Boxed Warning
Suicidality and antidepressant drugs:
Antidepressants increased the risk compared with placebo of suicidal thinking and behavior (suicidality) in short-term studies in children, adolescents, and young adults with major depressive disorder (MDD) and other psychiatric disorders. Anyone considering the use of fluoxetine or any other antidepressant in a child, adolescent, or young adult must balance this risk with the clinical need. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared with placebo in adults older than 24 years; there was a reduction in risk with antidepressants compared with placebo in adults 65 years and older. Depression and certain other psychiatric disorders are themselves associated with increases in the risk of suicide. Appropriately monitor and closely observe patients of all ages who are started on antidepressant therapy for clinical worsening, suicidality, or unusual changes in behavior. Advise families and caregivers of the need for close observation and communication with the prescribing health care provider.
Fluoxetine is approved for use in children with MDD (aged 8 years and older) and obsessive-compulsive disorder (OCD; aged 7 years and older). Sarafem is not approved for use in children.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
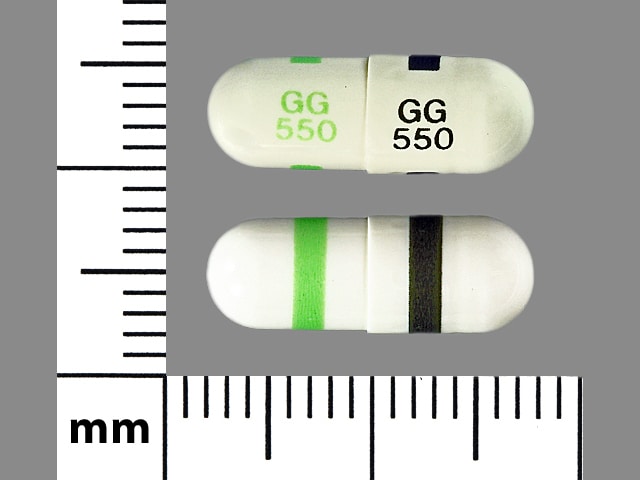
Capsule, Oral:
PROzac: 10 mg, 20 mg, 40 mg
Generic: 10 mg, 20 mg, 40 mg
Capsule Delayed Release, Oral:
PROzac Weekly: 90 mg [DSC]
Generic: 90 mg
Solution, Oral:
Generic: 20 mg/5 mL (5 mL, 120 mL)
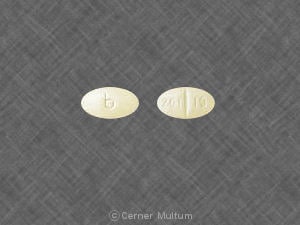
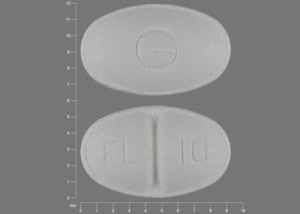
Tablet, Oral:
Sarafem: 10 mg, 20 mg [contains fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Generic: 10 mg, 20 mg, 60 mg
Pharmacology
Mechanism of Action
Inhibits CNS neuron serotonin reuptake; minimal or no effect on reuptake of norepinephrine or dopamine; does not significantly bind to alpha-adrenergic, histamine, or cholinergic receptors
Pharmacokinetics/Pharmacodynamics
Absorption
Well absorbed; delayed 1 to 2 hours with weekly formulation
Distribution
Vd: 12 to 43 L/kg
Metabolism
Hepatic, via CYP2C19 and 2D6, to norfluoxetine (activity equal to fluoxetine)
Excretion
Urine (10% as norfluoxetine, 2.5% to 5% as fluoxetine)
Onset of Action
Depression: The onset of action is within a week; however, individual response varies greatly and full response may not be seen until 8 to 12 weeks after initiation of treatment.
Time to Peak
Serum: 6 to 8 hours
Half-Life Elimination
Adults: Parent drug: 1 to 3 days (acute), 4 to 6 days (chronic), 7.6 days (cirrhosis); Metabolite (norfluoxetine): 9.3 days (range: 4 to 16 days), 12 days (cirrhosis)
Protein Binding
95% to albumin and alpha1 glycoprotein
Use in Specific Populations
Special Populations: Hepatic Function Impairment
The half-life for fluoxetine and norfluoxetine is prolonged.
Special Populations: Children
Average steady-state fluoxetine serum concentrations in children (n=10; 6 to <13 years of age) were 2-fold higher than in adolescents (n=11; 13 to <18 years of age); all patients received 20 mg/day; average steady-state norfluoxetine serum concentrations were 1.5-fold higher in the children compared with adolescents; differences in weight almost entirely explained the differences in serum concentrations.
Use: Labeled Indications
Bipolar major depression (excluding Sarafem): Acute treatment of major depressive episodes (in combination with olanzapine [preferred], other antipsychotics, or antimanic agents) (WFSBP [Grunze 2010]) associated with bipolar I disorder
Bulimia nervosa (excluding Sarafem): Acute and maintenance treatment of binge eating and vomiting behaviors in patients with moderate to severe bulimia nervosa
Major depressive disorder (unipolar) (excluding Sarafem): Acute and maintenance treatment of unipolar major depressive disorder (MDD)
Obsessive-compulsive disorder (excluding Sarafem): Acute and maintenance treatment of obsessions and compulsions in patients with obsessive-compulsive disorder
Panic disorder (excluding Sarafem): Acute treatment of panic disorder with or without agoraphobia
Premenstrual dysphoric disorder (Sarafem only): Treatment of premenstrual dysphoric disorder
Treatment-resistant depression (excluding Sarafem): Acute treatment of treatment-resistant depression (patients with MDD who do not respond to 2 separate trials of different antidepressants of adequate dose and duration in the current episode) in combination with olanzapine or other antipsychotics (APA 2010)
Use: Off Label
Binge eating disorderc
Data from a limited number of patients studied suggest that fluoxetine may be beneficial to improve binge frequency, weight loss, body mass index, and severity of illness in patients with binge eating disorder Arnold 2002a, Leombruni 2008.
Body dysmorphic disorderb
Data from a double-blind, randomized, placebo-controlled trial support the use of fluoxetine in the treatment of body dysmorphic disorder (with or without delusions) Phillips 2002.
Fibromyalgia, refractorybyes
Data from 2 double-blind, randomized trials support the use of fluoxetine in the treatment of pain, depression, sleep disturbance, and other symptoms of fibromyalgia Arnold 2002, Goldenberg 1996.
Based on
Generalized anxiety disorderyes
Based on the World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the pharmacological treatment of anxiety disorders, SSRIs are effective and recommended in the management of generalized anxiety disorder; however, evidence for fluoxetine is limited WFSBP [Bandelow 2008], WFSBP [Bandelow 2012].
Posttraumatic stress disorderbyes
Data from double-blind, randomized controlled trials support the use of fluoxetine for acute treatment and relapse prevention in patients with posttraumatic stress disorder (PTSD) Connor 1999, Martenyi 2002b, Martenyi 2002a.
Based on the
Premature ejaculationcyes
Data from a limited number of patients suggest that fluoxetine may have some benefit in the treatment of premature ejaculation Kara 1996.
According to the
Selective mutismc
Data from a limited number of patients studied in an open-label clinical trial and a double-blind, randomized, placebo-controlled trial suggest that fluoxetine may be beneficial for the treatment of selective mutism in children and adolescents Black 1994, Dummit 1996.
Social anxiety disorderbyes
Data from a large randomized, double-blind, placebo-controlled trial support the use of fluoxetine in the treatment of social anxiety disorder Davidson 2004.
Based on the WFSBP guidelines for the pharmacological treatment of anxiety, obsessive-compulsive, and posttraumatic stress disorders, SSRIs such as fluoxetine are effective and recommended for first-line treatment of social anxiety disorder; however, evidence for fluoxetine is more limited in comparison to other SSRIs.
Contraindications
Hypersensitivity to fluoxetine or any component of the formulation; use of MAO inhibitors intended to treat psychiatric disorders (concurrently, within 5 weeks of discontinuing fluoxetine, or within 2 weeks of discontinuing the MAO inhibitor); initiation of fluoxetine in a patient receiving linezolid or intravenous methylene blue; use with pimozide or thioridazine (Note: Thioridazine should not be initiated until 5 weeks after the discontinuation of fluoxetine.)
