Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Capsule, Oral:
Zarontin: 250 mg [contains fd&c yellow #10 (quinoline yellow)]
Generic: 250 mg
Solution, Oral:
Zarontin: 250 mg/5 mL (474 mL) [raspberry flavor]
Generic: 250 mg/5 mL (473 mL, 474 mL)
Pharmacology
Mechanism of Action
Increases the seizure threshold and suppresses paroxysmal spike-and-wave pattern in absence seizures; depresses nerve transmission in the motor cortex
Pharmacokinetics/Pharmacodynamics
Absorption
Complete and rapid
Distribution
Vd: 0.7 L/kg (Battino 1995)
Metabolism
Hepatic via CYP3A to >40% inactive glucuronide conjugates (Patsalos 2018).
Excretion
Urine, slowly (12% to 20% as unchanged drug)
Time to Peak
Serum: 1 to 7 hours
Half-Life Elimination
Serum: Children: 30 hours; Adults: 50 to 60 hours
Protein Binding
21.8% (Patsalos 2017).
Use: Labeled Indications
Absence (petit mal) seizures: Management of absence (petit mal) seizures
Contraindications
Hypersensitivity to ethosuximide, succinimides, or any component of the formulation.
Dosage and Administration
Dosing: Adult
Absence (petit mal) seizures:
Oral: Initial: 500 mg/day. Individualize dose based on patient response by increasing in small increments (eg, ≤250 mg); doses >1,500 mg/day, in divided doses, should only be used under the strict supervision of a physician; higher doses may be necessary in some patients.
Note: Single daily doses have been shown to be effective and well tolerated in clinical trials (in children) and pharmacokinetic analysis (Buchanan 1976; Colburn 1978; Vajda 2014).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Absence (petit mal) seizures:
Note: In clinical practice, the daily dose is given in 2 divided doses or can be divided into 3 divided doses for patient tolerability (Pellock 2008).
Fixed dosing:
Children 3 to 6 years: Oral: Initial: 250 mg daily. Individualize dose based on patient response by increasing in small increments (eg, ≤250 mg) every 4 to 7 days as needed; usual optimal daily dose: 20 mg/kg/day; usual maximum daily dose: 1,500 mg/day in divided doses; higher doses may be necessary in some patients
Children ≥6 years and Adolescents: Oral: Initial: 500 mg daily. Individualize dose based on patient response by increasing in small increments (eg, 250 mg) every 4 to 7 days as needed; usual optimal daily dose: 20 mg/kg/day; usual maximum daily dose: 1,500 mg/day in divided doses; higher doses may be necessary in some patients
Weight-directed dosing: Children ≥2 years and Adolescents: Limited data available: Oral: Initial: 10 mg/kg/day, titrated to response in 5 to 10 mg/kg/day increments every 7 days as required; usual range: 20 to 30 mg/kg/day in 2 to 3 divided doses (Glauser 2010; Kleigman 2016). Single daily doses have also been shown to be effective and tolerated (Buchanan 1976; Dooley 1990). In a comparative efficacy trial of 446 pediatric patients ≤13 years of age (n=154 ethosuximide treatment group), the mean reported dose was 33.5 ± 15.3 mg/kg/day; short-term data (16 to 20 weeks) from this study showed ethosuximide to be effective as initial monotherapy for absence seizures with fewer adverse effects on attention compared to valproic acid; a follow-up study showed efficacy persisted 12 months after initiation (Glauser 2010; Glauser 2013). Doses reported in literature range from 6.5 to 50 mg/kg/day (Browne 1975; Sato 1982). Maximum daily dose: 60 mg/kg/day or 2,000 mg/day, whichever is less (Glauser 2010).
Storage
Capsules:
US labeling: Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
Canadian labeling: Store at 15ºC to 25ºC (59°F to 77°F). Protect from heat.
Solution:
US labeling: Store at 20°C to 25°C (68°F to 77°F); do not freeze. Protect from light.
Canadian labeling: Store at 15ºC to 25ºC (59°F to 77°F); do not freeze. Protect from light.
