Boxed Warning
Suicidality and antidepressant drugs:
Compared with placebo, antidepressants increase the risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults in short-term studies of major depressive disorder (MDD) and other psychiatric disorders. Anyone considering the use of clomipramine or any other antidepressant in a child, adolescent, or young adult must balance this risk with the clinical need. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared with placebo in adults older than 24 years; there was a reduction in risk with antidepressants compared with placebo in adults 65 years and older. Depression and certain other psychiatric disorders are associated with increased risk of suicide. Appropriately monitor patients of all ages who are started on antidepressant therapy and observe closely for clinical worsening, suicidality, or unusual changes in behavior. Advise families and caregivers of the need for close observation and communication with the prescriber. Clomipramine is not approved for use in pediatric patients except for patients with obsessive-compulsive disorder (OCD).
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
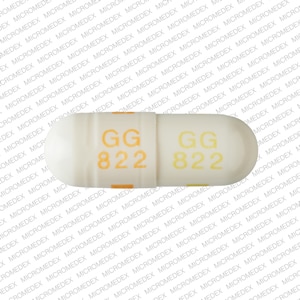
Capsule, Oral, as hydrochloride:
Anafranil: 25 mg, 50 mg, 75 mg
Generic: 25 mg, 50 mg, 75 mg
Pharmacology
Mechanism of Action
Clomipramine appears to affect serotonin uptake while its active metabolite, desmethylclomipramine, affects norepinephrine uptake
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid
Distribution
Distributes into CSF and brain, active metabolite (desmethylclomipramine) also distributes into CSF with average CSF to plasma ratio: 2.6
Metabolism
Hepatic to desmethylclomipramine (DMI; active); extensive first-pass effect; metabolites undergo glucuronide conjugation; metabolism of clomipramine and DMI may be capacity limited (ie, may display nonlinear pharmacokinetics); with multiple dosing, plasma concentrations of DMI are greater than clomipramine
Excretion
Urine (50% to 60%; 0.8% to 1.3% as parent drug and active metabolite (combined amount); feces (24% to 32%)
Onset of Action
Onset of action: 1 to 2 weeks; maximum effect: 8 to 12 weeks
Time to Peak
2 to 6 hours
Duration of Action
1 to 2 days
Half-Life Elimination
Adults (following a 150 mg dose): Clomipramine 19 to 37 hours (mean: 32 hours); DMI: 54 to 77 hours (mean: 69 hours)
Protein Binding
97%, primarily to albumin
Use: Labeled Indications
Obsessive-compulsive disorder: Treatment of obsessive-compulsive disorder
Use: Off Label
Major depressive disorderbyes
Data from randomized, double-blind studies supports the use of clomipramine in the treatment of major depressive disorder DUAG 1986, DUAG 1990, DUAG 1999, Lépine 2000, Zohar 2003. Additional trials may be necessary to further define the role of clomipramine in this condition.
According to the American Psychiatric Association treatment guidelines, clomipramine is effective and recommended for the management of major depressive disorder. Although the WFSBP treatment guidelines also recommend clomipramine, particularly for patients with severe depression or concomitant obsessive-compulsive disorder, the guidelines recommend prescribing a limited supply for severely depressed patients at risk of overdose.
Panic disorderbyes
Data from randomized, double-blind, placebo-controlled studies supports the use of clomipramine in the management of panic disorder with or without agoraphobia to decrease severity of anxiety and phobias, as well as severity and frequency of panic attacks. Additional trials may be necessary to further define the role of clomipramine in this condition.
Based on the American Psychiatric Association guidelines for the treatment of panic disorder, selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), and benzodiazepines all have roughly comparable efficacy in the treatment of panic disorder, but SSRIs are likely to have the most favorable balance of efficacy and adverse effects for most patients. Based on the Canadian Psychiatric Association guidelines for the management of anxiety disorders, TCAs like clomipramine are second-line choices for panic disorder. Based on the World Federation of the Societies of Biological Psychiatry guidelines for the management of anxiety disorders, TCAs are recommended in panic disorder in patients who have not responded to SSRIs or SNRIs.
Contraindications
Hypersensitivity to clomipramine, other tricyclic agents, or any component of the formulation; use of MAO inhibitors intended to treat psychiatric disorders (concurrently or within 14 days of discontinuing either clomipramine or the MAO inhibitor); initiation of clomipramine in a patient receiving linezolid or intravenous methylene blue; use in a patient during the acute recovery phase of MI
Canadian labeling: Additional contraindications (not in US labeling): Acute heart failure; hepatic impairment; renal impairment; history of blood dyscrasias; glaucoma
ClomiPRAMINE Images
Dosage and Administration
Dosing: Adult
Obsessive-compulsive disorder (OCD), treatment: Oral:
Initial: 25 mg daily; may gradually increase as tolerated over the first 2 weeks to ~100 mg daily in divided doses
Maintenance: After the initial titration, wait 2 to 3 weeks between dosing adjustments to assess tolerability and effectiveness. May further increase over next several weeks up to a maximum of 250 mg/day; after titration, may give as a single once daily dose at bedtime
Major depressive disorder (off-label use): Oral: Initial: 12.5 to 50 mg once daily at bedtime; titrate every 1 to 3 days in 50 mg increments to an effective dose (usual dose: 150 mg/day); doses as high as 250 mg/day have been studied (DUAG 1990; DUAG 1999; Lépine 2000; WFSBP [Bauer 2013]; Zohar 2003)
Panic disorder (off-label use): Oral: Initial: 10 to 25 mg daily; increase by 10 to 25 mg every 2 to 3 days based on efficacy and tolerability to a target dose of 50 to 150 mg/day, in 1 to 3 divided doses; guidelines recommend doses ranging from 50 to 250 mg/day (APA [Stein 2009]; Caillard 1999; Lecrubier 1997a; Lecrubier 1997b; WFSBP [Bandelow 2012]).
