Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule Delayed Release Particles, Oral, as base:
Generic: 250 mg
Solution Reconstituted, Intravenous, as lactobionate [preservative free]:
Erythrocin Lactobionate: 500 mg (1 ea)
Suspension Reconstituted, Oral, as ethylsuccinate:
E.E.S. Granules: 200 mg/5 mL (100 mL, 200 mL) [cherry flavor]
EryPed 200: 200 mg/5 mL (100 mL) [fruit flavor]
EryPed 400: 400 mg/5 mL (100 mL) [banana flavor]
Generic: 200 mg/5 mL (100 mL, 200 mL); 400 mg/5 mL (100 mL)
Suspension Reconstituted, Oral, as ethylsuccinate [preservative free]:
Generic: 200 mg/5 mL (100 mL)
Tablet, Oral, as base:
Generic: 250 mg, 500 mg
Tablet, Oral, as ethylsuccinate:
E.E.S. 400: 400 mg [contains fd&c red #40, fd&c yellow #10 (quinoline yellow)]
Generic: 400 mg
Tablet, Oral, as stearate:
Erythrocin Stearate: 250 mg [contains corn starch]
Tablet Delayed Release, Oral, as base:
Ery-Tab: 250 mg, 333 mg, 500 mg
PCE: 333 mg [DSC]
PCE: 500 mg [DSC] [dye free, no artificial color(s)]
Generic: 250 mg, 333 mg, 500 mg
Pharmacology
Mechanism of Action
Inhibits RNA-dependent protein synthesis at the chain elongation step; binds to the 50S ribosomal subunit resulting in blockage of transpeptidation
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Variable but better with salt forms than with base form; 18% to 45%; ethylsuccinate may be better absorbed with food (Thompson 1980).
Distribution
Vd: 0.64 L/kg
Relative diffusion from blood into CSF: Minimal even with inflammation
CSF:blood level ratio: Normal meninges: 2% to 13%; Inflamed meninges: 7% to 25%
Metabolism
Demethylation primarily via hepatic CYP3A4
Excretion
Primarily feces; urine (2% to 15% as unchanged drug)
Time to Peak
Serum: Base: 4 hours; Ethylsuccinate: 0.5 to 2.5 hours; Stearate: 3 hours (Steigbigel 2000); delayed with food due to differences in absorption
Half-Life Elimination
Neonates (≤15 days of age): 2.1 hours; Adults: Peak: 1.5-2 hours; End-stage renal disease: 5-6 hours
Protein Binding
Base: 73% to 81%
Use: Labeled Indications
Bacterial infections: Treatment of susceptible bacterial infections, including S. pyogenes, some S. pneumoniae, some S. aureus, M. pneumoniae, Legionella pneumophila, diphtheria, pertussis, Chlamydia, erythrasma, N. gonorrhoeae, E. histolytica, syphilis and nongonococcal urethritis, and Campylobacter gastroenteritis; used in conjunction with neomycin for decontaminating the bowel
Surgical (preoperative) prophylaxis (colorectal): Colorectal decontamination, in conjunction with other agents, prior to surgical intervention
Use: Off Label
Acne vulgarisyes
Based on the American Academy of Dermatology guidelines of care for the management of acne vulgaris, oral erythromycin, in combination with topical therapy, may be considered as a treatment option for moderate and severe acne and forms of inflammatory acne that are resistant to topical treatments. However, its use should be restricted due to an increased risk of bacterial resistance and limited to patients who cannot receive a tetracycline (ie, pregnant women). Concomitant topical therapy with benzoyl peroxide or a retinoid should be administered with systemic antibiotic therapy (eg, oral erythromycin) and continued for maintenance after the oral antibiotic course is completed.
Bartonella spp. infections (treatment)cyes
Based on the Infectious Diseases Society of America (IDSA) guidelines for the diagnosis and management of skin and soft tissue infections (SSTI), erythromycin may be considered for the treatment of cutaneous bacillary angiomatosis. Guidelines state that therapy has not been systematically examined and erythromycin appears effective based on case reports and small series.
Data from a study with a limited number of patients suggest that erythromycin may be beneficial for the treatment of Bartonella spp infections Koehler 1992, Tappero 1993. Expert opinion recommendations based upon clinical experience also suggests the utility of erythromycin in the treatment of this condition Rolain 2004.
Bartonella spp. infections (treatment) in HIV-infected patients (adolescents and adults)yes
Based on the US Department of Health and Human Services (HHS) Guidelines for Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents, erythromycin is a recommended and effective agent for treatment of bacillary angiomatosis, peliosis hepatis, bacteremia, osteomyelitis, and other severe infections (excluding CNS infections or endocarditis) due to Bartonella in adolescent and adult HIV-infected patients.
Chancroidyes
Based on Centers for Disease Control and Prevention (CDC) sexually transmitted diseases treatment guidelines, erythromycin (base) is effective and recommended for the treatment of chancroid due to H. ducreyi. However, intermediate resistance to erythromycin has been reported in several isolates. Potential resistance issues should be considered when initiating therapy for the treatment of chancroid.
Chronic obstructive pulmonary disease, prevention of exacerbationsbyes
Data from 2 randomized, double-blind, placebo-controlled trials and a prospective, randomized, controlled, but not blinded, trial support the use of erythromycin in prevention of exacerbations of chronic obstructive pulmonary disease (COPD) He 2010, Seemungal 2008, Suzuki 2001. In addition, data from a meta-analysis support the prophylactic use of erythromycin in prevention of COPD exacerbations Donath 2013.
Based on the European Respiratory Society and American Thoracic Society Guideline for the Prevention of COPD exacerbations and the Global Initiative for Chronic Obstructive Lung Disease (GOLD) for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease guidelines, erythromycin is effective and recommended to prevent exacerbations in patients with moderate to severe COPD despite optimal maintenance inhaler therapy.
Endoscopy/esophagogastroduodenoscopy, adjunctive prokinetic agentb
Data from 4 small randomized, controlled studies support the use of IV erythromycin as a prokinetic agent to improve quality of examination by reducing the amount of blood in the stomach prior to endoscopy in patients with acute upper GI bleeding Altraif 2011, Carbonell 2006, Coffin 2002, Frossard 2002. Two meta-analyses also support the use of IV erythromycin as a prokinetic agent prior to esophagogastroduodenoscopy (EGD) to reduce the need for second endoscopy in patients with acute upper GI bleeding Bai 2011, Barkun 2010.
Gastroparesis (management)yes
Based on the American College of Gastroenterology (ACG) guidelines for the management of gastroparesis, erythromycin is effective and recommended for the management of gastroparesis.
Granuloma inguinale (donovanosis)yes
Based on Centers for Disease Control and Prevention (CDC) sexually transmitted diseases treatment guidelines, erythromycin (base) is effective and recommended for the treatment of granuloma inguinale when azithromycin is not appropriate.
