Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Nebulization Solution, Inhalation, as fumarate dihydrate:
Perforomist: 20 mcg/2 mL (2 mL)
Pharmacology
Mechanism of Action
Relaxes bronchial smooth muscle by selective action on beta2 receptors with little effect on heart rate. Formoterol has a long-acting effect.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapidly into plasma
Metabolism
Hepatic via direct glucuronidation and O-demethylation; CYP2D6, CYP2C19, CYP2C8/9, CYP2A6 involved in O-demethylation
Excretion
Children 5-12 years: Urine (6% as unchanged drug, 7% to 9% as direct glucuronide metabolites)
Adults: Urine (15% to 18% as direct glucuronide metabolites, 2% to 10% as unchanged drug)
Onset of Action
Dry powder inhaler: Within 3 minutes.
Peak effect: Dry powder inhaler: 80% of peak effect within 15 minutes; Nebulization solution: 2 hours.
Time to Peak
Maximum improvement in FEV1 in 1-3 hours
Duration of Action
Improvement in FEV1 observed for 12 hours in most patients
Half-Life Elimination
Dry powder inhaler: ~10 to 14 hours; Nebulization solution: ~7 hours.
Protein Binding
61% to 64% in vitro at higher concentrations than achieved with usual dosing
Use: Labeled Indications
US labeling:
Asthma: Treatment of asthma (only as concomitant therapy with an inhaled corticosteroid) in patients with reversible obstructive airway disease, including patients with symptoms of nocturnal asthma (Foradil Aerolizer).
Chronic obstructive pulmonary disease (COPD): Maintenance treatment of bronchoconstriction in patients with COPD (Foradil Aerolizer, Perforomist).
Exercise-induced bronchospasm: Prevention of exercise-induced bronchospasm when administered on an as-needed basis (monotherapy may be indicated in patients without persistent asthma) (Foradil Aerolizer).
Canadian labeling:
Asthma: Treatment of asthma (only as concomitant therapy with an inhaled corticosteroid) in patients with reversible obstructive airway disease, including patients with symptoms of nocturnal asthma (Foradil, Oxeze Turbuhaler).
COPD: Maintenance treatment of COPD (Foradil).
Exercise-induced bronchospasm: Prevention of exercise-induced bronchospasm when administered on an as-needed basis (monotherapy may be indicated in patients without persistent asthma) (Oxeze Turbuhaler).
Contraindications
Hypersensitivity to formoterol or any component of the formulation (Foradil Aerolizer only); treatment of status asthmaticus or other acute episodes of asthma or chronic obstructive pulmonary disease (Foradil Aerolizer only); monotherapy (without use of a concomitant inhaled corticosteroid) in the treatment of asthma.
Documentation of allergenic cross-reactivity for sympathomimetics is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Canadian labeling: Additional contraindications (not in US labeling): Presence of tachyarrhythmias
Dosage and Administration
Dosing: Adult
Note: Foradil Aerolizer is no longer available in the US.
Asthma: Oral inhalation: Note: For asthma control, long-acting beta-2 agonists (LABAs) should be used in combination with inhaled corticosteroids and not as monotherapy.
US labeling: Foradil Aerolizer: Dry powder inhaler: 12 mcg every 12 hours (maximum: 24 mcg daily)
Canadian labeling:
Foradil: Dry powder inhaler: 12 mcg every 12 hours; in severe cases, 24 mcg every 12 hours may be given (maximum: 48 mcg daily)
Oxeze Turbuhaler: Dry powder inhaler: 6 mcg or 12 mcg every 12 hours (maximum: 48 mcg daily)
Chronic obstructive pulmonary disease: Oral inhalation:
US labeling:
Foradil Aerolizer: Dry powder inhaler: 12 mcg every 12 hours (maximum dose: 24 mcg/day)
Perforomist: Nebulization solution: 20 mcg twice daily (maximum dose: 40 mcg/day)
Canadian labeling: Foradil: Dry powder inhaler: 12 mcg or 24 mcg twice daily (maximum dose: 48 mcg/day)
Exercise-induced bronchospasm: Oral inhalation: Note: If already using for asthma maintenance, then should not use additional doses for exercise-induced bronchospasm. Because LABAs may disguise poorly controlled persistent asthma, frequent or chronic use of LABAs for exercise-induced bronchospasm is discouraged by the Asthma Guidelines (NAEPP 2007).
