Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
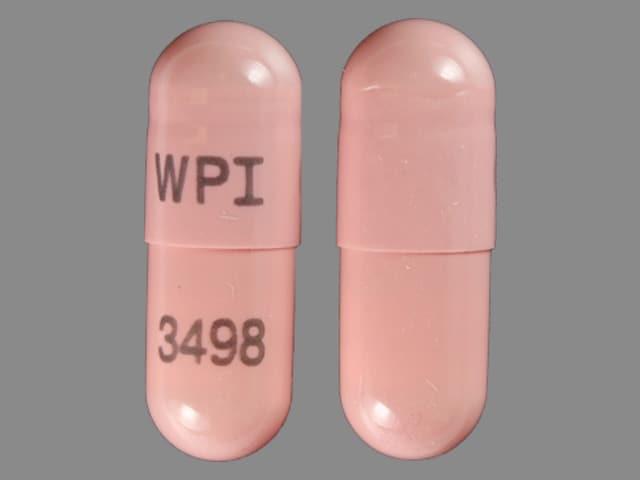
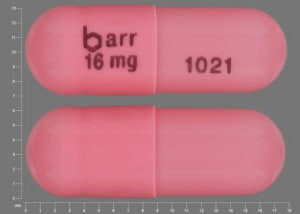
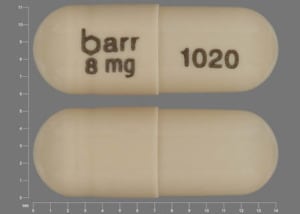
Capsule Extended Release 24 Hour, Oral, as hydrobromide [strength expressed as base]:
Razadyne ER: 8 mg, 16 mg, 24 mg
Generic: 8 mg, 16 mg, 24 mg
Solution, Oral, as hydrobromide:
Generic: 4 mg/mL (100 mL)
Tablet, Oral, as hydrobromide [strength expressed as base]:
Razadyne: 4 mg, 8 mg
Razadyne: 12 mg [contains fd&c yellow #6 aluminum lake]
Generic: 4 mg, 8 mg, 12 mg
Pharmacology
Mechanism of Action
Centrally-acting cholinesterase inhibitor (competitive and reversible). It elevates acetylcholine in cerebral cortex by slowing the degradation of acetylcholine. Modulates nicotinic acetylcholine receptor to increase acetylcholine from surviving presynaptic nerve terminals. May increase glutamate and serotonin levels.
Pharmacokinetics/Pharmacodynamics
Distribution
175 L
Metabolism
Hepatic metabolism primarily via CYP2D6 to O-desmethyl-galantamine and 3A4 to galantamine-N-oxide; the activity of galantamine metabolites is not considered to be clinically relevant (Farlow 2003; Scott 2000)
Excretion
Urine (20%)
Time to Peak
Immediate release: 1 hour (2.5 hours with food); extended release: 4.5-5 hours
Half-Life Elimination
~7 hours
Protein Binding
18%
Use in Specific Populations
Special Populations: Renal Function Impairment
AUC increased 37% and 67% in moderate and severe renal function impairment.
Special Populations: Hepatic Function Impairment
Cl decreased about 25% in moderate (Child-Pugh score 7 to 9) hepatic function impairment.
Special Populations: Elderly
Concentrations are about 30% to 40% higher.
Special Populations: Gender
Cl is about 20% lower in women than in men.
Special Populations Note
CYP2D6 poor metabolizers: There is an approximate 35% increase in AUC of unchanged drug and 25% decrease in median Cl.
Use: Labeled Indications
Alzheimer dementia, mild to moderate: Treatment of mild to moderate dementia of Alzheimer disease
Use: Off Label
Alzheimer dementia, severebyes
Based on the American Psychiatric Association guidelines for the treatment of Alzheimer's disease and other dementias, cholinesterase inhibitors, including galantamine, may be considered in patients with severe dementia of Alzheimer disease.