Discontinuation of therapy: When discontinuing antidepressant treatment that has lasted for >3 weeks, gradually taper the dose (eg, over 2 to 4 weeks) to minimize withdrawal symptoms and detect reemerging symptoms (APA 2010; WFSBP [Bauer 2015]). Reasons for a slower titration (eg, over 4 weeks) include use of a drug with a half-life <24 hours (eg, paroxetine, venlafaxine), prior history of antidepressant withdrawal symptoms, or high doses of antidepressants (APA 2010; Hirsch 2019). If intolerable withdrawal symptoms occur, resume the previously prescribed dose and/or decrease dose at a more gradual rate (Shelton 2001). Select patients (eg, those with a history of discontinuation syndrome) on long-term treatment (>6 months) may benefit from tapering over >3 months (WFSBP [Bauer 2015]). Evidence supporting ideal taper rates is limited (Shelton 2001; WFSBP [Bauer 2015]).
MAO inhibitor recommendations:
Switching to or from an MAO inhibitor intended to treat psychiatric disorders:
Allow 14 days to elapse between discontinuing an MAO inhibitor intended to treat psychiatric disorders and initiation of clomipramine.
Allow 14 days to elapse between discontinuing clomipramine and initiation of an MAO inhibitor intended to treat psychiatric disorders.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Obsessive-compulsive disorder (OCD), treatment: Children ≥10 years and Adolescents: Oral:
Initial: 25 mg daily; gradually increase as tolerated over the first 2 weeks to 3 mg/kg/day or 100 mg daily (whichever is less) in divided doses (may be divided with meals)
Maintenance: May further increase over next several weeks up to maximum daily dose: 3 mg/kg/day or 200 mg/day (whichever is less); after titration, may give as a single once daily dose at bedtime
Discontinuation of therapy: Upon discontinuation of antidepressant therapy, gradually taper the dose to minimize the incidence of withdrawal symptoms and allow for the detection of reemerging symptoms. Evidence supporting ideal taper rates is limited. APA and NICE guidelines suggest tapering therapy over at least several weeks with consideration to the half-life of the antidepressant; antidepressants with a shorter half-life may need to be tapered more conservatively. In addition for long-term treated patients, WFSBP guidelines recommend tapering over 4 to 6 months. If intolerable withdrawal symptoms occur following a dose reduction, consider resuming the previously prescribed dose and/or decrease dose at a more gradual rate (APA 2007; APA 2010; Bauer 2002; Haddad 2001; NCCMH 2010; Schatzberg 2006; Shelton 2001; Warner 2006).
MAO inhibitor recommendations:
Switching to or from an MAO inhibitor intended to treat psychiatric disorders:
Allow 14 days to elapse between discontinuing an MAO inhibitor intended to treat psychiatric disorders and initiation of clomipramine.
Allow 14 days to elapse between discontinuing clomipramine and initiation of an MAO inhibitor intended to treat psychiatric disorders.
Use with other MAO inhibitors (linezolid or IV methylene blue):
Do not initiate clomipramine in patients receiving linezolid or IV methylene blue; consider other interventions for psychiatric condition.
If urgent treatment with linezolid or IV methylene blue is required in a patient already receiving clomipramine and potential benefits outweigh potential risks, discontinue clomipramine promptly and administer linezolid or IV methylene blue. Monitor for serotonin syndrome for 2 weeks or until 24 hours after the last dose of linezolid or IV methylene blue, whichever comes first. May resume clomipramine 24 hours after the last dose of linezolid or IV methylene blue.
Administration
During titration, may divide doses and administer with meals to decrease gastrointestinal side effects. After titration, may administer total daily dose at bedtime to decrease daytime sedation.
Drug Interactions
Abiraterone Acetate: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of abiraterone with CYP2D6 substrates that have a narrow therapeutic index whenever possible. When concurrent use is not avoidable, monitor patients closely for signs/symptoms of toxicity. Consider therapy modification
Acetylcholinesterase Inhibitors: May diminish the therapeutic effect of Anticholinergic Agents. Anticholinergic Agents may diminish the therapeutic effect of Acetylcholinesterase Inhibitors. Monitor therapy
Aclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Ajmaline: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Alcohol (Ethyl): CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). Monitor therapy
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Almotriptan: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Alosetron: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Alpha-/Beta-Agonists: Tricyclic Antidepressants may enhance the vasopressor effect of Alpha-/Beta-Agonists. Management: Avoid, if possible, the use of alpha-/beta-agonists in patients receiving tricyclic antidepressants. If combined, monitor for evidence of increased pressor effects and consider reductions in initial dosages of the alpha-/beta-agonist. Consider therapy modification
Alpha1-Agonists: Tricyclic Antidepressants may enhance the therapeutic effect of Alpha1-Agonists. Tricyclic Antidepressants may diminish the therapeutic effect of Alpha1-Agonists. Monitor therapy
Alpha2-Agonists: Tricyclic Antidepressants may diminish the antihypertensive effect of Alpha2-Agonists. Management: Consider avoiding this combination. If used, monitor for decreased effects of the alpha2-agonist. Exercise great caution if discontinuing an alpha2-agonist in a patient receiving a TCA. Exceptions: Apraclonidine; Brimonidine (Ophthalmic); Lofexidine. Consider therapy modification
Alpha2-Agonists (Ophthalmic): Tricyclic Antidepressants may diminish the therapeutic effect of Alpha2-Agonists (Ophthalmic). Monitor therapy
Altretamine: May enhance the orthostatic hypotensive effect of Tricyclic Antidepressants. Monitor therapy
Amantadine: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Amifampridine: Agents With Seizure Threshold Lowering Potential may enhance the neuroexcitatory and/or seizure-potentiating effect of Amifampridine. Monitor therapy
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Amphetamines: Tricyclic Antidepressants may enhance the adverse/toxic effect of Amphetamines. Tricyclic Antidepressants may potentiate the cardiovascular effects of Amphetamines. Amphetamines may enhance the serotonergic effect of Tricyclic Antidepressants. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and increased cardiovascular effects when these agents are combined. Monitor therapy
Anticholinergic Agents: May enhance the adverse/toxic effect of other Anticholinergic Agents. Monitor therapy
Antiemetics (5HT3 Antagonists): May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Alosetron; Ondansetron; Ramosetron. Monitor therapy
