Boxed Warning
Lactic acidosis:
Postmarketing cases of metformin-associated lactic acidosis have resulted in death, hypothermia, hypotension, and resistant bradyarrhythmias. The onset of metformin-associated lactic acidosis is often subtle, accompanied only by nonspecific symptoms, such as malaise, myalgias, respiratory distress, somnolence, and abdominal pain. Metformin-associated lactic acidosis is characterized by elevated blood lactate levels (>5 mmol/L), anion gap acidosis (without evidence of ketonuria or ketonemia), an increased lactate/pyruvate ratio, and metformin plasma levels generally >5 mcg/mL.
Risk factors for metformin-associated lactic acidosis include renal impairment, concomitant use of certain drugs (eg, cationic drugs such as topiramate), age ≥65 years, having a radiological study with contrast, surgery and other procedures, hypoxic states (eg, congestive heart failure), excessive alcohol intake, and hepatic impairment.
Steps to reduce the risk of and manage metformin-associated lactic acidosis in these high risk groups are provided.
If metformin-associated lactic acidosis is suspected, immediately discontinue glipizide and metformin hydrochloride and institute general supportive measures in a hospital setting. Prompt hemodialysis is recommended.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, oral: 2.5/250: Glipizide 2.5 mg and metformin hydrochloride 250 mg; 2.5/500: Glipizide 2.5 mg and metformin hydrochloride 500 mg; 5/500: Glipizide 5 mg and metformin hydrochloride 500 mg
Pharmacology
Mechanism of Action
The combination of glipizide and metformin is used to improve glycemic control in patients with type 2 diabetes mellitus (noninsulin dependent, NIDDM) by using two different, but complementary, mechanisms of action:
Glipizide: Stimulates insulin release from the pancreatic beta cells; reduces glucose output from the liver; insulin sensitivity is increased at peripheral target sites
Metformin: Decreases hepatic glucose production, decreasing intestinal absorption of glucose and improves insulin sensitivity (increases peripheral glucose uptake and utilization)
Use: Labeled Indications
Diabetes mellitus, type 2: Adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus
Contraindications
Hypersensitivity to glipizide, metformin, or any component of the formulation; severe renal impairment (eGFR <30 mL/minute/1.73 m2); acute or chronic metabolic acidosis, including diabetic ketoacidosis, with or without coma
Dosage and Administration
Dosing: Adult
Diabetes mellitus, type 2: Oral:
Patients inadequately controlled on diet and exercise alone: Initial: Glipizide 2.5 mg/metformin 250 mg once daily. In patients with fasting plasma glucose (FPG) 280 to 320 mg/dL, initiate therapy with glipizide 2.5 mg/metformin 500 mg twice daily. Dose titration: Increase dose every 2 weeks per glycemic response. Maximum dose evaluated in clinical trials: Glipizide 10 mg/metformin 2,000 mg/day in divided doses.
Patients inadequately controlled on a sulfonylurea and/or metformin: Initial: Glipizide 2.5 mg/metformin 500 mg or glipizide 5 mg/metformin 500 mg twice daily; starting dose should not exceed current daily dose of glipizide (or sulfonylurea equivalent) and/or metformin. Dose titration: Increase dose in increments of no more than glipizide 5 mg/metformin 500 mg/day. Maximum: Glipizide 20 mg/metformin 2,000 mg/day in divided doses.
Dosing: Geriatric
Refer to adult dosing. Conservative doses are recommended in the elderly due to potentially decreased renal function; generally avoid titration to maximum dose.
Administration
Oral: Administer with a meal in the morning and in the evening (if twice-daily dosing). Patients without oral intake (NPO) or who require decreased caloric intake may need doses held to avoid hypoglycemia.
Dietary Considerations
May cause GI upset; should be taken with food to decrease GI upset. Individualized medical nutrition therapy (MNT) based on ADA recommendations is an integral part of therapy. Monitor for signs and symptoms of vitamin B12 and folic acid deficiency; supplementation may be required.
Storage
Store at 20°C to 25°C (68°F to 77°F); protect from light.
