Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution, Injection:
Lanoxin: 0.25 mg/mL (2 mL) [contains alcohol, usp, propylene glycol]
Lanoxin Pediatric: 0.1 mg/mL (1 mL) [contains alcohol, usp, propylene glycol]
Generic: 0.25 mg/mL (2 mL)
Solution, Oral:
Generic: 0.05 mg/mL (60 mL)
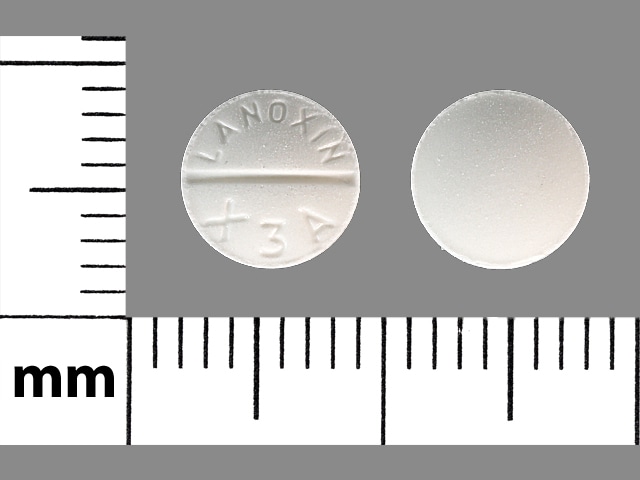
Tablet, Oral:
Digitek: 125 mcg [scored; contains fd&c yellow #10 aluminum lake]
Digitek: 250 mcg [scored]
Digox: 125 mcg [scored; contains fd&c yellow #10 aluminum lake]
Digox: 250 mcg [scored]
Lanoxin: 62.5 mcg [contains corn starch, fd&c yellow #6 (sunset yellow)]
Lanoxin: 125 mcg [scored; contains fd&c yellow #10 (quinoline yellow), fd&c yellow #6 (sunset yellow)]
Lanoxin: 187.5 mcg
Lanoxin: 250 mcg [scored]
Generic: 125 mcg, 250 mcg
Pharmacology
Mechanism of Action
Heart failure: Inhibition of the sodium/potassium ATPase pump in myocardial cells results in a transient increase of intracellular sodium, which in turn promotes calcium influx via the sodium-calcium exchange pump leading to increased contractility. May improve baroreflex sensitivity (Gheorghiade 1991).
Supraventricular arrhythmias: Direct suppression of the AV node conduction to increase effective refractory period and decrease conduction velocity - positive inotropic effect, enhanced vagal tone, and decreased ventricular rate to fast atrial arrhythmias. Atrial fibrillation may decrease sensitivity and increase tolerance to higher serum digoxin concentrations.
Pharmacokinetics/Pharmacodynamics
Absorption
By passive nonsaturable diffusion in the upper small intestine; food may delay, but does not affect extent of absorption
Distribution
Normal renal function: 6 to 7 L/kg
Vd: Extensive to peripheral tissues, with a distinct distribution phase which lasts 6 to 8 hours; concentrates in heart, liver, kidney, skeletal muscle, and intestines. Heart/serum concentration is 70:1. Pharmacologic effects are delayed and do not correlate well with serum concentrations during distribution phase.
Hyperthyroidism: Increased Vd
Hyperkalemia, hyponatremia: Decreased digoxin distribution to heart and muscle
Hypokalemia: Increased digoxin distribution to heart and muscles
Concomitant quinidine therapy: Decreased Vd
Chronic renal failure: 4 to 6 L/kg
Decreased sodium/potassium ATPase activity - decreased tissue binding
Neonates, full-term: 7.5 to 10 L/kg
Children: 16 L/kg
Adults: 7 L/kg, decreased with renal disease
Metabolism
Via sequential sugar hydrolysis in the stomach or by reduction of lactone ring by intestinal bacteria (in ~10% of population, gut bacteria may metabolize up to 40% of digoxin dose); once absorbed, only ~16% is metabolized to 3-beta-digoxigenin, 3-keto-digoxigenin, and glucuronide and sulfate conjugates; metabolites may contribute to therapeutic and toxic effects of digoxin; metabolism is reduced with decompensated HF
Excretion
Urine (50% to 70% as unchanged drug)
Onset of Action
Heart rate control: Oral: 1 to 2 hours; IV: 5 to 60 minutes
Peak effect: Heart rate control: Oral: 2 to 8 hours; IV: 1 to 6 hours; Note: In patients with atrial fibrillation, median time to ventricular rate control in one study was 6 hours (range: 3 to 15 hours) (Siu 2009)
Time to Peak
Serum: Oral: 1 to 3 hours
Duration of Action
Adults: 3 to 4 days
Half-Life Elimination
Age, renal and cardiac function dependent:
Neonates: Premature: 61 to 170 hours; Full-term: 35 to 45 hours
Infants: 18 to 25 hours
Children: 18 to 36 hours
Adults: 36 to 48 hours
Adults, anephric: 3.5 to 5 days
Parent drug: 38 hours; Metabolites: Digoxigenin: 4 hours; Monodigitoxoside: 3 to 12 hours
Protein Binding
~25%; in uremic patients, digoxin is displaced from plasma protein binding sites
Use in Specific Populations
Special Populations: Renal Function Impairment
Clearance correlates with CrCl. Half-life is 3.5 to 5 days in anuric patients.
Use: Labeled Indications
Atrial fibrillation or atrial flutter, rate control: Control of ventricular response rate in adults with chronic atrial fibrillation.
Heart failure with reduced ejection fraction (HFrEF): Treatment of mild to moderate (or stage C as recommended by the ACCF/AHA) heart failure in adults; to increase myocardial contractility in pediatric patients with heart failure
Use: Off Label
Fetal supraventricular tachyarrhythmia, sustained (maternal administration for transplacental transfer to the fetus)cyes
Data from retrospective studies of fetuses with tachycardia with or without hydrops suggest that digoxin via maternal administration may be beneficial for the treatment of fetal tachycardia Azancot-Benisty 1992, Jaeggi 2011, Simpson 1998, van Engelen 1994.