Antipsychotic Agents: Serotonergic Agents (High Risk) may enhance the adverse/toxic effect of Antipsychotic Agents. Specifically, serotonergic agents may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotic Agents may enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Monitor therapy
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Aspirin: Tricyclic Antidepressants (Tertiary Amine) may enhance the antiplatelet effect of Aspirin. Monitor therapy
Asunaprevir: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Consider therapy modification
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Barbiturates: May increase the metabolism of Tricyclic Antidepressants. Consider therapy modification
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Beta2-Agonists: Tricyclic Antidepressants may enhance the adverse/toxic effect of Beta2-Agonists. Monitor therapy
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Blood Pressure Lowering Agents: May enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Botulinum Toxin-Containing Products: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Broccoli: May decrease the serum concentration of CYP1A2 Substrates (High risk with Inducers). Monitor therapy
Bromopride: May enhance the adverse/toxic effect of Tricyclic Antidepressants. Avoid combination
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
BusPIRone: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May decrease the serum concentration of CYP1A2 Substrates (High risk with Inducers). Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
CarBAMazepine: May decrease the serum concentration of ClomiPRAMINE. Monitor therapy
Chloral Betaine: May enhance the adverse/toxic effect of Anticholinergic Agents. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Cimetidine: May decrease the metabolism of Tricyclic Antidepressants. Monitor therapy
Cimetropium: Anticholinergic Agents may enhance the anticholinergic effect of Cimetropium. Avoid combination
Cinacalcet: May increase the serum concentration of Tricyclic Antidepressants. Management: Seek alternatives when possible. If these combinations are used, monitor closely for increased effects/toxicity and/or elevated serum concentrations (when testing is available) of the tricyclic antidepressant. Consider therapy modification
Citalopram: Tricyclic Antidepressants may enhance the serotonergic effect of Citalopram. Tricyclic Antidepressants may increase the serum concentration of Citalopram. Citalopram may increase the serum concentration of Tricyclic Antidepressants. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and increased TCA and citalopram concentrations/effects. Monitor therapy
CloBAZam: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
Cobicistat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Cocaine (Topical): May enhance the adverse/toxic effect of Tricyclic Antidepressants. Monitor therapy
Cyclobenzaprine: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
CYP1A2 Inducers (Moderate): May decrease the serum concentration of ClomiPRAMINE. Monitor therapy
CYP1A2 Inhibitors (Moderate): May increase the serum concentration of ClomiPRAMINE. Monitor therapy
CYP2C19 Inducers (Moderate): May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Monitor therapy
CYP2C19 Inducers (Strong): May increase the metabolism of CYP2C19 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP2D6 Inhibitors (Moderate): May decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CYP2D6 Inhibitors (Strong): May decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP2C19 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dacomitinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of dacomitinib with CYP2D6 subtrates that have a narrow therapeutic index. Consider therapy modification
Dapoxetine: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Do not use serotonergic agents (high risk) with dapoxetine or within 7 days of serotonergic agent discontinuation. Do not use dapoxetine within 14 days of monoamine oxidase inhibitor use. Dapoxetine labeling lists this combination as contraindicated. Avoid combination
Darunavir: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Desmopressin: Tricyclic Antidepressants may enhance the adverse/toxic effect of Desmopressin. Monitor therapy
Dexmethylphenidate-Methylphenidate: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Dextromethorphan: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Dronedarone: Tricyclic Antidepressants may enhance the arrhythmogenic effect of Dronedarone. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Avoid combination
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
DULoxetine: May enhance the serotonergic effect of Tricyclic Antidepressants. This could result in serotonin syndrome. DULoxetine may increase the serum concentration of Tricyclic Antidepressants. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and increased TCA concentrations and effects if these agents are combined. Monitor therapy
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Eletriptan: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Eluxadoline: Anticholinergic Agents may enhance the constipating effect of Eluxadoline. Avoid combination
Enzalutamide: May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Conversely, concentrations of active metabolites may be increased for those drugs activated by CYP2C19. Management: Concurrent use of enzalutamide with CYP2C19 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP2C19 substrate should be performed with caution and close monitoring. Consider therapy modification
Ergot Derivatives: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Nicergoline. Monitor therapy
Escitalopram: Tricyclic Antidepressants may enhance the serotonergic effect of Escitalopram. Escitalopram may increase the serum concentration of Tricyclic Antidepressants. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and increased TCA concentrations/effects if these agents are combined. Monitor therapy
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Fexinidazole [INT]: Tricyclic Antidepressants may enhance the QTc-prolonging effect of Fexinidazole [INT]. Avoid combination
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
FLUoxetine: May enhance the serotonergic effect of Tricyclic Antidepressants. FLUoxetine may increase the serum concentration of Tricyclic Antidepressants. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and increased TCA concentrations/effects if these agents are combined. Consider therapy modification
FluvoxaMINE: May enhance the serotonergic effect of Tricyclic Antidepressants. FluvoxaMINE may increase the serum concentration of Tricyclic Antidepressants. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and increased TCA concentrations/effects if these agents are combined. Monitor therapy
Gastrointestinal Agents (Prokinetic): Anticholinergic Agents may diminish the therapeutic effect of Gastrointestinal Agents (Prokinetic). Monitor therapy
