Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule, Oral:
Fiorinal: Butalbital 50 mg, aspirin 325 mg, and caffeine 40 mg [DSC]
Fiorinal: Butalbital 50 mg, aspirin 325 mg, and caffeine 40 mg [contains fd&c yellow #10 (quinoline yellow)]
Generic: Butalbital 50 mg, aspirin 325 mg, and caffeine 40 mg
Tablet, Oral:
Generic: Butalbital 50 mg, aspirin 325 mg, and caffeine 40 mg
Pharmacology
Mechanism of Action
Aspirin: Inhibits prostaglandin synthesis in the CNS and peripherally blocks pain impulse generation
Butalbital: Short- to intermediate-acting barbiturate; depresses the sensory cortex, decreases motor activity, alters cerebellar function, and produces drowsiness, sedation, hypnosis, and dose-dependent respiratory depression
Caffeine: A CNS stimulant
Use: Labeled Indications
Tension or muscle contraction headache: Relief of the symptomatic complex of tension (or muscle contraction) headache
Contraindications
Hypersensitivity to aspirin, caffeine, butalbital, or any component of the formulation; hemorrhagic diathesis (eg, hemophilia, hypoprothrombinemia, von Willebrand disease, thrombocytopenias, thrombasthenia and other ill-defined hereditary platelet dysfunctions, severe vitamin K deficiency, severe liver damage); syndrome of nasal polyps, angioedema, and bronchospastic reactivity to aspirin or other nonsteroidal anti-inflammatory drugs; peptic ulcer or other serious GI lesions; porphyria.
Canadian labeling: Additional contraindications (not in US labeling): History of abuse or overdose due to alcohol, hypnotics, analgesics, or psychotropic drugs
Dosage and Administration
Dosing: Adult
Note: Limit butalbital use to ≤3 days per month to avoid medication overuse headache (Garza 2006); studies have found increased risk with use of ≥5 days per month (Da Silva 2014).
Tension or muscle contraction headache: Oral: 1 to 2 capsules every 4 hours as needed; maximum: 6 capsules per day.
Discontinuation of therapy: For low butalbital doses or less frequent use, consider abrupt discontinuation of therapy or a gradual taper over 2 to 4 weeks. If use is frequent, at high doses, or if a patient has developed chronic migraines, discontinuing the butalbital-containing product and replacing with a gradual (eg, over 2 to 4 weeks) phenobarbital taper is advised to avoid withdrawal symptoms (ie, worsened headache, nausea/vomiting, restlessness, anxiety, diaphoresis, disturbed sleep, seizures). Consider providing bridge therapy with a medication to treat acute headaches and optimizing a preventative regimen to avoid rebound headaches (Boes 2006; Garza 2019).
Dosing: Geriatric
Avoid use (Beers Criteria [AGS 2019]).
Storage
Store below 25°C (77°F). Protect from moisture.
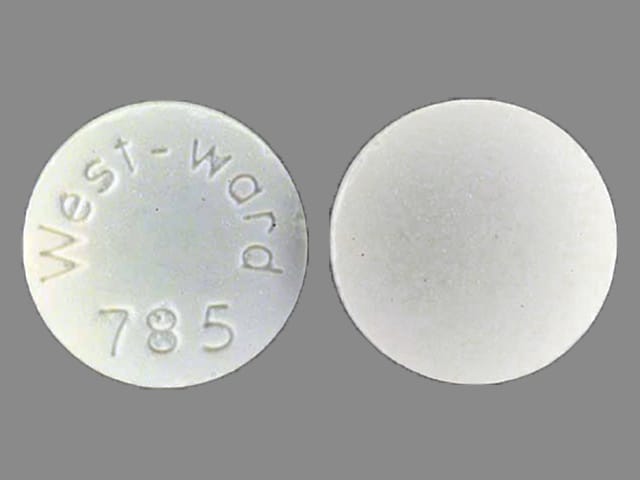
Butalbital, Aspirin, and Caffeine Images
Drug Interactions
Acalabrutinib: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Acebrophylline: May enhance the stimulatory effect of CNS Stimulants. Avoid combination
Adenosine: Caffeine and Caffeine Containing Products may diminish the therapeutic effect of Adenosine. Management: Monitor for decreased effect of adenosine if patient is receiving caffeine. Discontinue caffeine in advance of scheduled diagnostic use of adenosine whenever possible. Consider therapy modification
Agents with Antiplatelet Properties (e.g., P2Y12 inhibitors, NSAIDs, SSRIs, etc.): May enhance the adverse/toxic effect of Salicylates. Increased risk of bleeding may result. Monitor therapy
Agents with Antiplatelet Properties (e.g., P2Y12 inhibitors, NSAIDs, SSRIs, etc.): May enhance the antiplatelet effect of other Agents with Antiplatelet Properties. Monitor therapy
Ajmaline: Salicylates may enhance the adverse/toxic effect of Ajmaline. Specifically, the risk for cholestasis may be increased. Monitor therapy
Alcohol (Ethyl): May enhance the adverse/toxic effect of Aspirin. Specifically, alcohol may increase the bleeding risk of aspirin. Alcohol (Ethyl) may diminish the therapeutic effect of Aspirin. Specifically, alcohol may interfere with the controlled release mechanism of extended release aspirin. Management: Monitor patients who drink 3 or more alcoholic drinks a day for increased bleeding while taking aspirin. Counsel patients about the risk of bleeding and discourage such consumption. Give extended release aspirin 2 hours before, or 1 hour after, alcohol. Consider therapy modification