Based on the American Heart Association Scientific Statement for the Diagnosis and Treatment of Fetal Cardiac Disease, digoxin may be considered for the in utero management of fetal supraventricular tachycardia (SVT) or atrial flutter with hydrops or ventricular dysfunction. Digoxin may also be considered for SVT without hydrops or ventricular dysfunction if heart rate is ≥200 bpm, atrial flutter, or other rare tachycardias with an average heart rate of ≥200 bpm AHA [Donofrio 2014].
Supraventricular tachycardia (eg, atrioventricular nodal reentrant tachycardia), rate controlyes
Based on the American College of Cardiology/American Heart Association/Heart Rhythm Society guideline for the management of adult patients with supraventricular tachycardia, digoxin may be a reasonable alternative therapeutic option for the ongoing management of symptomatic SVT (eg, atrioventricular nodal reentrant tachycardia [AVNRT]) if preferred therapies fail in patients who are not candidates for, or prefer not to undergo, catheter ablation.
Contraindications
Hypersensitivity to digoxin, other forms of digitalis, or any component of the formulation; ventricular fibrillation
Dosage and Administration
Dosing: Adult
Note: When changing from oral (tablets or liquid) to IV therapy, dosage may be reduced by 20% to 25%. Periodically monitor digoxin concentrations as appropriate for the condition being treated, especially if renal impairment occurs. Toxicity may occur even at therapeutic concentrations in some settings (eg, hypokalemia).
Atrial fibrillation or atrial flutter, rate control (alternative agent): Note: Some experts reserve digoxin for patients whose rate has not adequately been controlled with other agents or interventions (Ganz 2018; Giardina 2018). Additionally, digoxin is not effective for rate control during high-adrenergic states (eg, exercise); a beta-blocker is preferred. Do not use in patients with preexcitation associated with an accessory pathway, as this can lead to ventricular arrhythmias (AHA/ACC/HRS [January 2014]).
Total digitalizing dose (TDD): Initial:
IV: 0.25 to 0.5 mg over several minutes, with repeat doses of 0.25 mg every 6 hours to a maximum of 1.5 mg over 24 hours (AHA/ACC/HRS [January 2014]; Giardina 2018)
or
IV: A total of 8 to 12 mcg/kg (use lean body weight) (not to exceed 0.75 to 1.5 mg) administered by giving 50% of TDD over 5 minutes and the remaining 50% as 2 doses of 25% of TDD at 4- to 8-hour intervals after the initial dose (ACLS [Neumar 2010]).
Note: follow either of these TDD regimens with an oral maintenance regimen (Giardina 2018).
Maintenance dose: Oral: 0.125 to 0.25 mg once daily (AHA/ACC/HRS [January 2014]).
Fetal supraventricular tachyarrhythmia, sustained (maternal administration for transplacental transfer to the fetus) (off-label use): Note: These patients should be managed by a highly experienced fetal arrhythmia team. Due to decreased placental transfer, maternal administration of digoxin may be less effective when fetal hydrops is present (AHA [Donofrio 2014]; Alsaied 2017; Jaeggi 2011; Levine 2019). The lowest effective dose should be used to avoid maternal adverse events (Moatassim 2018). Prior to use, evaluate appropriateness of therapy to the mother (eg, maternal electrolytes, renal function, ECG).
Maternal dose:
Loading dose (may be given oral or IV):
IV: 1.2 to 1.5 mg over 24 hours given in divided doses every 8 hours; follow with oral maintenance regimen (AHA [Donofrio 2014]). Some experts do not recommend IV administration (Levine 2019).
Oral: 1 to 2 mg given over 24 to 48 hours in divided doses (eg, 0.5 mg followed by 0.25 mg, then 0.25 mg over the first 18 to 24 hours with subsequent additional doses as needed to achieve target levels); follow with an oral maintenance regimen (Alsaied 2017; Jaeggi 2011; Levine 2019).
Maintenance dose: Oral: 0.375 mg to 0.75 mg per day given in divided doses every 8 to 12 hours. Adjust dose to maintain a target maternal blood level between 0.7 and 2 ng/mL (AHA [Donofrio 2014]). Some experts recommend dividing into 3 times daily dosing to ensure adequate drug levels (Levine 2019).
Heart failure with reduced ejection fraction (HFrEF): Note: Some experts reserve use of digoxin for patients with persistent New York Heart Association functional class III or IV symptoms despite optimal guideline-directed medical therapy (ACCF/AHA [Yancy 2013]; Colucci 2019).
Maintenance dose (loading dose not recommended): Oral: 0.125 to 0.25 mg once daily; higher daily doses are rarely necessary. If patient is >70 years of age, has impaired renal function, or has a low lean body mass, low doses (eg, 0.125 mg daily or every other day) should be used initially (ACCF/AHA [Yancy 2013]). A dosing nomogram is also available based on lean body weight and CrCl (DiDomenico 2014).
Supraventricular tachycardia (eg, atrioventricular nodal reentrant tachycardia [AVNRT]), rate control (alternative agent) (off-label use): Note: Some experts reserve digoxin for supraventricular tachycardia that is not terminated or controlled by other agents or maneuvers (Knight 2018; Spragg 2018).
Total digitalizing dose: Initial:
Oral: 0.5 mg loading dose, with additional 0.125 to 0.25 mg doses administered at 6- to 8-hour intervals until evidence of adequate effect (maximum total dose over 24 hours: 8 to 12 mcg/kg [use lean body weight], not to exceed 0.75 to 1.5 mg) (ACC/AHA/HRS [Page 2015]; Giardina 2018).
IV: 0.25 to 0.5 mg bolus; may repeat 0.25 mg administered at 6- to 8-hour intervals until evidence of adequate effect (maximum total dose over 24 hours: 8 to 12 mcg/kg [use lean body weight], not to exceed 0.75 to 1.5 mg) (ACC/AHA/HRS [Page 2015]; Giardina 2018).