Glucagon: Anticholinergic Agents may enhance the adverse/toxic effect of Glucagon. Specifically, the risk of gastrointestinal adverse effects may be increased. Monitor therapy
Glycopyrrolate (Oral Inhalation): Anticholinergic Agents may enhance the anticholinergic effect of Glycopyrrolate (Oral Inhalation). Avoid combination
Glycopyrronium (Topical): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Grapefruit Juice: May increase the serum concentration of ClomiPRAMINE. Monitor therapy
Guanethidine: Tricyclic Antidepressants may diminish the therapeutic effect of Guanethidine. Monitor therapy
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Imatinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Iobenguane Radiopharmaceutical Products: Tricyclic Antidepressants may diminish the therapeutic effect of Iobenguane Radiopharmaceutical Products. Management: Discontinue all drugs that may inhibit or interfere with catecholamine transport or uptake for at least 5 biological half-lives before iobenguane administration. Do not administer these drugs until at least 7 days after each iobenguane dose. Avoid combination
Iohexol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iohexol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iohexol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iomeprol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iomeprol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iomeprol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iopamidol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iopamidol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iopamidol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Ipratropium (Oral Inhalation): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Itopride: Anticholinergic Agents may diminish the therapeutic effect of Itopride. Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Lasmiditan: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Levosulpiride: Anticholinergic Agents may diminish the therapeutic effect of Levosulpiride. Avoid combination
Linezolid: May enhance the serotonergic effect of Tricyclic Antidepressants. This could result in serotonin syndrome. Avoid combination
Lofexidine: Tricyclic Antidepressants may diminish the therapeutic effect of Lofexidine. Management: Consider avoiding this drug combination when possible. If concurrent administration is required, monitor blood pressure carefully at the beginning of the combined therapy and when either drug is stopped. Adjust the dosage accordingly. Consider therapy modification
Lorcaserin: May enhance the serotonergic effect of Tricyclic Antidepressants. This could result in serotonin syndrome. Lorcaserin may increase the serum concentration of Tricyclic Antidepressants. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and increased TCA concentrations and effects if these agents are combined. Monitor therapy
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Lumacaftor and Ivacaftor: May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Monitor therapy
Lumefantrine: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Metaxalone: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
Methylene Blue: Tricyclic Antidepressants may enhance the serotonergic effect of Methylene Blue. This could result in serotonin syndrome. Avoid combination
Metoclopramide: May enhance the adverse/toxic effect of Tricyclic Antidepressants. Management: Seek alternatives to this combination when possible. Monitor patients receiving metoclopramide with tricyclic antidepressants for signs of extrapyramidal symptoms, neuroleptic malignant syndrome, and serotonin syndrome. Consider therapy modification
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
MetyroSINE: May enhance the adverse/toxic effect of Tricyclic Antidepressants. Monitor therapy
Mianserin: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mirabegron: Anticholinergic Agents may enhance the adverse/toxic effect of Mirabegron. Monitor therapy
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Monoamine Oxidase Inhibitors (Antidepressant): May enhance the serotonergic effect of Tricyclic Antidepressants. This could result in serotonin syndrome. Avoid combination
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nefazodone: Tricyclic Antidepressants may enhance the serotonergic effect of Nefazodone. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: Tricyclic Antidepressants may enhance the hypotensive effect of Nicorandil. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nitroglycerin: Anticholinergic Agents may decrease the absorption of Nitroglycerin. Specifically, anticholinergic agents may decrease the dissolution of sublingual nitroglycerin tablets, possibly impairing or slowing nitroglycerin absorption. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective): Tricyclic Antidepressants (Tertiary Amine) may enhance the antiplatelet effect of Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective). Monitor therapy
Nonsteroidal Anti-Inflammatory Agents (Nonselective): Tricyclic Antidepressants (Tertiary Amine) may enhance the antiplatelet effect of Nonsteroidal Anti-Inflammatory Agents (Nonselective). Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Ondansetron: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxatomide: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Oxitriptan: Serotonergic Agents (High Risk) may enhance the serotonergic effect of Oxitriptan. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Panobinostat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
PARoxetine: May enhance the serotonergic effect of Tricyclic Antidepressants. PARoxetine may increase the serum concentration of Tricyclic Antidepressants. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and increased TCA concentrations/effects if these agents are combined. Consider therapy modification
Peginterferon Alfa-2b: May decrease the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Peginterferon Alfa-2b may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Perhexiline: CYP2D6 Substrates (High risk with Inhibitors) may increase the serum concentration of Perhexiline. Perhexiline may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pitolisant: Tricyclic Antidepressants may diminish the therapeutic effect of Pitolisant. Avoid combination
Potassium Chloride: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Chloride. Management: Patients on drugs with substantial anticholinergic effects should avoid using any solid oral dosage form of potassium chloride. Avoid combination
Potassium Citrate: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Citrate. Avoid combination
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
Pramlintide: May enhance the anticholinergic effect of Anticholinergic Agents. These effects are specific to the GI tract. Consider therapy modification