US labeling: Foradil Aerolizer: Dry powder inhaler: 12 mcg at least 15 minutes before exercise on an occasional "as needed" basis; additional doses should not be used for another 12 hours
Canadian labeling: Oxeze Turbuhaler: Dry powder inhaler: 6 mcg or 12 mcg at least 15 minutes before exercise on an occasional "as needed" basis (maximum: 48 mcg/24-hour period)
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Foradil Aerolizer has been discontinued >1 year. Foradil Aerolizer and Perforomist are not interchangeable.
Asthma, maintenance treatment: Note: For asthma control, long-acting beta2-agonists (LABAs) should be used in combination with inhaled corticosteroids and not as monotherapy.
Foradil Aerolizer (12 mcg/inhalation): Children ≥5 years and Adolescents: Oral inhalation: 12 mcg every 12 hours; maximum daily dose: 24 mcg/day
Canadian labeling: Foradil 12 mcg/inhalation [Canadian product]: Oral inhalation:
Children ≥6 years and Adolescents ≤16 years: 12 mcg every 12 hours; maximum daily dose: 24 mcg/day
Adolescents ≥17 years: 12 mcg every 12 hours; in severe cases, 24 mcg every 12 hours may be necessary; maximum daily dose: 48 mcg/day
Canadian labeling: Oxeze Turbuhaler 6 mcg/inhalation and 12 mcg/inhalation [Canadian products]: Oral Inhalation:
Children ≥6 years and Adolescents ≤16 years: 6 mcg or 12 mcg every 12 hours; maximum daily dose: 24 mcg/day
Adolescents ≥17 years: 6 mcg or 12 mcg every 12 hours; in severe cases, 24 mcg every 12 hours may be necessary; maximum daily dose: 48 mcg/day
Exercise-induced bronchospasm, prevention: Note: If already using formoterol for asthma maintenance, then patients should not use additional doses for exercise-induced bronchospasm. Because long-acting beta2-agonists (LABAs) may disguise poorly-controlled persistent asthma, frequent or chronic use of LABAs for exercise-induced bronchospasm is discouraged by the NAEPP and GINA Asthma Guidelines (GINA 2017; NAEPP 2007).
Foradil Aerolizer (12 mcg/inhalation): Children ≥5 years and Adolescents: Oral Inhalation: 12 mcg 15 minutes prior to exercise on an occasional "as needed" basis; additional doses should not be used for 12 hours; maximum daily dose: 24 mcg/day
Canadian labeling: Oxeze Turbuhaler 6 mcg/inhalation and 12 mcg/inhalation [Canadian products]: Children ≥6 years and Adolescents: Oral Inhalation: 6 mcg or 12 mcg before exercise on an occasional "as needed" basis; maximum daily dose: 24 mcg/day
Administration
Dry powder inhaler:
Foradil Aerolizer: Remove capsule from foil blister immediately before use. Place capsule in the capsule-chamber in the base of the Aerolizer Inhaler. Capsules must not be swallowed whole; must only use the Aerolizer Inhaler. Press both buttons once only and then release. Keep inhaler in a level, horizontal position with the blue buttons to the left and right (not up and down). Exhale fully. Do not exhale into inhaler. Tilt head slightly back and inhale (rapidly, steadily, and deeply). Hold breath as long as possible. If any powder remains in capsule, exhale and inhale again. Repeat until capsule is empty. Throw away empty capsule; do not leave in inhaler. Do not use a spacer with the Aerolizer Inhaler. Always keep capsules and inhaler dry.
Oxeze Turbuhaler [Canadian product]: Hold inhaler upright. Turn colored grip as far as it will go in one direction and then turn back to original position; a clicking sound should be heard which means the inhaler is ready for use. Exhale fully. Do not exhale into mouthpiece of inhaler. Place mouthpiece to lips and inhale forcefully and deeply. Do not chew or bite on mouthpiece. Clean outside of mouthpiece once weekly with a dry tissue. Avoid getting inhaler wet. If the inhaler is accidently dropped or shaken, or if the patient exhales into the inhaler, the dose will be lost and a new dose should be loaded.
Nebulization solution: Perforomist: Remove unit-dose vial from foil pouch immediately before use. Solution does not require dilution prior to administration; do not mix other medications with formoterol solution. Place contents of unit-dose vial into the reservoir of a standard jet nebulizer connected to an air compressor; assemble nebulizer based on the manufacturer’s instructions and turn nebulizer on; breathe deeply and evenly until all of the medication has been inhaled. The average inhalation time is 9 minutes. Discard any unused medication immediately; do not ingest contents of vial. Clean nebulizer after use.
Storage
Foradil Aerolizer: Prior to dispensing, store in refrigerator at 2°C to 8°C (36°F to 46°F). After dispensing, store at room temperature at 20°C to 25°C (68°F to 77°F). Protect from heat and moisture. Capsules should always be stored in the blister and only removed immediately before use.