Maintenance dose: Oral: 0.125 to 0.25 mg once daily (ACC/AHA/HRS [Page 2015]).
Dosing: Geriatric
Dose is based on assessment of lean body mass and renal function. Elderly patients with low lean body mass may experience higher digoxin concentrations due to reduced volume of distribution (Cheng 2010). Decrease dose in patients with decreased renal function (see Dosing in Renal Impairment).
Atrial fibrillation: Avoid as first-line therapy; if used, do not exceed 0.125 mg/day in patients ≥65 years (Beers Criteria [AGS 2019]).
Heart failure: If patient is >70 years of age, low doses (eg, 0.125 mg daily or every other day) should be used (ACCF/AHA [Yancy 2013]). Avoid as first-line therapy; if used, do not exceed 0.125 mg/day in patients ≥65 years (Beers Criteria [AGS 2019]).
Dosing: Pediatric
Note: Dosage must be individualized due to substantial individual variation and must take into account renal function. Doses should be based on lean body weight. When changing from oral solution to IV therapy, dosage should be reduced by 20% to 25%.
Heart failure: Injection, Oral: Infants, Children, and Adolescents: The dosage tables below list dosage recommendations for normal renal function and are based upon average patient response; lower doses are needed for patients with renal impairment.
Digitalizing dose, initial regimen (optional): Total digitalizing dose should be divided (see below); digitalizing dose (loading dose) may not be necessary; consider use if rapid titration is desired. To avoid toxicity, consider doses at lower end of the recommended range; dosage should be individualized based on patient response (eg, clinical response, serum drug levels).
|
Age |
Total Digitalizing Dose Administer in 3 divided dosesB (mcg/kg) |
||
|---|---|---|---|
|
Oral Solution |
Tablets |
IVC |
|
|
ABased on lean body weight and normal renal function for age. |
|||
|
BDo not give full total digitalizing dose (TDD) at once. Give one-half of the TDD for the initial dose, then give one-quarter of the TDD for each of 2 subsequent doses at 6- to 8-hour intervals; prior to additional doses, clinical response should be fully evaluated (eg, ECG). |
|||
|
CMay also be administered by IM; however, not recommended. |
|||
|
1 to 24 months |
35 to 60 |
− |
30 to 50 |
|
2 to 5 years |
30 to 45 |
− |
25 to 35 |
|
5 to 10 years |
20 to 35 |
20 to 45 |
15 to 30 |
|
>10 years |
10 to 15 |
10 to 15 |
8 to 12 |
Table has been converted to the following text:
Dosage Recommendations for Digitalizing Dose (Optional): Total Digitalizing Dose (based on lean body weight and normal renal function for age): Administer in 3 divided doses. Do not give full total digitalizing dose (TDD) at once. Give one-half of the TDD for the initial dose, then give one-quarter of the TDD for each of 2 subsequent doses at 6- to 8-hour intervals; prior to additional doses, clinical response should be fully evaluated (eg, ECG). May also be administered IM; however, not recommended.
1 to 24 months: Total digitalizing dose: Oral solution: 35 to 60 mcg/kg; IV: 30 to 50 mcg/kg
2 to 5 years: Total digitalizing dose: Oral solution: 30 to 45 mcg/kg; IV: 25 to 35 mcg/kg
5 to 10 years: Total digitalizing dose: Oral solution: 20 to 35 mcg/kg; Tablets: 20 to 45 mcg/kg; IV: 15 to 30 mcg/kg
>10 years: Total digitalizing dose: Oral solution: 10 to 15 mcg/kg; Tablets: 10 to 15 mcg/kg; IV: 8 to 12 mcg/kg
|
Age |
Daily Maintenance Dose If ≤10 years, administer in equal divided doses twice daily If >10 years, administer once daily (mcg/kg/day) |
||
|---|---|---|---|
|
Oral Solution |
Tablets |
IVC,D |
|
|
ADosing reflects clinical practice and in some cases, varies from manufacturer labeling (Bakir 1994; Bendayan 1983; Latifi 2000; Park 1986). |
|||
|
BBased on lean body weight and normal renal function for age. Decrease maintenance dose in patients with decreased renal function. |
|||
|
CMay also be administered by IM; however, not recommended. |
|||
|
DDaily maintenance IV dose is typically 20% to 30% of total digitalizing IV dose in pediatric patients ≤24 months and 25% to 35% in older pediatric patients. |
|||
|
1 to 24 months |
10 to 15 |
− |
9 to 15 |
|
2 to 5 years |
8 to 10 |
− |
6 to 9 |
|
5 to 10 years |
5 to 10 |
6 to 12 |
4 to 8 |
|
>10 years |
2.5 to 5 |
2.5 to 5 |
2 to 3 |
Table has been converted to the following text:
Maintenance Dosage Recommendations for Digoxin: Daily Maintenance Dose (based on lean body weight and normal renal function for age; decrease maintenance dose in patients with decreased renal function); dosing reflects clinical practice and in some cases, varies from manufacturer labeling (Bakir 1994; Bendayan 1983; Latifi 2000; Park 1986). If ≤10 years, administer in divided doses twice daily; if >10 years, administer once daily. May also be administered by IM; however, not recommended. Daily maintenance IV dose is typically 20% to 30% of total digitalizing IV dose in pediatric patients ≤24 months and 25% to 35% in older pediatric patients.