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Protease Inhibitors: May increase the serum concentration of Tricyclic Antidepressants. Monitor therapy
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
QuiNIDine: Tricyclic Antidepressants may enhance the QTc-prolonging effect of QuiNIDine. QuiNIDine may increase the serum concentration of Tricyclic Antidepressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
QuiNINE: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Ramosetron: Anticholinergic Agents may enhance the constipating effect of Ramosetron. Monitor therapy
Ramosetron: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Rasagiline: May enhance the serotonergic effect of Tricyclic Antidepressants. This could result in serotonin syndrome. Avoid combination
Revefenacin: Anticholinergic Agents may enhance the anticholinergic effect of Revefenacin. Avoid combination
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Safinamide: May enhance the serotonergic effect of Tricyclic Antidepressants. This could result in serotonin syndrome. Avoid combination
Secretin: Anticholinergic Agents may diminish the therapeutic effect of Secretin. Management: Avoid concomitant use of anticholinergic agents and secretin. Discontinue anticholinergic agents at least 5 half-lives prior to administration of secretin. Consider therapy modification
Selegiline: May enhance the serotonergic effect of ClomiPRAMINE. This could result in serotonin syndrome. Avoid combination
Serotonergic Agents (High Risk, Miscellaneous): Tricyclic Antidepressants may enhance the serotonergic effect of Serotonergic Agents (High Risk, Miscellaneous). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Serotonergic Non-Opioid CNS Depressants: Tricyclic Antidepressants may enhance the CNS depressant effect of Serotonergic Non-Opioid CNS Depressants. Tricyclic Antidepressants may enhance the serotonergic effect of Serotonergic Non-Opioid CNS Depressants. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and CNS depression when these agents are combined. Monitor therapy
Serotonergic Opioids (High Risk): Tricyclic Antidepressants may enhance the CNS depressant effect of Serotonergic Opioids (High Risk). Serotonergic Opioids (High Risk) may enhance the serotonergic effect of Tricyclic Antidepressants. This could result in serotonin syndrome. Management: Consider alternatives to this drug combination. If combined, monitor for signs and symptoms of serotonin syndrome/serotonin toxicity and CNS depression. Consider therapy modification
Serotonin 5-HT1D Receptor Agonists (Triptans): May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Almotriptan; Eletriptan. Monitor therapy
Serotonin/Norepinephrine Reuptake Inhibitors: May enhance the serotonergic effect of Tricyclic Antidepressants. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes when these agents are combined. Exceptions: DULoxetine. Monitor therapy
Sertraline: May enhance the serotonergic effect of Tricyclic Antidepressants. Sertraline may increase the serum concentration of Tricyclic Antidepressants. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and increased TCA concentrations/effects if these agents are combined. Monitor therapy
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Sodium Phosphates: Tricyclic Antidepressants may enhance the adverse/toxic effect of Sodium Phosphates. Specifically, the risk of seizure and/or loss of consciousness may be increased in patients with significant sodium phosphate induced fluid/electrolyte abnormalities. Monitor therapy
St John's Wort: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. St John's Wort may decrease the serum concentration of Serotonergic Agents (High Risk). Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Sulfonylureas: Cyclic Antidepressants may enhance the hypoglycemic effect of Sulfonylureas. Monitor therapy
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Syrian Rue: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Thiazide and Thiazide-Like Diuretics: Anticholinergic Agents may increase the serum concentration of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Thyroid Products: May enhance the arrhythmogenic effect of Tricyclic Antidepressants. Thyroid Products may enhance the stimulatory effect of Tricyclic Antidepressants. Monitor therapy
Tiotropium: Anticholinergic Agents may enhance the anticholinergic effect of Tiotropium. Avoid combination
Tobacco (Smoked): May decrease the serum concentration of ClomiPRAMINE. Monitor therapy
Topiramate: Anticholinergic Agents may enhance the adverse/toxic effect of Topiramate. Monitor therapy
Tricyclic Antidepressants: May enhance the anticholinergic effect of other Tricyclic Antidepressants. Tricyclic Antidepressants may enhance the CNS depressant effect of other Tricyclic Antidepressants. Tricyclic Antidepressants may enhance the serotonergic effect of other Tricyclic Antidepressants. This could result in serotonin syndrome. Management: Monitor closely for increased TCA adverse effects, including serotonin syndrome/serotonin toxicity, CNS depression, and anticholinergic effects. Monitor therapy
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Umeclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Valproate Products: May increase the serum concentration of Tricyclic Antidepressants. Monitor therapy
Vilazodone: Tricyclic Antidepressants may enhance the serotonergic effect of Vilazodone. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) if these agents are combined. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Tricyclic Antidepressants may enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Vortioxetine: Tricyclic Antidepressants may enhance the serotonergic effect of Vortioxetine. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) if these agents are combined. Monitor therapy
Yohimbine: Tricyclic Antidepressants may increase the serum concentration of Yohimbine. Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Test Interactions
May interfere with urine detection of methadone (false-positive) (Brahm 2010)
Adverse Reactions
>10%:
Central nervous system: Dizziness (adults: 54%; children and adolescents: 41%), drowsiness (46% to 54%), headache (adults: 52%), fatigue (35% to 39%), insomnia (adults: 25%; children and adolescents: 11%), nervousness (adults: 18%; children and adolescents: 4%), myoclonus (adults: 13%; children and adolescents: 2%)
Dermatologic: Diaphoresis (adults: 29%; children and adolescents: 9%)
Endocrine & metabolic: Change in libido (adults: 21%), weight gain (adults: 18%; children and adolescents: 2%)
Gastrointestinal: Xerostomia (adults: 84%, children and adolescents: 63%), constipation (adults: 47%; children and adolescents: 22%), nausea (adults: 33%), dyspepsia (13% to 22%), anorexia (12% to 22%), diarrhea (7% to 13%), abdominal pain (adults: 11%), increased appetite (adults: 11%)