Data from a randomized, placebo-controlled, double-blind trial support the use of galantamine in the treatment of patients with severe dementia of Alzheimer disease. Additional trials may be necessary to further define the role of galantamine in this condition Burns 2009.
Dementia associated with Parkinson diseasecyes
Based on the American Psychiatric Association guidelines for the treatment of Alzheimer's Disease and Other Dementias, cholinesterase inhibitors may be given for patients with mild to moderate dementia associated with Parkinson disease. Only rivastigmine has been approved by the FDA for this indication, however, other cholinesterase inhibitors, including galantamine, may be considered for use in the management of this condition.
Data from a limited number of patients studied in an open-label trial and an open-label, controlled clinical trial suggest that galantamine may be beneficial for the treatment of dementia associated with Parkinson disease. Additional data may be necessary to further define the role of drug galantamine in this condition Aarsland 2003, Litvinenko 2008.
Lewy body dementiacyes
Based on the American Psychiatric Association guidelines for the treatment of Alzheimer's Disease and Other Dementias, cholinesterase inhibitors, including galantamine may be considered for patients with Lewy body dementia.
Data from a limited number of patients in an open-label trial suggest that galantamine may be beneficial for the treatment Lewy body dementia. Additional data may be necessary to further define the role of galantamine in this condition Edwards 2007.
Vascular dementiacyes
Data from a meta-analysis suggest that galantamine may be beneficial for the treatment of cognitive symptoms of vascular dementia; however, clinical effects were modest Chen 2016.
Based on the British Association for Psychopharmacology consensus statement on clinical practice with antidementia drugs, cholinesterase inhibitors, including galantamine, are not recommended for patients with vascular dementia; however, those with mixed vascular dementia and Alzheimer disease may benefit BAP [O'Brien 2017].
Contraindications
Hypersensitivity to galantamine or any component of the formulation
Canadian labeling: Additional contraindications (not in U.S. labeling): Hypersensitivity to other tertiary alkaloids
Dosage and Administration
Dosing: Adult
Alzheimer dementia, mild to moderate: Oral:
Immediate-release tablet or solution: Initial: 4 mg twice daily for 4 weeks; if tolerated, increase to 8 mg twice daily for ≥4 weeks; if tolerated, increase to 12 mg twice daily. Range: 16 to 24 mg daily in 2 divided doses.
Extended-release capsule: Initial: 8 mg once daily for 4 weeks; if tolerated, increase to 16 mg once daily for ≥4 weeks; if tolerated, increase to 24 mg once daily. Range: 16 to 24 mg once daily.
Note: If therapy is interrupted for ≥3 days, restart at the lowest dose and increase to current dose.
Alzheimer dementia, severe (off-label use): Immediate-release tablet: Initial: 4 mg twice daily for 4 weeks; if tolerated, increase to 8 mg twice daily for ≥4 weeks; if tolerated, increase to 12 mg twice daily. May decrease to 8 mg twice daily if the target dose is not tolerated. Range: 16 to 24 mg daily in 2 divided doses (Burns 2009).
Dementia associated with Parkinson disease and Lewy body dementia (off-label use): Oral: American Psychiatric Association recommends dosing and titration similar to those for patients with Alzheimer disease (APA [Rabins 2007]).
Vascular dementia (off-label use): Initial: 4 mg twice daily for 4 weeks; increase to 8 mg twice daily for 4 weeks; if tolerated, increase to 12 mg twice daily. Range: 16 to 24 mg/day in 2 divided doses (Auchus 2007).
Conversion from immediate release to extended release formulation: Patients may be switched from the immediate-release formulation to the extended-release formulation by taking the last immediate-release dose in the evening and beginning the extended-release dose the following morning; the same total daily dose should be used.
Conversion to galantamine from other cholinesterase inhibitors: Patients experiencing poor tolerability with donepezil or rivastigmine should wait until side effects subside or allow a 7-day washout period prior to beginning galantamine. Patients not experiencing side effects with donepezil or rivastigmine may begin galantamine therapy the day immediately following discontinuation of previous therapy (Morris 2001).
