Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution Reconstituted, Injection, as sodium succinate [strength expressed as base, preservative free]:
Solu-CORTEF: 100 mg (1 ea); 250 mg (1 ea); 500 mg (1 ea); 1000 mg (1 ea)
Tablet, Oral, as base:
Cortef: 5 mg, 10 mg, 20 mg [scored]
Generic: 5 mg, 10 mg, 20 mg
Pharmacology
Mechanism of Action
Short-acting corticosteroid with minimal sodium-retaining potential; decreases inflammation by suppression of migration of polymorphonuclear leukocytes and reversal of increased capillary permeability
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid
Distribution
Vd: IV: 27 ± 7 L (Czock 2005)
Metabolism
Hepatic
Excretion
Urine (Czock 2005)
Onset of Action
IV: 1 hour
Time to Peak
Plasma: Oral: 1.2 ± 0.4 hours (Czock 2005)
Half-Life Elimination
IV: 2 ± 0.3 hours; Oral: 1.8 ± 0.5 hours (Czock 2005)
Protein Binding
IV: 92% ± 2% (Czock 2005)
Use: Labeled Indications
Allergic states: Control of severe or incapacitating allergic conditions intractable to adequate trials of conventional treatment in drug hypersensitivity reactions, perennial or seasonal allergic rhinitis, serum sickness, transfusion reactions, or acute noninfectious laryngeal edema (epinephrine is the drug of first choice).
Dermatologic diseases: Atopic dermatitis; bullous dermatitis herpetiformis; contact dermatitis; exfoliative dermatitis; exfoliative erythroderma; pemphigus; severe erythema multiforme (Stevens-Johnson syndrome); severe psoriasis; severe seborrheic dermatitis; mycosis fungoides.
Edematous states: To induce diuresis or remission of proteinuria in the nephrotic syndrome, without uremia, of the idiopathic type or that due to lupus erythematosus.
Endocrine disorders: Acute adrenocortical insufficiency; congenital adrenal hyperplasia; hypercalcemia associated with cancer; nonsuppurative thyroiditis; primary or secondary adrenocortical insufficiency; preoperatively and in the event of serious trauma or illness, in patients with known adrenal insufficiency or when adrenocortical reserve is doubtful; shock unresponsive to conventional therapy if adrenocortical insufficiency exists or is suspected.
GI diseases: To tide the patient over a critical period of the disease in ulcerative colitis and regional enteritis.
Hematologic disorders: Acquired (autoimmune) hemolytic anemia; congenital (erythroid) hypoplastic anemia (Diamond Blackfan anemia); erythroblastopenia (RBC anemia); immune thrombocytopenia (formerly known as idiopathic thrombocytopenic purpura) in adults; pure red cell aplasia; select cases of secondary thrombocytopenia.
Neoplastic diseases: Palliative management of leukemias and lymphomas (adults); acute leukemia of childhood.
Nervous system: Cerebral edema associated with primary or metastatic brain tumor, or craniotomy.
Ophthalmic diseases: Severe acute and chronic allergic and inflammatory processes involving the eye, such as allergic conjunctivitis; allergic corneal marginal ulcers; anterior segment inflammation; chorioretinitis; diffuse posterior uveitis and choroiditis; herpes zoster ophthalmicus; iritis and iridocyclitis; keratitis; optic neuritis; sympathetic ophthalmia; other ocular inflammatory conditions unresponsive to topical corticosteroids.
Respiratory diseases: Aspiration pneumonitis; bronchial asthma; berylliosis; fulminating or disseminated pulmonary tuberculosis when used concurrently with appropriate antituberculous chemotherapy; idiopathic eosinophilic pneumonias; Loeffler syndrome (not manageable by other means); symptomatic sarcoidosis.
Rheumatic disorders: As adjunctive therapy for short-term administration in acute and subacute bursitis, acute gouty arthritis, acute nonspecific tenosynovitis, ankylosing spondylitis, epicondylitis, posttraumatic osteoarthritis, psoriatic arthritis, rheumatoid arthritis, including juvenile rheumatoid arthritis, synovitis of osteoarthritis; during an exacerbation or as maintenance therapy in acute rheumatic carditis, dermatomyositis (polymyositis), temporal arteritis, and systemic lupus erythematosus.
