Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Capsule, Oral:
Suprax: 400 mg
Generic: 400 mg
Suspension Reconstituted, Oral:
Suprax: 100 mg/5 mL (50 mL) [strawberry flavor]
Suprax: 200 mg/5 mL (50 mL, 75 mL); 500 mg/5 mL (10 mL, 20 mL) [contains sodium benzoate; strawberry flavor]
Generic: 100 mg/5 mL (50 mL); 200 mg/5 mL (50 mL, 75 mL)
Tablet Chewable, Oral:
Suprax: 100 mg, 200 mg [contains aspartame, fd&c red #40 aluminum lake; tutti-frutti flavor]
Pharmacology
Mechanism of Action
Inhibits bacterial cell wall synthesis by binding to one or more of the penicillin-binding proteins (PBPs); which in turn inhibits the final transpeptidation step of peptidoglycan synthesis in bacterial cell walls, thus inhibiting cell wall biosynthesis. Bacteria eventually lyse due to ongoing activity of cell wall autolytic enzymes (autolysins and murein hydrolases) while cell wall assembly is arrested.
Pharmacokinetics/Pharmacodynamics
Absorption
40% to 50%; Note: Capsule AUC reduced by ~15% and Cmax by ~25% when taken with food.
Distribution
Widely throughout the body and reaches therapeutic concentration in most tissues and body fluids, including synovial, pericardial, pleural, peritoneal; bile, sputum, and urine; bone, myocardium, gallbladder, and skin and soft tissue
Excretion
Urine (50% of absorbed dose as active drug); feces (10%)
Time to Peak
Serum: Suspension: 2 to 6 hours; Capsule: 3 to 8 hours; Delayed with food
Half-Life Elimination
Normal renal function: 3 to 4 hours; Moderate impairment (CrCl 20 to 40 mL/minute): 6.4 hours; Renal failure: Up to 11.5 hours
Protein Binding
65%
Use in Specific Populations
Special Populations: Elderly
Average AUCs at steady state in elderly patients are ~40% higher than average AUCs in healthy adults.
Use: Labeled Indications
Treatment of uncomplicated urinary tract infections (due to Escherichia coli and Proteus mirabilis), otitis media (due to Haemophilus influenzae, Moraxella catarrhalis, and Streptococcus pyogenes), pharyngitis and tonsillitis (due to Streptococcus pyogenes), acute exacerbations of chronic bronchitis (due to Streptococcus pneumoniae and Haemophilus influenzae); uncomplicated cervical/urethral gonorrhea (due to N. gonorrhoeae [penicillinase- and nonpenicillinase-producing])
Note: Due to concerns of resistance, the CDC no longer recommends use of cefixime as a first-line regimen in the treatment of uncomplicated gonorrhea in the US; ceftriaxone is the preferred cephalosporin in combination with azithromycin (CDC 2012; CDC [Workowski 2015]).
Use: Off Label
Gonococcal infection, expedited partner therapyyes
Based on the Centers for Disease Control and Prevention (CDC) sexually transmitted diseases treatment guidelines, cefixime in combination with azithromycin is an effective and recommended treatment of gonorrhea only in the following circumstances: Heterosexual partners with gonorrhea if health department partner-management strategies are impractical/unavailable and there is concern by the provider for the prompt evaluation and treatment of the partner; medication may be delivered to partner by patient, collaborating pharmacy, or disease investigation specialist as permitted by law; written materials to educate partners about their exposure to gonorrhea, importance of therapy, and when to seek clinical evaluation for adverse reactions/complications must also be provided with the medication.
Gonococcal, uncomplicated infection of the rectumyes
Based on the Centers for Disease Control and Prevention (CDC) sexually transmitted diseases treatment guidelines, cefixime, in combination with azithromycin, may be used as an alternative agent to ceftriaxone (in combination with azithromycin) for the treatment of uncomplicated gonococcal infections of the rectum only if ceftriaxone is unavailable.
Rhinosinusitis, acute bacterialcyes
Based on the Infectious Diseases Society of America (IDSA) guidelines for acute bacterial rhinosinusitis (ABRS) in children and adults, cefixime (among other cephalosporins) is effective and recommended alternative agent (in combination with clindamycin) for the treatment of ABRS.
Clinical experience suggests the utility of cefixime (in combination with clindamycin) for the treatment of ABRS Patel 2018.
Typhoid feverc
Clinical experience suggests the utility of cefixime for the treatment of this condition, as an alternative oral agent in the treatment of multidrug-resistant or quinolone-resistant strains Parry 2002. However, high failure rates have been reported Pandit 2007. Additional trials may be necessary to further define the role of cefixime for this condition.