Canadian labeling: Additional contraindications (not in the US labeling): Initiation of fluoxetine within 2 weeks of thioridazine discontinuation
Dosage and Administration
Dosing: Adult
Note: In patients sensitive to adverse effects, some experts suggest lower starting doses of 5 to 10 mg/day and gradual titration in increments of no more than 10 mg, particularly in patients with anxiety who are generally more sensitive to overstimulation effects (eg, anxiety, insomnia) with antidepressants (Hirsch 2018c; Stein 2018; WFSBP [Bandelow 2012]).
Binge eating disorder (off-label use): Limited data available: Oral: Initial: 10 to 20 mg once daily; may increase dose based on response and tolerability in increments of 10 to 20 mg at intervals ≥1 week up to 80 mg/day (Arnold 2002a; Leombruni 2008; Sysko 2018).
Bipolar major depression: Oral: Initial: 20 mg once daily in the evening in combination with olanzapine (preferred), another second-generation antipsychotic, or antimanic agent; may increase dose in 10 to 20 mg increments every 1 to 7 days (Kupka 2018; Shelton 2019; Tohen 2003; WFSBP [Grunze 2010]; manufacturer's labeling); usual dose range: 20 to 50 mg/day (Kupka 2018; manufacturer's labeling). May also use the fixed-dose combination instead of the separate components. See Dosing conversion below for conversion to or from olanzapine/fluoxetine fixed-dose combination.
Body dysmorphic disorder (BDD) (off-label use): Oral: Initial: 20 mg once daily; may increase dose gradually based on response and tolerability in increments of 20 mg every 2 to 3 weeks to a usual dose of 70 to 80 mg/day by week 6 to 10 (Phillips 2002; Phillips 2018). Doses up to 120 mg/day, if tolerated, may be necessary in some patients for optimal response (Phillips 2018). Note: An adequate trial for assessment of effect in BDD is 12 to 16 weeks, including maximum tolerated doses for at least 3 to 4 of those weeks (Phillips 2018).
Bulimia nervosa: Oral: Initial: 20 mg once daily; may increase dose gradually (eg, at intervals ≥1 week) based on response and tolerability in 20 mg increments up to a target dose of 60 mg/day (Leombruni 2006).
Manufacturer's labeling: Dosing in prescribing information may not reflect current clinical practice. Initial: 60 mg/day
Fibromyalgia, refractory (alternative agent) (off-label use): Note: For patients not responsive to first-line agents (EULAR [Macfarlane 2017]). Oral: Initial: 20 mg once daily; may increase dose based on response and tolerability in 10 to 20 mg increments at ≥2-week intervals up to 80 mg/day. Mean dose in clinical trials was 45 mg/day (Arnold 2002b; EULAR [Macfarlane 2017]). In patients with an insufficient response to first-line monotherapy, some experts suggest low-dose combination therapy (eg, fluoxetine 20 mg/day with a tricyclic antidepressant) (Goldenberg 1996; Goldenberg 2018).
Generalized anxiety disorder (off-label use): Limited data available: Oral: Initial: 10 to 20 mg once daily; may gradually increase dose based on response and tolerability in 10 to 20 mg increments at intervals of ≥1 week up to 60 mg/day (Bystritsky 2018; Hirsch 2018c)
Major depressive disorder (unipolar): Oral: Initial: 20 mg once daily; may increase dose based on response and tolerability in 20 mg increments at intervals ≥1 week up to a maximum dose of 80 mg/day (Fava 1998). Usual dose: 20 to 60 mg/day (APA 2010). Note: For treatment-resistant depression, combination with olanzapine or another second-generation antipsychotic may be used; in major depression with psychotic features, fluoxetine plus an antipsychotic is standard treatment (APA 2010; Brunner 2014; Rothschild 2004). May consider use of the fixed-dose combination instead of the separate components. See Dosing conversions below for conversion to or from the olanzapine/fluoxetine fixed-dose combination.
Obsessive-compulsive disorder: Oral: Initial: 10 to 20 mg once daily; may increase dose gradually in 20 mg increments at intervals ≥1 week based on response and tolerability; recommended range: 40 to 80 mg/day (APA [Koran 2007]; Romano 2001; Simpson 2018; manufacturer's labeling). Based on clinical experience, some patients may require up to 120 mg/day for a response; however, adverse effects may increase (APA [Koran 2007]; Simpson 2018). Note: An adequate trial for assessment of effect in OCD is considered to be ≥6 weeks at maximum tolerated dose (Issari 2016).
Panic disorder: Oral: Initial: 5 to 10 mg once daily; after 3 to 7 days, gradually increase dose based on response and tolerability in 5 to 10 mg increments at intervals ≥1 week up to a usual dose of 20 to 40 mg/day (APA 2009). Maximum dose: 60 mg/day (manufacturer's labeling).
Posttraumatic stress disorder (PTSD) (off-label use): Oral: Initial: 10 to 20 mg once daily; may increase dose based on response and tolerability in 10 to 20 mg increments at intervals ≥1 week up to 80 mg/day. Usual dosage range in clinical trials: 20 to 60 mg/day (Connor 1999; Martenyi 2002a).
Premature ejaculation (off-label use): Limited data available: Oral: Initial: 20 mg once daily; may increase dose based on response and tolerability after ≥1 week (some experts suggest 3- to 4-week titration intervals [Khera 2018]) to 40 mg once daily (Kara 1996).
Premenstrual dysphoric disorder (PMDD):
Continuous daily dosing regimen: Oral: Initial: 10 mg once daily; increase to usual effective dose of 20 mg once daily over the first month; in a subsequent menstrual cycle, a further increase to 30 mg/day may be necessary in some patients for optimal response (Casper 2018).
Intermittent regimens:
Luteal phase dosing regimen: Oral: Initial: 10 mg once daily during the luteal phase of menstrual cycle only (ie, beginning therapy 14 days before anticipated onset of menstruation and continued to the onset of menses); over the first month, may increase to usual effective dose of 20 mg once daily during the luteal phase; in a subsequent menstrual cycle, a further increase to 30 mg/day during the luteal phase may be necessary in some patients for optimal response (Casper 2018).
Symptom-onset dosing regimen (off-label dosing): Oral: Limited data available: Initial 10 mg once daily from the day of symptom onset until a few days after the start of menses; over the first month, may increase dose based on response and tolerability up to 20 mg/day (Casper 2018).
Social anxiety disorder (off-label use): Oral: Initial: 10 to 20 mg once daily; after ~6 weeks may gradually increase dose based on response and tolerability in 10 mg increments at intervals of ≥1 week up to 60 mg/day (Davidson 2004; Stein 2018)
Dosing conversion:
Delayed release (once-weekly formulation): Immediate-release fluoxetine 20 mg/day = delayed-release fluoxetine 90 mg/week. When converting from immediate-release fluoxetine daily dosing, initiate delayed-release fluoxetine (90 mg once weekly) 7 days after the last 20 mg/day dose of immediate-release fluoxetine. Patients must be stabilized on immediate-release fluoxetine 20 mg once daily prior to switching.
Olanzapine/fluoxetine fixed-dose combination: When using individual components of fluoxetine with olanzapine rather than fixed-dose combination product, corresponding approximate dosage equivalents are as follows:
Olanzapine 2.5 mg + fluoxetine 20 mg = combination strength 3/25
Olanzapine 5 mg + fluoxetine 20 mg = combination strength 6/25
Olanzapine 12.5 mg + fluoxetine 20 mg = combination strength 12/25
Olanzapine 5 mg + fluoxetine 50 mg = combination strength 6/50
Olanzapine 12.5 mg + fluoxetine 50 mg = combination strength 12/50
Discontinuation of therapy: When discontinuing antidepressant treatment that has lasted for >3 weeks, gradually taper the dose (eg, over 1 to 4 weeks) to minimize withdrawal symptoms and detect re-emerging symptoms (APA 2010; WFSBP [Bauer 2015]). Reasons for a slower titration (eg, over 4 weeks) include prior history of antidepressant withdrawal symptoms or high doses of antidepressants (APA 2010; Hirsch 2019a ). If necessary, some clinicians allow for abrupt discontinuation based on fluoxetine's long half-life (Hirsch 2019a). If intolerable withdrawal symptoms occur, resume the previously prescribed dose and/or decrease dose at a more gradual rate (Shelton 2001). Select patients (eg, those with a history of discontinuation syndrome) on long-term treatment (>6 months) may benefit from tapering over >3 months (WFSBP [Bauer 2015]). Evidence supporting ideal taper rates is limited (Shelton 2001; WFSBP [Bauer 2015]).