1 to 24 months: Oral solution: 10 to 15 mcg/kg/day; IV: 9 to 15 mcg/kg/day
2 to 5 years: Oral solution: 8 to 10 mcg/kg/day; IV: 6 to 9 mcg/kg/day
5 to 10 years: Oral solution: 5 to 10 mcg/kg/day; Tablets: 6 to 12 mcg/kg/day; IV: 4 to 8 mcg/kg/day
>10 years: Oral solution: 2.5 to 5 mcg/kg/day; Tablets: 2.5 to 5 mcg/kg/day; IV: 2 to 3 mcg/kg/day
Tachyarrhythmias, treatment: Limited data available (Escudero 2012): Injection, Oral: Infants, Children, and Adolescents:
Initial (digitalizing dose):
IV: 10 to 12 mcg/kg/dose every 8 hours for 3 doses
Oral: 13 to 17 mcg/kg/dose every 8 hours for 3 doses
Maintenance: Oral: 8 to 10 mcg/kg/day divided once or twice daily (Escudero 2012); use twice daily dosing in infants and young children (O'Sullivan 1995)
Reconstitution
IM: No dilution required.
IV: May be administered undiluted or diluted fourfold in D5W, NS, or SWFI for direct injection. Less than fourfold dilution may lead to drug precipitation.
Administration
IM: IV route preferred. If IM injection necessary, administer by deep injection followed by massage at the injection site. Inject no more than 2 mL per injection site. May cause intense pain.
IV: May be administered undiluted or diluted. Inject slowly over ≥5 minutes.
When used for the management of fetal tachycardia (off-label use), IV or oral doses are administered to the mother for transplacental transfer to the fetus (AHA [Donofrio 2014]).
Vesicant; ensure proper needle or catheter placement prior to and during administration; avoid extravasation.
Extravasation management: If extravasation occurs, stop IV administration immediately and disconnect (leave cannula/needle in place); gently aspirate extravasated solution (do NOT flush the line); remove needle/cannula; elevate extremity.
Dietary Considerations
Maintain adequate amounts of potassium in diet to decrease risk of hypokalemia (hypokalemia may increase risk of digoxin toxicity).
Storage
Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect elixir, injection, and tablets from light.
Digoxin Images
Drug Interactions
5-Aminosalicylic Acid Derivatives: May decrease the serum concentration of Cardiac Glycosides. Monitor therapy
Acarbose: May decrease the serum concentration of Digoxin. Monitor therapy
Adenosine: Digoxin may enhance the adverse/toxic effect of Adenosine. Monitor therapy
Aminoglycosides: May decrease the serum concentration of Cardiac Glycosides. This effect has only been demonstrated with oral aminoglycoside administration. Exceptions: Amikacin (Systemic); Arbekacin; Isepamicin; Plazomicin; Streptomycin; Tobramycin (Systemic). Monitor therapy
Aminoquinolines (Antimalarial): May increase the serum concentration of Cardiac Glycosides. Monitor therapy
Amiodarone: May increase the serum concentration of Cardiac Glycosides. Management: Reduce the dose of cardiac glycosides by 30% to 50% or reduce the frequency of administration when initiating concomitant amiodarone therapy. Monitor for increased serum concentrations and toxic effects of cardiac glycosides. Consider therapy modification
Amphotericin B: May enhance the adverse/toxic effect of Cardiac Glycosides. Monitor therapy
Anagliptin: May increase the serum concentration of Digoxin. Monitor therapy
Anthracyclines: Cardiac Glycosides may diminish the cardiotoxic effect of Anthracyclines. Anthracyclines may decrease the serum concentration of Cardiac Glycosides. The effects of liposomal formulations may be unique from those of the free drug, as liposomal formulation have unique drug disposition and toxicity profiles, and liposomes themselves may alter digoxin absorption/distribution. Monitor therapy
Antithyroid Agents: May increase the serum concentration of Cardiac Glycosides. Monitor therapy
Asunaprevir: May increase the serum concentration of Digoxin. Monitor therapy
AtorvaSTATin: May increase the serum concentration of Digoxin. Monitor therapy
Barnidipine: May enhance the adverse/toxic effect of Digoxin. Monitor therapy
Benidipine: May increase the serum concentration of Digoxin. Monitor therapy
Beta-Blockers: May enhance the bradycardic effect of Cardiac Glycosides. Exceptions: Levobunolol; Metipranolol. Monitor therapy
Bile Acid Sequestrants: May decrease the absorption of Cardiac Glycosides. Exceptions: Colesevelam. Monitor therapy
Bradycardia-Causing Agents: May enhance the bradycardic effect of other Bradycardia-Causing Agents. Monitor therapy
Bretylium: May enhance the adverse/toxic effect of Cardiac Glycosides. Management: Bretylium should only be used in digitalis-treated patients when other antiarrhythmic options are ineffective and when arrhythmia is not suspected to be related to digitalis toxicity. Bretylium is contraindicated in digitalis-induced arrhythmias. Consider therapy modification
Brimonidine (Topical): May enhance the bradycardic effect of Digoxin. Monitor therapy
BuPROPion: May decrease the serum concentration of Digoxin. Monitor therapy
Calcium Channel Blockers (Nondihydropyridine): May enhance the AV-blocking effect of Cardiac Glycosides. Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of Cardiac Glycosides. Monitor therapy
Calcium Polystyrene Sulfonate: May enhance the adverse/toxic effect of Cardiac Glycosides. Monitor therapy
Calcium Salts: May enhance the arrhythmogenic effect of Cardiac Glycosides. Monitor therapy
Canagliflozin: May increase the serum concentration of Digoxin. Monitor therapy
Carvedilol: Digoxin may enhance the bradycardic effect of Carvedilol. Carvedilol may increase the serum concentration of Digoxin. Monitor therapy
Ceritinib: Bradycardia-Causing Agents may enhance the bradycardic effect of Ceritinib. Management: If this combination cannot be avoided, monitor patients for evidence of symptomatic bradycardia, and closely monitor blood pressure and heart rate during therapy. Exceptions are discussed in separate monographs. Consider therapy modification
CloNIDine: May enhance the AV-blocking effect of Cardiac Glycosides. Sinus node dysfunction may also be enhanced. Monitor therapy
Cobicistat: May increase the serum concentration of Digoxin. Monitor therapy
Colchicine: Digoxin may increase the serum concentration of Colchicine. Monitor therapy