Miscellaneous: Trichinosis with neurologic or myocardial involvement; tuberculous meningitis with subarachnoid block or impending block when used concurrently with appropriate antituberculous chemotherapy.
Use: Off Label
In-hospital cardiac arrestcyes
Data from two randomized controlled trials in patients experiencing in-hospital cardiac arrest (IHCA) suggest that the combination of vasopressin, epinephrine (standard dose), and methylprednisolone administered during cardiac arrest followed by hydrocortisone given after return of spontaneous circulation may be beneficial for the treatment of patients in this setting Mentzelopoulos 2009, Mentzelopoulos 2013. Additional trials are necessary to further define the role of this regimen and of hydrocortisone (post-arrest) for the treatment of patients who experience IHCA.
Based on the 2015 American Heart Association (AHA) Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care, the intra-arrest use of vasopressin (in combination with epinephrine and methylprednisolone) in patients with IHCA followed by hydrocortisone given after return of spontaneous circulation may be considered (based on limited evidence); however, further studies are warranted before routine administration of this combination can be recommended.
Septic shockbyes
Data from two double-blind, placebo controlled, randomized trials suggest that hydrocortisone may be beneficial in patients with septic shock refractory to initial volume resuscitation and vasopressors. In these trials, hydrocortisone did not improve mortality compared to placebo but did aid in more rapid reversal of shock Sprung 2008, Venkatesh 2018. Two additional double-blind, placebo controlled, randomized trials suggest the combination of hydrocortisone plus fludrocortisone may be beneficial in this same population, and may also provide a mortality benefit Annane 2002, Annane 2018 .
Based on the Surviving Sepsis Campaign International Guidelines for Management of Severe Sepsis and Septic Shock, intravenous hydrocortisone is suggested, only after adequate fluid resuscitation and vasopressor therapy are unable to restore hemodynamic stability, in adults with septic shock Rhodes 2017. Note: Corticosteroids should not be administered for the treatment of sepsis in the absence of shock or for septic shock that is responsive to fluid resuscitation and vasopressors. Rhodes 2017, SCCM/ESICM [Annane 2017].
Thyroid stormyes
Based on the American Thyroid Association guidelines for the diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis, a multimodal approach including beta blockade, antithyroid drug therapy, inorganic iodide, corticosteroid therapy, aggressive cooling with acetaminophen and cooling blankets, volume resuscitation, nutritional and respiratory support, and monitoring in an intensive care unit is effective and suggested when treating thyroid storm.
Contraindications
Hypersensitivity to hydrocortisone or any component of the formulation; systemic fungal infections; use in premature infants (formulations containing benzyl alcohol only); idiopathic thrombocytopenia purpura (IM administration only); intrathecal administration; live or live, attenuated virus vaccines (with immunosuppressive doses of corticosteroids).
Canadian labeling: Additional contraindications (not in US labeling): Herpes simplex of the eye (except for short-term or emergency therapy); vaccinia and varicella (except for short-term or emergency therapy)
Documentation of allergenic cross-reactivity for corticosteroids is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Dosage and Administration
Dosing: Adult
Note: Adjust dose depending upon condition being treated and response of patient. The lowest possible dose should be used to control the condition; when dose reduction is possible, the dose should be reduced gradually. In life-threatening situations, parenteral doses larger than the oral dose may be needed.
Asthma, acute exacerbation (off-label dose): Oral: 200 mg in divided doses for 5 to 7 days (GINA 2018).
Anti-inflammatory or immunosuppressive:
IM, IV: Initial: 100 to 500 mg/dose at intervals of 2, 4, or 6 hours.
Oral: Initial: 20 to 240 mg/day.
Adrenal insufficiency, acute (adrenal crisis):
Note: Appropriate fluid resuscitation is also required (Endocrine Society [Bornstein 2016]; Gardner 2011).