Alendronate: Aspirin may enhance the adverse/toxic effect of Alendronate. Specifically, the incidence of upper gastrointestinal adverse events may be increased Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Amifampridine: Agents With Seizure Threshold Lowering Potential may enhance the neuroexcitatory and/or seizure-potentiating effect of Amifampridine. Monitor therapy
Ammonium Chloride: May increase the serum concentration of Salicylates. Monitor therapy
Angiotensin-Converting Enzyme Inhibitors: Salicylates may enhance the nephrotoxic effect of Angiotensin-Converting Enzyme Inhibitors. Salicylates may diminish the therapeutic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Anticoagulants: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Anticoagulants. Exceptions: Bemiparin; Enoxaparin; Heparin. Monitor therapy
Anticoagulants: Salicylates may enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Apixaban: Aspirin may enhance the adverse/toxic effect of Apixaban. Specifically, the risk for bleeding may be increased. Management: Carefully consider risks and benefits of this combination and monitor closely. Consider therapy modification
AtoMOXetine: May enhance the hypertensive effect of Sympathomimetics. AtoMOXetine may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Bemiparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Bemiparin. Management: Avoid concomitant use of bemiparin with antiplatelet agents. If concomitant use is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Benzbromarone: Salicylates may diminish the therapeutic effect of Benzbromarone. Monitor therapy
Beta-Blockers: Barbiturates may decrease the serum concentration of Beta-Blockers. Exceptions: Atenolol; Levobunolol; Metipranolol; Nadolol. Monitor therapy
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Blood Glucose Lowering Agents: Salicylates may enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Blood Pressure Lowering Agents: Barbiturates may enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Broccoli: May decrease the serum concentration of CYP1A2 Substrates (High risk with Inducers). Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
BuPROPion: May enhance the neuroexcitatory and/or seizure-potentiating effect of Agents With Seizure Threshold Lowering Potential. Monitor therapy
Calcium Channel Blockers: Barbiturates may increase the metabolism of Calcium Channel Blockers. Management: Monitor for decreased therapeutic effects of calcium channel blockers with concomitant barbiturate therapy. Calcium channel blocker dose adjustments may be necessary. Nimodipine Canadian labeling contraindicates concomitant use with phenobarbital. Exceptions: Clevidipine. Monitor therapy
Calcium Channel Blockers (Nondihydropyridine): May enhance the antiplatelet effect of Aspirin. Monitor therapy
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May decrease the serum concentration of CYP1A2 Substrates (High risk with Inducers). Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Carbonic Anhydrase Inhibitors: Salicylates may enhance the adverse/toxic effect of Carbonic Anhydrase Inhibitors. Salicylate toxicity might be enhanced by this same combination. Management: Avoid these combinations when possible.Dichlorphenamide use with high-dose aspirin as contraindicated. If another combination is used, monitor patients closely for adverse effects. Tachypnea, anorexia, lethargy, and coma have been reported. Exceptions: Brinzolamide; Dorzolamide. Consider therapy modification
Carisoprodol: Aspirin may increase serum concentrations of the active metabolite(s) of Carisoprodol. Specifically, Meprobamate concentrations may be increased. Aspirin may decrease the serum concentration of Carisoprodol. Monitor therapy
Cephalothin: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Cephalothin. Specifically, the risk for bleeding may be increased. Monitor therapy
Chloramphenicol (Systemic): May decrease the metabolism of Barbiturates. Barbiturates may increase the metabolism of Chloramphenicol (Systemic). Consider therapy modification
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
CloZAPine: CYP1A2 Inhibitors (Weak) may increase the serum concentration of CloZAPine. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
Cocaine (Topical): May enhance the hypertensive effect of Sympathomimetics. Management: Consider alternatives to use of this combination when possible. Monitor closely for substantially increased blood pressure or heart rate and for any evidence of myocardial ischemia with concurrent use. Consider therapy modification