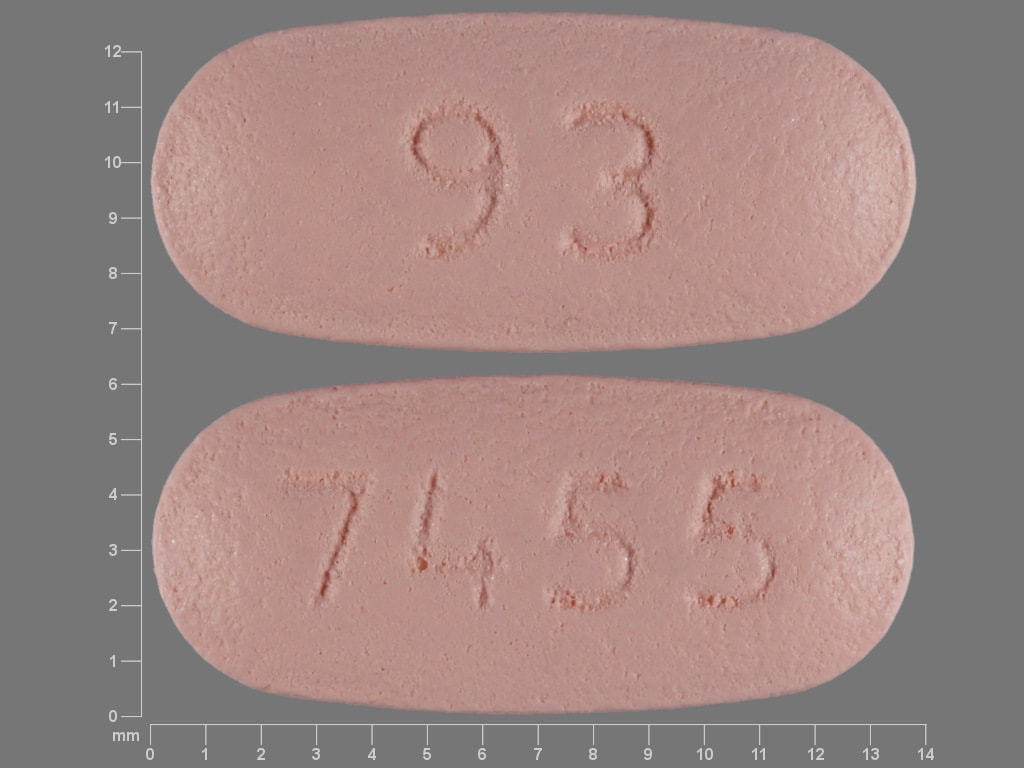
Glipizide and Metformin Images
Drug Interactions
Abemaciclib: May increase the serum concentration of MetFORMIN. Monitor therapy
Ajmaline: Sulfonamides may enhance the adverse/toxic effect of Ajmaline. Specifically, the risk for cholestasis may be increased. Monitor therapy
Alcohol (Ethyl): May enhance the adverse/toxic effect of MetFORMIN. Specifically, alcohol may potentiate the risk of lactic acidosis Avoid combination
Alpelisib: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Monitor therapy
Alpha-Lipoic Acid: May enhance the hypoglycemic effect of Antidiabetic Agents. Monitor therapy
Aminolevulinic Acid (Systemic): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Systemic). Avoid combination
Aminolevulinic Acid (Topical): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Topical). Monitor therapy
Androgens: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Exceptions: Danazol. Monitor therapy
Antidiabetic Agents: May enhance the hypoglycemic effect of Hypoglycemia-Associated Agents. Monitor therapy
Beta-Blockers: May enhance the hypoglycemic effect of Sulfonylureas. Cardioselective beta-blockers (eg, acebutolol, atenolol, metoprolol, and penbutolol) may be safer than nonselective beta-blockers. All beta-blockers appear to mask tachycardia as an initial symptom of hypoglycemia. Ophthalmic beta-blockers are probably associated with lower risk than systemic agents. Exceptions: Levobunolol; Metipranolol. Monitor therapy
Bictegravir: May increase the serum concentration of MetFORMIN. Monitor therapy
Carbocisteine: Sulfonylureas may enhance the adverse/toxic effect of Carbocisteine. Specifically, sulfonylureas may enhance adverse effects of alcohol that is present in liquid formulations of carbocisteine-containing products. Monitor therapy
Carbonic Anhydrase Inhibitors: May enhance the adverse/toxic effect of MetFORMIN. Specifically, the risk of developing lactic acidosis may be increased. Exceptions: Brinzolamide; Dorzolamide. Monitor therapy
Cephalexin: May increase the serum concentration of MetFORMIN. Monitor therapy
Chloramphenicol (Systemic): May decrease the metabolism of Sulfonylureas. Monitor therapy
Cimetidine: May increase the serum concentration of MetFORMIN. Management: Consider alternatives to cimetidine in patients receiving metformin due to a potential for increased metformin concentrations and toxicity (including lactic acidosis). Consider therapy modification
Clarithromycin: May increase the serum concentration of GlipiZIDE. Monitor therapy
Colesevelam: May decrease the serum concentration of GlipiZIDE. Management: Administer glipizide at least 4 hours prior to colesevelam. Consider therapy modification
Cyclic Antidepressants: May enhance the hypoglycemic effect of Sulfonylureas. Monitor therapy
CYP2C9 Inhibitors (Moderate): May decrease the metabolism of CYP2C9 Substrates (High risk with Inhibitors). Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP2C9 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dalfampridine: MetFORMIN may increase the serum concentration of Dalfampridine. Dalfampridine may increase the serum concentration of MetFORMIN. Monitor therapy
Dexketoprofen: May enhance the adverse/toxic effect of Sulfonamides. Monitor therapy
Dipeptidyl Peptidase-IV Inhibitors: May enhance the hypoglycemic effect of Sulfonylureas. Management: Consider a decrease in sulfonylurea dose when initiating therapy with a dipeptidyl peptidase-IV inhibitor and monitor patients for hypoglycemia. Consider therapy modification
Direct Acting Antiviral Agents (HCV): May enhance the hypoglycemic effect of Antidiabetic Agents. Monitor therapy
Dofetilide: MetFORMIN may increase the serum concentration of Dofetilide. Monitor therapy