Genitourinary: Ejaculation failure (adults: 42%, children and adolescents: 6%), impotence (adults: 20%), difficulty in micturition (adults: 14%; children and adolescents: 4%)
Neuromuscular & skeletal: Tremor (adults: 54%; children and adolescents: 33%), myalgia (adults: 13%)
Ophthalmic: Visual disturbance (adults: 18%; children and adolescents: 7%)
Respiratory: Pharyngitis (adults: 14%), rhinitis (adults: 12%)
1% to 10%:
Cardiovascular: Flushing (7% to 8%), chest pain (children and adolescents: 7%), orthostatic hypotension (children, adolescents, and adults: 4% to 6%), palpitations (4%), tachycardia (children, adolescents, and adults: 2% to 4%), ECG abnormality (2%), syncope (children and adolescents: 2%)
Central nervous system: Anxiety (adults: 9%; children and adolescents: 2%), paresthesia (adults: 9%), memory impairment (7% to 9%), sleep disorder (4% to 9%), twitching (adults: 7%), depression (adults: 5%), lack of concentration (adults: 5%), pain (3% to 4%), hypertonia (2% to 4%), abnormal dreams (adults: 3%), agitation (adults: 3%), migraine (adults: 3%), psychosomatic disorder (adults: 3%), speech disturbance (adults: 3%), yawning (adults: 3%), confusion (2% to 3%), aggressive behavior (children and adolescents: 2%), chills (adults: 2%), depersonalization (2%), emotional lability (adults: 2%), irritability (children and adolescents: 2%), paresis (children and adolescents: 2%), myasthenia (1% to 2%), panic attack (1% to 2%), abnormality in thinking (≥1%), vertigo (≥1%), seizure (≤1%)
Dermatologic: Skin rash (4% to 8%), pruritus (adults: 6%), body odor (children and adolescents: 2%), dermatitis (adults: 2%), xeroderma (adults: 2%), urticaria (adults: 1%)
Endocrine & metabolic: Weight loss (children and adolescents: 7%), hot flash (2% to 5%), menstrual disease (adults: 4%), amenorrhea (adults: 1%)
Gastrointestinal: Dysgeusia (4% to 8%), vomiting (7%), flatulence (adults: 6%), aphthous stomatitis (children and adolescents: 2%), dysphagia (adults: 2%), gastrointestinal disease (adults: 2%), halitosis (children and adolescents: 2%), esophagitis (adults: 1%)
Genitourinary: Urinary retention (children and adolescents: 7%; adults: 2%), urinary tract infection (adults: 6%), urinary frequency (adults: 5%), lactation (nonpuerperal; adults: 4%), breast hypertrophy (adults: 2%), cystitis (adults: 2%), leukorrhea (adults: 2%), vaginitis (adults: 2%), mastalgia (adults: 1%)
Hematologic & oncologic: Purpuric disease (adults: 3%)
Hepatic: Increased serum alanine aminotransferase (>3 x ULN: 3%), increased serum aspartate aminotransferase (>3 x ULN: 1%)
Hypersensitivity: Hypersensitivity reaction (children and adolescents: 7%)
Neuromuscular & skeletal: Asthenia (1% to 2%)
Ophthalmic: Abnormal lacrimation (adults: 3%), anisocoria (children and adolescents: 2%), blepharospasm (children and adolescents: 2%), mydriasis (adults: 2%), ocular allergy (children and adolescents: 2%), conjunctivitis (adults: 1%)
Otic: Tinnitus (4% to 6%)
Respiratory: Bronchospasm (children and adolescents: 7%; adults: 2%), sinusitis (adults: 6%), dyspnea (children and adolescents: 2%), epistaxis (adults: 2%), laryngitis (children and adolescents: 2%)
Miscellaneous: Fever (adults: 4%)
<1%, postmarketing, and/or case reports: Abnormal electroencephalogram, abnormal sensory symptoms, accommodation disturbance, acute myocardial infarction, agranulocytosis, albuminuria, alopecia, altered sense of smell, anemia, aneurysm, angle-closure glaucoma, anticholinergic syndrome, apathy, aphasia, apraxia, ataxia, atrial flutter, blepharitis, blood in stool, bone marrow depression, bradycardia, brain disease, breast fibroadenosis, bronchitis, bundle branch block, cardiac arrhythmia, cardiac failure, catatonic-like state, cellulitis, cerebral hemorrhage, cervical dysplasia, cheilitis, chloasma, cholinergic syndrome, choreoathetosis, chromatopsia, chronic enteritis, colitis, coma, conjunctival hemorrhage, cyanosis, deafness, dehydration, delirium, delusions, dental caries, dermal ulcer, diabetes mellitus, diplopia, drug reaction with eosinophilia and systemic symptoms, duodenitis, dyskinesia, dystonia, eczema, edema, edema (oral), endometrial hyperplasia, endometriosis, enlargement of salivary glands, epididymitis, erythematous rash, exophthalmos, exostosis, extrapyramidal reaction, extrasystoles, gastric dilation, gastric ulcer, gastroesophageal reflux disease, glycosuria, goiter, gout, gynecomastia, hallucination, heart block, hematuria, hemiparesis, hemoptysis, hepatic injury (severe), hepatitis, hostility, hyperacusis, hypercholesterolemia, hyperesthesia, hyperglycemia, hyperkinetic muscle activity, hyperreflexia, hyperthermia, hyperthyroidism, hyperuricemia, hyperventilation, hypnogenic hallucinations, hypoesthesia, hypokalemia, hypokinesia, hyponatremia, hypothyroidism, hypoventilation, intestinal obstruction, irritable bowel syndrome, ischemic heart disease, keratitis, laryngismus, leukemoid reaction, leukopenia, local inflammation (uterine), lupus erythematous-like rash, lymphadenopathy, maculopapular rash, manic reaction, muscle spasm, mutism, myopathy, myositis, nephrolithiasis, neuralgia, neuropathy, nocturnal amblyopia, oculogyric crisis, oculomotor nerve paralysis, ovarian cyst, pancytopenia, paralytic ileus, paranoid ideation, peptic ulcer, periarteritis nodosa, peripheral ischemia, pharyngeal edema, phobia, photophobia, pneumonia, premature ejaculation, pseudolymphoma, psoriasis, psychosis, pyelonephritis, pyuria, rectal hemorrhage, renal cyst, schizophreniform disorder, scleritis, serotonin syndrome, SIADH, skin hypertrophy, skin photosensitivity, somnambulism, strabismus, stupor, suicidal ideation, suicidal tendencies, teeth clenching, thrombocytopenia, thrombophlebitis, tongue ulcer, torticollis, urinary incontinence, uterine hemorrhage, vaginal hemorrhage, vasospasm, ventricular tachycardia, visual field defect, voice disorder, withdrawal syndrome
Warnings/Precautions
Major psychiatric warnings:
- Suicidal thinking/behavior: [US Boxed Warning]: Antidepressants increase the risk of suicidal thinking and behavior in children, adolescents, and young adults (18 to 24 years of age) with major depressive disorder (MDD) and other psychiatric disorders; consider risk prior to prescribing. Short-term studies did not show an increased risk in patients >24 years of age and showed a decreased risk in patients ≥65 years. Closely monitor patients for clinical worsening, suicidality, or unusual changes in behavior, particularly during the initial 1 to 2 months of therapy or during periods of dosage adjustments (increases or decreases); the patient's family or caregiver should be instructed to closely observe the patient and communicate condition with health care provider. A medication guide concerning the use of antidepressants should be dispensed with each prescription. Clomipramine is FDA approved for the treatment of OCD in children ≥10 years of age.