Conivaptan: May increase the serum concentration of Digoxin. Monitor therapy
CycloSPORINE (Systemic): May increase the serum concentration of Digoxin. Monitor therapy
Daclatasvir: May increase the serum concentration of Digoxin. Management: See full interaction monograph for details. Consider therapy modification
Diacerein: May enhance the arrhythmogenic effect of Cardiac Glycosides. Monitor therapy
Dronedarone: Digoxin may enhance the AV-blocking effect of Dronedarone. Digoxin may also enhance the other electrophysiologic effects of Dronedarone. Dronedarone may increase the serum concentration of Digoxin. Management: Avoid concurrent use of digoxin when possible. If concurrent use is necessary, reduce adult digoxin dose by 50%, monitor digoxin concentration closely, and increase monitoring for both clinical response to therapy and the occurrence of adverse effects. Consider therapy modification
Edrophonium: May enhance the AV-blocking effect of Cardiac Glycosides. Monitor therapy
Elagolix: May increase the serum concentration of Digoxin. Monitor therapy
Elexacaftor, Tezacaftor, and Ivacaftor: May increase the serum concentration of Digoxin. Monitor therapy
Eliglustat: May increase the serum concentration of Digoxin. Management: In patients receiving digoxin, measure digoxin serum concentrations prior to initiating eliglustat. Preemptively reduce digoxin doses by 30% and continue monitoring following eliglustat initiation. Consider therapy modification
EPHEDrine (Nasal): Cardiac Glycosides may enhance the arrhythmogenic effect of EPHEDrine (Nasal). Monitor therapy
EPHEDrine (Systemic): May enhance the arrhythmogenic effect of Cardiac Glycosides. Monitor therapy
Epoprostenol: May increase the serum concentration of Digoxin. Monitor therapy
Erdafitinib: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Etravirine: May increase the serum concentration of Digoxin. Management: Monitor serum digoxin concentrations and adjust dose as needed. In patients initiating a regimen of digoxin with etravirine, digoxin should be initiated at the lowest dose. Monitor therapy
Fexinidazole [INT]: May increase the serum concentration of Products Containing Propylene Glycol. Avoid combination
Fexinidazole [INT]: Bradycardia-Causing Agents may enhance the arrhythmogenic effect of Fexinidazole [INT]. Avoid combination
Flecainide: May increase the serum concentration of Digoxin. Monitor therapy
Flibanserin: May increase the serum concentration of Digoxin. Monitor therapy
Fostamatinib: May increase the serum concentration of Digoxin. Monitor therapy
Glecaprevir and Pibrentasvir: May increase the serum concentration of Digoxin. Management: Measure serum digoxin concentrations before initiating glecaprevir/pibrentasvir. Reduce digoxin concentrations by decreasing the digoxin dose by approximately 50% or by modifying the dosing frequency; continue monitoring during concomitant therapy. Consider therapy modification
Glycopyrrolate (Systemic): May increase the serum concentration of Digoxin. Monitor therapy
Ibrutinib: May increase the serum concentration of Digoxin. Monitor therapy
Isavuconazonium Sulfate: May increase the serum concentration of Digoxin. Monitor therapy
Istradefylline: May increase the serum concentration of Digoxin. Monitor therapy
Itraconazole: May increase the serum concentration of Cardiac Glycosides. Management: Consider preemptive cardiac glycoside dose adjustments with initiation / changes / discontinuation of itraconazole. Consider therapy modification
Ivabradine: Bradycardia-Causing Agents may enhance the bradycardic effect of Ivabradine. Monitor therapy
Ivacaftor: May increase the serum concentration of Digoxin. Monitor therapy
Kaolin: May decrease the serum concentration of Cardiac Glycosides. Monitor therapy
Lacosamide: Bradycardia-Causing Agents may enhance the AV-blocking effect of Lacosamide. Monitor therapy
Lasmiditan: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Avoid combination
Lenalidomide: May increase the serum concentration of Digoxin. Monitor therapy
Levosulpiride: May enhance the adverse/toxic effect of Cardiac Glycosides. Specifically, levosulpiride may diminish symptoms of cardiac glycoside-related toxicity. Monitor therapy
Licorice: May enhance the adverse/toxic effect of Cardiac Glycosides. Monitor therapy
Loop Diuretics: May enhance the adverse/toxic effect of Cardiac Glycosides. Specifically, cardiac glycoside toxicity may be enhanced by the hypokalemic and hypomagnesemic effect of loop diuretics. Monitor therapy
Lumacaftor and Ivacaftor: May decrease the serum concentration of Digoxin. Lumacaftor and Ivacaftor may increase the serum concentration of Digoxin. Monitor therapy
Macrolide Antibiotics: May increase the serum concentration of Cardiac Glycosides. Exceptions: Fidaxomicin; Roxithromycin; Spiramycin. Monitor therapy
Metaraminol: May enhance the arrhythmogenic effect of Cardiac Glycosides. Monitor therapy
MetroNIDAZOLE (Systemic): May enhance the adverse/toxic effect of Products Containing Propylene Glycol. A disulfiram-like reaction may occur. Avoid combination
Midodrine: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
MiFEPRIStone: May increase the serum concentration of Digoxin. Management: Measure serum digoxin concentration 1-2 weeks following mifepristone initiation, and in accordance with normal clinical practice thereafter, adjusting dose as needed. Monitor therapy
Milnacipran: May enhance the adverse/toxic effect of Digoxin. The risk of postural hypotension and tachycardia may be increased, particularly with IV digoxin. Management: Avoid concurrent use of intravenous (IV) digoxin in patients receiving milnacipran. Use caution when using oral digoxin and milnacipran together, monitoring closely for possible postural hypotension and tachycardia. Consider therapy modification
Mirabegron: May increase the serum concentration of Digoxin. Management: Consider using the lowest dose of digoxin when initiating concurrent mirabegron. Monitor serum digoxin concentrations closely to help guide digoxin dosing. Consider therapy modification
Multivitamins/Fluoride (with ADE): May enhance the arrhythmogenic effect of Cardiac Glycosides. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): May enhance the arrhythmogenic effect of Cardiac Glycosides. Monitor therapy