Perforomist: Prior to dispensing, store in refrigerator at 2°C to 8°C (36°F to 46°F). After dispensing, store in refrigerator at 2°C to 8°C (36°F to 46°F) or room temperature at 20°C to 25°C (68°F to 77°F) for up to 3 months. Protect from light and heat. Unit-dose vials should always be stored in the foil pouch and only removed immediately before use.
Oxeze Turbuhaler [Canadian product]: Store at 15°C to 30°C (59°F to 86°F). Protect from moisture.
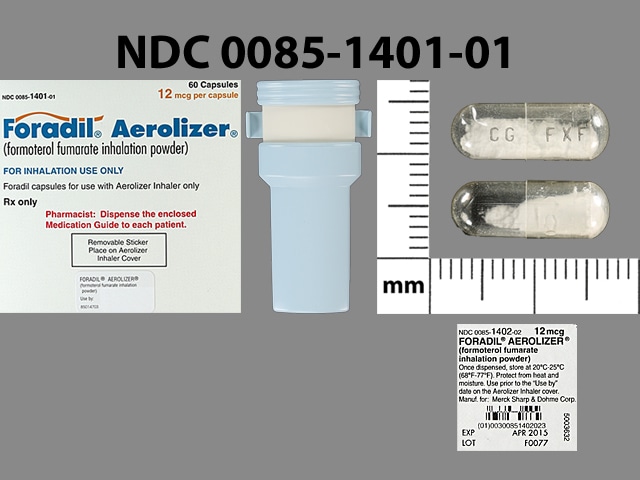
Formoterol Images
Drug Interactions
AtoMOXetine: May enhance the tachycardic effect of Beta2-Agonists. Monitor therapy
AtoMOXetine: May enhance the hypertensive effect of Sympathomimetics. AtoMOXetine may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
Atosiban: Beta2-Agonists may enhance the adverse/toxic effect of Atosiban. Specifically, there may be an increased risk for pulmonary edema and/or dyspnea. Monitor therapy
Beta2-Agonists (Long-Acting): May enhance the adverse/toxic effect of other Beta2-Agonists (Long-Acting). Avoid combination
Beta-Blockers (Beta1 Selective): May diminish the bronchodilatory effect of Beta2-Agonists. Of particular concern with nonselective beta-blockers or higher doses of the beta1 selective beta-blockers. Monitor therapy
Beta-Blockers (Nonselective): May diminish the bronchodilatory effect of Beta2-Agonists. Avoid combination
Betahistine: May diminish the therapeutic effect of Beta2-Agonists. Monitor therapy
Caffeine and Caffeine Containing Products: May enhance the adverse/toxic effect of Formoterol. Caffeine and Caffeine Containing Products may enhance the hypokalemic effect of Formoterol. Monitor therapy
Cannabinoid-Containing Products: May enhance the tachycardic effect of Sympathomimetics. Exceptions: Cannabidiol. Monitor therapy
Cocaine (Topical): May enhance the hypertensive effect of Sympathomimetics. Management: Consider alternatives to use of this combination when possible. Monitor closely for substantially increased blood pressure or heart rate and for any evidence of myocardial ischemia with concurrent use. Consider therapy modification
Doxofylline: Sympathomimetics may enhance the adverse/toxic effect of Doxofylline. Monitor therapy
Guanethidine: May enhance the arrhythmogenic effect of Sympathomimetics. Guanethidine may enhance the hypertensive effect of Sympathomimetics. Monitor therapy
Haloperidol: QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of Haloperidol. Monitor therapy
Inhalational Anesthetics: May enhance the arrhythmogenic effect of Formoterol. Monitor therapy
Linezolid: May enhance the hypertensive effect of Sympathomimetics. Management: Reduce initial doses of sympathomimetic agents, and closely monitor for enhanced pressor response, in patients receiving linezolid. Specific dose adjustment recommendations are not presently available. Consider therapy modification
Loop Diuretics: Beta2-Agonists may enhance the hypokalemic effect of Loop Diuretics. Monitor therapy
Loxapine: Agents to Treat Airway Disease may enhance the adverse/toxic effect of Loxapine. More specifically, the use of Agents to Treat Airway Disease is likely a marker of patients who are likely at a greater risk for experiencing significant bronchospasm from use of inhaled loxapine. Management: This is specific to the Adasuve brand of loxapine, which is an inhaled formulation. This does not apply to non-inhaled formulations of loxapine. Avoid combination
Methacholine: Beta2-Agonists (Long-Acting) may diminish the therapeutic effect of Methacholine. Management: Hold long-acting beta2 agonists for 36 hours before methacholine use. Consider therapy modification
Monoamine Oxidase Inhibitors: May enhance the adverse/toxic effect of Beta2-Agonists. Monitor therapy
QT-prolonging Agents (Highest Risk): QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Solriamfetol: Sympathomimetics may enhance the hypertensive effect of Solriamfetol. Monitor therapy
Sympathomimetics: May enhance the adverse/toxic effect of other Sympathomimetics. Monitor therapy