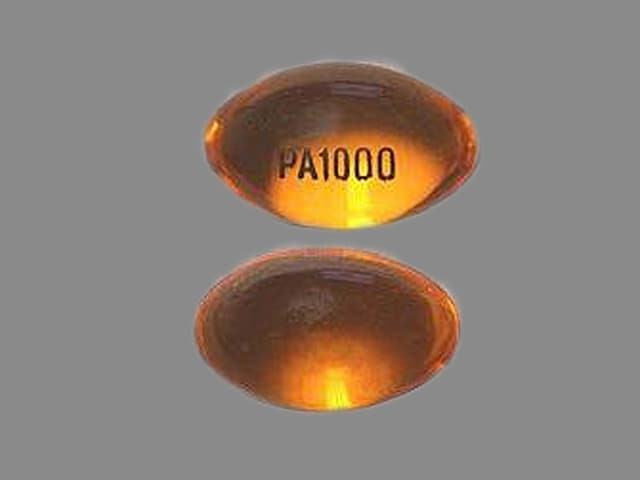
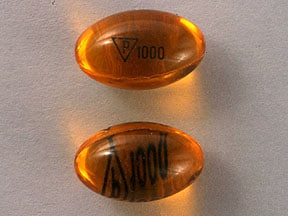
Ethosuximide Images
Drug Interactions
Alcohol (Ethyl): CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Amphetamines: May diminish the therapeutic effect of Ethosuximide. Amphetamines may decrease the serum concentration of Ethosuximide. Monitor therapy
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
Cobicistat: May increase the serum concentration of Ethosuximide. Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosphenytoin: Ethosuximide may enhance the CNS depressant effect of Fosphenytoin. Fosphenytoin may decrease the serum concentration of Ethosuximide. Ethosuximide may increase the serum concentration of Fosphenytoin. Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mefloquine: May diminish the therapeutic effect of Anticonvulsants. Mefloquine may decrease the serum concentration of Anticonvulsants. Management: Mefloquine is contraindicated for malaria prophylaxis in persons with a history of convulsions. Monitor anticonvulsant concentrations and treatment response closely with concurrent use. Consider therapy modification
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Mianserin: May diminish the therapeutic effect of Anticonvulsants. Monitor therapy
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orlistat: May decrease the serum concentration of Anticonvulsants. Monitor therapy
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Phenytoin: Ethosuximide may enhance the CNS depressant effect of Phenytoin. Phenytoin may decrease the serum concentration of Ethosuximide. Ethosuximide may increase the serum concentration of Phenytoin. Monitor therapy
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Valproate Products: Ethosuximide may decrease the serum concentration of Valproate Products. Valproate Products may increase the serum concentration of Ethosuximide. Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Adverse Reactions
Frequency not defined.
Central nervous system: Aggressive behavior, ataxia, delusional paranoid disorder, depression (with cases of overt suicidal intentions), disturbed sleep dizziness, drowsiness, euphoria, fatigue, headache, hyperactivity, irritability, lack of concentration, lethargy, night terrors
Dermatologic: Pruritus, skin rash, Stevens-Johnson syndrome, urticaria
Endocrine & metabolic: Hirsutism, increased libido, weight loss
Gastrointestinal: Abdominal pain, anorexia, abdominal cramps, diarrhea, epigastric pain, gastric distress, gingival hyperplasia, hiccups, nausea, swollen tongue, vomiting
Genitourinary: Occult blood in urine, vaginal hemorrhage
Hematologic & oncologic: Agranulocytosis, eosinophilia, leukopenia, pancytopenia
Hypersensitivity: Hypersensitivity reaction
Immunologic: DRESS syndrome (drug rash with eosinophilia and systemic symptoms)
Neuromuscular & skeletal: Systemic lupus erythematosus
Ophthalmic: Myopia
Warnings/Precautions
Concerns related to adverse effects:
- Blood dyscrasias: Severe blood dyscrasias (some fatal) have been reported. Monitor blood counts periodically, especially if signs/symptoms of infection develop.
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving).
- Dermatologic reactions: Severe reactions, including Stevens-Johnson syndrome (SJS), have been reported with an onset usually within 28 days, but may be observed later. Drug should be discontinued if there are any signs of rash, unless the rash is clearly not drug-related. If SJS is suspected do not resume ethosuximide and consider alternative therapy.