Multivitamins/Minerals (with AE, No Iron): May enhance the arrhythmogenic effect of Cardiac Glycosides. Monitor therapy
Nefazodone: May increase the serum concentration of Digoxin. Monitor therapy
Neratinib: May increase the serum concentration of Digoxin. Monitor therapy
Neuromuscular-Blocking Agents: May enhance the arrhythmogenic effect of Cardiac Glycosides. Monitor therapy
NIFEdipine: May increase the serum concentration of Digoxin. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents: May increase the serum concentration of Digoxin. Monitor therapy
Ombitasvir, Paritaprevir, and Ritonavir: May increase the serum concentration of Digoxin. Management: When initiating the ombitasvir/paritaprevir/ritonavir combination product in patients taking digoxin, decrease the digoxin dose by 30% to 50% and monitor serum digoxin levels to determine further dose adjustments. Consider therapy modification
Parathyroid Hormone: May enhance the adverse/toxic effect of Cardiac Glycosides. More specifically, Parathyroid Hormone-related hypercalcemia may predispose to digitalis toxicity. Monitor therapy
Paricalcitol: May enhance the adverse/toxic effect of Digoxin. Monitor therapy
PenicillAMINE: May decrease the serum concentration of Digoxin. Monitor therapy
P-glycoprotein/ABCB1 Inducers: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inducers may also further limit the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
P-glycoprotein/ABCB1 Inhibitors: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inhibitors may also enhance the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
Polyethylene Glycol 3350: May decrease the serum concentration of Digoxin. Monitor therapy
Polyethylene Glycol 4000: May decrease the serum concentration of Digoxin. Monitor therapy
Posaconazole: May increase the serum concentration of Digoxin. Monitor therapy
Potassium-Sparing Diuretics: May diminish the therapeutic effect of Cardiac Glycosides. In particular, the inotropic effects of digoxin appear to be diminished. Potassium-Sparing Diuretics may increase the serum concentration of Cardiac Glycosides. This particular effect may be unique to Spironolactone. Monitor therapy
Propafenone: May increase the serum concentration of Cardiac Glycosides. Monitor therapy
QuiNIDine: May increase the serum concentration of Cardiac Glycosides. Management: Upon quinidine initiation, consider reducing cardiac glycoside dose by 25% to 50%, with continued monitoring of glycoside serum concentrations and clinical response until the quinidine reaches steady state (5-10 days). Consider therapy modification
QuiNINE: May increase the serum concentration of Digoxin. Monitor therapy
Ranolazine: May increase the serum concentration of Digoxin. Monitor therapy
Regorafenib: May enhance the bradycardic effect of Digoxin. Monitor therapy
Reserpine: May enhance the adverse/toxic effect of Cardiac Glycosides. Monitor therapy
Ritonavir: May increase the serum concentration of Digoxin. Consider therapy modification
Roxithromycin: May increase the serum concentration of Cardiac Glycosides. Monitor therapy
Ruxolitinib: May enhance the bradycardic effect of Bradycardia-Causing Agents. Management: Ruxolitinib Canadian product labeling recommends avoiding use with bradycardia-causing agents to the extent possible. Monitor therapy
Sarecycline: May increase the serum concentration of Digoxin. Monitor therapy
Simeprevir: May increase the serum concentration of Digoxin. Monitor therapy
Siponimod: Bradycardia-Causing Agents may enhance the bradycardic effect of Siponimod. Management: Avoid coadministration of siponimod with drugs that may cause bradycardia. Consider therapy modification
SITagliptin: May increase the serum concentration of Digoxin. Monitor therapy
Sodium Polystyrene Sulfonate: May enhance the adverse/toxic effect of Digoxin. Monitor therapy
Spironolactone: May increase the serum concentration of Digoxin. Spironolactone (and/or its metabolites) may also interfere with the assays used to determine Digoxin concentrations, falsely increasing or decreasing Digoxin concentrations. Monitor therapy
St John's Wort: May decrease the serum concentration of Digoxin. Monitor therapy
Sucralfate: May decrease the serum concentration of Digoxin. Specifically, sucralfate may decrease the absorption of digoxin. Management: Administer digoxin at least 2 hours before sucralfate. Consider therapy modification
Telmisartan: May increase the serum concentration of Cardiac Glycosides. Monitor therapy
Terlipressin: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Tezacaftor and Ivacaftor: May increase the serum concentration of Digoxin. Monitor therapy
Thiazide and Thiazide-Like Diuretics: May enhance the adverse/toxic effect of Cardiac Glycosides. Specifically, cardiac glycoside toxicity may be enhanced by the hypokalemic and hypomagnesemic effect of thiazide diuretics. Monitor therapy
Ticagrelor: May increase the serum concentration of Digoxin. Monitor therapy
Tofacitinib: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Tolvaptan: May increase the serum concentration of Digoxin. Monitor therapy
Trimethoprim: May increase the serum concentration of Digoxin. Monitor therapy
Valbenazine: May increase the serum concentration of Digoxin. Monitor therapy
Vandetanib: May increase the serum concentration of Digoxin. Monitor therapy
Velpatasvir: May increase the serum concentration of Digoxin. Monitor therapy
Vemurafenib: May increase the serum concentration of Digoxin. Management: Avoid coadministration of vemurafenib and digoxin when possible. If concomitant use cannot be avoided, consider digoxin dose reduction. Consider therapy modification
Venetoclax: May increase the serum concentration of Digoxin. Management: Administer digoxin at least 6 hours before venetoclax when concomitant therapy is required. Consider therapy modification
Vilazodone: May increase the serum concentration of Digoxin. Monitor therapy
Vitamin D Analogs: May enhance the arrhythmogenic effect of Cardiac Glycosides. Monitor therapy
Test Interactions
Spironolactone may interfere with digoxin radioimmunoassay.