- The possibility of a suicide attempt is inherent in major depression and may persist until remission occurs. Worsening depression and severe abrupt suicidality that are not part of the presenting symptoms may require discontinuation or modification of drug therapy. Use caution in high-risk patients during initiation of therapy.
- Prescriptions should be written for the smallest quantity consistent with good patient care. The patient's family or caregiver should be alerted to monitor patients for the emergence of suicidality and associated behaviors such as anxiety, agitation, panic attacks, insomnia, irritability, hostility, impulsivity, akathisia, hypomania, and mania; patients should be instructed to notify their health care provider if any of these symptoms or worsening depression or psychosis occur.
Concerns related to adverse effects:
- Anticholinergic effects: May cause anticholinergic effects (constipation, xerostomia, blurred vision, urinary retention); use with caution in patients with decreased GI motility, paralytic ileus, urinary retention, BPH, xerostomia, or visual problems. The degree of anticholinergic blockade produced by this agent is very high relative to other antidepressants.
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery, driving). The degree of sedation is very high relative to other antidepressants.
- Drug rash with eosinophilia and systemic syndrome (DRESS): DRESS has been reported with the use of clomipramine. If a severe, acute reaction such as DRESS occurs, discontinue clomipramine immediately.
- Fractures: Bone fractures have been associated with antidepressant treatment. Consider the possibility of a fragility fracture if an antidepressant-treated patient presents with unexplained bone pain, point tenderness, swelling, or bruising (Rabenda 2013; Rizzoli 2012).
- Hematologic effects: TCAs may rarely cause bone marrow suppression; monitor for any signs of infection and obtain CBC if symptoms (eg, fever, sore throat) evident.
- Ocular effects: May cause mild pupillary dilation, which, in susceptible individuals, can lead to an episode of narrow-angle glaucoma. Consider evaluating patients who have not had an iridectomy for narrow-angle glaucoma risk factors.
- Orthostatic hypotension: May cause orthostatic hypotension (risk is moderate relative to other antidepressants); use with caution in patients at risk of this effect or in those who would not tolerate transient hypotensive episodes (cerebrovascular disease, cardiovascular disease, hypovolemia, or concurrent medication use that may predispose to hypotension/bradycardia).
- Seizures: May cause seizures (relationship to dose and/or duration of therapy); do not exceed maximum doses. Use with caution in patients with a previous seizure disorder or condition predisposing to seizures such as brain damage, alcoholism, or concurrent therapy with other drugs that lower the seizure threshold.
- Serotonin syndrome: Potentially life-threatening serotonin syndrome has occurred with serotonergic agents (eg, SSRIs, SNRIs), particularly when used in combination with other serotonergic agents (eg, triptans, TCAs, fentanyl, lithium, tramadol, buspirone, St. John's wort, tryptophan) or agents that impair metabolism of serotonin (eg, MAO inhibitors intended to treat psychiatric disorders, other MAO inhibitors [ie, linezolid and IV methylene blue]). Monitor patients closely for signs of serotonin syndrome such as mental status changes (eg, agitation, hallucinations, delirium, coma); autonomic instability (eg, tachycardia, labile blood pressure, diaphoresis); neuromuscular changes (eg, tremor, rigidity, myoclonus); GI symptoms (eg, nausea, vomiting, diarrhea); and/or seizures. Discontinue treatment (and any concomitant serotonergic agent) immediately if signs/symptoms arise.
- Sexual dysfunction: Has been associated with a high incidence of male sexual dysfunction.
- SIADH and hyponatremia: Antidepressant agents have been associated with the development of SIADH and hyponatremia, predominately in elderly patients. Other risk factors include volume depletion, concurrent use of diuretics, female gender, low body weight, and severe physical illness. TCAs have a lower risk for hyponatremia in comparison to SSRIs (De Picker 2014).
- Weight gain: May cause weight gain.
Disease-related concerns:
- Adrenal tumor: Use with caution in patients with tumors of the adrenal medulla (eg, pheochromocytoma, neuroblastoma); may cause hypertensive crises.
- Cardiovascular disease: Use with caution in patients with a history of cardiovascular disease (including previous MI, stroke, tachycardia, or conduction abnormalities); the risk of conduction abnormalities with this agent is high relative to other antidepressants. In a scientific statement from the American Heart Association, clomipramine has been determined to be an agent that may exacerbate underlying myocardial dysfunction (magnitude: moderate) (AHA [Page 2016]).
- Hepatic impairment: Use with caution in patients with hepatic impairment; increases in ALT/AST have occurred, including rare reports of severe hepatic injury (some fatal); monitor hepatic transaminases periodically in patients with hepatic impairment.