Tedizolid: May enhance the hypertensive effect of Sympathomimetics. Tedizolid may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
Theophylline Derivatives: May enhance the adverse/toxic effect of Formoterol. Theophylline Derivatives may enhance the hypokalemic effect of Formoterol. Monitor therapy
Thiazide and Thiazide-Like Diuretics: Beta2-Agonists may enhance the hypokalemic effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Tricyclic Antidepressants: May enhance the adverse/toxic effect of Beta2-Agonists. Monitor therapy
Adverse Reactions
1% to 10%:
Cardiovascular: Chest pain (2% to 3%)
Central nervous system: Anxiety (2%), dizziness (2%), insomnia (2%), voice disorder (1%), headache
Dermatologic: Pruritus (2%), skin rash (1%)
Gastrointestinal: Diarrhea (5%), nausea (5%), xerostomia (1% to 3%), vomiting (2%), abdominal pain, dyspepsia, gastroenteritis
Neuromuscular & skeletal: Muscle cramps (2%), tremor
Respiratory: Respiratory tract infection (3% to 7%), exacerbation of asthma (ages 5 to 12 years: 5% to 6%; age >12 years: <4%; acute deterioration: <1%), bronchitis (5%), pharyngitis (3% to 4%), sinusitis (3%), dyspnea (2%), tonsillitis (1%)
Miscellaneous: Fever (2%)
<1%, postmarketing, and/or case reports: Agitation, anaphylaxis (including severe hypotension/angioedema), angina pectoris, atrial fibrillation, behavioral changes, cardiac arrhythmia, cough, decreased glucose tolerance, dermatitis, disturbed sleep, dysgeusia, fatigue, hyperglycemia, hypertension, hypokalemia, malaise, metabolic acidosis, muscle spasm, nervousness, palpitations, paradoxical bronchospasm, prolonged Q-T interval on ECG, restlessness, tachycardia, urticaria, variable blood pressure, ventricular premature contractions
Warnings/Precautions
Concerns related to adverse effects:
- Asthma-related deaths: Monotherapy with a long-acting beta-2 agonist (LABA) is contraindicated in the treatment of asthma. In a large, randomized, placebo-controlled US clinical trial (SMART 2006), salmeterol was associated with an increase in asthma-related deaths (when added to usual asthma therapy); risk is considered a class effect among all LABAs. When LABAs are used in a fixed-dose combination with inhaled corticosteroids, data from large clinical trials do not show a significant increase in the risk of serious asthma-related events (hospitalizations, intubations, death) compared to inhaled corticosteroids alone. Current guidelines recommend the use of an inhaled corticosteroid before adding a LABA (GINA 2018; NIH/NHLBI 2007). It is unknown if formoterol increases asthma-related deaths. In a more recent multicenter, randomized, double-blinded trial, the use of salmeterol and an inhaled corticosteroid (ie, fluticasone) combined in a single inhaler in a large number of children, adolescent, and adult patients with persistent asthma (non-life threatening and stable) did not increase the risk of serious asthma-related events compared with fluticasone alone; in addition, patients receiving fluticasone/salmeterol had fewer severe asthma exacerbations compared with patients receiving fluticasone alone (Peters 2016; Stempel 2016a; Stempel 2016b). Available data do not suggest an increased risk of death with use of LABAs in patients with chronic obstructive pulmonary disease (COPD).
- Bronchospasm: Paradoxical bronchospasm that may be life-threatening and may occur with use of inhaled bronchodilating agents; this reaction should be distinguished from inadequate response. Discontinue immediately if paradoxical bronchospasm occurs and institute alternative therapy.
- Hypersensitivity reactions: Immediate hypersensitivity reactions (urticaria, angioedema, rash, bronchospasm) have been reported.
- Serious effects/fatalities: Do not exceed recommended dose or frequency or use with other medications containing LABAs; serious adverse events, including fatalities, have been associated with excessive use of inhaled sympathomimetics.