- Hepatic effects: Changes in hepatic function have been reported. Monitor liver function studies periodically.
- Multiorgan hypersensitivity reactions: Potentially serious, sometimes fatal drug reaction with eosinophilia and systemic symptoms (DRESS), also known as multiorgan hypersensitivity reactions, have been reported. Monitor for signs and symptoms (eg, fever, rash, exfoliative dermatitis, lymphadenopathy, facial swelling, eosinophilia) in association with other organ system involvement (eg, hepatitis, nephritis, hematologic abnormalities, pneumonitis, myocarditis, myositis, pericarditis). If DRESS is suspected, discontinue therapy.
- Renal effects: Changes in renal function have been reported. Monitor urinalysis periodically.
- Systemic lupus erythematous: Cases of systemic lupus erythematosus (SLE) have been reported.
- Suicidal ideation: Pooled analysis of trials involving various antiepileptics (regardless of indication) showed an increased risk of suicidal thoughts/behavior (incidence rate: 0.43% treated patients compared to 0.24% of patients receiving placebo); risk observed as early as 1 week after initiation and continued through duration of trials (most trials ≤24 weeks). Monitor all patients for notable changes in behavior that might indicate suicidal thoughts or depression; notify healthcare provider immediately if symptoms occur.
Disease-related concerns:
- Hepatic impairment: Use with extreme caution in patients with hepatic impairment.
- Renal impairment: Use with extreme caution in patients with renal impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity ("gasping syndrome") in neonates; the "gasping syndrome" consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP 1997; CDC 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol derivative with caution in neonates. See manufacturer's labeling.
Other warnings/precautions:
- Appropriate use: May be used in combination with other anticonvulsants in patients with both absence and tonic-clonic seizures. May increase tonic-clonic seizures when used alone in patients with mixed seizure disorders.
- Withdrawal: Anticonvulsants should not be discontinued abruptly because of the possibility of increasing seizure frequency; therapy should be withdrawn gradually to minimize the potential of increased seizure frequency, unless safety concerns require a more rapid withdrawal.
Monitoring Parameters
Seizure frequency; trough serum concentrations, CBC, platelets, liver enzymes (periodic), urinalysis (periodic); signs of rash; suicidality (eg, suicidal thoughts, depression, behavioral changes)
Pregnancy
Pregnancy Considerations
Ethosuximide crosses the placenta. Birth defects have been reported in infants. Epilepsy itself, the number of medications, genetic factors, or a combination of these may influence the teratogenicity of anticonvulsant therapy. In general, polytherapy may increase the risk of congenital malformations; monotherapy with the lowest effective dose is recommended (Harden 2009). For women with epilepsy who are planning a pregnancy in advance, baseline serum concentrations should be measured once or twice prior to pregnancy during a period when seizure control is optimal. Monitoring can then be continued up to once a month during pregnancy in women with stable seizure control (Patsalos 2008; Patsalos 2018).
Patients exposed to ethosuximide during pregnancy are encouraged to enroll themselves into the NAAED Pregnancy Registry by calling 1-888-233-2334. Additional information is available at www.aedpregnancyregistry.org.
Patient Education
What is this drug used for?
- It is used to help control certain kinds of seizures.
Frequently reported side effects of this drug
- Fatigue
- Headache
- Dizziness
- Hiccups
- Nausea
- Vomiting
- Diarrhea
- Lack of appetite
- Abdominal pain
- Abdominal cramps
- Weight loss
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Depression like thoughts of suicide, anxiety, emotional instability, or confusion.
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Lupus like rash on the cheeks or other body parts, sunburn easy, muscle or joint pain, chest pain or shortness of breath, or swelling in the arms or legs
- Chest pain
- Confusion
- Sensing things that seem real but are not
- Difficulty focusing
- Nightmares
- Trouble sleeping
- Change in balance
- Abnormal gait
- Vision changes
- Gingival changes
- Swollen glands
- Unable to pass urine
- Change in amount of urine passed
- Severe loss of strength and energy
- Bruising
- Bleeding
- Petechiae
- Seizures
- Agitation
- Irritability
- Panic attacks
- Mood changes
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.