Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule, Oral:
Daxbia: 333 mg [DSC] [contains brilliant blue fcf (fd&c blue #1), fd&c yellow #10 (quinoline yellow), fd&c yellow #6 (sunset yellow)]
Keflex: 250 mg, 500 mg, 750 mg [contains brilliant blue fcf (fd&c blue #1), fd&c yellow #10 (quinoline yellow), fd&c yellow #6 (sunset yellow)]
Generic: 250 mg, 500 mg, 750 mg
Suspension Reconstituted, Oral:
Generic: 125 mg/5 mL (100 mL, 200 mL); 250 mg/5 mL (100 mL, 200 mL)
Tablet, Oral:
Generic: 250 mg, 500 mg
Pharmacology
Mechanism of Action
Inhibits bacterial cell wall synthesis by binding to one or more of the penicillin-binding proteins (PBPs) which in turn inhibits the final transpeptidation step of peptidoglycan synthesis in bacterial cell walls, thus inhibiting cell wall biosynthesis. Bacteria eventually lyse due to ongoing activity of cell wall autolytic enzymes (autolysins and murein hydrolases) while cell wall assembly is arrested.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid (90%); delayed in young children and may be decreased up to 50% in neonates
Distribution
Widely into most body tissues and fluids, including gallbladder, liver, kidneys, bone, sputum, bile, and pleural and synovial fluids; CSF penetration is poor
Excretion
Urine (>90% as unchanged drug) within 8 hours
Time to Peak
Serum: ~1 hour
Half-Life Elimination
Neonates: 5 hours; Children 3 to 12 months: 2.5 hours; Adults: 0.5 to 1.2 hours (prolonged with renal impairment)
Protein Binding
10% to 15%
Use: Labeled Indications
Bone infections: Treatment of bone infections caused by Staphylococcus aureus and/or Proteus mirabilis.
Genitourinary tract infections: Treatment of genitourinary tract infections, including acute prostatitis, caused by Escherichia coli, P. mirabilis, and Klebsiella pneumoniae.
Otitis media: Treatment of otitis media caused by Streptococcus pneumoniae, Haemophilus influenzae, S. aureus, Streptococcus pyogenes, and Moraxella catarrhalis.
Respiratory tract infections: Treatment of respiratory tract infections (including pharyngitis) caused by S. pneumoniae and S. pyogenes.
Skin and skin structure infections: Treatment of skin and skin structure infections caused by S. aureus and/or S. pyogenes.
Use: Off Label
Endocarditis, prophylaxisyes
Based on the American Heart Association (AHA) guidelines for the prevention of infective endocarditis, cephalexin is an effective and recommended alternative agent for prophylaxis against infective endocarditis in patients with certain cardiac conditions who are undergoing dental or respiratory tract procedures and are allergic to penicillins or ampicillin. Note: Cephalexin should not be used in patients with a history of anaphylaxis, angioedema, or urticaria with penicillins or ampicillin.
Prosthetic joint infectionyes
Based on the Infectious Diseases Society of America (IDSA) guidelines for the management of prosthetic joint infection, cephalexin is an effective and recommended agent for treatment (following pathogen-specific IV therapy in patients undergoing 1-stage exchange or debridement with retention of prosthesis) and long-term oral antimicrobial suppression of prosthetic joint infection caused by staphylococci (methicillin-susceptible) (for the first 3 to 6 months of therapy, in combination with rifampin), and an effective and recommended alternative agent when this condition is caused by beta-hemolytic streptococci or Cutibacterium species.
Contraindications
Hypersensitivity to cephalexin, other cephalosporins, or any component of the formulation
Dosage and Administration
Dosing: Adult
Usual dosage range: Oral: 250 to 1,000 mg every 6 hours or 500 mg every 12 hours (maximum: 4 g/day).
Indication-specific dosing:
Cellulitis (nonpurulent)/erysipelas, mild (alternative agent): Oral: 500 mg 4 times daily for at least 5 days (duration should be extended if not resolved/slow response) (IDSA [Stevens 2014]).
Endocarditis, prophylaxis (dental or invasive respiratory tract procedures) (alternative agent) (off-label use): Oral: 2 g 30 to 60 minutes prior to procedure. Note: AHA guidelines recommend prophylaxis only in patients undergoing invasive procedures and in whom underlying cardiac conditions may predispose to a higher risk of adverse outcomes should infection occur (AHA [Wilson 2007]).
Impetigo or ecthyma: Oral: 250 to 500 mg 4 times daily for 7 days. Note: Not an appropriate agent if MRSA is suspected or confirmed (Baddour 2019; IDSA [Stevens 2014]).