Collagenase (Systemic): Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Collagenase (Systemic). Specifically, the risk of injection site bruising and/or bleeding may be increased. Monitor therapy
Corticosteroids (Systemic): Salicylates may enhance the adverse/toxic effect of Corticosteroids (Systemic). These specifically include gastrointestinal ulceration and bleeding. Corticosteroids (Systemic) may decrease the serum concentration of Salicylates. Withdrawal of corticosteroids may result in salicylate toxicity. Monitor therapy
CycloSPORINE (Systemic): Barbiturates may increase the metabolism of CycloSPORINE (Systemic). Consider therapy modification
CYP1A2 Inducers (Moderate): May decrease the serum concentration of Caffeine and Caffeine Containing Products. Monitor therapy
CYP1A2 Inhibitors (Moderate): May increase the serum concentration of Caffeine and Caffeine Containing Products. Monitor therapy
Dabigatran Etexilate: Aspirin may enhance the adverse/toxic effect of Dabigatran Etexilate. Specifically, the risk for bleeding may be increased. Management: Carefully consider risks and benefits of this combination and monitor closely; Canadian labeling states that low dose aspirin could be considered, but the use of antiplatelets are not recommended for stroke prevention in patients with atrial fibrillation. Consider therapy modification
Dasatinib: May enhance the anticoagulant effect of Agents with Antiplatelet Properties. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Deoxycholic Acid: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Deoxycholic Acid. Specifically, the risk for bleeding or bruising in the treatment area may be increased. Monitor therapy
Dexibuprofen: Aspirin may enhance the adverse/toxic effect of Dexibuprofen. Dexibuprofen may diminish the cardioprotective effect of Aspirin. Avoid combination
Dexketoprofen: Salicylates may enhance the adverse/toxic effect of Dexketoprofen. Dexketoprofen may diminish the therapeutic effect of Salicylates. Salicylates may decrease the serum concentration of Dexketoprofen. Management: The use of high-dose salicylates (3 g/day or more in adults) together with dexketoprofen is inadvisable. Consider administering dexketoprofen 30-120 min after or at least 8 hrs before cardioprotective doses of aspirin to minimize any possible interaction. Avoid combination
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Doxofylline: Caffeine and Caffeine Containing Products may enhance the adverse/toxic effect of Doxofylline. Avoid combination
Doxycycline: Barbiturates may decrease the serum concentration of Doxycycline. Consider therapy modification
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Edoxaban: Aspirin may enhance the adverse/toxic effect of Edoxaban. Specifically, the risk of bleeding may be increased. Aspirin may increase the serum concentration of Edoxaban. Management: Carefully consider the anticipated risks and benefits of this combination. If combined, increased monitoring for bleeding is recommended. Consider therapy modification
Enoxaparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Enoxaparin. Management: Discontinue antiplatelet agents prior to initiating enoxaparin whenever possible. If concomitant administration is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Esketamine: May enhance the hypertensive effect of CNS Stimulants. Monitor therapy
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Estrogen Derivatives (Contraceptive): Barbiturates may diminish the therapeutic effect of Estrogen Derivatives (Contraceptive). Contraceptive failure is possible. Management: Use of a non-hormonal contraceptive is recommended. Consider therapy modification
Fat Emulsion (Fish Oil Based): May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Monitor therapy
Felbamate: May increase the serum concentration of Barbiturates. Barbiturates may decrease the serum concentration of Felbamate. Management: Monitor for elevated barbiturate concentrations/toxicity if felbamate is initiated/dose increased, or reduced concentrations/effects if felbamate is discontinued/dose decreased. Refer to phenobarbital dosing guidelines for patients receiving that agent. Monitor therapy
Felbinac: May enhance the adverse/toxic effect of Aspirin. Monitor therapy
Floctafenine: May enhance the adverse/toxic effect of Aspirin. An increased risk of bleeding may be associated with use of this combination. Floctafenine may diminish the cardioprotective effect of Aspirin. Avoid combination
