowel obstruction: Use with caution in patients with a history of ileus or bowel obstruction; buccal film, immediate-release injection, and transdermal patch are contraindicated in patients with known or suspected GI obstruction, including paralytic ileus.
- CNS depression/coma: Avoid use in patients with impaired consciousness or coma because these patients are susceptible to intracranial effects of CO2 retention.
- Delirium tremens: Use with caution in patients with delirium tremens.
- Dermatological conditions: Subdermal implant: Use subdermal implants with caution in patients with a history of keloid formation, connective tissue disease (ie, scleroderma), or history of recurrent MRSA infections.
- Head trauma: Use with extreme caution in patients with head injury, intracranial lesions, or elevated intracranial pressure (ICP); exaggerated elevation of ICP may occur. Buprenorphine can produce miosis and changes in the level of consciousness that may interfere with patient evaluation.
- Hepatic impairment: Use buccal film and sublingual tablet with caution in patients with moderate hepatic impairment; dosage adjustment recommended in severe hepatic impairment. Use immediate-release injection with caution in patients with severe impairment. Subdermal implants should not be used in patients with preexisting moderate to severe hepatic impairment. Transdermal patch should not be used in patients with severe hepatic impairment; consider alternative therapy with more flexibility for dosing adjustments. Patients with preexisting moderate or severe hepatic impairment are not candidates for the extended-release injection. If moderate or severe impairment develops during treatment with the extended-release injection, continue with caution and monitor for toxicity for several months.
- Obesity: Use with caution in patients who are morbidly obese.
- Oral mucositis: Buccal film: Oral mucositis may lead to more rapid absorption and higher buprenorphine plasma levels; reduce dose in patients with oral mucositis and monitor closely for signs and symptoms of toxicity or overdose.
- Prostatic hyperplasia/urinary stricture: Use with caution in patients with prostatic hyperplasia and/or urinary stricture.
- Psychosis: Use with caution in patients with toxic psychosis.
- Renal impairment: Use with caution in patients with renal impairment.
- Respiratory disease: Use with caution and monitor for respiratory depression in patients with significant chronic obstructive pulmonary disease or cor pulmonale, and those with a substantially decreased respiratory reserve, hypoxia, hypercapnia, or preexisting respiratory depression, particularly when initiating and titrating therapy; critical respiratory depression may occur, even at therapeutic dosages. Consider the use of alternative nonopioid analgesics in these patients.
- Seizure: Use with caution in patients with a history of seizure disorders; may cause or exacerbate preexisting seizures.
- Sleep-related disorders: Opioid use increases the risk for sleep-related disorders (eg, central sleep apnea [CSA], hypoxemia) in a dose-dependent fashion. Use with caution for chronic pain and titrate dosage cautiously in patients with risk factors for sleep-disordered breathing (eg, heart failure, obesity). Consider dose reduction in patients presenting with CSA. Avoid opioids in patients with moderate to severe sleep-disordered breathing (Dowell [CDC 2016]).
- Thyroid dysfunction: Use with caution in patients with thyroid dysfunction.
Concurrent drug therapy issues:
- Benzodiazepines and other CNS depressants: [US Boxed Warning]: Buccal film, extended-release and immediate-release injection, transdermal patch: Concomitant use of benzodiazepines or other CNS depressants, including alcohol and opioids, may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing of opioids and benzodiazepines or other CNS depressants for use in patients for whom alternative treatment options are inadequate. Limit dosages and durations to the minimum required. Follow patients for signs and symptoms of respiratory depression and sedation. Prohibiting medication-assisted treatment of opioid use disorder may increase the risk of morbidity and mortality, therefore patients should be educated on the risks of concomitant use with benzodiazepines, sedatives, opioid analgesics, and alcohol. Strategies should be developed to manage use of prescribed or illicit benzodiazepines or other CNS depressants at initiation of or during treatment with buprenorphine; adjustments to induction procedures and additional monitoring may be required. If appropriate, delay or omit buprenorphine dose if a patient is sedated at time of buprenorphine dosing. Discontinuation of benzodiazepines or other CNS depressants is preferred; gradual tapering of benzodiazepine or other CNS depressant, decreasing to lowest effective dose, or monitoring in a higher level of care for taper may be appropriate. Benzodiazepines are not the treatment of choice for anxiety or insomnia for patients in buprenorphine treatment; make sure patients are appropriately diagnosed and consider alternative medications for anxiety and insomnia prior to coadministration of benzodiazepines and buprenorphine.