Switching antidepressants: Evidence for ideal antidepressant switching strategies is limited; strategies include cross-titration (gradually discontinuing the first antidepressant while at the same time gradually increasing the new antidepressant) and direct switch (abruptly discontinuing the first antidepressant and then starting the new antidepressant at an equivalent dose or lower dose and increasing it gradually). Cross-titration (eg, over 1 to 4 weeks depending upon sensitivity to discontinuation symptoms and adverse effects) is standard for most switches, but is contraindicated when switching to or from an MAOI. A direct switch may be an appropriate approach when switching to another agent in the same or similar class (eg, when switching between two SSRIs), when the antidepressant to be discontinued has been used for <1 week, or when the discontinuation is for adverse effects. When choosing the switch strategy, consider the risk of discontinuation symptoms, potential for drug interactions, other antidepressant properties (eg, half-life, adverse effects, and pharmacodynamics), and the degree of symptom control desired (Hirsch 2018b; Ogle 2013; WFSBP [Bauer 2013]).
Switching to or from an MAOI:
Allow 14 days to elapse between discontinuing an MAOI and initiation of fluoxetine.
Allow 5 weeks to elapse between discontinuing fluoxetine and initiation of an MAOI.
Dosing: Geriatric
Major depressive disorder (unipolar): Oral: Some patients may require an initial dose of 10 mg once daily with dosage increases of 10 to 20 mg every several weeks as tolerated; should not be taken at night unless patient experiences sedation. Refer to adult dosing; use with caution given the long half-life of fluoxetine.
Dosing conversion: Refer to adult dosing.
Discontinuation of therapy: Refer to adult dosing.
Switching antidepressants: Refer to adult dosing.
Dosing: Pediatric
Anxiety with associated phobias and panic attacks: Very limited data available: Children 2 to 6 years: Oral: 5 mg/dose or 0.25 mg/kg/dose once daily; adequate trial is considered to be 8 to 10 weeks; continuation of therapy should be evaluated at 6 to 9 months after initiation; dosing based on case report in a 2.5-year old child and expert recommendations (Gleason 2007).
Bulimia nervosa adjunct therapy with cognitive behavioral therapy: Limited data available: Children ≥12 years and Adolescents: Oral: Initial: 20 mg once daily for 3 days, then 40 mg once daily for 3 days, then 60 mg once daily; dosing based on an open-label study of 10 pediatric patients (age: 12 to 18 years) which showed significant decrease in number of weekly purges; other reports describe use in adolescents (Gable 2005; Kotler 2003; Rosen 2010).
Depression:
Manufacturer's labeling: Children ≥8 years and Adolescents:
Lower weight Children: Oral: Initial: 10 mg once daily; usual daily dose: 10 mg/day; if needed, may increase dose to 20 mg once daily after several weeks; maximum daily dose: 20 mg/day.
Higher weight Children and Adolescents: Oral: Initial: 10 to 20 mg once daily; in patients started at 10 mg once daily, may increase dose to 20 mg after 1 week; maximum daily dose: 20 mg/day.
Alternate dosing: Limited data available: Lower initial dosing has been recommended by some experts (Dopheide 2006; Gleason 2007):
Children ≤11 years: Oral: Initial: 5 mg once daily; clinically, doses have been titrated up to 40 mg once daily in pediatric patients.
Children ≥12 years and Adolescents: Oral: Initial: 10 mg once daily; clinically, doses have been titrated up to 40 mg once daily in pediatric patients.
Depression associated with bipolar I disorder (in combination with olanzapine): Children ≥10 years and Adolescents: Oral: Initial: 20 mg in the evening; adjust dose, if needed, as tolerated; safety of fluoxetine doses >50 mg in combination with doses >12 mg of olanzapine has not been studied in pediatrics. Note: When using individual components of fluoxetine with olanzapine rather than fixed-dose combination product (Symbyax), approximate dosage correspondence is as follows:
Olanzapine 2.5 mg + fluoxetine 20 mg = Symbyax 3/25.
Olanzapine 5 mg + fluoxetine 20 mg = Symbyax 6/25.
Olanzapine 12.5 mg + fluoxetine 20 mg = Symbyax 12/25.
Olanzapine 5 mg + fluoxetine 50 mg = Symbyax 6/50.
Olanzapine 12.5 mg + fluoxetine 50 mg = Symbyax 12/50.
Obsessive-compulsive disorder:
Children <7 years: Limited data available: Oral: Initial: 5 mg once daily (Gleason 2007).
Children ≥7 years and Adolescents: Oral:
Lower weight Children: Initial: 10 mg once daily; if needed, may increase dose after several weeks; usual daily dose: 20 to 30 mg/day; minimal experience with doses >20 mg/day; no experience with doses >60 mg/day.
Higher weight Children and Adolescents: Initial: 10 mg once daily; increase dose to 20 mg once daily after 2 weeks; may increase dose after several more weeks, if needed; usual daily dose: 20 to 60 mg/day.
Repetitive behavior associated with autism spectrum disorders (ASD): Limited data available: Children ≥5 years and Adolescents: Oral: Initial: 2.5 mg once daily for 7 days; then may titrate at weekly intervals using weight-based dosing: 0.3 mg/kg/day during week 2; followed by 0.5 mg/kg/day during week 3, up to a maximum of 0.8 mg/kg/day; dosing based on a double-blind, crossover, placebo-controlled trial in 39 pediatric patients (age: 5 to 16 years) which showed statistically significant improvement in behavior scores compared to placebo; mean final dose: 9.9 mg/day (range: 2.4 to 20 mg/day) or 0.36 ± 0.116 mg/kg/day (Hollander 2005).
Selective mutism: Limited data available: Children ≥5 years and Adolescents: Oral: Initial: 5 mg once daily for 7 days, then increase to 10 mg daily for 7 days, and then increase to 20 mg daily; may further titrate in 20 mg/day increments if needed every 2 weeks; maximum daily dose: 60 mg/day. Dosing is based on an open-label study of 21 pediatric patients (age: 5 to 14 years); positive responses were reported in 76% of patients and required a dose of at least 20 mg/day; mean final dose: 28.1 mg/day (1.1 mg/kg/day) (Dummitt 1996). Weight-based dosing has been reported in a double-blind placebo-controlled trial (treatment group: n=6; placebo: n=9; age: 6-12 years) using the following titration: 0.2 mg/kg/day for 1 week, then 0.4 mg/kg/day for 1 week, then 0.6 mg/kg/day for 10 weeks; mean final dose: 21.4 mg/day (Black 1994). To fully assess therapeutic response, a therapeutic trial of at least 9 to 12 weeks or longer has been suggested (Black 1994; Dummitt 1996; Kaakeh 2008).
Discontinuation of therapy: Consider planning antidepressant discontinuation for lower-stress times, recognizing non-illness-related factors could cause stress or anxiety and be misattributed to antidepressant discontinuation (Hathaway 2018). Upon discontinuation of antidepressant therapy, gradually taper the dose to minimize the incidence of discontinuation syndromes (withdrawal) and allow for the detection of reemerging disease state symptoms (eg, relapse). Evidence supporting ideal taper rates after illness remission is limited. APA and NICE guidelines suggest tapering therapy over at least several weeks with consideration to the half-life of the antidepressant; antidepressants with a shorter half-life may need to be tapered more conservatively. After long-term (years) antidepressant treatment, WFSBP guidelines recommend tapering over 4 to 6 months, with close monitoring during and for 6 months after discontinuation. If intolerable discontinuation symptoms occur following a dose reduction, consider resuming the previously prescribed dose and/or decrease dose at a more gradual rate (APA 2010; Bauer 2002; Fenske 2009; Haddad 2001; NCCMH 2010; Schatzberg 2006; Shelton 2001; Warner 2006).
MAO inhibitor recommendations:
Switching to or from an MAO inhibitor intended to treat psychiatric disorders:
Allow 14 days to elapse between discontinuing an MAO inhibitor intended to treat psychiatric disorders and initiation of fluoxetine.
Allow 5 weeks to elapse between discontinuing fluoxetine and initiation of an MAO inhibitor intended to treat psychiatric disorders.