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
Formoterol: Caffeine and Caffeine Containing Products may enhance the adverse/toxic effect of Formoterol. Caffeine and Caffeine Containing Products may enhance the hypokalemic effect of Formoterol. Monitor therapy
Ginkgo Biloba: May enhance the anticoagulant effect of Salicylates. Management: Consider alternatives to this combination of agents. Monitor for signs and symptoms of bleeding (especially intracranial bleeding) if salicylates are used in combination with ginkgo biloba. Consider therapy modification
Glucosamine: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Gold Sodium Thiomalate: Aspirin may enhance the adverse/toxic effect of Gold Sodium Thiomalate. Specifically, liver function tests may be elevated when these agents are combined. Monitor therapy
Griseofulvin: Barbiturates may decrease the serum concentration of Griseofulvin. Monitor therapy
Guanethidine: May enhance the arrhythmogenic effect of Sympathomimetics. Guanethidine may enhance the hypertensive effect of Sympathomimetics. Monitor therapy
Hemin: Barbiturates may diminish the therapeutic effect of Hemin. Avoid combination
Heparin: Aspirin may enhance the anticoagulant effect of Heparin. Monitor therapy
Herbs (Anticoagulant/Antiplatelet Properties) (eg, Alfalfa, Anise, Bilberry): May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Bleeding may occur. Management: Avoid combination when possible. If used, monitor more closely for evidence of bleeding. Discontinue herbal products with anticoagulant or antiplatelet actions 2 weeks prior to surgical, dental, or invasive procedures. Consider therapy modification
Herbs (Anticoagulant/Antiplatelet Properties) (eg, Alfalfa, Anise, Bilberry): May enhance the adverse/toxic effect of Salicylates. Bleeding may occur. Consider therapy modification
Hyaluronidase: Salicylates may diminish the therapeutic effect of Hyaluronidase. Management: Patients receiving salicylates (particularly at larger doses) may not experience the desired clinical response to standard doses of hyaluronidase. Larger doses of hyaluronidase may be required. Consider therapy modification
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of Barbiturates. Management: Consider a decrease in the barbiturate dose, as appropriate, when used together with hydroxyzine. With concurrent use, monitor patients closely for excessive response to the combination. Consider therapy modification
Ibritumomab Tiuxetan: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Ibritumomab Tiuxetan. Both agents may contribute to impaired platelet function and an increased risk of bleeding. Monitor therapy
Ibrutinib: May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Monitor therapy
Indacaterol: Caffeine and Caffeine Containing Products may enhance the adverse/toxic effect of Indacaterol. Caffeine and Caffeine Containing Products may enhance the hypokalemic effect of Indacaterol. Monitor therapy
Influenza Virus Vaccine (Live/Attenuated): May enhance the adverse/toxic effect of Salicylates. Specifically, Reye's syndrome may develop. Avoid combination
Inotersen: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Iohexol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iohexol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iohexol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iomeprol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iomeprol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iomeprol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iopamidol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iopamidol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iopamidol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Ketorolac (Nasal): May enhance the adverse/toxic effect of Aspirin. An increased risk of bleeding may be associated with use of this combination. Ketorolac (Nasal) may diminish the cardioprotective effect of Aspirin. Avoid combination
Ketorolac (Systemic): May enhance the adverse/toxic effect of Aspirin. An increased risk of bleeding may be associated with use of this combination. Ketorolac (Systemic) may diminish the cardioprotective effect of Aspirin. Avoid combination
LamoTRIgine: Barbiturates may decrease the serum concentration of LamoTRIgine. Management: See lamotrigine prescribing information for specific age-dependent dosing guidelines regarding concurrent use with a barbiturate, as well as for adjusting lamotrigine dosing if concurrent barbiturate therapy is discontinued. Consider therapy modification