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Cachectic or debilitated patients: Use with caution in cachectic or debilitated patients; there is a greater potential for life-threatening respiratory depression, even at therapeutic dosages. Consider the use of alternative nonopioid analgesics in these patients.
- Elderly: Use with caution in elderly patients; may be more sensitive to adverse effects (eg, life-threatening respiratory depression). In chronic pain, monitor opioid use closely in this age group due to an increased potential for risks, including certain risks such as falls/fracture, cognitive impairment, and constipation (Dowell [CDC 2016]). Consider the use of alternative nonopioid analgesics in these patients.
- Neonates: Neonatal withdrawal syndrome: Buccal film, extended-release and immediate-release injection, transdermal patch: [US Boxed Warning]: Prolonged use of opioids during pregnancy can cause neonatal withdrawal syndrome, which may be life-threatening if not recognized and treated according to protocols developed by neonatology experts. If opioid use is required for a prolonged period in a pregnant woman, advise the patient of the risk of neonatal withdrawal syndrome and ensure that appropriate treatment will be available. Signs and symptoms include irritability, hyperactivity and abnormal sleep pattern, high-pitched cry, tremor, vomiting, diarrhea, and failure to gain weight. Onset, duration, and severity depend on the drug used, duration of use, maternal dose, and rate of drug elimination by the newborn.
Dosage form specific issues:
- Extended-release injection: [US Boxed Warning]: Serious harm or death could result if extended-release injection is administered IV. The injection forms a solid mass upon contact with body fluids and may cause occlusion, local tissue damage, and thromboembolic events, including life-threatening pulmonary emboli if administered IV. Because of the risk of serious harm or death that could result from IV self-administration, buprenorphine extended-release injection is only available through a restricted program called the Sublocade REMS Program. Health care settings and pharmacies that order and dispense buprenorphine extended-release injection must be certified in this program and comply with the REMS requirements. Administer via subcutaneous route only. Do not administer IM or IV.
- Subdermal implant: [US Boxed Warning]: Insertion and removal of implant are associated with the risk of implant migration, protrusion, and expulsion. Rare but serious complications including nerve damage and migration resulting in embolism and death may result from improper insertion in the upper arm. Additional complications may include local migration, protrusion, and expulsion. Incomplete insertions or infections may lead to protrusion or expulsion. Because of the risks associated with insertion and removal, buprenorphine implant is available only through a restricted program. All health care providers must successfully complete a live training program on the insertion and removal procedures and become certified, prior to performing insertions or prescribing buprenorphine implants. Patients must be monitored to ensure that the implant is removed by a health care provider certified to perform insertions.
- Transdermal patch: To properly dispose of transdermal patch, fold it over on itself and flush down the toilet immediately (if a drug take-back option is not readily available); alternatively, seal the used patch in the provided Patch-Disposal Unit and dispose of in the trash. Avoid exposure of application site and surrounding area to direct external heat sources (eg, heating pads, electric blankets, heat or tanning lamps, hot baths/saunas, hot water bottles, direct sunlight). Buprenorphine release from the patch is temperature-dependent and may result in overdose. Patients who experience fever or increase in core temperature should be monitored closely and adjust dose if signs of respiratory depression or CNS depression occur. Application-site reactions, including rare cases of severe reactions (eg, vesicles, discharge, "burns"), have been observed with use; onset varies from days to months after initiation; patients should be instructed to report severe reactions promptly and discontinue therapy.
Special handling:
- Disposal: Extended-release injection and subdermal implant: Handle the removed depots or implants with adequate security, accountability, and proper disposal, per facility procedure for a Schedule III drug product, and per applicable federal, state, and local regulations.
Other warnings/precautions:
- Abrupt discontinuation/withdrawal: Abrupt discontinuation in patients who are physically dependent to opioids has been associated with serious withdrawal symptoms, uncontrolled pain, attempts to find other opioids (including illicit), and suicide. Use a collaborative, patient-specific taper schedule that minimizes the risk of withdrawal, considering factors such as current opioid dose, duration of use, type of pain, and physical and psychological factors. Monitor pain control, withdrawal symptoms, mood changes, suicidal ideation, and for use of other substances and provide care as needed. Concurrent use of opioid agonist/antagonist analgesics may also precipitate withdrawal symptoms and/or reduced analgesic efficacy in patients following prolonged therapy with mu opioid agonists. Withdrawal signs and symptoms will be delayed in patients who discontinue the ER injection or have it removed; transmucosal buprenorphine may be needed to treat withdrawal in these patients. Tablets, which are used for induction treatment of opioid dependence, should not be started until objective and clear signs of moderate withdrawal are evident. If subdermal implants are not immediately replaced in contralateral arm after removal, maintain patients on their previous dosage of sublingual buprenorphine.