Contraindications
Hypersensitivity to cefixime, any component of the formulation, or other cephalosporins or penicillins
Dosage and Administration
Dosing: Adult
Usual dosage range: Oral: 400 mg daily divided every 12 to 24 hours.
Gonococcal infection, uncomplicated infections of the cervix, urethra or rectum (rectum off-label use): Oral: 400 mg as a single dose in combination with oral azithromycin as a single dose (CDC [Workowski 2015]). Note: CDC no longer recommends cefixime as a first-line agent (ceftriaxone is the preferred cephalosporin in combination with azithromycin); cefixime should only be used if ceftriaxone is unavailable. In addition, cefixime is not an option for the treatment of uncomplicated gonorrhea of the pharynx due to limited efficacy; if it must be used instead of ceftriaxone, a test-of-cure follow up should be performed 14 days after treatment (CDC [Workowski 2015]). In Canada, due to increased antimicrobial resistance, the Public Health Agency of Canada recommends 800 mg as a single dose (off-label dose) for treatment of uncomplicated gonococcal infections.
Gonococcal infection, expedited partner therapy (off-label use): Oral: 400 mg as a single dose in combination with oral azithromycin (CDC [Workowski 2015]). Note: To be used only for heterosexual partners with gonorrhea if health department partner-management strategies are impractical/unavailable and there is concern by the provider for the prompt evaluation and treatment of the partner; medication may be delivered to partner by patient, collaborating pharmacy, or disease investigation specialist as permitted by law; written materials to educate partners about their exposure to gonorrhea, importance of therapy, and when to seek clinical evaluation for adverse reactions/complications must also be provided with the medication (CDC [Workowski 2015]).
Rhinosinusitis, acute bacterial (alternative agent for penicillin-allergic patients able to tolerate cephalosporins) (off-label use): Oral: 400 mg once daily for 5 to 7 days; if concern for pneumococcal resistance, add clindamycin (IDSA [Chow 2012]; Patel 2018). Note: In uncomplicated acute bacterial rhinosinusitis, initial observation and symptom management without antibiotic therapy is appropriate in most patients (AAO-HNS [Rosenfeld 2015]; Harris 2016).
Streptococcal pharyngitis (group A) (alternative agent for mild [non-anaphylactic] penicillin allergy): Oral: 400 mg once daily for 10 days (IDSA [Shulman 2012]; Pichichero 2018; manufacturer’s labeling)
Manufacturer’s labeling: Dosing in the prescribing information may not reflect current clinical practice: 200 mg twice daily
Typhoid fever (off-label use): Oral: 100 to 200 mg twice daily for 7 to 14 days (WHO 2003)
Urinary tract infection (UTI) (alternative agent): Note: Use with caution and only when recommended agents cannot be used (due to decreased efficacy of oral beta-lactams compared to other agents) (ESMID/IDSA [Gupta 2011]; Hooton 2018a).
Cystitis, acute uncomplicated: Oral: 400 mg once daily for 7 days (ESMID/IDSA [Gupta 2011]; Nicolle 2008)
UTI, complicated, including pyelonephritis: Oral: 400 mg once daily (Johnson 2018; Moustafa 2016; Sanchez 2002) for 10 to 14 days (ESMID/IDSA [Gupta 2011]; Johnson 2018). Note: Oral therapy should follow appropriate parenteral therapy. For outpatient treatment of mild infection, a single dose of a long-acting parenteral agent is acceptable (ESMID/IDSA [Gupta 2011]; Hooton 2018b).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Unless otherwise specified, any dosage form may be used.
General dosing; susceptible infection (mild to moderate): Infants, Children, and Adolescents: Oral: 8 mg/kg/day divided every 12 to 24 hours; maximum daily dose: 400 mg/day (Red Book [AAP 2015])
Febrile neutropenia (low-risk): Limited data available: Infants, Children, and Adolescents: Oral: 8 mg/kg/day in divided doses every 12 to 24 hours; in most trials, cefixime therapy was initiated as step-down therapy after 48 to 72 hours of empiric parenteral antibiotic therapy with first cefixime dose administered at the end of the last IV infusion (Klaassen 2000; Lehrnbecher 2017; Paganini 2000; Shenep 2001). Note: In clinical trials, doses were repeated if patient vomited within 2 hours.