Dolutegravir: May increase the serum concentration of MetFORMIN. Management: Consider the risks and benefits of this combination. If combined, limit the daily metformin dose to 1,000 mg when used with dolutegravir. Monitor for increased metformin effects/toxicities (including lactic acidosis) during concomitant use. Consider therapy modification
Elexacaftor, Tezacaftor, and Ivacaftor: May increase the serum concentration of GlipiZIDE. Monitor therapy
Enzalutamide: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP2C9 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP2C9 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May increase the serum concentration of OCT2 Substrates. Monitor therapy
Fibric Acid Derivatives: May enhance the hypoglycemic effect of Sulfonylureas. Monitor therapy
Fluconazole: May increase the serum concentration of Sulfonylureas. Management: Seek alternatives when possible. If used together, monitor closely for increased effects of sulfonylureas if fluconazole is initiated/dose increased, or decreased effects if fluconazole is discontinued/dose decreased. Consider therapy modification
Glucagon-Like Peptide-1 Agonists: May enhance the hypoglycemic effect of Sulfonylureas. Management: Consider sulfonylurea dose reductions when used in combination with glucagon-like peptide-1 agonists. Consider therapy modification
Glycopyrrolate (Systemic): May increase the serum concentration of MetFORMIN. Monitor therapy
Guanethidine: May enhance the hypoglycemic effect of Antidiabetic Agents. Monitor therapy
Herbs (Hypoglycemic Properties): May enhance the hypoglycemic effect of Hypoglycemia-Associated Agents. Monitor therapy
Hyperglycemia-Associated Agents: May diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Hypoglycemia-Associated Agents: May enhance the hypoglycemic effect of other Hypoglycemia-Associated Agents. Monitor therapy
Hypoglycemia-Associated Agents: Antidiabetic Agents may enhance the hypoglycemic effect of Hypoglycemia-Associated Agents. Monitor therapy
Indobufen: May increase the serum concentration of GlipiZIDE. Monitor therapy
Iodinated Contrast Agents: May enhance the adverse/toxic effect of MetFORMIN. Renal dysfunction that may be caused by iodinated contrast agents may lead to metformin-associated lactic acidosis. Management: Management advice varies. Refer to the full drug interaction monograph content for details. Exceptions: Diatrizoate Meglumine; Diatrizoate Sodium; Ethiodized Oil. Consider therapy modification
Isavuconazonium Sulfate: May increase the serum concentration of MetFORMIN. Monitor therapy
LamoTRIgine: May increase the serum concentration of MetFORMIN. Management: The lamotrigine Canadian product monograph states that coadministration of these drugs is not recommended. Monitor therapy
Lumacaftor and Ivacaftor: May decrease the serum concentration of CYP2C9 Substrates (High Risk with Inhibitors or Inducers). Lumacaftor and Ivacaftor may increase the serum concentration of CYP2C9 Substrates (High Risk with Inhibitors or Inducers). Monitor therapy
Maitake: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Mecamylamine: Sulfonamides may enhance the adverse/toxic effect of Mecamylamine. Avoid combination
Metreleptin: May enhance the hypoglycemic effect of Sulfonylureas. Management: Sulfonylurea dosage adjustments (including potentially large decreases) may be required to minimize the risk for hypoglycemia with concurrent use of metreleptin. Monitor closely. Consider therapy modification
Miconazole (Oral): May enhance the hypoglycemic effect of Sulfonylureas. Miconazole (Oral) may increase the serum concentration of Sulfonylureas. Monitor therapy
MiFEPRIStone: May increase the serum concentration of CYP2C9 Substrates (High risk with Inhibitors). Management: Use CYP2C9 substrates at the lowest recommended dose, and monitor closely for adverse effects, during and in the 2 weeks following mifepristone treatment. Consider therapy modification
Mitiglinide: May enhance the adverse/toxic effect of Sulfonylureas. Avoid combination