Contraindications
Hypersensitivity to erythromycin, any macrolide antibiotics, or any component of the formulation
Concomitant use with pimozide, cisapride, ergotamine or dihydroergotamine, terfenadine, astemizole, lovastatin, or simvastatin
Dosage and Administration
Dosing: Adult
Note: PCE tablets have been discontinued in the US for more than 1 year.
Note: Due to differences in absorption, 400 mg erythromycin ethylsuccinate produces the same serum levels as 250 mg erythromycin base or stearate.
Usual dosage range:
Oral:
Base: 250 to 500 mg every 6 to 12 hours; maximum: 4 g daily
Ethylsuccinate: 400 to 800 mg every 6 to 12 hours; maximum: 4 g daily
IV: Lactobionate: 15 to 20 mg/kg/day divided every 6 hours or 500 mg to 1 g every 6 hours; maximum: 4 g daily
Indication-specific dosing:
Acne vulgaris (alternative therapy) (off-label use): Oral: Initial: 250 to 500 mg (base) twice daily, followed by 250 to 500 mg (base) once daily (Tan 2003; Tan 2005). The shortest possible duration should be used to minimize development of bacterial resistance; re-evaluate at 3 to 4 months (AAD [Zaenglein 2016])
Bartonella spp infections (bacillary angiomatosis [BA], peliosis hepatis [PH]) (off-label use): Oral: 500 mg (base) 4 times daily for 3 months (BA) or 4 months (PH) (Koehler 1992; Rolain 2004; Stevens 2014; Tappero 1993). Note: IDSA skin and soft tissue infection guidelines recommend a duration of initial therapy of 2 weeks to 2 months for cutaneous BA, although treatment durations are not standardized (IDSA [Stevens 2014])
Bartonella spp infections in HIV-infected patients (off-label use; HHS [OI adult 2015]): Note: Duration of therapy is at least 3 months; continuation of therapy depends on relapse occurrence and clinical condition
Bacillary angiomatosis, peliosis hepatis, bacteremia, and osteomyelitis: Oral, IV: 500 mg every 6 hours
Other severe infections (excluding CNS infections or endocarditis): Oral, IV: 500 mg every 6 hours with rifampin
Chancroid (off-label use): Oral: 500 mg (base) 3 times daily for 7 days; Note: Isolates with intermediate resistance have been documented (CDC [Workowski 2015])
Chlamydia trachomatis infection, uncomplicated: Oral:
Urogenital infections (off-label): 500 mg (base) four times daily or 800 mg (ethylsuccinate) four times daily for 7 days (CDC [Workowski 2015])
Lymphogranuloma venereum (off-label; alternative therapy to doxycycline): Oral: 500 mg (base) 4 times daily for 21 days (CDC [Workowski 2015])
Chronic obstructive pulmonary disease (COPD), prevention of exacerbations (off-label use): Oral: 200 to 400 mg/day (formulation not specified) (Suzuki 2001) or 250 mg (stearate) twice daily (Seemungal 2008).
Endoscopy/esophagogastroduodenoscopy, adjunctive prokinetic agent (off-label use): IV: 3 mg/kg as a single dose over 30 minutes administered 30 to 90 minutes prior to endoscopy (Coffin 2002; Saltzman 2019) or 250 mg as a single dose over 5 to 30 minutes administered 20 to 30 minutes prior to endoscopy (Carbonell 2006; Frossard 2002)
Gastroparesis (off-label use):
IV: 3 mg/kg administered over 45 minutes every 8 hours (Camilleri 2013)
Oral: Patients refractory/intolerant to other prokinetic agents (eg, metoclopramide, domperidone): 250 to 500 mg (base) 3 times daily before meals. Limit duration of therapy, tachyphylaxis may occur after 4 weeks (Camilleri 2013).
Granuloma inguinale (donovanosis) (off-label use): Oral: 500 mg (base) 4 times daily for at least 21 days and resolution of lesions (CDC [Workowski 2015]). Note: If symptoms do not improve within the first few days of therapy, the addition of gentamicin may be considered (CDC [Workowski 2015]).
Impetigo (IDSA [Stevens 2014]): Oral:
Base: 250 mg 4 times daily for 7 days, depending on response
Ethylsuccinate: 400 mg 4 times daily for 7 days, depending on response
Legionnaire disease: Oral: 1.6 to 4 g (ethylsuccinate) daily or 1 to 4 g (base) daily in divided doses for 21 days. Note: No longer preferred therapy and only used in nonhospitalized patients.
Nongonococcal urethritis: Oral:
500 mg (base) 4 times daily or 800 mg (ethylsuccinate) 4 times daily for 7 days (CDC [Workowski 2015]).
Manufacturer's labeling: Dosing in the prescribing information may not reflect current clinical practice.
Base: 500 mg (base) 4 times daily or two 333 mg (base) tablets every 8 hours
Ethylsuccinate: 800 mg (ethylsuccinate) 3 times daily. Note: May use 250 mg (base) or 400 mg (ethylsuccinate) 4 times daily
Pertussis: Oral: 500 mg (base) every 6 hours for 14 days
Surgical (preoperative) prophylaxis (colorectal) (off-label dose): Oral: 1 g erythromycin base per dose at 1 PM, 2 PM, and 11 PM on the day before 8 AM surgery combined with mechanical cleansing of the large intestine, oral neomycin. Perioperative IV antibiotics are also given on the day of surgery (Bratzler 2013).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
General dosing, susceptible infection: Infants, Children, and Adolescents:
Manufacturer's labeling:
Oral: Base, ethylsuccinate, stearate: 30 to 50 mg/kg/day divided every 6 to 8 hours usually; for severe infection may double dose; maximum daily dose: Mild to moderate infection: 2,000 mg/day; severe infection: 4,000 mg/day
IV: Lactobionate: 15 to 20 mg/kg/day divided every 6 hours; maximum daily dose: 4,000 mg/day
Alternate dosing (Red Book 2012):
Mild to moderate infection: Oral: 50 mg/kg/day divided every 6 to 8 hours; maximum daily dose: 2,000 mg/day
Severe infection: IV: Lactobionate: 5 mg/kg/dose every 6 hours, maximum daily dose: 4,000 mg/day
Acne, moderate to severe; treatment: Children and Adolescents: Oral: 250 to 500 mg 1 to 2 times daily in conjunction with topical therapy (eg, benzoyl peroxide); maximum daily dose: 50 mg/kg/day; duration of 4 to 8 weeks of therapy usually necessary to evaluate initial clinical response with a longer duration for a maximum effect (3 to 6 months); resistance problematic with therapy, use typically reserved for patients <8 years who cannot receive tetracycline derivatives (Eichenfield 2013)