Adverse Reactions
Incidence not always reported.
Cardiovascular: Accelerated junctional rhythm, asystole, atrial tachycardia with or without block, AV dissociation, first-, second- (Wenckebach), or third-degree heart block, facial edema, PR prolongation, PVCs (especially bigeminy or trigeminy), ST segment depression, ventricular tachycardia or ventricular fibrillation
Central nervous system: Dizziness (6%), mental disturbances (5%), headache (4%), apathy, anxiety, confusion, delirium, depression, fever, hallucinations
Dermatologic: Rash (erythematous, maculopapular [most common], papular, scarlatiniform, vesicular or bullous), pruritus, urticaria, angioneurotic edema
Gastrointestinal: Nausea (4%), vomiting (2%), diarrhea (4%), abdominal pain, anorexia
Neuromuscular & skeletal: Weakness
Ophthalmic: Visual disturbances (blurred or yellow vision)
Respiratory: Laryngeal edema
<1%, postmarketing, and/or case reports (limited to important or life-threatening): Asymmetric chorea, gynecomastia, thrombocytopenia, palpitation, intestinal ischemia, hemorrhagic necrosis of the intestines, vaginal cornification, eosinophilia, sexual dysfunction, diaphoresis
Warnings/Precautions
Concerns related to adverse effects:
- Digoxin toxicity: Signs and symptoms of digoxin toxicity include anorexia, nausea, vomiting, visual changes, and cardiac arrhythmias; toxicity is usually associated with digoxin levels >2 ng/mL, although symptoms may occur at lower levels. Patients at increased risk for digoxin toxicity include those with low body weight, advanced age, renal impairment, hypokalemia, hypercalcemia, or hypomagnesemia.
- Extravasation: IV administration: Vesicant; ensure proper needle or catheter placement prior to and during administration; avoid extravasation.
- Proarrhythmic effects: Monitor for proarrhythmic effects (especially with digoxin toxicity)
Disease-related concerns:
- Accessory bypass tract (eg, Wolff-Parkinson-White [WPW] syndrome): During an episode of atrial fibrillation or flutter in patients with an accessory bypass tract or pre-excitation syndrome, use has been associated with increased anterograde conduction down the accessory pathway leading to ventricular fibrillation; avoid use in such patients (ACLS [Neumar 2010]; AHA/ACC/HRS [January 2014]).
- Acute coronary syndrome: Use with caution in patients with an acute MI; may increase myocardial oxygen demand and lead to ischemia. During an acute coronary syndrome, digoxin administered IV may be used to slow a rapid ventricular response and improve left ventricular (LV) function in the acute treatment of atrial fibrillation associated with severe LV function and heart failure or hemodynamic instability (AHA/ACC/HRS [January 2014]).
- Atrial fibrillation: When used for rate control in patients with atrial fibrillation, monitor serum concentrations closely; may be associated with an increased risk of mortality especially when serum concentrations are not properly controlled (Vamos 2015).
- Beri beri heart disease: Patients with beri beri heart disease may fail to adequately respond to digoxin therapy; treat underlying thiamine deficiency concomitantly.
- Electrolyte imbalance: Correct electrolyte disturbances, especially hypokalemia or hypomagnesemia, prior to use and throughout therapy; toxicity may occur despite therapeutic digoxin concentrations (eg, <2 ng/mL). Hypercalcemia may increase the risk of digoxin toxicity and hypocalcemia can nullify the effects of digoxin; maintain normocalcemia.
- Heart failure: Digoxin should be considered for use only in heart failure (HF) with reduced ejection fraction (HFrEF) when symptoms remain despite guideline-directed medical therapy. It may also be considered in patients with both HF and atrial fibrillation; however, beta blockers may offer better ventricular rate control than digoxin (ACCF/AHA [Yancy 2013]). Withdrawal of digoxin in clinically stable patients with HF may lead to recurrence of HF symptoms (Packer 1993). Monitor serum concentrations closely; may be associated with an increased risk of mortality especially when serum concentrations are not properly controlled (Vamos 2015).
- Hypermetabolic states: Atrial arrhythmias associated with hypermetabolic (eg, hyperthyroidism) or hyperdynamic (hypoxia, arteriovenous shunt) states are very difficult to treat; treat underlying condition first. If digoxin is used, ensure digoxin toxicity does not occur.
- Hypertrophic cardiomyopathy (HCM) with outflow tract obstruction: Outflow obstruction may worsen due to the positive inotropic effects of digoxin; avoid use unless used to control ventricular response with atrial fibrillation. Digoxin is potentially harmful in the treatment of dyspnea in patients with HCM in the absence of atrial fibrillation (ACCF/AHA [Gersh 2011]).
- Myocarditis: In a murine model of viral myocarditis, digoxin in high doses was shown to be detrimental (Matsumori 1999). If used in humans, therefore, digoxin should be used with caution and only at low doses (Frishman 2007). The manufacturer recommends avoiding the use of digoxin in patients with myocarditis.
- Preserved left ventricular function: Decreased cardiac output may occur in patients with preserved left ventricular systolic function, including restrictive or hypertrophic cardiomyopathy, constrictive pericarditis, amyloid heart disease, and acute cor pulmonale; in general, the manufacturer recommends to avoid use unless used to control ventricular response with atrial fibrillation.
- Renal impairment: Use with caution in patients with renal impairment; dosage adjustment needed.
- Sinus node disease and atrioventricular (AV) block: Because digoxin slows sinoatrial and AV conduction, the drug commonly prolongs the PR interval. Digoxin may cause severe sinus bradycardia or sinoatrial block particularly in patients with preexisting sinus node disease. Avoid use in patients with second- or third-degree heart block (except in patients with a functioning artificial pacemaker) (ACCF/AHA [Yancy 2013]); incomplete AV block (eg, Stokes-Adams attacks) may progress to complete block with digoxin administration. In such patients, if treatment with digoxin is necessary, consider the insertion of a pacemaker before treatment.