Monoamine Oxidase Inhibitors: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents: May enhance the adverse/toxic effect of MetFORMIN. Monitor therapy
Ombitasvir, Paritaprevir, and Ritonavir: May enhance the adverse/toxic effect of MetFORMIN. Specifically, the risk for lactic acidosis may be increased. Monitor therapy
Ombitasvir, Paritaprevir, Ritonavir, and Dasabuvir: May enhance the adverse/toxic effect of MetFORMIN. Specifically, the risk for lactic acidosis may be increased. Monitor therapy
Ondansetron: May increase the serum concentration of MetFORMIN. Monitor therapy
Patiromer: May decrease the serum concentration of MetFORMIN. Management: Administer metformin at least 3 hours before or 3 hours after patiromer. Consider therapy modification
Pegvisomant: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Porfimer: Photosensitizing Agents may enhance the photosensitizing effect of Porfimer. Monitor therapy
Posaconazole: May enhance the hypoglycemic effect of GlipiZIDE. Posaconazole may increase the serum concentration of GlipiZIDE. Monitor therapy
Probenecid: May decrease the protein binding of Sulfonylureas. Probenecid may increase the serum concentration of Sulfonylureas. Monitor therapy
Prothionamide: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Quinolones: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Quinolones may diminish the therapeutic effect of Blood Glucose Lowering Agents. Specifically, if an agent is being used to treat diabetes, loss of blood sugar control may occur with quinolone use. Monitor therapy
RaNITIdine: May increase the serum concentration of Sulfonylureas. Monitor therapy
Ranolazine: May increase the serum concentration of MetFORMIN. Management: Limit the metformin dose to a maximum of 1,700 mg per day when used together with ranolazine 1,000 mg twice daily. Monitor patients for metformin toxicities, including lactic acidosis and carefully weigh the risks and benefits of this combination. Consider therapy modification
RifAMPin: May decrease the serum concentration of Sulfonylureas. Management: Seek alternatives to these combinations when possible. Monitor closely for diminished therapeutic effects of sulfonylureas if rifampin is initiated/dose increased, or enhanced effects if rifampin is discontinued/dose decreased. Consider therapy modification
Rifapentine: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Monitor therapy
Ritodrine: May diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Salicylates: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Selective Serotonin Reuptake Inhibitors: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Sodium-Glucose Cotransporter 2 (SGLT2) Inhibitors: May enhance the hypoglycemic effect of Sulfonylureas. Management: Consider a decrease in sulfonylurea dose when initiating therapy with a sodium-glucose cotransporter 2 inhibitor and monitor patients for hypoglycemia. Consider therapy modification
Sulfonamide Antibiotics: May enhance the hypoglycemic effect of Sulfonylureas. Monitor therapy
Tafenoquine: May increase the serum concentration of MATE1 Substrates. Management: Avoid use of MATE substrates with tafenoquine, and if the combination cannot be avoided, monitor closely for evidence of toxicity of the MATE substrate and consider a reduced dose of the MATE substrate according to that substrate's labeling. Consider therapy modification
Tafenoquine: May increase the serum concentration of OCT2 Substrates. Management: Avoid use of OCT2 substrates with tafenoquine, and if the combination cannot be avoided, monitor closely for evidence of toxicity of the OCT2 substrate and consider a reduced dose of the OCT2 substrate according to that substrate's labeling. Consider therapy modification
Tezacaftor and Ivacaftor: May increase the serum concentration of GlipiZIDE. Monitor therapy