Anthrax, cutaneous, community-acquired (Stevens 2005): Infants, Children, and Adolescents:
Oral: 10 mg/kg/dose every 6 hours; treatment duration of 5 to 9 days usually adequate in most cases
IV: 20 to 40 mg/kg/day divided every 6 hours; maximum daily dose: 4,000 mg; treatment duration of 5 to 9 days usually adequate in most cases
Bartonella sp infections [bacillary angiomatosis (BA), peliosis hepatis (PH)]:
Non-HIV-exposed/-positive; treatment: Infants, Children, and Adolescents: Oral: Ethylsuccinate: 10 mg/kg/ dose 4 times daily; maximum daily dose: 2,000 mg/day; treatment duration: BA: 3 months; PH: 4 months (Rolain 2004)
HIV-exposed/-positive:
Prophylaxis: Infants and Children (CDC 2009): Oral: 30 to 50 mg/kg/day divided into 2 to 4 doses daily; maximum daily dose: 2,000 mg/day
Treatment: Duration of therapy: ≥3 months (of sufficient duration to prevent relapse)
Infants and Children (CDC 2009):
Oral: 30 to 50 mg/kg/day divided into 2 to 4 doses daily; maximum daily dose: 2,000 mg/day
IV: 15 to 50 mg/kg/day divided into 4 doses daily; maximum daily dose: 2,000 mg/day
Adolescents: IV, Oral: 500 mg every 6 hours with or without rifampin (DHHS [adult] 2013)
Catheter (peritoneal dialysis); exit-site or tunnel infection: Infants, Children, and Adolescents: Oral (base): 30 to 50 mg/kg/day divided 3 to 4 times daily; maximum dose: 500 mg/dose (Warady [ISPD 2012])
Chlamydia trachomatis infection (CDC 2010; Red Book 2012):
Conjunctivitis or pneumonia: Infants, Children, and Adolescents: Oral (base or ethylsuccinate): 50 mg/kg/day divided every 6 hours for 14 days; maximum daily dose: 2,000 mg/day; a repeat course may be necessary; for severe trachoma, longer durations may be necessary (40 days)
Anogenital tract infection:
Children and Adolescents <45 kg: Oral (base or ethylsuccinate): 50 mg/kg/day divided every 6 hours for 14 days; maximum daily dose: 2,000 mg/day
Adolescents ≥45 kg: Oral:
Base: 500 mg 4 times daily for 7 days
Ethylsuccinate: 800 mg 4 times daily for 7 days
Lymphogranuloma venereum (LGV): Adolescents ≥45 kg: Oral (base): 500 mg 4 times daily for 21 days
Impetigo: Infants, Children, and Adolescents: Oral: 10 mg/kg/dose 4 times daily (Stevens 2005)
Lyme Disease: Infants, Children, and Adolescents: Oral: 50 mg/kg/day divided every 6 hours for 14 to 21 days; maximum dose: 500 mg (Wormser 2006)
Pertussis (CDC 2005; Red Book 2012):
Infants 1 to 5 months: Oral: 10 mg/kg/dose 4 times daily for 14 days
Infants ≥6 months and Children: Oral: 10 mg/kg/dose 4 times daily for 7 to 14 days; maximum daily dose: 2,000 mg/day
Adolescents: Oral: 500 mg 4 times daily for 7 to 14 days
Pneumonia, community-acquired (CAP) (Bradley 2011): Infants >3 months, Children, and Adolescents: Note: A beta-lactam antibiotic should be added if typical bacterial pneumonia cannot be ruled out.
Presumed atypical (M. pneumoniae, C. pneumoniae, C. trachomatis); mild infection or step-down therapy: Oral: 10 mg/kg/dose every 6 hours; maximum daily dose: 2,000 mg/day
Moderate to severe atypical infection: IV: Lactobionate: 5 mg/kg/dose every 6 hours; maximum daily dose: 4,000 mg/day
Preoperative bowel preparation: Children and Adolescents: Oral: Base: 20 mg/kg; maximum dose: 1,000 mg administered at 1, 2, and 11 PM on the day before surgery combined with mechanical cleansing of the large intestine and oral neomycin (Bratzler 2013)
Prokinetic (GI motility) agent: Limited data available: Infants, Children, and Adolescents:
Diagnosis; gastric emptying study (provocative testing): IV: 2.8 mg/kg infused over 20 minutes was reported from one center's experience; maximum dose: 250 mg (Waseem 2012)
Treatment: Oral: 3 mg/kg/dose 4 times daily; may increase as needed to effect; maximum dose: 10 mg/kg or 250 mg (Rodriguez 2012)
Pneumococcal, prophylaxis in penicillin-allergic patients with sickle cell disease (SCD) and functional or anatomic asplenia (Knight-Madden 2001): Oral:
Infants and Children: 4 months to <3 years: 125 mg twice daily; salt not specified
Children 3 to 4 years: 250 mg twice daily; salt not specified
Reconstitution
Erythromycin lactobionate should be reconstituted with sterile water for injection without preservatives to a concentration of 50 mg/mL. No less than 100 mL of IV diluent should be used for an infusion bag. The final diluted solution should be 1 to 5 mg/mL.
Administration
Oral: Administer base, PCE or stearate dosage forms on an empty stomach (2 hours before or after a meal); administer ethylsuccinate (EES) or delayed-release (ERY-TAB) without regards to meals; may consider administering after food to decrease GI discomfort. Swallow delayed release capsule or enteric coated tablets whole, do not chew or break.
IV: Infuse 1 g over 20 to 60 minutes. IV infusion may be very irritating to the vein; infusion should be sufficiently slow to minimize pain along the vein. Do not administer IV push or bolus.
Dietary Considerations
Some products may contain sodium.
Base, PCE or stearate dosage forms should be taken on an empty stomach (2 hours before or after a meal).
Ethylsuccinate (EES) or delayed-release (ERY-TAB) dosage forms may be administered without regards to meals.
May consider administering after food to decrease GI discomfort.
Storage
Injection: Store unreconstituted vials at 20°C to 25°C (68°F to 77°F). Reconstituted solution (50 mg/mL) is stable for 2 weeks when refrigerated or for 24 hours at room temperature. Erythromycin IV infusion solution is stable at pH 6 to 8; stability of lactobionate is pH dependent; IV form has longest stability in NS. Parenteral admixture in NS is stable for 24 hours at 4°C. Admixtures in NS (including Add-Vantage containers) should be infused within 8 hours of preparation.
Oral suspension:
Granules: Prior to mixing, store at 20°C to 25°C (68°F to 77°F). After mixing, store under refrigeration and use within 10 days.
Powder: Prior to mixing, store at <30°C (86°F). After mixing, store at ≤25°C (77°F) and use within 35 days.
Tablet and capsule formulations: Store at 20°C to 25°C (68°F to 77°F).