Gonococcal infection, uncomplicated infections of the cervix, urethra, or rectum: Children ≥45 kg and Adolescents: Oral: 400 mg as a single dose in combination with oral azithromycin as a single dose (CDC [Workowski 2015]). Note: CDC no longer recommends cefixime as a first-line agent (ceftriaxone is the preferred cephalosporin in combination with azithromycin); cefixime should only be used if ceftriaxone is unavailable. In addition, cefixime is not an option for the treatment of uncomplicated gonorrhea of the pharynx due to limited efficacy; if it must be used instead of ceftriaxone, a test-of-cure follow up should be performed 14 days after treatment (CDC [Workowski 2015]). In Canada, due to increased antimicrobial resistance, the Public Health Agency of Canada recommends 800 mg as a single dose for treatment of uncomplicated gonococcal infections (Public Health Agency of Canada 2012).
Irinotecan-associated diarrhea, prophylaxis: Limited data available: Infants, Children, and Adolescents: Oral: 8 mg/kg once daily; begin 5 days before oral irinotecan therapy and continue throughout course (Wagner 2008)
Otitis media, acute: Oral suspension or chewable tablets: Infants, Children, and Adolescents: Oral: 8 mg/kg/day divided every 12 to 24 hours; maximum daily dose: 400 mg/day
Pharyngitis or tonsillitis; S. pyogenes: Note: Not preferred for treatment in IDSA Guidelines due to unnecessary broad spectrum, and lack of selectivity for antibiotic resistant flora (IDSA [Schulman 2012]); Infants, Children, and Adolescents: Oral: 8 mg/kg/day in divided doses every 12 to 24 hours for ≥10 days; maximum daily dose: 400 mg/day
Pneumonia, community-acquired (CAP); haemophilus influenza types A-F or nontypeable; mild infection or step-down therapy: Infants ≥3 months, Children, and Adolescents: Oral: 8 mg/kg/day in divided doses every 12 to 24 hours; maximum daily dose: 400 mg/day (IDSA/PIDS [Bradley 2011]) Red Book [AAP 2015])
Rhinosinusitis, acute bacterial: Infants, Children, and Adolescents: Oral: 4 mg/kg/dose every 12 hours with concomitant clindamycin for 10 to 14 days; maximum daily dose: 400 mg/day. Note: Recommended in patients with non-type I penicillin allergy, after failure of initial therapy or in patients at risk for antibiotic resistance (eg, daycare attendance, age <2 years, recent hospitalization, antibiotic use within the past month) (Chow 2012).
Typhoid fever (Salmonella typhi): Limited data available; efficacy results variable: Infants, Children and Adolescents: Oral: 7.5 to 10 mg/kg/dose every 12 hours for 7 to 14 days (Cao 1999; Girgis 1995; Stephens 2002)
Urinary tract infection; acute: Oral:
Manufacturer's labeling: Infants ≥6 months, Children, and Adolescents: 8 mg/kg/day in divided doses every 12 to 24 hours; maximum daily dose: 400 mg/day
Alternate dosing: Infants ≥2 months and Children ≤2 years: Initial: 8 mg/kg/day every 24 hours for 7 to 14 days; in patients <24 months, shorter courses (1 to 3 days) have been shown to be inferior to longer durations of therapy (AAP 2011)
Reconstitution
Powder for suspension: Refer to manufacturer’s product labeling for reconstitution instructions.
Administration
May be administered with or without food. Shake oral suspension well before use. Chewable tablets must be chewed or crushed before swallowing.
Dietary Considerations
Chewable tablets contain phenylalanine; avoid use or use with caution in patients with phenylketonuria (PKU).
Storage
Capsule, chewable tablet: Store at 20°C to 25°C (68°F to 77°F).
Powder for suspension: Prior to reconstitution, store at 20°C to 25°C (68°F to 77°F). After reconstitution, suspension may be stored for 14 days at room temperature or under refrigeration.