Thiazide and Thiazide-Like Diuretics: May diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Thiazolidinediones: May enhance the hypoglycemic effect of Sulfonylureas. Management: Consider sulfonylurea dose adjustments in patients taking thiazolidinediones and monitor for hypoglycemia. Consider therapy modification
Topiramate: May enhance the adverse/toxic effect of MetFORMIN. Monitor therapy
Trimethoprim: May increase the serum concentration of MetFORMIN. Monitor therapy
Trospium: MetFORMIN may decrease the serum concentration of Trospium. Monitor therapy
Vandetanib: May increase the serum concentration of MetFORMIN. Monitor therapy
Verapamil: May diminish the therapeutic effect of MetFORMIN. Monitor therapy
Verteporfin: Photosensitizing Agents may enhance the photosensitizing effect of Verteporfin. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Sulfonylureas may enhance the anticoagulant effect of Vitamin K Antagonists. Vitamin K Antagonists may enhance the hypoglycemic effect of Sulfonylureas. Monitor therapy
Voriconazole: May increase the serum concentration of Sulfonylureas. Monitor therapy
Adverse Reactions
Also see individual agents.
>10%:
Central nervous system: Headache (13%)
Endocrine & metabolic: Hypoglycemia (8% to 13%)
Gastrointestinal: Diarrhea (2% to 18%)
1% to 10%:
Cardiovascular: Hypertension (3% to 4%)
Central nervous system: Dizziness (2% to 5%)
Gastrointestinal: Nausea and vomiting (≤8%), abdominal pain (6%)
Genitourinary: Urinary tract infection (1%)
Neuromuscular & skeletal: Musculoskeletal pain (8%)
Respiratory: Upper respiratory tract infection (8% to 10%)
Warnings/Precautions
Concerns related to adverse effects:
- Cardiovascular mortality: Product labeling states oral hypoglycemic drugs may be associated with an increased cardiovascular mortality as compared to treatment with diet alone or diet plus insulin. Data to support this association are limited, and several studies, including a large prospective trial (UKPDS 1998), have not supported an association. Metformin does not appear to share this risk. In patients with established atherosclerotic cardiovascular disease (ASCVD), other agents are preferred (ADA 2019).
- Hypoglycemia: All sulfonylurea drugs are capable of producing severe hypoglycemia. Hypoglycemia is more likely to occur when caloric intake is deficient, after severe or prolonged exercise, when ethanol is ingested, or when more than one glucose-lowering drug is used. It is also more likely in elderly patients, malnourished patients and in patients with impaired renal, hepatic, adrenal and/or pituitary function; use with caution.
- Lactic acidosis: [US Boxed Warning]: Postmarketing cases of metformin-associated lactic acidosis have resulted in death, hypothermia, hypotension, and resistant bradyarrhythmias. The onset is often subtle, accompanied by nonspecific symptoms (eg, malaise, myalgias, respiratory distress, somnolence, abdominal pain); elevated blood lactate levels (>5 mmol/L); anion gap acidosis (without evidence of ketonuria or ketonemia); increased lactate:pyruvate ratio; metformin plasma levels generally >5 mcg/mL. Risk factors for lactic acidosis include patients with renal impairment, concomitant use of certain drugs (eg, cationic drugs such as topiramate), ≥65 years of age, having a radiologic study with contrast, surgery and other procedures, hypoxic states (eg, acute heart failure), excessive alcohol intake, and hepatic impairment. Discontinue immediately if lactic acidosis is suspected; prompt hemodialysis is recommended. Lactic acidosis should be suspected in any patient with diabetes receiving metformin with evidence of acidosis but without evidence of ketoacidosis. Discontinue metformin in patients with conditions associated with dehydration, sepsis, or hypoxemia. The risk of accumulation and lactic acidosis increases with the degree of impairment of renal function.