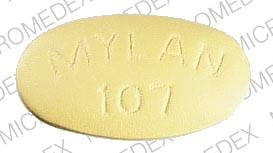
Erythromycin (Systemic) Images
Drug Interactions
Abemaciclib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Abemaciclib. Monitor therapy
Acalabrutinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Acalabrutinib. Management: Reduce acalabrutinib dose to 100 mg once daily with concurrent use of a moderate CYP3A4 inhibitor. Monitor patient closely for both acalabrutinib response and evidence of adverse effects with any concurrent use. Consider therapy modification
Afatinib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Afatinib. Management: Reduce afatinib by 10 mg if not tolerated. Some non-US labeling recommends avoiding combination if possible. If used, administer the P-gp inhibitor simultaneously with or after the dose of afatinib. Consider therapy modification
Alfentanil: Erythromycin (Systemic) may increase the serum concentration of Alfentanil. Management: For patients who are actively receiving erythromycin, caution should be used in administering alfentanil; monitor for increased anesthetic and respiratory depressant effects. Consider using lower doses of alfentanil or an alternative anesthetic. Consider therapy modification
ALPRAZolam: Erythromycin (Systemic) may increase the serum concentration of ALPRAZolam. Monitor therapy
Amiodarone: May enhance the QTc-prolonging effect of Erythromycin (Systemic). Erythromycin (Systemic) may enhance the QTc-prolonging effect of Amiodarone. Erythromycin (Systemic) may increase the serum concentration of Amiodarone. Avoid combination
Antineoplastic Agents (Vinca Alkaloids): Macrolide Antibiotics may increase the serum concentration of Antineoplastic Agents (Vinca Alkaloids). Macrolides may also increase the distribution of Vinca Alkaloids into certain cells and/or tissues. Management: Consider an alternative to using a macrolide antibiotic when possible in order to avoid the potential for increased vinca alkaloid toxicity. Consider therapy modification
Apixaban: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Apixaban. Monitor therapy
Aprepitant: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Aprepitant. Avoid combination
ARIPiprazole: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of ARIPiprazole. Management: Monitor for increased aripiprazole pharmacologic effects. Aripiprazole dose adjustments may or may not be required based on concomitant therapy and/or indication. Consult full interaction monograph for specific recommendations. Monitor therapy
Astemizole: May enhance the QTc-prolonging effect of Erythromycin (Systemic). Erythromycin (Systemic) may enhance the QTc-prolonging effect of Astemizole. Erythromycin (Systemic) may increase the serum concentration of Astemizole. Avoid combination
Asunaprevir: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Asunaprevir. Avoid combination
AtorvaSTATin: Erythromycin (Systemic) may increase the serum concentration of AtorvaSTATin. Monitor therapy
Avanafil: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Avanafil. Management: The maximum avanafil adult dose is 50 mg per 24-hour period when used together with a moderate CYP3A4 inhibitor. Patients receiving such a combination should also be monitored more closely for evidence of adverse effects. Consider therapy modification
Avapritinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Avapritinib. Management: Avoid use of moderate CYP3A4 inhibitors with avapritinib. If this combination cannot be avoided, reduce the avapritinib dose from 300 mg once daily to 100 mg once daily. Consider therapy modification
Axitinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Axitinib. Monitor therapy
Barnidipine: Erythromycin (Systemic) may increase the serum concentration of Barnidipine. Avoid combination
BCG (Intravesical): Antibiotics may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG Vaccine (Immunization): Antibiotics may diminish the therapeutic effect of BCG Vaccine (Immunization). Monitor therapy
Benzhydrocodone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Benzhydrocodone. Specifically, the concentration of hydrocodone may be increased. Monitor therapy
Betrixaban: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Betrixaban. Management: Decrease the adult betrixaban dose to an initial single dose of 80 mg followed by 40 mg once daily if combined with a P-glycoprotein inhibitor. Consider therapy modification
Bilastine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Bilastine. Management: Consider alternatives when possible; bilastine should be avoided in patients with moderate to severe renal insufficiency who are receiving p-glycoprotein inhibitors. Consider therapy modification
Blonanserin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Blonanserin. Monitor therapy
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Bosentan: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Bosentan. Management: Concomitant use of both a CYP2C9 inhibitor and a CYP3A inhibitor or a single agent that inhibits both enzymes with bosentan is likely to cause a large increase in serum concentrations of bosentan and is not recommended. See monograph for details. Monitor therapy
Bosutinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Bosutinib. Avoid combination
Brentuximab Vedotin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Brentuximab Vedotin. Specifically, concentrations of the active monomethyl auristatin E (MMAE) component may be increased. Monitor therapy
Brexpiprazole: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Brexpiprazole. Management: The brexpiprazole dose should be reduced to 25% of usual if used together with both a moderate CYP3A4 inhibitor and a strong or moderate CYP2D6 inhibitor, or if a moderate CYP3A4 inhibitor is used in a CYP2D6 poor metabolizer. Monitor therapy
Brigatinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Brigatinib. Management: Avoid concurrent use of brigatinib with moderate CYP3A4 inhibitors when possible. If such a combination cannot be avoided, reduce the dose of brigatinib by approximately 40% (ie, from 180 mg to 120 mg, from 120 mg to 90 mg, or from 90 mg to 60 mg). Consider therapy modification
Bromocriptine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Bromocriptine. Management: The bromocriptine dose should not exceed 1.6 mg daily with use of a moderate CYP3A4 inhibitor. The Cycloset brand specifically recommends this dose limitation, but other bromocriptine products do not make such specific recommendations. Consider therapy modification
Budesonide (Systemic): CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Budesonide (Systemic). Avoid combination
Budesonide (Topical): CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Budesonide (Topical). Management: Per US prescribing information, avoid this combination. Canadian product labeling does not recommend strict avoidance. If combined, monitor for excessive glucocorticoid effects as budesonide exposure may be increased. Consider therapy modification
BusPIRone: Erythromycin (Systemic) may increase the serum concentration of BusPIRone. Management: Limit the buspirone dose to 2.5 mg twice daily and monitor for increased buspirone effects/toxicities if combined with erythromycin. Consider therapy modification
Calcium Channel Blockers: Macrolide Antibiotics may decrease the metabolism of Calcium Channel Blockers. Management: Consider using a noninteracting macrolide. Felodipine Canadian labeling specifically recommends avoiding its use in combination with clarithromycin. Exceptions: Clevidipine. Consider therapy modification
Cannabidiol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Cannabidiol. Monitor therapy
Cannabis: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Cannabis. More specifically, tetrahydrocannabinol and cannabidiol serum concentrations may be increased. Monitor therapy
CarBAMazepine: Erythromycin (Systemic) may increase the serum concentration of CarBAMazepine. Management: Consider alternative antimicrobial therapy in combination with carbamazepine. If combined, monitor for increased carbamazepine effects/toxicities. Consider therapy modification
Cardiac Glycosides: Macrolide Antibiotics may increase the serum concentration of Cardiac Glycosides. Monitor therapy
Celiprolol: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Celiprolol. Monitor therapy
Ceritinib: QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may enhance the QTc-prolonging effect of Ceritinib. Ceritinib may enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of Ceritinib. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Cholera Vaccine: Antibiotics may diminish the therapeutic effect of Cholera Vaccine. Management: Avoid cholera vaccine in patients receiving systemic antibiotics, and within 14 days following the use of oral or parenteral antibiotics. Avoid combination