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Lesinurad: Aspirin may diminish the therapeutic effect of Lesinurad. Monitor therapy
Limaprost: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Linezolid: May enhance the hypertensive effect of Sympathomimetics. Management: Reduce initial doses of sympathomimetic agents, and closely monitor for enhanced pressor response, in patients receiving linezolid. Specific dose adjustment recommendations are not presently available. Consider therapy modification
Lithium: Caffeine and Caffeine Containing Products may decrease the serum concentration of Lithium. Monitor therapy
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Loop Diuretics: Salicylates may diminish the diuretic effect of Loop Diuretics. Loop Diuretics may increase the serum concentration of Salicylates. Monitor therapy
Macimorelin: Aspirin may diminish the diagnostic effect of Macimorelin. Avoid combination
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Methotrexate: Salicylates may increase the serum concentration of Methotrexate. Salicylate doses used for prophylaxis of cardiovascular events are not likely to be of concern. Consider therapy modification
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
Methoxyflurane: Barbiturates may enhance the nephrotoxic effect of Methoxyflurane. Barbiturates may increase the metabolism of Methoxyflurane. Avoid combination
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Mianserin: May enhance the CNS depressant effect of Barbiturates. Mianserin may diminish the therapeutic effect of Barbiturates. Barbiturates may decrease the serum concentration of Mianserin. Avoid combination
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Multivitamins/Fluoride (with ADE): May enhance the antiplatelet effect of Aspirin. Aspirin may decrease the serum concentration of Multivitamins/Fluoride (with ADE). Specifically, aspirin may decrease the absorption of ascorbic acid. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): May enhance the antiplatelet effect of Aspirin. Aspirin may decrease the serum concentration of Multivitamins/Minerals (with ADEK, Folate, Iron). Specifically, aspirin may decrease absorption of ascorbic acid. Monitor therapy
Multivitamins/Minerals (with AE, No Iron): May enhance the antiplatelet effect of Aspirin. Aspirin may decrease the serum concentration of Multivitamins/Minerals (with AE, No Iron). Specifically, aspirin may decrease the absorption of ascorbic acid. Monitor therapy
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Nicorandil: Aspirin may enhance the adverse/toxic effect of Nicorandil. Specifically, the risk of gastrointestinal ulceration and hemorrhage may be increased. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective): Aspirin may enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective). Management: Concurrent use of aspirin at doses beyond cardioprotective levels is not recommended. While concurrent use of low-dose aspirin with a COX-2 inhibitor is permissable, patients should be monitored closely for signs/symptoms of GI ulceration/bleeding. Consider therapy modification
Nonsteroidal Anti-Inflammatory Agents (Nonselective): May enhance the adverse/toxic effect of Salicylates. An increased risk of bleeding may be associated with use of this combination. Nonsteroidal Anti-Inflammatory Agents (Nonselective) may diminish the cardioprotective effect of Salicylates. Salicylates may decrease the serum concentration of Nonsteroidal Anti-Inflammatory Agents (Nonselective). Consider therapy modification
Norfloxacin: May increase the serum concentration of Caffeine and Caffeine Containing Products. Monitor therapy
Obinutuzumab: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Obinutuzumab. Specifically, the risk of serious bleeding-related events may be increased. Monitor therapy
Olodaterol: Caffeine and Caffeine Containing Products may enhance the adverse/toxic effect of Olodaterol. Caffeine and Caffeine Containing Products may enhance the hypokalemic effect of Olodaterol. Monitor therapy
Omacetaxine: Aspirin may enhance the adverse/toxic effect of Omacetaxine. Specifically, the risk for bleeding-related events may be increased. Management: Avoid concurrent use of aspirin with omacetaxine in patients with a platelet count of less than 50,000/uL. Avoid combination