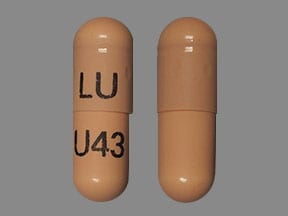
Cefixime Images
Drug Interactions
Aminoglycosides: Cephalosporins (3rd Generation) may enhance the nephrotoxic effect of Aminoglycosides. Monitor therapy
BCG (Intravesical): Antibiotics may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG Vaccine (Immunization): Antibiotics may diminish the therapeutic effect of BCG Vaccine (Immunization). Monitor therapy
Cholera Vaccine: Antibiotics may diminish the therapeutic effect of Cholera Vaccine. Management: Avoid cholera vaccine in patients receiving systemic antibiotics, and within 14 days following the use of oral or parenteral antibiotics. Avoid combination
Lactobacillus and Estriol: Antibiotics may diminish the therapeutic effect of Lactobacillus and Estriol. Monitor therapy
Probenecid: May increase the serum concentration of Cephalosporins. Monitor therapy
Sodium Picosulfate: Antibiotics may diminish the therapeutic effect of Sodium Picosulfate. Management: Consider using an alternative product for bowel cleansing prior to a colonoscopy in patients who have recently used or are concurrently using an antibiotic. Consider therapy modification
Typhoid Vaccine: Antibiotics may diminish the therapeutic effect of Typhoid Vaccine. Only the live attenuated Ty21a strain is affected. Management: Vaccination with live attenuated typhoid vaccine (Ty21a) should be avoided in patients being treated with systemic antibacterial agents. Use of this vaccine should be postponed until at least 3 days after cessation of antibacterial agents. Consider therapy modification
Vitamin K Antagonists (eg, warfarin): Cephalosporins may enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Test Interactions
Positive direct Coombs', false-positive urinary glucose test using cupric sulfate (Benedict's solution, Clinitest®, Fehling's solution), may cause false-positive serum or urine creatinine with the alkaline picrate-based Jaffé reaction for measuring creatinine; false-positive urine ketones using tests with nitroprusside (but not those using nitroferricyanide).
Adverse Reactions
>10%: Gastrointestinal: Diarrhea (16%)
2% to 10%: Gastrointestinal: Abdominal pain, nausea, dyspepsia, flatulence, loose stools
<2%: Acute renal failure, anaphylactoid reaction, anaphylaxis, angioedema, candidiasis, dizziness, drug fever, eosinophilia, erythema multiforme, facial edema, fever, headache, hepatitis, hyperbilirubinemia, increased blood urea nitrogen, increased serum creatinine, increased serum transaminases, jaundice, leukopenia, neutropenia, prolonged prothrombin time, pruritus, pseudomembranous colitis, seizure, serum sickness-like reaction, skin rash, Stevens-Johnson syndrome, thrombocytopenia, toxic epidermal necrolysis, urticaria, vaginitis, vomiting
Warnings/Precautions
Concerns related to adverse effects:
- Dermatologic reactions: Severe cutaneous reactions (eg, toxic epidermal necrolysis, Stevens-Johnson syndrome, drug rash with eosinophilia and systemic symptoms [DRESS]) have been reported. If a reaction occurs, discontinue and institute supportive therapy.
- Hemolytic anemia: Immune-mediated hemolytic anemia (including fatalities) have been reported. Monitor patient (including hematologic parameters and drug-induced antibody testing when clinically appropriate) during and for 2 to 3 weeks after therapy. If hemolytic anemia occurs during therapy, discontinue use.
- Hypersensitivity: Hypersensitivity and anaphylaxis have been reported in patients receiving beta-lactam drugs. Use caution in patients with a history of hypersensitivity to cephalosporins, penicillins, or other beta-lactams. If administered to penicillin-sensitive patients, use with caution and discontinue use if allergic reaction occurs.
- Renal failure: May cause acute renal failure including tubulointerstitial nephritis. If renal failure occurs, discontinue and initiate appropriate supportive therapy.
- Superinfection: Prolonged use may result in fungal or bacterial superinfection, including C. difficile-associated diarrhea (CDAD) and pseudomembranous colitis; CDAD has been observed >2 months postantibiotic treatment.
Disease-related concerns:
- Renal impairment: Use with caution in patients with renal impairment; may increase the risk of seizures if dosage not reduced; modify dosage.
- Gastrointestinal disease: Use with caution in patients with a history of gastrointestinal disease.
- Hemolytic anemia: Should not be administered to patients with a history of cephalosporin-associated hemolytic anemia; recurrence of hemolysis is more severe.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol derivative with caution in neonates. See manufacturer’s labeling.
- Phenylalanine: Chewable tablets contain phenylalanine; avoid use or use with caution in patients with phenylketonuria (PKU).
Monitoring Parameters
Renal function; with prolonged therapy, monitor renal and hepatic function periodically. Observe for signs and symptoms of anaphylaxis during first dose. When used as part of alternative treatment for gonococcal infection, test-of-cure 7 days after dose (CDC 2012).
Pregnancy
Pregnancy Considerations
Cefixime crosses the placenta and can be detected in the amniotic fluid (Ozyüncü 2010).
An increased risk of major birth defects or other adverse fetal or maternal outcomes has generally not been observed following use of cephalosporin antibiotics.
Patient Education
What is this drug used for?
- It is used to treat bacterial infections.
Frequently reported side effects of this drug
- Nausea
- Vomiting
- Abdominal pain
- Diarrhea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Clostridioides (formerly Clostridium) difficile-associated diarrhea like abdominal pain or cramps, severe diarrhea or watery stools, or bloody stools.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.