Cilostazol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Cilostazol. Management: Consider reducing the cilostazol dose to 50 mg twice daily in adult patients who are also receiving moderate inhibitors of CYP3A4. Consider therapy modification
Cisapride: May enhance the QTc-prolonging effect of Erythromycin (Systemic). Erythromycin (Systemic) may enhance the QTc-prolonging effect of Cisapride. Erythromycin (Systemic) may increase the serum concentration of Cisapride. Avoid combination
Citalopram: May enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of Citalopram. Monitor therapy
Clindamycin (Topical): Erythromycin (Systemic) may diminish the therapeutic effect of Clindamycin (Topical). Avoid combination
Clopidogrel: Erythromycin (Systemic) may diminish the antiplatelet effect of Clopidogrel. Monitor therapy
Cobicistat: May increase the serum concentration of Erythromycin (Systemic). Management: Consider alternatives to this combination when cobicistat is combined with atazanavir or darunavir. If combined, monitor for increased erythromycin and cobicistat effects/toxicities. Consider therapy modification
Cobimetinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Cobimetinib. Management: Avoid the concomitant use of cobimetinib and moderate CYP3A4 inhibitors. If concurrent short term (14 days or less) use cannot be avoided, reduce the cobimetinib dose to 20 mg daily. Avoid combination
Codeine: CYP3A4 Inhibitors (Moderate) may increase serum concentrations of the active metabolite(s) of Codeine. Monitor therapy
Colchicine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Colchicine. Management: Reduce colchicine dose as directed when using with a moderate CYP3A4 inhibitor, and increase monitoring for colchicine-related toxicity. See full monograph for details. Use extra caution in patients with impaired renal and/or hepatic function. Consider therapy modification
Colchicine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Colchicine. Colchicine distribution into certain tissues (e.g., brain) may also be increased. Management: Colchicine is contraindicated in patients with impaired renal or hepatic function who are also receiving a p-glycoprotein inhibitor. In those with normal renal and hepatic function, reduce colchicine dose as directed. See full monograph for details. Consider therapy modification
Crizotinib: QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may enhance the QTc-prolonging effect of Crizotinib. QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of Crizotinib. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
CycloSPORINE (Systemic): Erythromycin (Systemic) may increase the serum concentration of CycloSPORINE (Systemic). Monitor therapy
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP3A4 Substrates (High risk with Inhibitors): CYP3A4 Inhibitors (Moderate) may decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Exceptions: Alitretinoin (Systemic); Praziquantel; Trabectedin; Vinorelbine. Monitor therapy
Dabigatran Etexilate: P-glycoprotein/ABCB1 Inhibitors may increase serum concentrations of the active metabolite(s) of Dabigatran Etexilate. Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dapoxetine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Dapoxetine. Management: The dose of dapoxetine should be limited to 30 mg per day when used together with a moderate inhibitor of CYP3A4. Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Deflazacort: CYP3A4 Inhibitors (Moderate) may increase serum concentrations of the active metabolite(s) of Deflazacort. Management: Administer one third of the recommended deflazacort dose when used together with a strong or moderate CYP3A4 inhibitor. Consider therapy modification
Domperidone: May enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of Domperidone. Avoid combination
Doxofylline: Erythromycin (Systemic) may increase the serum concentration of Doxofylline. Monitor therapy
DOXOrubicin (Conventional): CYP3A4 Inhibitors (Moderate) may increase the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to moderate CYP3A4 inhibitors in patients treated with doxorubicin whenever possible. One U.S. manufacturer (Pfizer Inc.) recommends that these combinations be avoided. Consider therapy modification
DOXOrubicin (Conventional): P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to P-glycoprotein inhibitors in patients treated with doxorubicin whenever possible. One U.S. manufacturer (Pfizer Inc.) recommends that these combinations be avoided. Consider therapy modification
Dronabinol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Dronabinol. Monitor therapy
Dronedarone: May enhance the QTc-prolonging effect of Erythromycin (Systemic). Erythromycin (Systemic) may increase the serum concentration of Dronedarone. Avoid combination
Edoxaban: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Edoxaban. Management: See full monograph for details. Reduced doses are recommended for patients receiving edoxaban for venous thromboembolism in combination with certain P-gp inhibitors. Similar dose adjustment is not recommended for edoxaban use in atrial fibrillation. Consider therapy modification
Eletriptan: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Eletriptan. Management: The use of eletriptan within 72 hours of a moderate CYP3A4 inhibitor should be avoided. Consider therapy modification
Elexacaftor, Tezacaftor, and Ivacaftor: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Elexacaftor, Tezacaftor, and Ivacaftor. Management: When combined with moderate CYP3A4 inhibitors, two elexacaftor/tezacaftor/ivacaftor (100 mg/50 mg/75 mg) tablets should be given in the morning, every other day. Ivacaftor (150 mg) should be given in the morning, every other day on alternate days. Consider therapy modification
Eliglustat: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Eliglustat. Management: Use should be avoided under some circumstances. See full drug interaction monograph for details. Consider therapy modification
Encorafenib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Encorafenib. Management: Avoid concomitant use of encorafenib and moderate CYP3A4 inhibitors whenever possible. If concomitant administration is unavoidable, decrease the encorafenib dose prior to initiation of the CYP3A4 inhibitor. See full monograph for details. Consider therapy modification
Encorafenib: May enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of Encorafenib. Management: Avoid using moderate CYP3A4 inhibitors together with encorafenib if possible. If the combination must be used, reduce the encorafenib dose prior to initiation of the moderate CYP3A4 inhibitor and monitor QT interval. See full monograph for details. Consider therapy modification
Entrectinib: May enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of Entrectinib. Avoid combination
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Eplerenone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Eplerenone. Management: When used concomitantly with moderate inhibitors of CYP3A4, eplerenone dosing recommendations vary by indication and international labeling. See full drug interaction monograph for details. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Ergot Derivatives: Macrolide Antibiotics may increase the serum concentration of Ergot Derivatives. Cabergoline and Clarithromycin may interact, see specific monograph for full details. Exceptions: Cabergoline; Nicergoline; Pergolide. Consider therapy modification
Estrogen Derivatives: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Estrogen Derivatives. Monitor therapy
Everolimus: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Everolimus. Management: Everolimus dose reductions are required for most indications. See full monograph or prescribing information for specific dose adjustment and monitoring recommendations. Consider therapy modification
Everolimus: Inhibitors of CYP3A4 (Moderate) and P-glycoprotein may increase the serum concentration of Everolimus. Management: Everolimus dose reductions are required for most indications. See full monograph or prescribing information for specific dose adjustment and monitoring recommendations. Consider therapy modification
FentaNYL: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of FentaNYL. Management: Monitor patients closely for several days following initiation of this combination, and adjust fentanyl dose as necessary. Consider therapy modification