- Sulfonamide (“sulfa”) allergy: The FDA-approved product labeling for many medications containing a sulfonamide chemical group includes a broad contraindication in patients with a prior allergic reaction to sulfonamides. There is a potential for cross-reactivity between members of a specific class (eg, two antibiotic sulfonamides). However, concerns for cross-reactivity have previously extended to all compounds containing the sulfonamide structure (SO2NH2). An expanded understanding of allergic mechanisms indicates cross-reactivity between antibiotic sulfonamides and nonantibiotic sulfonamides may not occur or at the very least this potential is extremely low (Brackett 2004; Johnson 2005; Slatore 2004; Tornero 2004). In particular, mechanisms of cross-reaction due to antibody production (anaphylaxis) are unlikely to occur with nonantibiotic sulfonamides. T-cell-mediated (type IV) reactions (eg, maculopapular rash) are less well understood and it is not possible to completely exclude this potential based on current insights. In cases where prior reactions were severe (Stevens-Johnson syndrome/TEN), some clinicians choose to avoid exposure to these classes.
- Vitamin B12 concentrations: Long-term metformin use is associated with vitamin B12 deficiency; monitor vitamin B12 serum concentrations periodically with long-term therapy. Monitoring of B12 serum concentrations should be considered in all patients receiving metformin and in particular those with peripheral neuropathy or anemia (ADA 2019).
Disease-related concerns:
- Bariatric surgery:
– Altered absorption: Use IR formulations after surgery to minimize the potential effects of bypassing stomach and proximal small bowel with gastric bypass or more rapid gastric emptying and proximal small bowel transit with sleeve gastrectomy (Apovian 2015). ER tablets may have a reduced effect due to these procedures (Mechanick 2013; Melissas 2013). After gastric bypass (Roux-en-Y gastric bypass [RYGB]), administration of IR tablets led to increased absorption (AUC0-∞ increased by 21%) and bioavailability (increased by 50%) (Padwal 2011). ER formulations may have altered release and absorption patterns after gastric bypass or sleeve gastrectomy (but not gastric band). Compared to control, Tmax in a gastric bypass cohort administered tolbutamide was significantly shorter (1.4 ± 1.8 vs 5.1 ± 1.7 hours; P < 0.001) while Cmax and AUC0-∞ were not altered (Tandra 2013). Lactate levels decrease after gastric bypass (RYGB)-induced weight loss irrespective of the use of metformin. Routinely lowering metformin dose after gastric bypass is not necessary as long as normal renal function is preserved (Deden 2018).
– Hypoglycemia: Use an antidiabetic agent without the potential for hypoglycemia if possible; hypoglycemia may occur after gastric bypass, sleeve gastrectomy, and gastric band (Mechanick 2013). Insulin secretion and sensitivity may be partially or completely restored after these procedures (gastric bypass is most effective, followed by sleeve and finally band) (Korner 2009; Peterli 2012). First-phase insulin secretion and hepatic insulin sensitivity have been shown to be significantly improved in the immediate days after gastric bypass and sleeve gastrectomy. The restorative effects of these procedures on peripheral insulin sensitivity may occur later in the 3- to 12-month period postsurgery (Mingrone 2016).
- Weight gain: Evaluate risk vs benefit and consider alternative therapy after gastric bypass, sleeve gastrectomy, and gastric banding; weight gain may occur (Apovian 2015).
- Glucose-6-phosphate dehydrogenase (G6PD) deficiency: Patients with G6PD deficiency may be at an increased risk of sulfonylurea-induced hemolytic anemia; however, cases have also been described in patients without G6PD deficiency during postmarketing surveillance. Use with caution and consider a nonsulfonylurea alternative in patients with G6PD deficiency.
- Heart failure: Metformin may be used in patients with stable heart failure (HF); avoid use in unstable or hospitalized patients with HF (ADA 2019). Risk of lactic acidosis may be increased secondary to hypoperfusion. In a scientific statement from the American Heart Association, metformin has been determined to be an agent that may exacerbate underlying myocardial dysfunction (magnitude: major) (AHA [Page 2016]). Use of metformin in patients with HF may be associated with reduced mortality and reduction in hospital readmission for HF (Crowley 2017; Eurich 2013).