- Abuse/misuse/diversion: Buccal film, extended-release and immediate-release injection, transdermal patch: [US Boxed Warning]: Use exposes patients and other users to the risks of addiction, abuse, and misuse, potentially leading to overdose and death. Assess each patient's risk prior to prescribing; monitor all patients regularly for development of these behaviors or conditions. Use with caution in patients with a history of drug abuse or acute alcoholism; potential for drug dependency exists. Other factors associated with an increased risk for misuse include younger age and psychotropic medication use. Consider offering naloxone prescriptions in patients with factors associated with an increased risk for overdose, such as history of overdose or substance use disorder, higher opioid dosages (≥50 morphine milligram equivalents/day orally), and concomitant benzodiazepine use (Dowell [CDC 2016]). The misuse of buccal film by swallowing or of transdermal patch by placing it in the mouth, chewing it, swallowing it, or using it in ways other than indicated may cause choking, overdose, and death.
- Accidental ingestion: Buccal film, transdermal patch: [US Boxed Warning]: Accidental ingestion of even one dose, especially in children, can result in a fatal overdose of buprenorphine.
- Acute pain: When using buprenorphine for treatment of opioid dependence, treat acute pain with nonopioid analgesics whenever possible. If treatment with a high-affinity full opioid analgesic is required, monitor closely for respiratory depression because high doses may be necessary to achieve pain relief.
- Appropriate use: Buccal film, transdermal patch: Indicated for the management of pain severe enough to require daily, around-the-clock, long-term opioid treatment; should not be used for as-needed pain relief. Therapy with the buccal film or transdermal patch is not appropriate for use in the management of addictions. When used for chronic pain (outside of end-of-life or palliative care, active cancer treatment, sickle cell disease, or medication-assisted treatment for opioid use disorder) in outpatient setting in adults, opioids should not be used as first-line therapy for chronic pain management (pain >3-month duration or beyond time of normal tissue healing) due to limited short-term benefits, undetermined long-term benefits, and association with serious risks (eg, overdose, MI, auto accidents, risk of developing opioid use disorder). Preferred management includes nonpharmacologic therapy and nonopioid therapy (eg, NSAIDs, acetaminophen, certain anticonvulsants and antidepressants). If opioid therapy is initiated, it should be combined with nonpharmacologic and nonopioid therapy, as appropriate. Prior to initiation, known risks of opioid therapy should be discussed and realistic treatment goals for pain/function should be established, including consideration for discontinuation if benefits do not outweigh risks. Therapy should be continued only if clinically meaningful improvement in pain/function outweighs risks. Therapy should be initiated at the lowest effective dosage using immediate-release opioids (instead of extended-release/long-acting opioids). Risk associated with use increases with higher opioid dosages. Risks and benefits should be re-evaluated when increasing dosage to ≥50 morphine milligram equivalents (MME)/day orally; dosages ≥90 MME/day orally should be avoided unless carefully justified (Dowell [CDC 2016]).
- Appropriate use: Subdermal implant: Not appropriate for patients who are new to treatment or have not sustained prolonged clinical stability on buprenorphine ≤8 mg/day.
- Discontinuation of therapy: Extended-release injection and sublingual tablet: There is no maximum recommended duration for maintenance treatment of opioid addiction; patients may require treatment indefinitely. Advise patients of the potential to relapse to illicit drug use following discontinuation of opioid agonist/partial agonist medication-assisted treatment. If the extended-release injection is discontinued or the depot is removed, monitor the patient for several months for signs and symptoms of withdrawal. After steady-state has been achieved (4 to 6 months), patients discontinuing extended-release injections may have detectable plasma levels of buprenorphine for 12 months or longer.
- Optimal pain regimen: An opioid-containing analgesic regimen should be tailored to each patient's needs and based upon the type of pain being treated (acute versus chronic), the route of administration, degree of tolerance for opioids (naive versus chronic user), age, weight, and medical condition. The optimal analgesic dose varies widely among patients; doses should be titrated to pain relief/prevention. When switching patients from buprenorphine to naltrexone, do not initiate naltrexone until 7 to 14 days after buprenorphine discontinuation. No time delay is required when switching patients from buprenorphine to methadone (Kampman [ASAM 2015]).