Extemporaneously Prepared
Note: Commercial oral solution is available (4 mg/mL)
A 1 mg/mL fluoxetine oral solution may be prepared using the commercially available preparation (4 mg/mL). In separate graduated cylinders, measure 5 mL of the commercially available fluoxetine preparation and 15 mL of Simple Syrup, NF. Mix thoroughly in incremental proportions. For a 2 mg/mL solution, mix equal proportions of both the commercially available fluoxetine preparation and Simple Syrup, NF. Label "refrigerate". Both concentrations are stable for up to 56 days.
Nahata MC, Pai VB, and Hipple TF, Pediatric Drug Formulations, 5th ed, Cincinnati, OH: Harvey Whitney Books Co, 2004.
Administration
Administer without regard to meals.
Bipolar I disorder and treatment-resistant depression: Take once daily in the evening.
Major depressive disorder and obsessive compulsive disorder: Once daily doses should be taken in the morning, or twice daily (morning and noon).
Bulimia: Take once daily in the morning.
Storage
All dosage forms should be stored at controlled room temperature. Protect from light.
FLUoxetine Images
Drug Interactions
Abiraterone Acetate: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of abiraterone with CYP2D6 substrates that have a narrow therapeutic index whenever possible. When concurrent use is not avoidable, monitor patients closely for signs/symptoms of toxicity. Consider therapy modification
Acalabrutinib: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Agents with Antiplatelet Properties (e.g., P2Y12 inhibitors, NSAIDs, SSRIs, etc.): May enhance the antiplatelet effect of other Agents with Antiplatelet Properties. Monitor therapy
Ajmaline: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Ajmaline: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Ajmaline. Monitor therapy
Alcohol (Ethyl): May enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Management: Patients receiving selective serotonin reuptake inhibitors should be advised to avoid alcohol. Monitor for increased psychomotor impairment in patients who consume alcohol during treatment with selective serotonin reuptake inhibitors. Consider therapy modification
Almotriptan: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Alosetron: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Alpelisib: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Monitor therapy
Amphetamines: May enhance the serotonergic effect of Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors). This could result in serotonin syndrome. Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors) may increase the serum concentration of Amphetamines. Management: Monitor for increased amphetamine toxicities, including signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability) when these agents are combined. Monitor therapy
Anticoagulants: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Anticoagulants. Exceptions: Bemiparin; Enoxaparin; Heparin. Monitor therapy
Antiemetics (5HT3 Antagonists): May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Alosetron; Ondansetron; Ramosetron. Monitor therapy
Antipsychotic Agents: Serotonergic Agents (High Risk) may enhance the adverse/toxic effect of Antipsychotic Agents. Specifically, serotonergic agents may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotic Agents may enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Monitor therapy
Apixaban: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Apixaban. Specifically, the risk for bleeding may be increased. Management: Carefully consider risks and benefits of this combination and monitor closely. Monitor therapy
ARIPiprazole: FLUoxetine may enhance the adverse/toxic effect of ARIPiprazole. Specifically, the risk of neuroleptic malignant syndrome may be increased. ARIPiprazole may enhance the serotonergic effect of FLUoxetine. This could result in serotonin syndrome. FLUoxetine may increase the serum concentration of ARIPiprazole. Management: Aripiprazole dose should be reduced by at least half, except when used adjunctively for depression. Consult full interaction monograph or aripiprazole prescribing information for complete details. Consider therapy modification
ARIPiprazole Lauroxil: CYP2D6 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of ARIPiprazole Lauroxil. Management: Please refer to the full interaction monograph for details concerning the recommended dose adjustments. Consider therapy modification
Aspirin: Selective Serotonin Reuptake Inhibitors may enhance the antiplatelet effect of Aspirin. Monitor therapy
Asunaprevir: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Consider therapy modification
AtoMOXetine: CYP2D6 Inhibitors (Strong) may increase the serum concentration of AtoMOXetine. Management: Initiate atomoxetine at a reduced dose (adult doses -- patients up to 70kg: 0.5mg/kg/day; patients 70kg or more: 40mg/day) in patients receiving a strong CYP2D6 inhibitor. Consider therapy modification
Bemiparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Bemiparin. Management: Avoid concomitant use of bemiparin with antiplatelet agents. If concomitant use is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Benzhydrocodone: CYP2D6 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of Benzhydrocodone. Monitor therapy
Beta-Blockers: Selective Serotonin Reuptake Inhibitors may increase the serum concentration of Beta-Blockers. Exceptions: Acebutolol; Atenolol; Betaxolol (Ophthalmic); Betaxolol (Systemic); Bisoprolol; Carteolol (Ophthalmic); Esmolol; Labetalol; Levobunolol; Metipranolol; Nadolol; Sotalol. Monitor therapy
Blood Glucose Lowering Agents: Selective Serotonin Reuptake Inhibitors may enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Brexanolone: Selective Serotonin Reuptake Inhibitors may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brexpiprazole: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Brexpiprazole. Management: Reduce brexpiprazole dose to 50% of usual with a strong CYP2D6 inhibitor, reduce to 25% of usual if used with both a strong CYP2D6 inhibitor and a CYP3A4 inhibitor; these recommendations do not apply if treating major depressive disorder. Consider therapy modification
Bromopride: May enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Avoid combination
BuPROPion: FLUoxetine may enhance the neuroexcitatory and/or seizure-potentiating effect of BuPROPion. BuPROPion may increase the serum concentration of FLUoxetine. Monitor therapy
BusPIRone: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Cannabidiol: CYP2C19 Inhibitors (Moderate) may increase the serum concentration of Cannabidiol. Monitor therapy
CarBAMazepine: FLUoxetine may increase the serum concentration of CarBAMazepine. Monitor therapy
Cephalothin: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Cephalothin. Specifically, the risk for bleeding may be increased. Monitor therapy
Cilostazol: CYP2C19 Inhibitors (Moderate) may increase serum concentrations of the active metabolite(s) of Cilostazol. CYP2C19 Inhibitors (Moderate) may increase the serum concentration of Cilostazol. Management: Reduce the cilostazol dose to 50 mg twice daily in patients who are also receiving moderate inhibitors of CYP2C19. Monitor clinical response to cilostazol closely. Consider therapy modification
Cimetidine: May increase the serum concentration of FLUoxetine. Monitor therapy
Citalopram: May enhance the antiplatelet effect of FLUoxetine. Citalopram may enhance the serotonergic effect of FLUoxetine. This could result in serotonin syndrome. FLUoxetine may increase the serum concentration of Citalopram. Management: Limit citalopram dose to a maximum of 20 mg/day. Monitor for signs and symptoms of bleeding, QTc interval prolongation, or serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor) if combined. Consider therapy modification
Clarithromycin: FLUoxetine may enhance the QTc-prolonging effect of Clarithromycin. Clarithromycin may increase the serum concentration of FLUoxetine. Monitor therapy
CloBAZam: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Clopidogrel: CYP2C19 Inhibitors (Moderate) may decrease serum concentrations of the active metabolite(s) of Clopidogrel. Management: Due to a risk for impaired clopidogrel effectiveness with such a combination, carefully consider the need for a moderate CYP2C19 inhibitor in patients receiving clopidogrel. Monitor patients closely for evidence of a diminished response to clopidogrel. Consider therapy modification
CloZAPine: CYP2D6 Inhibitors (Strong) may increase the serum concentration of CloZAPine. Monitor therapy
CNS Depressants: May enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Cobicistat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Codeine: CYP2D6 Inhibitors (Strong) may diminish the therapeutic effect of Codeine. These CYP2D6 inhibitors may prevent the metabolic conversion of codeine to its active metabolite morphine. Consider therapy modification
Collagenase (Systemic): Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Collagenase (Systemic). Specifically, the risk of injection site bruising and/or bleeding may be increased. Monitor therapy
Cyclobenzaprine: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
CYP2C19 Substrates (High risk with Inhibitors): CYP2C19 Inhibitors (Moderate) may decrease the metabolism of CYP2C19 Substrates (High risk with Inhibitors). Monitor therapy
CYP2C9 Inducers (Moderate): May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Monitor therapy
CYP2C9 Inhibitors (Moderate): May decrease the metabolism of CYP2C9 Substrates (High risk with Inhibitors). Monitor therapy
CYP2D6 Inhibitors (Moderate): May decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CYP2D6 Inhibitors (Strong): May decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Consider therapy modification
CYP2D6 Substrates (High risk with Inhibitors): CYP2D6 Inhibitors (Strong) may decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Exceptions: Ajmaline; Dapoxetine; Indoramin; Metoprolol; Tamoxifen; Timolol (Ophthalmic); Tropisetron. Consider therapy modification
Cyproheptadine: May diminish the therapeutic effect of Selective Serotonin Reuptake Inhibitors. Monitor therapy
Dabigatran Etexilate: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Dabigatran Etexilate. Agents with Antiplatelet Properties may increase the serum concentration of Dabigatran Etexilate. This mechanism applies specifically to clopidogrel. Management: Carefully consider risks and benefits of this combination and monitor closely; Canadian labeling recommends avoiding prasugrel or ticagrelor. Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP2C9 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dacomitinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of dacomitinib with CYP2D6 subtrates that have a narrow therapeutic index. Consider therapy modification