- Hepatic impairment: The manufacturer recommends to generally avoid use in patients with hepatic impairment due to potential for lactic acidosis. However, continued use of metformin in patients with diabetes with liver dysfunction, including cirrhosis, may be associated with a survival benefit in carefully selected patients (Brackett 2010; Crowley 2017; Zhang 2014).
- Renal impairment: The metabolism and excretion of glipizide may be slowed in patients with renal impairment. Metformin is substantially excreted by the kidney; assess renal function prior to initiation of therapy and periodically thereafter using eGFR. The risk of metformin accumulation and lactic acidosis increases with degree of renal impairment. Initiation of therapy is not recommended if eGFR is between 30 to 45 mL/minute/1.73 m2 and is contraindicated in patients with eGFR <30 mL/minute/1.73 m2. Assess benefits/risks of continuing metformin therapy in patients whose eGFR falls below 45 mL/minute/1.73 m2 during therapy; if used, metformin dosage reduction is recommended (ADA [Lipska 2011]; Inzucchi 2014). Use of concomitant medications that may affect renal function (ie, affect tubular secretion) may also affect metformin disposition. Metformin should be withheld in patients with dehydration and/or prerenal azotemia.
- Stress-related states: It may be necessary to discontinue metformin and administer insulin if the patient is exposed to stress (fever, trauma, infection, surgery).
Special populations:
- Debilitated/malnourished: May be more susceptible to hypoglycemia; use with caution and do not titrate to maximum dose.
- Elderly: Use with caution; risk of metformin associated lactic acidosis increases with age.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Appropriate use: Not indicated for use in patients with type 1 diabetes mellitus or with diabetic ketoacidosis (DKA).
- Ethanol use: Instruct patients to avoid excessive acute or chronic ethanol use; ethanol may potentiate metformin's effect on lactate metabolism and increase risk of hypoglycemia.
- Iodinated contrast: According to the manufacturer, it is recommended to temporarily discontinue metformin at the time of or before iodinated contrast imaging procedures in patients with an eGFR 30 to 60 mL/minute/1.73 m2; with a history of hepatic disease, alcoholism, or heart failure; or in patients who will receive intra-arterial iodinated contrast. Reevaluate eGFR 48 hours after imaging procedure; restart if renal function is stable. Alternatively, the American College of Radiology (ACR) guidelines recommend that metformin may be used prior to or following administration of iodinated contrast media in patients with no evidence of acute kidney injury (AKI) and with an eGFR ≥30 mL/minute/1.73 m2; ACR guidelines recommend temporary discontinuation of metformin in patients with known AKI or severe chronic kidney disease (stage IV or V [ie, eGFR <30 mL/minute/1.73 m2]) or who are undergoing arterial catheter studies (ACR 2017).
- Surgical procedures: Metformin should be withheld the day of surgery (all other oral hypoglycemic agents should be withheld the morning of surgery or procedure) (ADA 2019). Resume only after oral intake resumed and normal renal function is verified.
Monitoring Parameters
Signs and symptoms of hypoglycemia, HbA1c (at least twice yearly in patients who have stable glycemic control and are meeting treatment goals; quarterly in patients not meeting treatment goals or with therapy change (ADA 2019), plasma glucose. Initial and periodic monitoring of hematologic parameters (eg, hemoglobin/hematocrit and red blood cell indices); renal function (eGFR) prior to therapy initiation and at least annually (more often in patients at risk of developing renal impairment; every 3 to 6 months if eGFR 45 to <60 mL/minute/1.73 m2; every 3 months if eGFR 30 to <45 mL/minute/1.73 m2 [Lipska 2011]); monitor vitamin B12 serum concentrations periodically with long-term therapy; folate (if megaloblastic anemia is suspected).
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Metformin crosses the placenta (ADA 2020). Animal reproduction studies were not conducted with this combination. Refer to individual agents.
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience headache, nausea, vomiting, diarrhea, common cold symptoms, abdominal pain, dizziness, or muscle pain. Have patient report immediately to prescriber signs of lactic acidosis (fast breathing, fast heartbeat, abnormal heartbeat, vomiting, fatigue, shortness of breath, severe loss of strength and energy, severe dizziness, feeling cold, or muscle pain or cramps), or signs of low blood sugar (dizziness, headache, fatigue, feeling weak, shaking, fast heartbeat, confusion, increased hunger, or sweating) (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for health care professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience, and judgment in diagnosing, treating, and advising patients.