Prosthetic joint infection (off-label use): Oral: Treatment (following pathogen-specific IV therapy in patients undergoing 1-stage exchange or debridement with retention of prosthesis). Note: Duration ranges from a minimum of 3 months to indefinitely, depending on patient-specific factors (Berbari 2019):
Staphylococci (methicillin-susceptible): 500 mg every 6 to 8 hours or 1 g every 8 to 12 hours. For the first 3 to 6 months of therapy, combine with rifampin (Berbari 2019; IDSA [Osmon 2013]).
Streptococci, beta-hemolytic (alternative agent): 500 mg every 6 to 8 hours (Berbari 2019; IDSA [Osmon 2013]).
Cutibacterium spp (alternative agent): 500 mg every 6 to 8 hours (IDSA [Osmon 2013]; Kanafani 2019).
Streptococcal pharyngitis (group A) (alternative agent for mild [non-anaphylactic] penicillin allergy): Oral: 500 mg every 12 hours for 10 days (IDSA [Shulman 2012]; Pichichero 2019; manufacturer's labeling).
Urinary tract infection:
Acute uncomplicated or simple cystitis (alternative agent): Oral: 250 to 500 mg every 6 hours for 5 to 7 days (Bolding 1978; Hooton 2019a; Hooton 2019b; Johnson 1972; Menday 2000).
Bacteriuria (≥105 CFU per mL), asymptomatic, in pregnancy: Oral: 250 to 500 mg every 6 hours for 4 to 7 days (ACOG 782 2019; Hooton 2019c; IDSA [Nicolle 2019]; Pedler 1985).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
General dosing, susceptible infection (Bradley 2019; Red Book [AAP 2018]): Infants, Children, and Adolescents:
Mild to moderate infection: Oral: 25 to 50 mg/kg/day divided every 6 or 12 hours; maximum daily dose: 2,000 mg/day.
Severe infection (eg, bone and joint infections): Oral: 75 to 100 mg/kg/day divided every 6 to 8 hours; maximum daily dose: 4,000 mg/day.
Catheter (peritoneal dialysis); exit-site or tunnel infection: Limited data available: Infants, Children, and Adolescents: Oral: 10 to 20 mg/kg/day once daily or divided into 2 doses; maximum dose: 1,000 mg/dose (ISPD [Warady 2012]).
Pharyngitis/tonsillitis (group A streptococcal): Note: Use is reserved for patients with penicillin allergy (non-anaphylactic) (IDSA [Shulman 2012]).
Infants, Children, and Adolescents: Oral: 40 mg/kg/day divided every 12 hours for 10 days, maximum dose: 500 mg/dose (IDSA [Shulman 2012]).
Impetigo (staphylococcus or streptococcus): Note: Do not use if MRSA is suspected or confirmed.
Infants, Children, and Adolescents: Oral: 25 to 50 mg/kg/day divided every 6 or 8 hours; some experts suggest up to 75 mg/kg/day divided every 8 hours may be necessary in some cases; maximum daily dose: 1,000 mg/day; continue for at least 7 days, full duration dependent upon clinical response (Bradley 2019; IDSA [Stevens 2014]).
Otitis media, acute (AOM): Note: Cephalexin is not routinely recommended as an empiric treatment option (AAP [Lieberthal 2013]).
Children >1 year and Adolescents <15 years: Oral: 75 to 100 mg/kg/day divided every 6 hours; maximum dose not established for AOM; usual maximum adult dose for mild to moderate infections: 500 mg/dose and for severe infections: 1,000 mg/dose.
Skin and skin structure infections (eg, cellulitis, erysipelas): Infants, Children, and Adolescents: Oral: 25 to 50 mg/kg/day divided every 6 hours; maximum dose: 500 mg/dose; continue for at least 5 days or longer depending upon clinical response (IDSA [Stevens 2014]).
Endocarditis prophylaxis: Note: AHA guidelines (Baltimore 2015) limit the use of prophylactic antibiotics to patients at the highest risk for infective endocarditis (IE) or adverse outcomes (eg, prosthetic heart valves, patients with previous IE, unrepaired cyanotic congenital heart disease, repaired congenital heart disease with prosthetic material or device during first 6 months after procedure, repaired congenital heart disease with residual defects at the site or adjacent to site of prosthetic patch or device, and heart transplant recipients with cardiac valvulopathy):
Dental or oral procedures, or respiratory tract procedures (eg, tonsillectomy, adenoidectomy): Note: Recommended for use in patients with penicillin allergy (non-anaphylactic):
Infants, Children, and Adolescents: Oral: 50 mg/kg administered 30 to 60 minutes prior to procedure; maximum dose: 2,000 mg/dose (AHA [Wilson 2007]).