Fexinidazole [INT]: May enhance the QTc-prolonging effect of QT-prolonging Agents (Moderate Risk). Avoid combination
Fexofenadine: Erythromycin (Systemic) may increase the serum concentration of Fexofenadine. Monitor therapy
Flibanserin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Flibanserin. Avoid combination
Fluconazole: May enhance the QTc-prolonging effect of Erythromycin (Systemic). Fluconazole may increase the serum concentration of Erythromycin (Systemic). Avoid combination
Fosaprepitant: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Fosaprepitant. Avoid combination
GuanFACINE: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of GuanFACINE. Management: Reduce the guanfacine dose by 50% when initiating this combination. Consider therapy modification
Haloperidol: QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may enhance the QTc-prolonging effect of Haloperidol. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
HYDROcodone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of HYDROcodone. Monitor therapy
Ibrutinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ibrutinib. Management: When treating B-cell malignancies, decrease ibrutinib to 280 mg daily when combined with moderate CYP3A4 inhibitors. When treating graft versus host disease, monitor patients closely and reduce the ibrutinib dose as needed based on adverse reactions. Consider therapy modification
Ifosfamide: CYP3A4 Inhibitors (Moderate) may decrease serum concentrations of the active metabolite(s) of Ifosfamide. Monitor therapy
Imatinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Imatinib. Monitor therapy
Ivabradine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ivabradine. Avoid combination
Ivacaftor: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ivacaftor. Management: Ivacaftor dose reductions may be required; consult full monograph content for age- and weight-specific dosage recommendations. Consider therapy modification
Ivosidenib: May enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of Ivosidenib. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Lactobacillus and Estriol: Antibiotics may diminish the therapeutic effect of Lactobacillus and Estriol. Monitor therapy
Larotrectinib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Larotrectinib. Monitor therapy
Lasmiditan: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Avoid combination
Lefamulin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Lefamulin. Management: Avoid concomitant use of lefamulin tablets with P-glycoprotein/ABCB1 inhibitors. If concomitant use is required, monitor for lefamulin adverse effects. Consider therapy modification
Lemborexant: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Lemborexant. Avoid combination
Lincomycin: Erythromycin (Systemic) may diminish the therapeutic effect of Lincomycin. Avoid combination
Lomitapide: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Lomitapide. Avoid combination
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Lovastatin: Erythromycin (Systemic) may increase the serum concentration of Lovastatin. Avoid combination
Lumacaftor and Ivacaftor: May decrease the serum concentration of Erythromycin (Systemic). Avoid combination
Lumateperone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Lumateperone. Avoid combination
Lurasidone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Lurasidone. Management: Lurasidone US labeling recommends reducing lurasidone dose by half with a moderate CYP3A4 inhibitor. Some non-US labeling recommends initiating lurasidone at 20 mg/day and limiting dose to 40 mg/day; avoid concurrent use of grapefruit products. Consider therapy modification
Meperidine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Meperidine. Monitor therapy
Mequitazine: Erythromycin (Systemic) may enhance the arrhythmogenic effect of Mequitazine. Management: Concurrent administration of intravenous erythromycin with mequitazine is contraindicated. Avoid combination
Methadone: May enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of Methadone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Midazolam: Macrolide Antibiotics may increase the serum concentration of Midazolam. Management: Consider an alternative less likely to interact. Azithromycin is likely a lower-risk macrolide, and benzodiazepines less dependent on CYP3A metabolism (e.g., lorazepam, oxazepam) are similarly less likely to interact. Consider therapy modification
Mirodenafil: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Mirodenafil. Monitor therapy
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Mizolastine: Macrolide Antibiotics may increase the serum concentration of Mizolastine. Avoid combination
Naldemedine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Naldemedine. Monitor therapy
Naldemedine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Naldemedine. Monitor therapy
Nalfurafine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Nalfurafine. Monitor therapy
Naloxegol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Naloxegol. Avoid combination
Neratinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Neratinib. Avoid combination
Nintedanib: Combined Inhibitors of CYP3A4 and P-glycoprotein may increase the serum concentration of Nintedanib. Monitor therapy
Olaparib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Olaparib. Management: Avoid use of moderate CYP3A4 inhibitors in patients being treated with olaparib, if possible. If such concurrent use cannot be avoided, the dose of olaparib should be reduced to 150 mg twice daily. Consider therapy modification
Ondansetron: May enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Oxybutynin: Erythromycin (Systemic) may increase the serum concentration of Oxybutynin. Monitor therapy
OxyCODONE: CYP3A4 Inhibitors (Moderate) may enhance the adverse/toxic effect of OxyCODONE. CYP3A4 Inhibitors (Moderate) may increase the serum concentration of OxyCODONE. Serum concentrations of the active metabolite Oxymorphone may also be increased. Monitor therapy
PAZOPanib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of PAZOPanib. Avoid combination
Pentamidine (Systemic): May enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Pexidartinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Pexidartinib. Monitor therapy
P-glycoprotein/ABCB1 Inducers: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inducers may also further limit the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
P-glycoprotein/ABCB1 Inhibitors: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inhibitors may also enhance the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
P-glycoprotein/ABCB1 Substrates: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inhibitors may also enhance the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Exceptions: Loperamide. Monitor therapy
Pimecrolimus: CYP3A4 Inhibitors (Moderate) may decrease the metabolism of Pimecrolimus. Monitor therapy
Pimozide: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Pimozide. Avoid combination
Pimozide: May enhance the QTc-prolonging effect of QT-prolonging Agents (Moderate Risk). Avoid combination
Pitavastatin: Erythromycin (Systemic) may increase the serum concentration of Pitavastatin. Management: Limit pitavastatin to a maximum of 1 mg/day (adult dose) when used in combination with erythromycin. If this combination is used, monitor patients more closely for evidence of pitavastatin toxicity. Consider therapy modification
Pivmecillinam: Erythromycin (Systemic) may diminish the therapeutic effect of Pivmecillinam. Monitor therapy
Pravastatin: Erythromycin (Systemic) may increase the serum concentration of Pravastatin. Monitor therapy
QT-prolonging Antidepressants (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). Exceptions: Citalopram. Monitor therapy
QT-prolonging Antipsychotics (Moderate Risk): QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Pimozide; QUEtiapine. Monitor therapy
QT-prolonging Class IA Antiarrhythmics (Highest Risk): May enhance the QTc-prolonging effect of Erythromycin (Systemic). Erythromycin (Systemic) may enhance the QTc-prolonging effect of QT-prolonging Class IA Antiarrhythmics (Highest Risk). Erythromycin (Systemic) may increase the serum concentration of QT-prolonging Class IA Antiarrhythmics (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