Dapoxetine: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Do not use serotonergic agents (high risk) with dapoxetine or within 7 days of serotonergic agent discontinuation. Do not use dapoxetine within 14 days of monoamine oxidase inhibitor use. Dapoxetine labeling lists this combination as contraindicated. Avoid combination
Darunavir: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Dasatinib: May enhance the anticoagulant effect of Agents with Antiplatelet Properties. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Deoxycholic Acid: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Deoxycholic Acid. Specifically, the risk for bleeding or bruising in the treatment area may be increased. Monitor therapy
Desmopressin: Selective Serotonin Reuptake Inhibitors may enhance the adverse/toxic effect of Desmopressin. Monitor therapy
Deutetrabenazine: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Deutetrabenazine. Management: The total daily dose of deutetrabenazine should not exceed 36 mg, and the maximum single dose of deutetrabenazine should not exceed 18 mg with concurrent use of a strong CYP2D6 inhibitor. Consider therapy modification
Dexmethylphenidate-Methylphenidate: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Dextromethorphan: May enhance the serotonergic effect of Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors). This could result in serotonin syndrome. Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors) may increase the serum concentration of Dextromethorphan. Management: Consider alternatives to this drug combination. If combined, monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes). Consider therapy modification
DOXOrubicin (Conventional): CYP2D6 Inhibitors (Strong) may increase the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to strong CYP2D6 inhibitors in patients treated with doxorubicin whenever possible. One U.S. manufacturer (Pfizer Inc.) recommends that these combinations be avoided. Consider therapy modification
DULoxetine: May enhance the antiplatelet effect of Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors). DULoxetine may enhance the serotonergic effect of Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors). This could result in serotonin syndrome. Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors) may increase the serum concentration of DULoxetine. Management: Monitor for increased duloxetine effects/toxicities and signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperthermia, tremor, mental status changes) when these agents are combined. In addition, monitor for signs and symptoms of bleeding. Monitor therapy
Edoxaban: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Edoxaban. Specifically, the risk of bleeding may be increased. Monitor therapy
Eletriptan: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Eliglustat: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Eliglustat. Management: Reduce the eliglustat dose to 84 mg daily. Avoid use of eliglustat in combination with a strong CYP2D6 inhibitor and a strong or moderate CYP3A4 inhibitor. Consider therapy modification
Enoxaparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Enoxaparin. Management: Discontinue antiplatelet agents prior to initiating enoxaparin whenever possible. If concomitant administration is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Enzalutamide: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP2C9 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP2C9 substrate should be performed with caution and close monitoring. Consider therapy modification
Ergot Derivatives: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Nicergoline. Monitor therapy
Fat Emulsion (Fish Oil Based): May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Monitor therapy
Fesoterodine: CYP2D6 Inhibitors may increase serum concentrations of the active metabolite(s) of Fesoterodine. Monitor therapy
Flibanserin: CYP2C19 Inhibitors (Moderate) may increase the serum concentration of Flibanserin. Monitor therapy
Fosphenytoin: May enhance the QTc-prolonging effect of FLUoxetine. FLUoxetine may increase the serum concentration of Fosphenytoin. Consider therapy modification
Galantamine: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Galantamine. Monitor therapy
Gilteritinib: May diminish the therapeutic effect of Selective Serotonin Reuptake Inhibitors. Management: Avoid use of this combination if possible. If the combination cannot be avoided, monitor closely for evidence of reduced response to the selective serotonin reuptake inhibitor. Consider therapy modification
Glucosamine: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Haloperidol: FLUoxetine may enhance the QTc-prolonging effect of Haloperidol. FLUoxetine may increase the serum concentration of Haloperidol. Monitor therapy
Heparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Heparin. Management: Decrease the dose of heparin or agents with antiplatelet properties if coadministration is required. Consider therapy modification
Herbs (Anticoagulant/Antiplatelet Properties) (eg, Alfalfa, Anise, Bilberry): May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Bleeding may occur. Management: Avoid combination when possible. If used, monitor more closely for evidence of bleeding. Discontinue herbal products with anticoagulant or antiplatelet actions 2 weeks prior to surgical, dental, or invasive procedures. Consider therapy modification
HYDROcodone: CYP2D6 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of HYDROcodone. Specifically, concentrations of hydromorphone may be decreased. Monitor therapy
Ibritumomab Tiuxetan: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Ibritumomab Tiuxetan. Both agents may contribute to impaired platelet function and an increased risk of bleeding. Monitor therapy
Ibrutinib: May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Monitor therapy
Iloperidone: CYP2D6 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Iloperidone. Specifically, concentrations of the metabolite P88 may be increased. CYP2D6 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of Iloperidone. Specifically, concentrations of the metabolite P95 may be decreased. CYP2D6 Inhibitors (Strong) may increase the serum concentration of Iloperidone. Management: Reduce iloperidone dose by half when administered with a strong CYP2D6 inhibitor. Consider therapy modification
Imatinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Indoramin: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Indoramin. Monitor therapy
Inotersen: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Ioflupane I 123: Selective Serotonin Reuptake Inhibitors may diminish the diagnostic effect of Ioflupane I 123. Monitor therapy
Lasmiditan: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Limaprost: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Linezolid: May enhance the serotonergic effect of Selective Serotonin Reuptake Inhibitors. This could result in serotonin syndrome. Avoid combination
Lofexidine: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Lofexidine. Monitor therapy
Lorcaserin: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Lumacaftor and Ivacaftor: May decrease the serum concentration of CYP2C9 Substrates (High Risk with Inhibitors or Inducers). Lumacaftor and Ivacaftor may increase the serum concentration of CYP2C9 Substrates (High Risk with Inhibitors or Inducers). Monitor therapy
Lumefantrine: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Mequitazine: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Mequitazine. Avoid combination
Metaxalone: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Methylene Blue: Selective Serotonin Reuptake Inhibitors may enhance the serotonergic effect of Methylene Blue. This could result in serotonin syndrome. Avoid combination
Metoclopramide: May enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Management: Seek alternatives to this combination when possible. Monitor patients receiving metoclopramide with selective serotonin reuptake inhibitors for signs of extrapyramidal symptoms, neuroleptic malignant syndrome, and serotonin syndrome. Consider therapy modification
Metoclopramide: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Metoclopramide. Management: Reduce metoclopramide dose to 5 mg 4 times daily (30 minutes before each meal and at bedtime) and limit the maximum daily dose to 20 mg if combined with strong CYP2D6 inhibitors. Consider therapy modification
Metoprolol: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Metoprolol. Monitor therapy
MetyroSINE: May enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Monitor therapy
MiFEPRIStone: May increase the serum concentration of CYP2C9 Substrates (High risk with Inhibitors). Management: Use CYP2C9 substrates at the lowest recommended dose, and monitor closely for adverse effects, during and in the 2 weeks following mifepristone treatment. Consider therapy modification
Monoamine Oxidase Inhibitors (Antidepressant): Selective Serotonin Reuptake Inhibitors may enhance the serotonergic effect of Monoamine Oxidase Inhibitors (Antidepressant). This could result in serotonin syndrome. Avoid combination
Multivitamins/Fluoride (with ADE): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Multivitamins/Minerals (with AE, No Iron): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Nebivolol: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Nebivolol. Monitor therapy
Nefazodone: May enhance the serotonergic effect of Selective Serotonin Reuptake Inhibitors. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Nicergoline: CYP2D6 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Nicergoline. Specifically, concentrations of the MMDL metabolite may be increased. CYP2D6 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of Nicergoline. Specifically, concentrations of the MDL metabolite may be decreased. Monitor therapy
NIFEdipine: FLUoxetine may enhance the adverse/toxic effect of NIFEdipine. Monitor therapy