Pneumonia, community-acquired: S. aureus (methicillin-susceptible), mild infection or step-down therapy: Infants >3 months, Children, and Adolescents: Oral: 75 to 100 mg/kg/day in 3 to 4 divided doses (IDSA/PIDS [Bradley 2011]); maximum daily dose: 4,000 mg/day (Red Book [AAP 2018]).
Urinary tract infection:
Empiric therapy in febrile patients: Infants ≥2 months and Children <24 months: Oral: 50 to 100 mg/kg/day divided every 6 hours for 7 to 14 days (AAP 2011).
Treatment:
Children and Adolescents <15 years: Oral: 25 to 50 mg/kg/day divided every 6 to 12 hours for 7 to 14 days, maximum dose: 500 mg/dose; for severe infections, 50 to 100 mg/kg/day divided every 6 to 12 hours may be necessary; maximum daily dose: 4,000 mg/day.
Adolescents ≥15 years: Oral: 250 mg every 6 hours or 500 mg every 12 hours for 7 to 14 days; higher doses may be necessary for severe infections; maximum daily dose: 4,000 mg/day.
Osteoarticular infection (eg, septic arthritis, osteomyelitis); step-down therapy: Infants, Children, and Adolescents: Oral: 100 mg/kg/day divided every 6 to 8 hours; maximum daily dose: 4,000 mg/day; duration of therapy variable, dependent upon clinical response and typically extensive (weeks of therapy); compliance should be monitored (Bradley 2019; Red Book [AAP 2018]); a small (n=11) prospective, open-label pharmacokinetic study reported a median dose of 40 mg/kg/dose every 8 hours (mean age: 7 years; range: 1 to 16 years; dose range: 19 to 51 mg/kg/dose every 8 hours) maintained serum concentrations long enough to meet the pharmacokinetic/pharmacodynamic target for efficacy (T>MIC ≥ 40%) (Autmizguine 2013).
Administration
Oral: Administer without regard to food. If GI distress, take with food. Give around-the-clock to promote less variation in peak and trough serum levels.
Storage
Capsule: Store at 25°C (77°F); excursions permitted to 15ºC to 30ºC (59ºF to 86ºF).
Powder for oral suspension: Store at 20°C to 25°C (68°F to 77°F). Refrigerate after reconstitution; discard after 14 days.
Tablet: Store at 20°C to 25°C (68°F to 77°F).
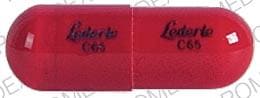
Cephalexin Images
Drug Interactions
BCG (Intravesical): Antibiotics may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG Vaccine (Immunization): Antibiotics may diminish the therapeutic effect of BCG Vaccine (Immunization). Monitor therapy
Cholera Vaccine: Antibiotics may diminish the therapeutic effect of Cholera Vaccine. Management: Avoid cholera vaccine in patients receiving systemic antibiotics, and within 14 days following the use of oral or parenteral antibiotics. Avoid combination
Lactobacillus and Estriol: Antibiotics may diminish the therapeutic effect of Lactobacillus and Estriol. Monitor therapy
MetFORMIN: Cephalexin may increase the serum concentration of MetFORMIN. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): May decrease the serum concentration of Cephalexin. Specifically, the zinc contained in many multivitamins may decrease cephalexin absorption. Management: Consider administering multivitamins at least 3 hours after cephalexin. Consider therapy modification
Multivitamins/Minerals (with AE, No Iron): May decrease the serum concentration of Cephalexin. Specifically, the zinc contained in many multivitamins may decrease cephalexin absorption. Management: Consider administering multivitamins at least 3 hours after cephalexin. Consider therapy modification
Probenecid: May increase the serum concentration of Cephalosporins. Monitor therapy
Sodium Picosulfate: Antibiotics may diminish the therapeutic effect of Sodium Picosulfate. Management: Consider using an alternative product for bowel cleansing prior to a colonoscopy in patients who have recently used or are concurrently using an antibiotic. Consider therapy modification
Sucroferric Oxyhydroxide: May decrease the serum concentration of Cephalexin. Management: Administer cephalexin at least 1 hour before administration of sucroferric oxyhydroxide. Consider therapy modification
Typhoid Vaccine: Antibiotics may diminish the therapeutic effect of Typhoid Vaccine. Only the live attenuated Ty21a strain is affected. Management: Vaccination with live attenuated typhoid vaccine (Ty21a) should be avoided in patients being treated with systemic antibacterial agents. Use of this vaccine should be postponed until at least 3 days after cessation of antibacterial agents. Consider therapy modification
Vitamin K Antagonists (eg, warfarin): Cephalosporins may enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Zinc Salts: May decrease the absorption of Cephalexin. Management: Consider administering oral zinc salts at least 3 hours after cephalexin. Exceptions: Zinc Chloride. Consider therapy modification
Test Interactions
Positive direct Coombs', false-positive urinary glucose test using cupric sulfate (Benedict's solution, Clinitest®, Fehling's solution), false-positive serum or urine creatinine with Jaffé reaction, false-positive urinary proteins and steroids
Adverse Reactions
Frequency not defined.