QT-prolonging Class IC Antiarrhythmics (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Class III Antiarrhythmics (Highest Risk): May enhance the QTc-prolonging effect of Erythromycin (Systemic). Erythromycin (Systemic) may enhance the QTc-prolonging effect of QT-prolonging Class III Antiarrhythmics (Highest Risk). Management: Avoid concomitant use of erythromycin and class III antiarrhythmic agents. Use of erythromycin with dronedarone is specifically contraindicated. Exceptions: Dronedarone. Avoid combination
QT-prolonging Kinase Inhibitors (Highest Risk): May enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of QT-prolonging Kinase Inhibitors (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Ivosidenib. Consider therapy modification
QT-prolonging Kinase Inhibitors (Moderate Risk): QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Kinase Inhibitors (Moderate Risk). QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of QT-prolonging Kinase Inhibitors (Moderate Risk). Exceptions: Encorafenib; Entrectinib. Monitor therapy
QT-prolonging Miscellaneous Agents (Highest Risk): May enhance the QTc-prolonging effect of Erythromycin (Systemic). Erythromycin (Systemic) may enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Astemizole; Cisapride; Terfenadine. Consider therapy modification
QT-prolonging Miscellaneous Agents (Moderate Risk): QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Moderate Risk). QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of QT-prolonging Miscellaneous Agents (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Domperidone. Monitor therapy
QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk): Erythromycin (Systemic) may enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Crizotinib; Fluconazole. Monitor therapy
QT-prolonging Quinolone Antibiotics (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Strong CYP3A4 Inhibitors (Moderate Risk): Erythromycin (Systemic) may enhance the QTc-prolonging effect of QT-prolonging Strong CYP3A4 Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Saquinavir. Monitor therapy
QUEtiapine: QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may enhance the QTc-prolonging effect of QUEtiapine. QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of QUEtiapine. Management: Monitor for increased quetiapine toxicities including QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QuiNIDine: Erythromycin (Systemic) may enhance the QTc-prolonging effect of QuiNIDine. Erythromycin (Systemic) may increase the serum concentration of QuiNIDine. Avoid combination
Ranolazine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ranolazine. Management: Limit the ranolazine adult dose to a maximum of 500 mg twice daily in patients concurrently receiving moderate CYP3A4 inhibitors (e.g., diltiazem, verapamil, erythromycin, etc.). Consider therapy modification
Repaglinide: Erythromycin (Systemic) may increase the serum concentration of Repaglinide. Management: The addition of a CYP2C8 inhibitor to this drug combination may substantially increase the magnitude of increase in repaglinide exposure. Monitor therapy
Rifamycin Derivatives: Macrolide Antibiotics may decrease the metabolism of Rifamycin Derivatives. Exceptions: Rifapentine. Consider therapy modification
RifAXIMin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of RifAXIMin. Monitor therapy
Rilpivirine: Macrolide Antibiotics may increase the serum concentration of Rilpivirine. Management: Consider the use of azithromycin or another non-macrolide alternative when appropriate to avoid this potential interaction. Consider therapy modification
Rivaroxaban: Erythromycin (Systemic) may increase the serum concentration of Rivaroxaban. Management: In patients with impaired renal function, erythromycin should not be used unless the potential benefits outweigh the potential risks. This interaction is unlikely clinically significant in patients with normal renal function. Consider therapy modification
Rupatadine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Rupatadine. Monitor therapy
Ruxolitinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ruxolitinib. Monitor therapy
Salmeterol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Salmeterol. Monitor therapy
Saquinavir: Erythromycin (Systemic) may enhance the QTc-prolonging effect of Saquinavir. Erythromycin (Systemic) may increase the serum concentration of Saquinavir. Avoid combination
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
SAXagliptin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of SAXagliptin. Monitor therapy
Sertraline: Erythromycin (Systemic) may enhance the adverse/toxic effect of Sertraline. Monitor therapy
Sildenafil: Erythromycin (Systemic) may increase the serum concentration of Sildenafil. Management: For pulmonary arterial hypertension, US label recommends no dose adjustment and Canadian label recommends reducing to 20 mg twice/day. For erectile dysfunction, consider using a lower starting dose of 25 mg in patients who are also taking erythromycin. Consider therapy modification
Silodosin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Silodosin. Monitor therapy
Silodosin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Silodosin. Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of Erythromycin (Systemic). Erythromycin (Systemic) may increase the serum concentration of Simeprevir. Avoid combination
Simvastatin: Erythromycin (Systemic) may increase the serum concentration of Simvastatin. Avoid combination
Sincalide: Drugs that Affect Gallbladder Function may diminish the therapeutic effect of Sincalide. Management: Consider discontinuing drugs that may affect gallbladder motility prior to the use of sincalide to stimulate gallbladder contraction. Consider therapy modification
Sirolimus: Erythromycin (Systemic) may increase the serum concentration of Sirolimus. Sirolimus may increase the serum concentration of Erythromycin (Systemic). Management: Monitor for increased serum concentrations of sirolimus if combined with erythromycin. Lower initial sirolimus doses or sirolimus dose reductions will likely be required. Consider therapy modification
Sodium Picosulfate: Antibiotics may diminish the therapeutic effect of Sodium Picosulfate. Management: Consider using an alternative product for bowel cleansing prior to a colonoscopy in patients who have recently used or are concurrently using an antibiotic. Consider therapy modification
Sonidegib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Sonidegib. Management: Avoid concomitant use of sonidegib and moderate CYP3A4 inhibitors when possible. When concomitant use cannot be avoided, limit CYP3A4 inhibitor use to less than 14 days and monitor for sonidegib toxicity (particularly musculoskeletal adverse reactions). Consider therapy modification
Suvorexant: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Suvorexant. Management: The recommended dose of suvorexant is 5 mg daily in patients receiving a moderate CYP3A4 inhibitor. The dose can be increased to 10 mg daily (maximum dose) if necessary for efficacy. Consider therapy modification
Tacrolimus (Systemic): Erythromycin (Systemic) may increase the serum concentration of Tacrolimus (Systemic). Monitor therapy
Tacrolimus (Topical): Macrolide Antibiotics may increase the serum concentration of Tacrolimus (Topical). Monitor therapy
Talazoparib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Talazoparib. Management: These listed exceptions are discussed in detail in separate interaction monographs. Monitor therapy
Tamsulosin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Tamsulosin. Monitor therapy
Tazemetostat: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Tazemetostat. Management: Avoid coadministration of tazemetostat and moderate CYP3A4 inhibitors. If coadministration cannot be avoided, dose reductions are required. See full monograph for dosing recommendations. Consider therapy modification
Tegaserod: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Tegaserod. Monitor therapy
Telithromycin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Telithromycin. Monitor therapy
Tetrahydrocannabinol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Tetrahydrocannabinol. Monitor therapy
Tezacaftor and Ivacaftor: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Tezacaftor and Ivacaftor. Management: When combined with moderate CYP3A4 inhibitors, tezacaftor/ivacaftor should be given in the morning, every other day. Ivacaftor alone should be given in the morning, every other day on alternate days. Consider therapy modification
Theophylline Derivatives: Macrolide Antibiotics may decrease the metabolism of Theophylline Derivatives. Exceptions: Dyphylline. Consider therapy modification
Ticagrelor: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ticagrelor. Monitor therapy