Omega-3 Fatty Acids: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Pentosan Polysulfate Sodium: May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Specifically, the risk of bleeding may be increased by concurrent use of these agents. Monitor therapy
Pentoxifylline: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Pipemidic Acid: May increase the serum concentration of Caffeine and Caffeine Containing Products. Monitor therapy
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Potassium Phosphate: May increase the serum concentration of Salicylates. Monitor therapy
PRALAtrexate: Salicylates may increase the serum concentration of PRALAtrexate. Salicylate doses used for prophylaxis of cardiovascular events are unlikely to be of concern. Consider therapy modification
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
Primidone: May enhance the adverse/toxic effect of Barbiturates. Primidone is converted to phenobarbital, and thus becomes additive with existing barbiturate therapy. Monitor therapy
Probenecid: Salicylates may diminish the therapeutic effect of Probenecid. Monitor therapy
Progestins (Contraceptive): Barbiturates may diminish the therapeutic effect of Progestins (Contraceptive). Contraceptive failure is possible. Management: Use of alternative, nonhormonal contraceptives is recommended. Consider therapy modification
Propacetamol: Barbiturates may increase the metabolism of Propacetamol. This may 1) diminish the desired effects of propacetamol; and 2) increase the risk of liver damage. Monitor therapy
Prostacyclin Analogues: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Pyridoxine: May increase the metabolism of Barbiturates. Apparent in high pyridoxine doses (eg, 200 mg/day) Monitor therapy
Regadenoson: Caffeine and Caffeine Containing Products may diminish the vasodilatory effect of Regadenoson. Management: Avoiding using caffeine or other methylxanthine containing products (e.g., theophylline) for at least 12 hours prior to the administration of regadenoson. Consider therapy modification
Rifamycin Derivatives: May increase the metabolism of Barbiturates. Monitor therapy
Rivaroxaban: Aspirin may enhance the adverse/toxic effect of Rivaroxaban. Specifically, the risk of bleeding may be increased. Management: Carefully consider risks and benefits of this combination and monitor closely. Consider therapy modification
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Salicylates: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Salicylates. Increased risk of bleeding may result. Monitor therapy
Salicylates: May enhance the anticoagulant effect of other Salicylates. Monitor therapy
Selective Serotonin Reuptake Inhibitors: May enhance the antiplatelet effect of Aspirin. Monitor therapy
Serotonin/Norepinephrine Reuptake Inhibitors: May enhance the antiplatelet effect of Aspirin. Monitor therapy
Sincalide: Drugs that Affect Gallbladder Function may diminish the therapeutic effect of Sincalide. Management: Consider discontinuing drugs that may affect gallbladder motility prior to the use of sincalide to stimulate gallbladder contraction. Consider therapy modification
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Solriamfetol: Sympathomimetics may enhance the hypertensive effect of Solriamfetol. Monitor therapy
Solriamfetol: CNS Stimulants may enhance the hypertensive effect of Solriamfetol. Monitor therapy
Somatostatin Acetate: May enhance the adverse/toxic effect of Barbiturates. Specifically, Somatostatin Acetate may enhance or prolong Barbiturate effects, including sedative effects. Avoid combination
Spironolactone: Aspirin may diminish the therapeutic effect of Spironolactone. Monitor therapy
Stiripentol: May increase the serum concentration of Caffeine and Caffeine Containing Products. Avoid combination
Sucroferric Oxyhydroxide: May decrease the serum concentration of Aspirin. Management: Administer aspirin at least 1 hour before administration of sucroferric oxyhydroxide. Consider therapy modification
Sulfinpyrazone: Salicylates may decrease the serum concentration of Sulfinpyrazone. Avoid combination
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Sympathomimetics: May enhance the adverse/toxic effect of other Sympathomimetics. Monitor therapy
Talniflumate: Aspirin may enhance the adverse/toxic effect of Talniflumate. Management: When possible, consider alternatives to this combination. Concurrent use is generally not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tedizolid: May enhance the hypertensive effect of Sympathomimetics. Tedizolid may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