NiMODipine: FLUoxetine may increase the serum concentration of NiMODipine. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective): Selective Serotonin Reuptake Inhibitors may enhance the antiplatelet effect of Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective). Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective) may diminish the therapeutic effect of Selective Serotonin Reuptake Inhibitors. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents (Nonselective): Selective Serotonin Reuptake Inhibitors may enhance the antiplatelet effect of Nonsteroidal Anti-Inflammatory Agents (Nonselective). Nonsteroidal Anti-Inflammatory Agents (Nonselective) may diminish the therapeutic effect of Selective Serotonin Reuptake Inhibitors. Management: Consider alternatives to NSAIDs. Monitor for evidence of bleeding and diminished antidepressant effects. It is unclear whether COX-2-selective NSAIDs reduce risk. Exceptions: Diclofenac (Topical); Ibuprofen (Topical); Piroxicam (Topical). Consider therapy modification
Nonsteroidal Anti-Inflammatory Agents (Topical): May enhance the antiplatelet effect of Selective Serotonin Reuptake Inhibitors. Monitor therapy
Obinutuzumab: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Obinutuzumab. Specifically, the risk of serious bleeding-related events may be increased. Monitor therapy
Omega-3 Fatty Acids: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Ondansetron: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Opioid Agonists: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: FentaNYL; Meperidine; TraMADol. Monitor therapy
Oxitriptan: Serotonergic Agents (High Risk) may enhance the serotonergic effect of Oxitriptan. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Panobinostat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
PARoxetine: FLUoxetine may enhance the antiplatelet effect of PARoxetine. FLUoxetine may enhance the serotonergic effect of PARoxetine. This could result in serotonin syndrome. FLUoxetine may increase the serum concentration of PARoxetine. PARoxetine may increase the serum concentration of FLUoxetine. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, mental status changes), bleeding, and increased SSRI toxicities when these agents are combined. Monitor therapy
Peginterferon Alfa-2b: May decrease the serum concentration of FLUoxetine. Monitor therapy
Pentosan Polysulfate Sodium: May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Specifically, the risk of bleeding may be increased by concurrent use of these agents. Monitor therapy
Pentoxifylline: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Perhexiline: CYP2D6 Inhibitors may increase the serum concentration of Perhexiline. Management: Consider alternatives to this combination if possible. If combined, monitor for increased perhexiline serum concentrations and toxicities (eg, hypoglycemia, neuropathy, liver dysfunction). Perhexiline dose reductions will likely be required. Consider therapy modification
Phenytoin: FLUoxetine may increase the serum concentration of Phenytoin. Monitor therapy
Pimozide: FLUoxetine may enhance the QTc-prolonging effect of Pimozide. FLUoxetine may increase the serum concentration of Pimozide. Avoid combination
Pitolisant: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Pitolisant. Management: Reduce the pitolisant dose by 50% if a strong CYP2D6 inhibitor is initiated. For patients receiving strong CYP2D6 inhibitors, initiate pitolisant at 8.9 mg once daily and increase after 7 days to a maximum of 17.8 mg once daily. Consider therapy modification
Primaquine: CYP2D6 Inhibitors (Strong) may diminish the therapeutic effect of Primaquine. Management: Monitor for signs and symptoms of possible treatment failure with primaquine in patients who are taking strong CYP2D6 inhibitors. If efficacy of primaquine is compromised, may consider adjusting therapies. Consider therapy modification
Propafenone: May enhance the QTc-prolonging effect of FLUoxetine. FLUoxetine may increase the serum concentration of Propafenone. Monitor therapy
Prostacyclin Analogues: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
QT-prolonging Agents (Highest Risk): QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QuiNINE: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Ramosetron: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Rasagiline: Selective Serotonin Reuptake Inhibitors may enhance the serotonergic effect of Rasagiline. This could result in serotonin syndrome. Avoid combination
Rifapentine: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Monitor therapy
Rivaroxaban: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Rivaroxaban. Management: Carefully consider risks and benefits of this combination and monitor closely; Canadian labeling recommends avoiding prasugrel or ticagrelor. Monitor therapy
Safinamide: May enhance the serotonergic effect of Selective Serotonin Reuptake Inhibitors. This could result in serotonin syndrome. Management: Use the lowest effective dose of SSRIs in patients treated with safinamide and monitor for signs and symptoms of serotonin syndrome/serotonin toxicity. Consider therapy modification
Salicylates: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Salicylates. Increased risk of bleeding may result. Monitor therapy
Selective Serotonin Reuptake Inhibitors: May enhance the antiplatelet effect of other Selective Serotonin Reuptake Inhibitors. Selective Serotonin Reuptake Inhibitors may enhance the serotonergic effect of other Selective Serotonin Reuptake Inhibitors. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, mental status changes) when these agents are combined. In addition, monitor for signs and symptoms of bleeding. Exceptions: Citalopram; Dapoxetine; Vortioxetine. Monitor therapy
Selegiline: Selective Serotonin Reuptake Inhibitors may enhance the serotonergic effect of Selegiline. This could result in serotonin syndrome. Avoid combination
Serotonergic Agents (High Risk, Miscellaneous): May enhance the serotonergic effect of Selective Serotonin Reuptake Inhibitors. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Serotonergic Non-Opioid CNS Depressants: Selective Serotonin Reuptake Inhibitors may enhance the serotonergic effect of Serotonergic Non-Opioid CNS Depressants. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Serotonergic Opioids (High Risk): May enhance the serotonergic effect of Selective Serotonin Reuptake Inhibitors. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) if these agents are combined. Exceptions: TraMADol. Monitor therapy
Serotonin 5-HT1D Receptor Agonists (Triptans): May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Almotriptan; Eletriptan. Monitor therapy
Serotonin/Norepinephrine Reuptake Inhibitors: Selective Serotonin Reuptake Inhibitors may enhance the antiplatelet effect of Serotonin/Norepinephrine Reuptake Inhibitors. Selective Serotonin Reuptake Inhibitors may enhance the serotonergic effect of Serotonin/Norepinephrine Reuptake Inhibitors. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, mental status changes) when these agents are combined. In addition, monitor for signs and symptoms of bleeding. Exceptions: DULoxetine. Monitor therapy
St John's Wort: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. St John's Wort may decrease the serum concentration of Serotonergic Agents (High Risk). Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Syrian Rue: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Tamoxifen: CYP2D6 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of Tamoxifen. Specifically, strong CYP2D6 inhibitors may decrease the metabolic formation of highly potent active metabolites. Avoid combination
Tamsulosin: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Tamsulosin. Monitor therapy
Tetrabenazine: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Tetrabenazine. Specifically, concentrations of the active alpha- and beta-dihydrotetrabenazine metabolites may be increased. Management: Tetrabenazine adult dose should be reduced by 50% when starting a strong CYP2D6 inhibitor. Maximum tetrabenazine adult dose is 50 mg/day when used with a strong CYP2D6 inhibitor. Consider therapy modification
Thiazide and Thiazide-Like Diuretics: Selective Serotonin Reuptake Inhibitors may enhance the hyponatremic effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Thioridazine: FLUoxetine may enhance the QTc-prolonging effect of Thioridazine. FLUoxetine may increase the serum concentration of Thioridazine. Avoid combination
Thrombolytic Agents: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Thrombolytic Agents. Monitor therapy
Thyroid Products: Selective Serotonin Reuptake Inhibitors may diminish the therapeutic effect of Thyroid Products. Thyroid product dose requirements may be increased. Monitor therapy
Timolol (Ophthalmic): CYP2D6 Inhibitors (Strong) may increase the serum concentration of Timolol (Ophthalmic). Monitor therapy
TraMADol: Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors) may enhance the adverse/toxic effect of TraMADol. Specifically, the risk for serotonin syndrome/serotonin toxicity and seizures may be increased. Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors) may diminish the therapeutic effect of TraMADol. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes), seizures, and decreased tramadol efficacy when these agents are combined. Monitor therapy
Tricyclic Antidepressants: FLUoxetine may enhance the serotonergic effect of Tricyclic Antidepressants. FLUoxetine may increase the serum concentration of Tricyclic Antidepressants. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and increased TCA concentrations/effects if these agents are combined. Consider therapy modification
Tropisetron: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Tropisetron. Monitor therapy
Urokinase: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Urokinase. Avoid combination
Valbenazine: CYP2D6 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Valbenazine. Monitor therapy
Vitamin E (Systemic): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Selective Serotonin Reuptake Inhibitors may enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Vortioxetine: Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors) may enhance the antiplatelet effect of Vortioxetine. Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors) may enhance the serotonergic effect of Vortioxetine. This could result in serotonin syndrome. Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors) may increase the serum concentration of Vortioxetine. Management: Consider alternatives to this drug combination. If combined, reduce the vortioxetine dose by half and monitor for signs and symptoms of bleeding and serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, autonomic instability). Consider therapy modification
Zanubrutinib: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Adverse Reactions
As reported in adults, unless otherwise noted.