- Partial opioid agonist and mixed opioid agonist/antagonist overdose: Reversal of partial opioid agonists or mixed opioid agonist/antagonists (eg, buprenorphine, pentazocine) may be incomplete and large doses of naloxone may be required.
- REMS program: [US Boxed Warning]: To ensure that the benefits of opioid analgesics outweigh the risks of addiction, abuse, and misuse, a REMS is required. Drug companies with approved opioid analgesic products must make REMS-compliant education programs available to health care providers. Health care providers are encouraged to complete a REMS-compliant education program; counsel patients and/or their caregivers, with every prescription, on safe use, serious risks, storage, and disposal of these products; emphasize to patients and their caregivers the importance of reading the Medication Guide every time it is provided by their pharmacist; and consider other tools to improve patient, household, and community safety.
- Surgery: In patients undergoing elective surgery (excluding caesarean section), discontinuation of buprenorphine 24 to 36 hours before anticipated need for surgical anesthesia may be considered. Short-acting opioids may be given during and/or after surgery. In patients unable to abruptly discontinue buprenorphine prior to surgery, full opioid agonists may be added to the buprenorphine to maintain proper anesthesia; however, increased doses may be required to overcome buprenorphine receptor blockade. If opioid therapy is required as part of anesthesia, patients should be continuously monitored in an anesthesia care setting by persons not involved in in the conduct of the surgical or diagnostic procedure. This guidance applies to anyone who has been treated with extended release buprenorphine injection within the past 6 months. The decision whether to discontinue buprenorphine prior to elective surgery should be made in consultation with the surgeon and anesthesiologist (Kampman [ASAM 2015]).
Monitoring Parameters
Pain relief, respiratory and mental status, CNS depression (especially in elderly, debilitated or cachectic patients particularly during treatment initiation or titration, or when using concomitant CNS depressants), blood pressure (monitor for hypotension during initiation and titration); LFTs (prior to initiation and during therapy); monthly for 300 mg maintenance treatment with extended-release injection); signs of addiction, abuse, or misuse; symptoms of withdrawal; patients with biliary tract disease for worsening symptoms; application site reactions (transdermal patch); signs or symptoms of hypogonadism or hypoadrenalism (Brennan 2013); signs and symptoms of toxicity or overdose (especially in patients with hepatic impairment); signs of infection or problems with wound healing one week after insertion of subdermal implant.
Alternate recommendations: Chronic pain (long-term therapy outside of end-of-life or palliative care, active cancer treatment, sickle cell disease, or medication-assisted treatment for opioid use disorder): Evaluate benefits/risks of opioid therapy within 1 to 4 weeks of treatment initiation and with dose increases. Re-evaluate benefits/risks every 3 months during therapy or more frequently in patients at increased risk of overdose or opioid use disorder. Urine drug testing is recommended prior to initiation and re-checking should be considered at least yearly (includes controlled prescription medications and illicit drugs of abuse). State prescription drug monitoring program (PDMP) data should be reviewed by clinicians prior to initiation and periodically during therapy (frequency ranging from every prescription to every 3 months) (Dowell [CDC 2016]).
Note: Patients undergoing planned surgical procedures, in advance of a procedure, should consult with their buprenorphine prescriber in collaboration with the surgeon, to consider buprenorphine taper and alternative opioid management. Patients undergoing urgent or emergent procedures may require higher than expected opioid doses to achieve adequate analgesia and should be monitored carefully for decreasing opioid requirements as buprenorphine is eliminated. Some patients may achieve adequate analgesia with continued or increased buprenorphine (Alford 2006; Chern 2013; Huang 2014).
Pregnancy
Pregnancy Considerations
Buprenorphine crosses the placenta; buprenorphine and norbuprenorphine can be detected in newborn serum, urine, hair, and meconium following in utero exposure (Di Trana 2019).
According to some studies, maternal use of opioids may be associated with birth defects (including neural tube defects, congenital heart defects, and gastroschisis), poor fetal growth, stillbirth, and preterm delivery (CDC [Dowell 2016]). Opioids used as part of obstetric analgesia/anesthesia during labor and delivery may temporarily affect the fetal heart rate (ACOG 209 2019).