Teniposide: Barbiturates may decrease the serum concentration of Teniposide. Management: Consider alternatives to combined treatment with barbiturates and teniposide due to the potential for decreased teniposide concentrations. If the combination cannot be avoided, monitor teniposide response closely. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Theophylline Derivatives: Barbiturates may decrease the serum concentration of Theophylline Derivatives. Exceptions: Dyphylline. Monitor therapy
Theophylline Derivatives: CYP1A2 Inhibitors (Weak) may increase the serum concentration of Theophylline Derivatives. Exceptions: Dyphylline. Monitor therapy
Thiopental: Aspirin may decrease the protein binding of Thiopental. Monitor therapy
Thrombolytic Agents: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Thrombolytic Agents. Monitor therapy
Thrombolytic Agents: Salicylates may enhance the adverse/toxic effect of Thrombolytic Agents. An increased risk of bleeding may occur. Monitor therapy
Ticagrelor: Aspirin may enhance the antiplatelet effect of Ticagrelor. Aspirin may diminish the therapeutic effect of Ticagrelor. More specifically, the benefits of ticagrelor relative to clopidogrel may be diminished in adult patients receiving daily aspirin doses greater than 100-150 mg daily. Management: Avoid daily aspirin doses greater than 100 mg in adults receiving ticagrelor. Canadian recommendations are to avoid adult daily aspirin doses greater than 150 mg. Daily low-dose aspirin (U.S.: 75-100 mg; Canada: 75-150 mg) is recommended. Consider therapy modification
Tiludronate: Aspirin may decrease the serum concentration of Tiludronate. Monitor therapy
Tipranavir: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
TiZANidine: CYP1A2 Inhibitors (Weak) may increase the serum concentration of TiZANidine. Management: Avoid these combinations when possible. If combined use is necessary, initiate tizanidine at an adult dose of 2 mg and increase in 2 to 4 mg increments based on patient response. Monitor for increased effects of tizanidine, including adverse reactions. Consider therapy modification
Tobacco (Smoked): May decrease the serum concentration of Caffeine and Caffeine Containing Products. Monitor therapy
Tricyclic Antidepressants: Barbiturates may increase the metabolism of Tricyclic Antidepressants. Consider therapy modification
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Ulipristal: Barbiturates may decrease the serum concentration of Ulipristal. Avoid combination
Urokinase: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Urokinase. Avoid combination
Valproate Products: May increase the serum concentration of Barbiturates. Barbiturates may decrease the serum concentration of Valproate Products. Monitor therapy
Valproate Products: Salicylates may increase the serum concentration of Valproate Products. Monitor therapy
Varicella Virus-Containing Vaccines: Salicylates may enhance the adverse/toxic effect of Varicella Virus-Containing Vaccines. Specifically, the risk for Reye's syndrome may increase. Avoid combination
Vitamin E (Systemic): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Salicylates may enhance the anticoagulant effect of Vitamin K Antagonists. Consider therapy modification
Vitamin K Antagonists (eg, warfarin): Barbiturates may increase the metabolism of Vitamin K Antagonists. Management: Monitor INR more closely. An anticoagulant dose increase may be needed after a barbiturate is initiated or given at an increased dose. Anticoagulant dose decreases may be needed following barbiturate discontinuation or dose reduction. Consider therapy modification
Voriconazole: Barbiturates may decrease the serum concentration of Voriconazole. Avoid combination
Zanubrutinib: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Adverse Reactions
Frequency not defined.
>10%:
Central nervous system: Dizziness, drowsiness, hangover effect
Gastrointestinal: Dyspepsia, epigastric distress, heartburn, nausea, stomach pain
1% to 10%:
Central nervous system: Confusion, depression, faintness, fatigue, headache, insomnia, nervousness, nightmares, unusual excitement
Dermatologic: Skin rash
Gastrointestinal: Constipation, gastrointestinal ulcer, vomiting
Hematologic and oncologic: Hemolytic anemia
Hypersensitivity: Anaphylactic shock
Neuromuscular & skeletal: Weakness
Respiratory: Respiratory distress
Warnings/Precautions
Concerns related to adverse effects:
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery or driving).