>10%:
Central nervous system: Insomnia (10% to 33%), headache (21%), drowsiness (5% to 17%), anxiety (6% to 15%), nervousness (8% to 14%), yawning (≤11%)
Endocrine & metabolic: Decreased libido (4% to 11%)
Gastrointestinal: Nausea (12% to 29%), diarrhea (8% to 18%), anorexia (4% to 17%), xerostomia (9% to 12%)
Neuromuscular & skeletal: Weakness (9% to 21%), tremor (3% to 13%)
Respiratory: Pharyngitis (10% to 11%)
1% to 10%:
Cardiovascular: Vasodilation (1% to 5%), palpitations (≥1%), prolonged Q-T interval on ECG (≥1%; QTcF ≥450 msec3), chest pain, hypertension
Central nervous system: Dizziness (9%), abnormal dreams (5%), agitation (children and adolescents: ≥2%), personality disorder (children and adolescents: ≥2%), abnormality in thinking (2%), chills (≥1%), emotional lability (≥1%), amnesia, confusion, sleep disorder
Dermatologic: Diaphoresis (7% to 8%), skin rash (4% to 6%), pruritus (3%)
Endocrine & metabolic: Hypermenorrhea (children and adolescents: ≥2%), increased thirst (children and adolescents: ≥2%), weight loss (2%), weight gain
Gastrointestinal: Dyspepsia (6% to 10%), constipation (5%), flatulence (3%), vomiting (3%), dysgeusia (≥1%), increased appetite
Genitourinary: Ejaculatory disorder (≤7%), impotence (≤7%), urinary frequency (children and adolescents: ≥2%), urination disorder (≥1%)
Neuromuscular & skeletal: Hyperkinesia (children and adolescents: ≥2%)
Ophthalmic: Visual disturbance (2%)
Otic: Otalgia, tinnitus
Respiratory: Flu-like symptoms (8% to 10%), sinusitis (5% to 6%), epistaxis (children and adolescents: ≥2%)
<1%, postmarketing, and/or case reports: Abnormal hepatic function tests, acne vulgaris, acute abdominal condition, akathisia, albuminuria, alopecia, amenorrhea, anaphylactoid reaction, anemia, angina pectoris, angle-closure glaucoma, aphthous stomatitis, aplastic anemia, arthritis, asthma, ataxia, atrial fibrillation, bruise, bruxism, bursitis, cardiac arrhythmia, cardiac failure, cataract, cerebrovascular accident, cholelithiasis, cholestatic jaundice, colitis, dehydration, delusions, depersonalization, dyskinesia, dysphagia, dysuria, ecchymoses, edema, eosinophilic pneumonitis, equilibrium disturbance, erythema multiforme, erythema nodosum, esophagitis, euphoria, exfoliative dermatitis, extrapyramidal reaction (rare), gastritis, gastroenteritis, gastrointestinal ulcer, glossitis, gout, gynecological bleeding, gynecomastia, hallucination, hemolytic anemia (immune-related), hepatic failure, hepatic necrosis, hepatitis, hiccups, hostility, hypercholesteremia, hyperprolactinemia, hypersensitivity reaction, hypertonia, hyperventilation, hypoglycemia, hypokalemia, hyponatremia (possibly in association with SIADH), hypotension, hypothyroidism, immune thrombocytopenia, laryngeal edema, laryngospasm, leg cramps, lupus-like syndrome, malaise, melena, memory impairment, migraine, mydriasis, myocardial infarction, myoclonus, neuroleptic malignant syndrome (Stevens 2008), optic neuritis, orthostatic hypotension, ostealgia, pancreatitis, pancytopenia, paranoia, petechia, priapism, pulmonary embolism, pulmonary fibrosis, pulmonary hypertension, purpuric rash, renal failure, serotonin syndrome, sexual disorder (may persist after discontinuation), skin photosensitivity, Stevens-Johnson syndrome, suicidal ideation, syncope, tachycardia, thrombocytopenia, toxic epidermal necrolysis, vasculitis, ventricular tachycardia (including torsades de pointes), violent behavior
Warnings/Precautions
Major psychiatric warnings:
- Suicidal thinking/behavior: [US Boxed Warning]: Antidepressants increase the risk of suicidal thinking and behavior in children, adolescents, and young adults (18 to 24 years of age) with major depressive disorder (MDD) and other psychiatric disorders; consider risk prior to prescribing. Short-term studies did not show an increased risk in patients >24 years of age and showed a decreased risk in patients ≥65 years. Closely monitor all patients for clinical worsening, suicidality, or unusual changes in behavior, particularly during the initial 1 to 2 months of therapy or during periods of dosage adjustments (increases or decreases); the patient’s family or caregiver should be instructed to closely observe the patient and communicate condition with health care provider. A medication guide concerning the use of antidepressants should be dispensed with each prescription. Fluoxetine is FDA approved for the treatment of OCD in children ≥7 years of age and MDD in children ≥8 years of age.
- The possibility of a suicide attempt is inherent in major depression and may persist until remission occurs. Worsening depression and severe abrupt suicidality that are not part of the presenting symptoms may require discontinuation or modification of drug therapy. Use caution in high-risk patients during initiation of therapy.
- Prescriptions should be written for the smallest quantity consistent with good patient care. The patient's family or caregiver should be alerted to monitor patients for the emergence of suicidality and associated behaviors such as anxiety, agitation, panic attacks, insomnia, irritability, hostility, impulsivity, akathisia, hypomania, and mania; patients should be instructed to notify their health care provider if any of these symptoms or worsening depression occur.
Concerns related to adverse effects:
- Allergic events and rash: Fluoxetine use has been associated with occurrences of significant rash and allergic events, including vasculitis, lupus-like syndrome, laryngospasm, anaphylactoid reactions, and pulmonary inflammatory disease. Discontinue if underlying cause of rash cannot be identified.
- Bleeding risk: May impair platelet aggregation resulting in increased risk of bleeding events, particularly if used concomitantly with aspirin, NSAIDs, warfarin or other anticoagulants. Bleeding related to SSRI use has been reported to range from relatively minor bruising and epistaxis to life-threatening hemorrhage.
- CNS depression: Has a low potential to impair cognitive or motor performance; caution operating hazardous machinery or driving.
- CNS effects: May cause insomnia, anxiety, nervousness, or anorexia.
- Fractures: Bone fractures have been associated with antidepressant treatment. Consider the possibility of a fragility fracture if an antidepressant-treated patient presents with unexplained bone pain, point tenderness, swelling, or bruising (Rabenda 2013; Rizzoli 2012).
- Ocular effects: May cause mild pupillary dilation, which in susceptible individuals can lead to an episode of narrow-angle glaucoma. Consider evaluating patients who have not had an iridectomy for narrow-angle glaucoma risk factors.
- QT prolongation: QT prolongation and ventricular arrhythmia including torsades de pointes has occurred. Use with caution in patients with risk factors for QT prolongation (eg, congenital long QT syndrome, history of prolonged QT, family history of prolonged QT or sudden cardiac death), other conditions that predispose to arrhythmias (eg, hypokalemia, hypomagnesemia, recent MI, uncompensated heart failure, bradyarrhythmias or other arrhythmias, concomitant use of other agents that prolong QT interval), or increased fluoxetine exposure (eg, overdose, hepatic impairment, use of CYP2D6 inhibitors, poor CYP2D6 metabolizer status, concomitant use of other highly protein-bound drugs). Consider ECG monitoring when initiating therapy in patients with risk factors for QT prolongation and ventricular arrhythmia. Consider discontinuing fluoxetine if ventricular arrhythmia suspected and initiate cardiac evaluation.