[US Boxed Warning]: Prolonged use of opioids during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated and requires management according to protocols developed by neonatology experts. If opioid use is required for a prolonged period in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure appropriate treatment will be available. Symptoms of neonatal abstinence syndrome (NAS) following opioid exposure may be autonomic (eg, fever, temperature instability), gastrointestinal (eg, diarrhea, vomiting, poor feeding/weight gain), or neurologic (eg, high-pitched crying, hyperactivity, increased muscle tone, increased wakefulness/abnormal sleep pattern, irritability, sneezing, seizure, tremor, yawning) (Dow 2012; Hudak 2012). The onset and duration of neonatal withdrawal symptoms are dependent upon the specific opioid used, maternal dosing, and rate of elimination by the newborn. NAS associated with buprenorphine may correlate to concentrations of norbuprenorphine in the cord blood (Shah 2016). Opioids may cause respiratory depression and psycho-physiologic effects in the neonate; newborns of mothers receiving opioids during pregnancy and/or labor should be monitored.
Opioid agonist pharmacotherapy is recommended for pregnant women with an opioid use disorder. Transmucosal buprenorphine is a recommended treatment option (ACOG 711 2017; SAMHSA 2018). Due to pregnancy-induced physiologic changes, some pharmacokinetic properties of sublingual buprenorphine may be altered (Bastian 2017; Caritis 2017; Zhang 2018). Use of the subcutaneous implant is not currently recommended in pregnant women (SAMHSA 2018). Maintenance doses of buprenorphine will not provide adequate pain relief during labor. Women receiving buprenorphine for the treatment of opioid use disorder should be maintained on their daily dose of buprenorphine in addition to receiving the same pain management options during labor and delivery as opioid-naive women; Opioid agonist-antagonists should be avoided for the treatment of labor pain in women maintained on buprenorphine due to the risk of precipitating acute withdrawal (ACOG 711 2017; SAMHSA 2018). Use of a multimodal approach to pain relief which can maximize non-opioid interventions is recommended. Monitor for maternal over sedation and somnolence (Krans 2019).
Pregnancy testing is recommended prior to initiating therapy for opioid use disorders (SAMHSA 2018). Long-term opioid use may cause infertility in males and females of reproductive potential. Amenorrhea may develop secondary to substance abuse. Initiation of buprenorphine maintenance treatment may improve fertility resulting in unplanned pregnancy. Contraception counseling is recommended (Dow 2012).
Patient Education
What is this drug used for?
Implant, long-acting injection, and under the tongue (sublingual) tablet:
- It is used to treat pain drug (opioid) addiction.
Implant and long-acting injection:
- This drug is only for use by people who have been taking pain drugs (opioids) and are used to their effects. Talk with the doctor.
Short-acting injection:
- It is used to ease pain.
Cheek film and patch:
- It is used to ease very bad pain.
- It is only to be used when around-the-clock (continuous) care is needed for a long time. It is also only to be used when other pain drugs do not treat your pain well enough or you cannot take them.
All oral products, short-acting injection, and patch:
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Tooth pain
- Back pain
- Dry mouth
- Common cold symptoms
- Numbness or tingling of mouth
- Mouth pain
- Throat pain
- Skin irritation
- Diarrhea
- Trouble sleeping
- Nausea
- Vomiting
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Slow breathing
- Shallow breathing
- Difficulty breathing
- Shortness of breath
- Numbness or weakness of arm
- Implant site bleeding
- Sexual dysfunction (males)
- No menstrual periods
- Decreased sex drive
- Trouble getting pregnant
- Severe dizziness
- Passing out
- Sweating a lot
- Fast heartbeat
- Slow heartbeat
- Abnormal heartbeat
- Confusion
- Severe constipation
- Severe loss of strength and energy
- Anxiety
- Chills
- Sore throat
- Change in balance
- Mood changes
- Severe abdominal pain
- Abnormal movements
- Slow movements
- Slurred speech
- Swelling of arms or legs
- Vision changes
- Burning or numbness feeling
- Difficulty speaking
- Chest pain
- Unable to pass urine
- Sensing things that seem real but are not
- Muscle pain
- Joint pain
- Trouble with memory
- Seizures
- Severe headache
- Tremors
- Severe fatigue
- Difficulty focusing
- Stumbling
- Drunk feeling
- Serotonin syndrome like dizziness, severe headache, agitation, sensing things that seem real but are not, fast heartbeat, abnormal heartbeat, flushing, tremors, sweating a lot, change in balance, severe nausea, or severe diarrhea.
- Adrenal gland problems like severe nausea, vomiting, severe dizziness, passing out, muscle weakness, severe fatigue, mood changes, lack of appetite, or weight loss.
- Depression
- Injection site irritation, edema, or redness
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.