Disease-related concerns:
- Asthma: Appropriate use:
- Foradil Aerolizer: Not indicated for the initial (rescue) treatment of acute episodes of bronchospasm. Short-acting beta-2 agonist (eg, albuterol) should be used for acute symptoms and symptoms occurring between treatments. Do not initiate in patients with significantly worsening or acutely deteriorating asthma; reports of severe (sometimes fatal) respiratory events have been reported when formoterol has been initiated in this situation.
- Perforomist: Not FDA approved for the treatment of asthma; safety and efficacy in asthma patients have not been established.
- Cardiovascular disease: Use with caution in patients with cardiovascular disease (arrhythmia, coronary insufficiency, or hypertension); beta-agonists may cause elevation in blood pressure and heart rate and result in CNS stimulation/excitation. Beta-2 agonists have been reported to produce ECG changes, such as flattening of the T wave, prolongation of the QTc interval, and ST segment depression.
- Chronic obstructive pulmonary disease: Appropriate use: Do not use for acute episodes of COPD. Do not initiate in patients with significantly worsening or acutely deteriorating COPD. Available data do not suggest an increased risk of death with use of LABAs in patients with COPD.
- Diabetes: Use with caution in patients with diabetes mellitus; beta-2 agonists may increase serum glucose and aggravate preexisting diabetes mellitus and ketoacidosis.
- Exercise-induced bronchospasm: Because LABAs may disguise poorly controlled persistent asthma, frequent or chronic use of LABAs for exercise-induced bronchospasm is discouraged by the NIH Asthma Guidelines (NIH, 2007).
- Hyperthyroidism: Use with caution in hyperthyroidism; may stimulate thyroid activity.
- Hypokalemia: Use with caution in patients with hypokalemia; beta-2 agonists may decrease serum potassium (transient).
- Seizures: Use with caution in patients with seizure disorders; beta-agonists may result in CNS stimulation/excitation.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Pediatric: Foradil Aerolizer: LABAs, when used as monotherapy, may increase the risk of asthma-related hospitalization in pediatric and adolescent patients. When LABAs are used in a fixed-dose combination with inhaled corticosteroids, data from large clinical trials in adolescents do not show a significant increase in the risk of serious asthma-related events (hospitalizations, intubations, death) compared to inhaled corticosteroids alone.
Dosage form specific issues:
- Foradil Aerolizer: The contents of the capsules are for inhalation only via the Aerolizer device. There have been reports of incorrect administration (swallowing of the capsules).
- Lactose: Powder for oral inhalation may contain lactose; very rare anaphylactic reactions have been reported in patients with severe milk protein allergy.
Other warnings/precautions:
- Patient information: Patients using inhaled, short-acting beta-2 agonists should be instructed to discontinue routine use of these medications prior to beginning treatment; short-acting agents should still be provided to patients; however, use should be reserved for symptomatic relief of acute symptoms. Patients must be instructed to seek medical attention in cases where acute symptoms are not relieved or a previous level of response is diminished. The need to increase frequency of use of short-acting beta-2 agonists may indicate deterioration of asthma or COPD, and medical evaluation must not be delayed.
- Tolerance/Tachyphylaxis: Tolerance to the bronchodilator effect, measured by FEV1, has been observed in studies.
Monitoring Parameters
FEV1, peak flow, and/or other pulmonary function tests; shortness of breath; blood pressure, heart rate; CNS stimulation; serum glucose, serum potassium
Pregnancy
Pregnancy Considerations
Adverse events were observed in some animal reproduction studies. Beta-agonists may interfere with uterine contractility if administered during labor.
Patient Education
What is this drug used for?
All inhaler products:
- It is used to treat asthma.
- It is used to prevent breathing problems that happen with exercise.
Liquid for breathing in:
- It is used to treat COPD (chronic obstructive pulmonary disease).
- This drug is not approved to treat asthma. Talk with your doctor.
All products:
- This drug is not to be used to treat intense flare-ups of shortness of breath. Use a rescue inhaler. Talk with the doctor.
Frequently reported side effects of this drug
- Nausea
- Vomiting
- Anxiety
- Tremors
- Dry mouth
- Trouble sleeping
- Loss of strength and energy
- Diarrhea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- High blood sugar like confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit.
- Low potassium like muscle pain or weakness, muscle cramps, or an abnormal heartbeat.
- Acidosis like confusion, fast breathing, fast heartbeat, abnormal heartbeat, severe abdominal pain, nausea, vomiting, fatigue, shortness of breath, or loss of strength and energy.
- Chest pain
- Fast heartbeat
- Abnormal heartbeat
- Severe dizziness
- Passing out
- Vision changes
- Severe headache
- Trouble breathing, wheezing, or coughing after use
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.