- Serotonin syndrome: Potentially life-threatening serotonin syndrome (SS) has occurred with serotonergic agents (eg, SSRIs, SNRIs), particularly when used in combination with other serotonergic agents (eg, triptans, TCAs, fentanyl, lithium, tramadol, buspirone, St John's wort, tryptophan) or agents that impair metabolism of serotonin (eg, MAO inhibitors intended to treat psychiatric disorders, other MAO inhibitors [ie, linezolid and intravenous methylene blue]). Monitor patients closely for signs of SS such as mental status changes (eg, agitation, hallucinations, delirium, coma); autonomic instability (eg, tachycardia, labile blood pressure, diaphoresis); neuromuscular changes (eg, tremor, rigidity, myoclonus); GI symptoms (eg, nausea, vomiting, diarrhea); and/or seizures. Discontinue treatment (and any concomitant serotonergic agent) immediately if signs/symptoms arise.
- Sexual dysfunction: May cause or exacerbate sexual dysfunction.
- SIADH and hyponatremia: SSRIs and SNRIs have been associated with the development of SIADH; hyponatremia has been reported rarely (including severe cases with serum sodium <110 mmol/L), predominately in the elderly. Volume depletion and/or concurrent use of diuretics likely increases risk. Consider discontinuation if symptomatic hyponatremia occurs.
- Weight loss: May cause anorexia and/or weight loss. Use caution in patients where weight loss is undesirable.
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with a history of MI or unstable heart disease; experience in these patients is limited.
- Diabetes: Use with caution in patients with diabetes mellitus; may alter glycemic control and may require adjustment of antidiabetic medication; hypoglycemia and hyperglycemia has been observed during and after cessation of therapy, respectively.
- Hepatic impairment: Use with caution in patients with hepatic impairment; clearance is decreased and plasma concentrations are increased; a lower dosage may be needed in patients with cirrhosis.
- Mania/hypomania: May worsen psychosis in some patients or precipitate a shift to mania or hypomania in patients with bipolar disorder. Monotherapy in patients with bipolar disorder should be avoided. Patients presenting with depressive symptoms should be screened for bipolar disorder. Fluoxetine monotherapy is not FDA approved for the treatment of bipolar depression.
- Renal impairment: Use with caution in patients with severe renal impairment; a lower dosage or less frequent dosing may be needed.
- Seizure disorders: Use with caution in patients with a previous seizure disorder or conditions predisposing to seizures such as brain damage or alcoholism.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: May also cause agitation, sleep disturbances, and excessive CNS stimulation in older adults. Given the long half-life and nonlinear disposition of the drug, use caution, particularly if they have systemic illness or are receiving multiple drugs for concomitant diseases.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol derivative with caution in neonates. See manufacturer’s labeling.
Other warnings/precautions:
- Discontinuation syndrome: Abrupt discontinuation or interruption of antidepressant therapy has been associated with a discontinuation syndrome. Symptoms arising may vary with antidepressant however commonly include nausea, vomiting, diarrhea, headaches, light-headedness, dizziness, diminished appetite, sweating, chills, tremors, paresthesias, fatigue, somnolence, and sleep disturbances (eg, vivid dreams, insomnia). Less common symptoms include electric shock-like sensations, cardiac arrhythmias (more common with tricyclic antidepressants), myalgias, parkinsonism, arthralgias, and balance difficulties. Psychological symptoms may also emerge such as agitation, anxiety, akathisia, panic attacks, irritability, aggressiveness, worsening of mood, dysphoria, mood lability, hyperactivity, mania/hypomania, depersonalization, decreased concentration, slowed thinking, confusion, and memory or concentration difficulties. Greater risks for developing a discontinuation syndrome have been associated with antidepressants with shorter half-lives, longer durations of treatment, and abrupt discontinuation. For antidepressants of short or intermediate half-lives, symptoms may emerge within 2 to 5 days after treatment discontinuation and last 7 to 14 days (APA 2010; Fava 2006; Haddad 2001; Shelton 2001; Warner 2006).
- Electroconvulsive therapy: May increase the risks associated with electroconvulsive therapy; consider discontinuing, when possible, prior to ECT treatment.
- Long half-life: Due to the long half-life of fluoxetine and its metabolites, the effects and interactions noted may persist for prolonged periods following discontinuation.
Monitoring Parameters
Serum sodium in at-risk populations (as clinically indicated); blood glucose (for diabetic patients); liver and renal function (baseline and as clinically indicated); ECG assessment and periodic monitoring in patients with risk factors for QT prolongation and ventricular arrhythmia; mental status for depression, suicidal ideation (especially at the beginning of therapy or when doses are increased or decreased), anxiety, social functioning, mania, panic attacks; signs/symptoms of serotonin syndrome; akathisia; sleep status
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Adverse events have been observed in animal reproduction studies. Fluoxetine and its metabolite cross the human placenta. Available studies evaluating teratogenic effects following maternal use of fluoxetine in the first trimester have shown inconsistent results. An increased risk of cardiovascular events was observed in one study; however, no specific pattern was observed and a causal relationship has not been established. Nonteratogenic effects in the newborn following SSRI/SNRI exposure late in the third trimester include respiratory distress, cyanosis, apnea, seizures, temperature instability, feeding difficulty, vomiting, hypoglycemia, hypo- or hypertonia, hyper-reflexia, jitteriness, irritability, constant crying, and tremor. Symptoms may be due to the toxicity of the SSRIs/SNRIs or a discontinuation syndrome and may be consistent with serotonin syndrome associated with SSRI treatment. Persistent pulmonary hypertension of the newborn (PPHN) has also been reported with SSRI exposure. The long-term effects of in utero SSRI exposure on infant development and behavior are not known.
Due to pregnancy-induced physiologic changes, women who are pregnant may require dose adjustments of fluoxetine to achieve euthymia. The ACOG recommends that therapy with SSRIs or SNRIs during pregnancy be individualized; treatment of depression during pregnancy should incorporate the clinical expertise of the mental health clinician, obstetrician, primary health care provider, and pediatrician. According to the American Psychiatric Association (APA), the risks of medication treatment should be weighed against other treatment options and untreated depression. For women who discontinue antidepressant medications during pregnancy and who may be at high risk for postpartum depression, the medications can be restarted following delivery. Treatment algorithms have been developed by the ACOG and the APA for the management of depression in women prior to conception and during pregnancy.
Pregnant women exposed to antidepressants during pregnancy are encouraged to enroll in the National Pregnancy Registry for Antidepressants (NPRAD). Women 18 to 45 years of age or their health care providers may contact the registry by calling 844-405-6185. Enrollment should be done as early in pregnancy as possible.
Patient Education
What is this drug used for?
- It is used to treat low mood (depression).
- It is used to treat obsessive-compulsive problems.
- It is used to treat mood problems caused by monthly periods.
- It is used to treat eating problems.
- It is used to treat panic attacks.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Nausea
- Vomiting
- Lack of appetite
- Dry mouth
- Fatigue
- Diarrhea
- Nightmares
- Trouble sleeping
- Loss of strength and energy
- Hot flashes
- Flu-like symptoms
- Yawning
- Tremors
- Sweating a lot
- Headache
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Depression like thoughts of suicide, anxiety, emotional instability, or confusion.
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Low sodium like headache, difficulty focusing, trouble with memory, confusion, weakness, seizures, or change in balance.
- Agitation
- Irritability
- Panic attacks
- Behavioral changes
- Mood changes
- Passing out
- Fast heartbeat
- Abnormal heartbeat
- Dizziness
- Excessive weight gain
- Excessive weight loss
- Sexual dysfunction
- Decreased sex drive
- Increased thirst
- Seizures
- Slow heartbeat
- Bruising
- Bleeding
- Anxiety
- Menstrual changes
- Passing a lot of urine
- Change in amount of urine passed
- Abnormal movements
- Eye redness
- Eye edema
- Vision changes
- Eye pain
- Serotonin syndrome like dizziness, severe headache, agitation, sensing things that seem real but are not, fast heartbeat, abnormal heartbeat, flushing, tremors, sweating a lot, change in balance, severe nausea, prescriber or severe diarrhea.
- Erection that lasts more than 4 hours
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.