Dosing: Geriatric
Refer to adult dosing; adjust dose with caution in patients with low body weight and/or serious comorbidities.
Administration
Oral: Administer solution or tablet with breakfast and dinner; administer extended release capsule with breakfast. If therapy is interrupted for ≥3 days, restart at the lowest dose and increase to current dose. If using oral solution, mix dose with 3 to 4 ounces of any nonalcoholic beverage; mix well and drink immediately.
Dietary Considerations
Administration with food is preferred, but not required; should be taken with breakfast and dinner (tablet or solution) or with breakfast (capsule).
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Do not freeze oral solution.
Galantamine Images
Drug Interactions
Amifampridine: Acetylcholinesterase Inhibitors may enhance the therapeutic effect of Amifampridine. Amifampridine side effects may also be increased. Amifampridine may enhance the therapeutic effect of Acetylcholinesterase Inhibitors. Acetylcholinesterase inhibitor side effects may also be increased. Monitor therapy
Anticholinergic Agents: Acetylcholinesterase Inhibitors may diminish the therapeutic effect of Anticholinergic Agents. Anticholinergic Agents may diminish the therapeutic effect of Acetylcholinesterase Inhibitors. Monitor therapy
Antipsychotic Agents: Acetylcholinesterase Inhibitors (Central) may enhance the neurotoxic (central) effect of Antipsychotic Agents. Severe extrapyramidal symptoms have occurred in some patients. Monitor therapy
Benoxinate: Acetylcholinesterase Inhibitors may enhance the therapeutic effect of Benoxinate. Specifically, the effects of benoxinate may be prolonged. Monitor therapy
Beta-Blockers: Acetylcholinesterase Inhibitors may enhance the bradycardic effect of Beta-Blockers. Exceptions: Levobunolol; Metipranolol. Monitor therapy
Bradycardia-Causing Agents: May enhance the bradycardic effect of other Bradycardia-Causing Agents. Monitor therapy
Ceritinib: Bradycardia-Causing Agents may enhance the bradycardic effect of Ceritinib. Management: If this combination cannot be avoided, monitor patients for evidence of symptomatic bradycardia, and closely monitor blood pressure and heart rate during therapy. Exceptions are discussed in separate monographs. Consider therapy modification
Cholinergic Agonists: Acetylcholinesterase Inhibitors may enhance the adverse/toxic effect of Cholinergic Agonists. Monitor therapy
Corticosteroids (Systemic): May enhance the adverse/toxic effect of Acetylcholinesterase Inhibitors. Increased muscular weakness may occur. Monitor therapy
CYP2D6 Inhibitors (Strong): May increase the serum concentration of Galantamine. Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Galantamine. Monitor therapy
Dipyridamole: May diminish the therapeutic effect of Acetylcholinesterase Inhibitors. Monitor therapy
Fexinidazole [INT]: Bradycardia-Causing Agents may enhance the arrhythmogenic effect of Fexinidazole [INT]. Avoid combination
Ivabradine: Bradycardia-Causing Agents may enhance the bradycardic effect of Ivabradine. Monitor therapy
Lacosamide: Bradycardia-Causing Agents may enhance the AV-blocking effect of Lacosamide. Monitor therapy
Midodrine: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Neuromuscular-Blocking Agents (Nondepolarizing): Acetylcholinesterase Inhibitors may diminish the neuromuscular-blocking effect of Neuromuscular-Blocking Agents (Nondepolarizing). Monitor therapy
Ruxolitinib: May enhance the bradycardic effect of Bradycardia-Causing Agents. Management: Ruxolitinib Canadian product labeling recommends avoiding use with bradycardia-causing agents to the extent possible. Monitor therapy
Siponimod: Bradycardia-Causing Agents may enhance the bradycardic effect of Siponimod. Management: Avoid coadministration of siponimod with drugs that may cause bradycardia. Consider therapy modification
Succinylcholine: Acetylcholinesterase Inhibitors may increase the serum concentration of Succinylcholine. Management: Consider alternatives to this combination due to a risk of prolonged neuromuscular blockade. Consider therapy modification