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Tofacitinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Tofacitinib. Monitor therapy
Tolvaptan: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Tolvaptan. Management: Jynarque dose requires adjustment when used with a moderate CYP3A4 inhibitor. See labeling or full interaction monograph for specific recommendations. Use of Samsca with moderate CYP3A4 ihibitors should generally be avoided. Consider therapy modification
Topotecan: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Topotecan. Avoid combination
Trabectedin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Trabectedin. Monitor therapy
Triazolam: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Triazolam. Management: Consider triazolam dose reduction in patients receiving concomitant moderate CYP3A4 inhibitors. Consider therapy modification
Typhoid Vaccine: Antibiotics may diminish the therapeutic effect of Typhoid Vaccine. Only the live attenuated Ty21a strain is affected. Management: Vaccination with live attenuated typhoid vaccine (Ty21a) should be avoided in patients being treated with systemic antibacterial agents. Use of this vaccine should be postponed until at least 3 days after cessation of antibacterial agents. Consider therapy modification
Ubrogepant: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ubrogepant. Management: Use an initial ubrogepant dose of 50 mg and avoid a second dose for 24 hours when used with moderate CYP3A4 inhibitors. Consider therapy modification
Udenafil: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Udenafil. Monitor therapy
Ulipristal: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ulipristal. Management: This is specific for when ulipristal is being used for signs/symptoms of uterine fibroids (Canadian indication). When ulipristal is used as an emergency contraceptive, patients receiving this combination should be monitored for ulipristal toxicity. Avoid combination
Vardenafil: Erythromycin (Systemic) may increase the serum concentration of Vardenafil. Management: Limit dose of vardenafil film-coated tablets (Levitra) to 5 mg per 24 hours with concomitant use of erythromycin. Concomitant use of vardenafil orally disintegrating tablets (Staxyn) with erythromycin is not recommended. Consider therapy modification
Venetoclax: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Venetoclax. Management: Reduce the venetoclax dose by at least 50% in patients requiring these combinations. Consider therapy modification
Venetoclax: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Venetoclax. Management: Consider a venetoclax dose reduction by at least 50% in patients requiring concomitant treatment with P-glycoprotein (P-gp) inhibitors. Consider therapy modification
Vilazodone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Vilazodone. Monitor therapy
VinCRIStine (Liposomal): P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of VinCRIStine (Liposomal). Avoid combination
Vitamin K Antagonists (eg, warfarin): Macrolide Antibiotics may increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Zafirlukast: Erythromycin (Systemic) may decrease the serum concentration of Zafirlukast. Monitor therapy
Zanubrutinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Zanubrutinib. Management: Decrease the zanubrutinib dose to 80 mg twice daily during coadministration with a moderate CYP3A4 inhibitor. Further dose adjustments may be required for zanubrutinib toxicities, refer to prescribing information for details. Consider therapy modification
Zopiclone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Zopiclone. Management: The starting adult dose of zopiclone should not exceed 3.75 mg if combined with a moderate CYP3A4 inhibitor. Monitor patients for signs and symptoms of zopiclone toxicity if these agents are combined. Consider therapy modification
Zuclopenthixol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Zuclopenthixol. Monitor therapy
Test Interactions
False-positive urinary catecholamines (fluorometric assay), 17-hydroxycorticosteroids and 17-ketosteroids
Adverse Reactions
Frequency not defined. Incidence may vary with formulation.
Cardiovascular: QTc prolongation, torsade de pointes, ventricular arrhythmia, ventricular tachycardia
Central nervous system: Seizure
Dermatologic: Erythema multiforme, pruritus, skin rash, Stevens-Johnson syndrome, toxic epidermal necrolysis, urticaria
Gastrointestinal: Abdominal pain, anorexia, diarrhea, nausea, oral candidiasis, pancreatitis, pseudomembranous colitis, pyloric stenosis (infantile hypertrophic), vomiting
Hepatic: Abnormal hepatic function tests, cholestatic jaundice (most common with estolate), hepatitis
Hypersensitivity: Anaphylaxis, hypersensitivity reaction
Local: Injection site phlebitis
Neuromuscular & skeletal: Weakness
Otic: Hearing loss
Renal: Interstitial nephritis
Postmarketing and/or case reports: Hepatotoxicity (idiosyncratic) (Chalasani 2014)
Warnings/Precautions
Concerns related to adverse effects:
- Altered cardiac conduction: Macrolides have been associated with rare QTc prolongation and ventricular arrhythmias, including torsade de pointes; use with caution in patients at risk of prolonged cardiac repolarization; avoid use in patients with prolonged QT interval, uncorrected hypokalemia or hypomagnesemia, clinically significant bradycardia, or concurrent use of Class IA (eg, quinidine, procainamide) or Class III (eg, amiodarone, dofetilide, sotalol) antiarrhythmic agents.
- Superinfection: Prolonged use may result in fungal or bacterial superinfection, including C. difficile-associated diarrhea (CDAD) and pseudomembranous colitis; CDAD has been observed >2 months postantibiotic treatment.
Disease-related concerns:
- Hepatic impairment: Use with caution in patients with preexisting liver disease; hepatic impairment, including hepatocellular and/or cholestatic hepatitis, with or without jaundice, has been observed. Discontinue if symptoms of malaise, nausea, vomiting, abdominal colic, and fever.
- Myasthenia gravis: Exacerbation of and new onset of myasthenia gravis symptoms have been reported.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
- Major inhibitor of CYP3A4: Use caution with any agents with substantial metabolism through the CYP3A4 pathway; high potential for drug interactions exists. Avoid concurrent use with strong CYP3A4 inhibitors; may increase the risk of sudden cardiac death (Ray 2004).
Special populations:
- Infants: Use of erythromycin has been associated with infantile hypertrophic pyloric stenosis (IHPS); observe for non-bilious vomiting or irritability with feeding.
- Elderly: May be at increased risk of adverse events, including hearing loss and/or torsade de pointes, particularly if concurrent renal/hepatic impairment.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol with caution in neonates. See manufacturer's labeling.
Pregnancy
Pregnancy Considerations
Erythromycin crosses the placenta. Cardiovascular anomalies following exposure in early pregnancy have been reported in some observational studies. Serum concentrations of erythromycin may be variable in pregnant women (Kiefer 1955; Philipson 1976).
Erythromycin is the antibiotic of choice for preterm prelabor rupture of membranes <34 0/7 weeks' gestation) (ACOG 188 2018), the treatment of lymphogranuloma venereum in pregnancy, and the treatment of or long-term suppression of Bartonella infection in HIV-infected pregnant patients. Erythromycin is one of the antibiotics that may be used for the treatment of chancroid or granuloma inguinale during pregnancy, and may be appropriate as an alternative agent for the treatment of chlamydial infections in pregnant women (consult current guidelines) (CDC [Workowski 2015]; HHS [opportunistic; adult] 2015).
Patient Education
What is this drug used for?
- It is used to treat or prevent bacterial infections.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Abdominal pain
- Nausea
- Vomiting
- Diarrhea
- Lack of appetite
- Injection site irritation
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes
- Not able to pass urine
- Change in amount of urine passed
- Severe dizziness
- Passing out
- Fast heartbeat
- Hearing loss
- Muscle weakness
- Trouble chewing or swallowing
- Trouble breathing
- Droopy eyelids
- Vision changes
- Blurred vision
- Double vision
- Irritability (newborns)
- Vomiting (newborns)
- Abnormal heartbeat
- Clostridioides (formerly Clostridium) difficile colitis (C. diff)-associated diarrhea like abdominal pain or cramps, severe diarrhea or watery stools, or bloody stools.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.