- Mania/hypomania: May worsen psychosis in some patients or precipitate a shift to mania or hypomania in patients with bipolar disorder. Monotherapy in patients with bipolar disorder should be avoided. Patients presenting with depressive symptoms should be screened for bipolar disorder. Clomipramine is not FDA approved for the treatment of bipolar depression.
- Renal impairment: Use with caution in patients with renal impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Discontinuation syndrome: Abrupt discontinuation or interruption of antidepressant therapy has been associated with a discontinuation syndrome. Symptoms arising may vary with antidepressant however commonly include nausea, vomiting, diarrhea, headaches, light-headedness, dizziness, diminished appetite, sweating, chills, tremors, paresthesias, fatigue, somnolence, and sleep disturbances (eg, vivid dreams, insomnia). Less common symptoms include electric shock-like sensations, cardiac arrhythmias (more common with tricyclic antidepressants), myalgias, parkinsonism, arthralgias, and balance difficulties. Psychological symptoms may also emerge such as agitation, anxiety, akathisia, panic attacks, irritability, aggressiveness, worsening of mood, dysphoria, mood lability, hyperactivity, mania/hypomania, depersonalization, decreased concentration, slowed thinking, confusion, and memory or concentration difficulties. Greater risks for developing a discontinuation syndrome have been associated with antidepressants with shorter half-lives, longer durations of treatment, and abrupt discontinuation. For antidepressants of short or intermediate half-lives, symptoms may emerge within 2 to 5 days after treatment discontinuation and last 7 to 14 days (APA 2010; Fava 2006; Haddad 2001; Shelton 2001; Warner 2006).
- Electroconvulsive therapy: May increase the risks associated with electroconvulsive therapy; consider discontinuing, when possible, prior to ECT treatment.
- Surgery: Recommended by the manufacturer to discontinue prior to elective surgery; risks exist for drug interactions with anesthesia and for cardiac arrhythmias. However, definitive drug interactions have not been widely reported in the literature and continuation of tricyclic antidepressants is generally recommended as long as precautions are taken to reduce the significance of any adverse events that may occur. Norepinephrine should be considered the vasopressor of choice for TCA-related hypotension (Pass 2004). Therapy should not be abruptly discontinued in patients receiving high doses for prolonged periods.
Monitoring Parameters
Serum sodium in at-risk populations (as clinically indicated) (De Picker 2014); pulse rate and blood pressure prior to and during therapy; ECG/cardiac status in older adults and patients with cardiac disease; suicidal ideation (especially at the beginning of therapy, after initiation, or when doses are increased or decreased); signs/symptoms of serotonin syndrome; hepatic transaminases (periodically during therapy in patients with preexisting hepatic impairment)
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Adverse events were observed in some animal reproduction studies. Clomipramine and its metabolite desmethylclomipramine cross the placenta and can be detected in cord blood and neonatal serum at birth (Loughhead 2006; ter Horst 2012). Data from five newborns found the half-life for clomipramine in the neonate to be 42 ± 16 hours following in utero exposure. Serum concentrations were not found to correlate to withdrawal symptoms (ter Horst 2012). Withdrawal symptoms (including jitteriness, tremor, and seizures) have been observed in neonates whose mothers took clomipramine up to delivery.
The ACOG recommends that therapy for depression during pregnancy be individualized; treatment should incorporate the clinical expertise of the mental health clinician, obstetrician, primary health care provider, and pediatrician (ACOG 2008). According to the American Psychiatric Association (APA), the risks of medication treatment should be weighed against other treatment options and untreated depression. For women who discontinue antidepressant medications during pregnancy and who may be at high risk for postpartum depression, the medications can be restarted following delivery (APA 2010). Treatment algorithms have been developed by the ACOG and the APA for the management of depression in women prior to conception and during pregnancy (Yonkers 2009).
Data collection to monitor pregnancy and infant outcomes following exposure to clomipramine is ongoing. Pregnant women exposed to antidepressants during pregnancy are encouraged to enroll in the National Pregnancy Registry for Antidepressants (NPRAD). Women 18 to 45 years of age or their health care providers may contact the registry by calling 844-405-6185. Enrollment should be done as early in pregnancy as possible.
Patient Education
What is this drug used for?
- It is used to treat obsessive-compulsive problems.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Dry mouth
- Constipation
- Diarrhea
- Abdominal pain
- Nausea
- Vomiting
- Passing gas
- Anxiety
- Fatigue
- Increased hunger
- Lack of appetite
- Tremors
- Weight gain
- Weight loss
- Back pain
- Sweating a lot
- Headache
- Trouble sleeping
- Flushing
- Stuffy nose
- Sore throat
- Cough
- Change in taste
- Muscle pain
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Low sodium like headache, difficulty focusing, trouble with memory, confusion, weakness, seizures, or change in balance.
- Depression like thoughts of suicide, anxiety, emotional instability, or confusion.
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Urinary tract infection like blood in the urine, burning or painful urination, passing a lot of urine, fever, lower abdominal pain, or pelvic pain.
- Infection
- Agitation
- Irritability
- Panic attacks
- Behavioral changes
- Passing out
- Severe dizziness
- Menstrual pain
- Sensing things that seem real but are not
- Severe loss of strength and energy
- Twitching
- Unable to pass urine
- Seizures
- Chest pain
- Fast heartbeat
- Abnormal heartbeat
- Bruising
- Bleeding
- Burning or numbness feeling
- Sexual dysfunction
- Sex drive changes
- Swollen glands
- Noise or ringing in the ears
- Vision changes
- Eye pain
- Eye swelling
- Eye redness
- Serotonin syndrome like dizziness, severe headache, agitation, sensing things that seem real but are not, fast heartbeat, abnormal heartbeat, flushing, tremors, sweating a lot, change in balance, severe nausea, or severe diarrhea.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.