- Thyroid disease: Use with caution in patients with hypothyroidism, higher digoxin concentrations may result due to significant reduction in digoxin clearance (Burk 2010). In patients with hyperthyroidism, lower digoxin concentrations may result due to an increase in renal clearance of digoxin. No significant differences in absorption were seen in either thyroid condition compared with those with normal thyroid function (Burk 2010). Note: New-onset atrial fibrillation or exacerbation of ventricular arrhythmias should prompt evaluation of thyroid status.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Infants: Newborn infants display considerable variability to their tolerance to digoxin; premature and immature infants are particularly sensitive to the effects of digoxin.
- Low body weight: Patients with decreased body weight are at an increased risk of drug-related toxicity.
Dosage form specific issues:
- Propylene glycol: Some dosage forms may contain propylene glycol; large amounts are potentially toxic and have been associated hyperosmolality, lactic acidosis, seizures, and respiratory depression; use caution (AAP 1997; Zar 2007).
Other warnings/precautions:
- Elective electrical cardioversion: It is not necessary to routinely reduce or hold digoxin therapy prior to elective electrical cardioversion for atrial fibrillation; however, exclusion of digoxin toxicity (eg, clinical and ECG signs) is necessary prior to cardioversion. If signs of digoxin excess exist, withhold digoxin and delay cardioversion until toxicity subsides (AHA/ACC/HRS [January 2014]).
Monitoring Parameters
Heart rate and rhythm should be monitored along with periodic ECGs to assess desired effects and signs of toxicity; baseline and periodic serum creatinine. Periodically monitor serum potassium, magnesium, and calcium especially if on medications where these electrolyte disturbances can occur (eg, diuretics), or if patient has a history of hypokalemia or hypomagnesemia. Observe patients for noncardiac signs of toxicity, confusion, and depression.
When to draw serum digoxin concentrations: Digoxin serum concentrations are monitored because digoxin possesses a narrow therapeutic serum range; the therapeutic endpoint is difficult to quantify and digoxin toxicity may be life-threatening. Digoxin serum concentrations should be drawn at least 6 to 8 hours after last dose, regardless of route of administration (optimally 12 to 24 hours after a dose). Note: Serum digoxin concentrations may decrease in response to exercise due to increased skeletal muscle uptake; a period of rest (eg, ~2 hours) after exercise may be necessary prior to drawing serum digoxin concentrations.
Initiation of therapy:
If a loading dose is given: Digoxin serum concentration may be drawn within 12 to 24 hours after the initial loading dose administration. Concentrations drawn this early may confirm the relationship of digoxin plasma concentrations and response but are of little value in determining maintenance doses.
If a loading dose is not given: Digoxin serum concentration should be obtained after 3 to 5 days of therapy.
Maintenance therapy:
Trough concentrations should be followed just prior to the next dose or at a minimum of 6 to 8 hours after last dose.
Digoxin serum concentrations should be obtained within 5 to 7 days (approximate time to steady-state) after any dosage changes. Continue to obtain digoxin serum concentrations 7 to 14 days after any change in maintenance dose. Note: In patients with end-stage renal disease, it may take 15 to 20 days to reach steady-state.
Patients who are receiving electrolyte-depleting medications such as diuretics, serum potassium, magnesium, and calcium should be monitored closely.
Digoxin serum concentrations should be obtained whenever any of the following conditions occur:
Questionable patient compliance or to evaluate clinical deterioration following an initial good response
Changing renal function
Suspected digoxin toxicity
Initiation or discontinuation of therapy with drugs (eg, amiodarone, quinidine, verapamil) which potentially interact with digoxin.
Any disease changes (eg, thyroid disease)
Pregnancy
Pregnancy Considerations
Digoxin crosses the placenta.
Available guidelines note experience with digoxin in pregnancy is extensive (ESG [Regitz-Zagrosek 2018]). Based on available data, an increased risk of adverse pregnancy outcomes has not been observed. However, untreated maternal heart failure and atrial fibrillation may increase the risk of preterm birth and low birth weight, respectively. The manufacturer recommends monitoring neonates for signs and symptoms of digoxin toxicity following in utero exposure.
Due to pregnancy-induced physiologic changes, some pharmacokinetic properties of digoxin may be altered. Close monitoring of maternal serum digoxin is recommended (Hebert 2008; Luxford 1983; Martin-Suarez 2017); dose adjustments may be required during pregnancy and postpartum.
Heart failure and atrial fibrillation may worsen during pregnancy. Digoxin is recommended as a first-line agent for the chronic treatment of highly symptomatic supraventricular tachycardia (SVT) in pregnancy; the lowest effective dose is recommended (ACC/AHA/HRS [Page 2015]). Digoxin may be considered for long-term rate control of maternal atrial tachycardia or atrial fibrillation when preferred agents fail (ESG [Regitz-Zagrosek 2018]). Monitor for an increased risk of maternal arrhythmias during labor and delivery.
Digoxin may be considered for the in utero management of fetal SVT or atrial flutter with hydrops or ventricular dysfunction. Digoxin may also be considered for SVT without hydrops or ventricular dysfunction if heart rate is ≥200 bpm, atrial flutter, or other rare tachycardias with an average heart rate of ≥200 bpm (AHA [Donofrio 2014]).
Patient Education
What is this drug used for?
- It is used to treat heart failure (weak heart).
- It is used to treat a certain type of abnormal heartbeat (atrial fibrillation).
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Headache
- Abdominal pain
- Injection site pain
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Severe dizziness
- Passing out
- Nausea
- Vomiting
- Severe diarrhea
- Vision changes
- Seeing halos or bright colors around lights
- Weight loss
- Lack of appetite
- Loss of strength and energy
- Black, tarry, or bloody stools
- Vomiting blood
- Confusion
- Slow heartbeat
- Fast heartbeat
- Abnormal heartbeat
- Sensing things that seem real but are not
- Behavioral changes
- Mood changes
- Enlarged breasts
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.