Central nervous system: Agitation, confusion, dizziness, fatigue, hallucination, headache
Dermatologic: Erythema multiforme (rare), genital pruritus, skin rash, Stevens-Johnson syndrome (rare), toxic epidermal necrolysis (rare), urticaria
Gastrointestinal: Abdominal pain, diarrhea, dyspepsia, gastritis, nausea (rare), pseudomembranous colitis, vomiting (rare)
Genitourinary: Genital candidiasis, vaginal discharge, vaginitis
Hematologic & oncologic: Eosinophilia, hemolytic anemia, neutropenia, thrombocytopenia
Hepatic: Cholestatic jaundice (rare), hepatitis (transient, rare), increased serum ALT, increased serum AST
Hypersensitivity: Anaphylaxis, angioedema, hypersensitivity reaction
Neuromuscular & skeletal: Arthralgia, arthritis, arthropathy
Renal: Interstitial nephritis (rare)
Warnings/Precautions
Concerns related to adverse effects:
- Hypersensitivity: Allergic reactions (eg, rash, urticaria, angioedema, anaphylaxis, erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis [TEN]) have been reported. If an allergic reaction occurs, discontinue immediately and institute appropriate treatment.
- Elevated INR: May be associated with increased INR, especially in nutritionally-deficient patients, prolonged treatment, hepatic or renal disease.
- Penicillin allergy: Use with caution in patients with a history of penicillin allergy, especially IgE-mediated reactions (eg, anaphylaxis, angioedema, urticaria).
- Seizure disorder: Use with caution in patients with a history of seizure disorder; high levels, particularly in the presence of renal impairment, may increase risk of seizures.
- Superinfection: Prolonged use may result in fungal or bacterial superinfection, including C. difficile-associated diarrhea (CDAD) and pseudomembranous colitis; CDAD has been observed >2 months post antibiotic treatment.
Disease-related concerns:
- Renal impairment: Use with caution in patients with renal impairment; modify dosage in severe impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Direct Coombs tests: Positive direct Coombs tests and acute intravascular hemolysis has been reported. If anemia develops during or after therapy, discontinue use and work up for drug-induced hemolytic anemia.
Monitoring Parameters
With prolonged therapy monitor renal, hepatic, and hematologic function periodically; monitor for signs of anaphylaxis during first dose
Pregnancy
Pregnancy Considerations
Cephalexin crosses the placenta and produces therapeutic concentrations in the fetal circulation and amniotic fluid (Creatsas 1980).
An increased risk of major birth defects or other adverse fetal or maternal outcomes has generally not been observed following use of cephalosporin antibiotics, including cephalexin, during pregnancy.
Peak concentrations in pregnant patients are similar to those in nonpregnant patients. Prolonged labor may decrease oral absorption (Griffith 1983; Paterson 1972). Cephalexin may be used in certain situations prior to vaginal delivery in females at high risk for endocarditis, and use may be considered for postcesarean delivery prophylaxis in obese females (ACOG 199 2018). Use of cephalexin may also be considered for the treatment of asymptomatic bacteriuria in pregnant women (Nicolle [IDSA 2019]).
Patient Education
What is this drug used for?
- It is used to treat bacterial infections.
Frequently reported side effects of this drug
- Nausea
- Vomiting
- Abdominal pain
- Diarrhea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Bruising
- Bleeding
- Chills
- Sore throat
- Severe loss of strength and energy
- Confusion
- Sensing things that seem real but are not
- Unable to pass urine
- Change in amount of urine passed
- Seizures
- Severe dizziness
- Severe headache
- Severe joint pain
- Vaginal pain, itching, and discharge
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes.
- Clostridioides (formerly Clostridium) difficile-associated diarrhea like abdominal pain or cramps, severe diarrhea or watery stools, or bloody stools.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.