Terlipressin: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Tofacitinib: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Adverse Reactions
>10%: Gastrointestinal: Nausea (21%), vomiting (11%)
1% to 10%:
Cardiovascular: Bradycardia (1%), syncope (1%)
Central nervous system: Dizziness (8%), headache (7%), depression (4%), falling (4%), fatigue (4%), drowsiness (2%), lethargy (1%), malaise (1%)
Endocrine & metabolic: Weight loss (5%)
Gastrointestinal: Decreased appetite (7%), diarrhea (7%), abdominal pain (4%), abdominal distress (2%), dyspepsia (2%)
Neuromuscular & skeletal: Tremor (2%), muscle spasm (1%)
Miscellaneous: Laceration (1%)
Frequency not defined:
Gastrointestinal: Anorexia
<1%, postmarketing, and/or case reports: Acute generalized exanthematous pustulosis, atrioventricular block, blurred vision, cerebrovascular accident, complete atrioventricular block, dehydration (includes rare, severe cases leading to renal insufficiency and renal failure), dysgeusia, erythema multiforme, first degree atrioventricular block, flushing, hallucination, hepatitis, hyperhidrosis, hypersensitivity reaction, hypersomnia, hypertension, hypotension, increased liver enzymes, myasthenia, myocardial infarction, palpitations, paresthesia, retching, seizure, sinus bradycardia, skin rash, Stevens-Johnson syndrome, supraventricular extrasystole, tinnitus
Warnings/Precautions
Concerns related to adverse effects:
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery or driving).
- Skin reactions: Skin reactions including Stevens-Johnson syndrome, acute generalized exanthematous pustulosis and erythema multiforme have been reported. Treatment discontinuation may be necessary if skin reaction occurs; if rash is suspected to be drug related, do not resume galantamine and consider alternative therapy.
- Vagotonic effects: Cholinesterase inhibitors may have vagotonic effects which may cause bradycardia and/or heart block with or without a history of cardiac disease.
- Weight loss: Weight loss has been observed; monitor body weight.
Disease-related concerns:
- Cardiac conduction abnormalities: Use with caution in patients with sick-sinus syndrome, bradycardia, or conduction abnormalities. Alzheimer's treatment guidelines consider bradycardia to be a relative contraindication for use of centrally-active cholinesterase inhibitors.
- Hepatic impairment: Use with caution in patients with mild to moderate liver impairment; not recommended in severe impairment. Dose adjustment recommended in moderate impairment.
- Peptic ulcer disease: Use with caution in patients at risk of ulcer disease (eg, previous history or NSAID use); may increase gastric acid secretion. Monitor for symptoms of bleeding.
- Renal impairment: Use with caution in patients with moderate renal impairment; not recommended in severe impairment (CrCl <9 mL/minute).
- Respiratory disease: Use with caution in patients with COPD and/or asthma.
- Seizure disorder: Use with caution in patients with a history of seizure disorder.
- Urinary tract obstruction: Use with caution in patients with bladder outlet obstruction or prostatic hyperplasia; cholinomimetics may cause or worsen outflow obstructions, including possible exacerbation of BPH symptoms.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Limited safety data in patients ≥85 years of age. Use with caution particularly in elderly patients with low body weight and/or serious comorbidities; adjust dose with caution.
Monitoring Parameters
Mental status; body weight, symptoms of GI intolerance, symptoms of active or occult GI bleeding
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Adverse events have been observed in animal reproduction studies.
Patient Education
What is this drug used for?
- It is used to treat dementia in people with Alzheimer disease.
Frequently reported side effects of this drug
- Dizziness
- Headache
- Lack of appetite
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Slow heartbeat
- Abnormal heartbeat
- Black, tarry, or bloody stools
- Vomiting blood
- Unable to pass urine
- Seizures
- Severe nausea
- Vomiting
- Severe diarrhea
- Excessive weight loss
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.