- Salicylate sensitivity: Patients with sensitivity to tartrazine dyes, nasal polyps, and asthma may have an increased risk of salicylate sensitivity; therapeutic doses of aspirin may cause anaphylactic shock and other severe allergic reactions.
Disease-related concerns:
- Addison disease: Use with caution in patients with Addison disease.
- Bleeding disorders: Use with caution in patients with platelet and bleeding disorders.
- Drug abuse: Use with caution in patients with a history of drug abuse or acute alcoholism; potential for drug dependency exists. Tolerance and psychological and physical dependence may occur with prolonged use.
- Gastrointestinal disease: Use with caution in patients with acute abdominal conditions, erosive gastritis, or other GI lesions, and extreme caution in patients with peptic ulcer disease.
- Head trauma: Use with extreme caution in patients with head injury, intracranial lesions, or elevated intracranial pressure (ICP); exaggerated elevation of ICP may occur.
- Hepatic impairment: Use with caution in patients with severe hepatic impairment.
- Prostatic hypertrophy/urinary stricture: Use with caution in patients with prostatic hypertrophy and/or urinary stricture.
- Renal impairment: Use with caution in patients with severe renal impairment.
- Respiratory disease: Use with caution in patients with preexisting respiratory compromise (hypoxia and/or hypercapnia), chronic obstructive pulmonary disease (COPD) or other obstructive pulmonary disease, and kyphoscoliosis or other skeletal disorder that may alter respiratory function; critical respiratory depression may occur, even at therapeutic dosages.
- Thyroid dysfunction: Use with caution in patients with thyroid dysfunction.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Debilitated patients: Use with caution in debilitated patients; there is a greater potential for critical respiratory depression, even at therapeutic dosages.
- Pediatric: Children and teenagers who have or are recovering from chickenpox or flu-like symptoms should not use this product. Changes in behavior (along with nausea and vomiting) may be an early sign of Reye syndrome; patients should be instructed to contact their health care provider if these occur.
- Surgical patients: Aspirin should be avoided (if possible) in surgical patients for 1 to 2 weeks prior to surgery, to reduce the risk of excessive bleeding.
Other warnings/precautions:
- Appropriate use: Limit butalbital use to ≤3 days per month to avoid medication overuse headache (Garza 2006); studies have found increased risk with use of ≥5 days per month (Da Silva 2014).
- Caffeine: Contains caffeine; limit the use of other caffeine-containing beverages or foods. May cause CNS and cardiovascular stimulation. Avoid in patients with symptomatic cardiac arrhythmias.
- Discontinuation of therapy: When discontinuing chronic or high-dose treatment with butalbital, or if a patient has developed chronic migraines on butalbital, discontinuing butalbital and replacing with a gradual phenobarbital taper is advised to avoid barbiturate withdrawal symptoms (ie, anxiety, diaphoresis, disturbed sleep, nausea/vomiting, restlessness, seizures, worsened headache). These patients will likely require bridge therapy with a medication to treat acute headaches and may benefit from an optimized preventative regimen (Boes 2006; Garza 2019).
- Geriatric considerations: Elderly patients may react to barbiturates with marked excitement, depression, and confusion.
Monitoring Parameters
Serial hepatic and/or renal function tests (in patients with hepatic and/or renal impairment)
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Animal reproduction studies have not been conducted with this combination. Withdrawal seizures were reported in an infant 2 days after birth following maternal use of a butalbital product during the last 2 months of pregnancy; butalbital was detected in the newborn's serum. Also refer to individual monographs for information specific to aspirin or caffeine.
Patient Education
What is this drug used for?
- It is used to treat tension headaches.
Frequently reported side effects of this drug
- Fatigue
- Dizziness
- Heart burn
- Nausea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding
- Severe abdominal pain
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.