IV: 100 mg IV bolus given immediately, followed by 25 to 75 mg IV every 6 hours or 200 mg/24 hours as a continuous IV infusion for the first 24 hours. After the initial 24 hours, may gradually taper the dose; once patient is stable, may resume oral maintenance dosing (Allolio 2015; Endocrine Society [Bornstein 2016]; Endocrine Society [Speiser 2018]; Gardner 2011).
Adrenal insufficiency, chronic (eg, primary, secondary, classic congenital adrenal hyperplasia): Oral: 15 to 25 mg/day in 2 to 3 divided doses. Administer the largest dose in the morning upon awakening, followed by next dose 2 hours after lunch (2-dose regimen) or next dose at lunch, followed by smallest dose in the afternoon no later than 4 to 6 hours before bedtime (3-dose regimen) (Endocrine Society [Bornstein 2016]; Endocrine Society [Fleseriu 2016]; Endocrine Society [Speiser 2018]).
Adrenal insufficiency (temporary), physiologic replacement following resection of an ACTH-producing tumor or unilateral adrenalectomy (off-label dose): Oral: 10 to 12 mg/m2/day in 2 to 3 divided doses, with the first dose taken as soon as possible after waking; continue hydrocortisone until HPA axis recovers, generally 6 to 12 months following resection of ACTH-producing tumors or 18 months following unilateral adrenalectomy (Endocrine Society [Neiman 2015]).
Stress dosing in patients known to be adrenally-suppressed (ie, prevention of adrenal crisis in glucocorticoid-treated patients) (off-label dose):
Sickness:
Illness with fever: Oral: Double the routine oral hydrocortisone dose until recovery for fever >38°C (100.4°F) or triple the routine oral hydrocortisone dose until recovery for fever >39°C (102.2°F); return to standard dose within 1 to 2 days (Allolio 2015).
Gastroenteritis with vomiting and/or diarrhea: IM, SubQ: 100 mg dose given early in course of illness; repeat after 6 to 12 hours (Allolio 2015).
Severe infection (eg, pneumonia/with altered cognition): IM, SubQ: 100 mg dose given early in course of illness; repeat after 6 to 12 hours until recovery (Allolio 2015).
Surgery:
Minor stress (ie, inguinal herniorrhaphy): IV: 25 mg/day for 1 day (Coursin 2002; Salem 1994).
Moderate stress (ie, joint replacement, cholecystectomy): IV: 50 to 75 mg/day (25 mg every 8 to 12 hours) for 1 to 2 days (Coursin 2002; Salem 1994).
Major stress (pancreatoduodenectomy, esophagogastrectomy, cardiac surgery): IV: 100 to 150 mg/day (50 mg every 8 to 12 hours) for 2 to 3 days (Coursin 2002; Salem 1994).
Septic shock (off-label use): Note: Corticosteroids should only be used for septic shock that is not responsive to volume resuscitation and vasopressors (Rhodes 2017; SCCM/ESICM [Annane 2017]).
IV: 50 mg bolus every 6 hours, either as monotherapy (Sprung 2008) or in combination with fludrocortisone (Annane 2002; Annane 2018) or 200 mg/day as a continuous infusion (Venkatesh 2018). Guidelines suggest a therapy duration of ≥3 days (Rhodes 2017; SCCM/ESICM [Annane 2017]); most studies treated for up to 7 days; not all studies tapered therapy. May consider a slow taper over several days when vasopressors are no longer required to avoid possible hemodynamic deterioration which may occur with abrupt withdrawal (Keh 2003; Rhodes 2017).
Note: Low-dose hydrocortisone in septic shock patients may cause a significant increase in hyperglycemia and hypernatremia. A small study demonstrated that repetitive bolus doses of hydrocortisone caused significant hyperglycemia that was not seen during continuous infusion (Weber-Carstens 2007); practice guidelines recommend strategies for avoidance and/or detection of these side effects, such as dosing by continuous infusion (Rhodes 2017).
Thyroid storm (off-label use): IV: 300 mg loading dose, followed by 100 mg every 8 hours (ATA [Ross 2016]).
Ulcerative colitis, acute (severe), remission induction (off-label dose): IV: 100 mg every 6 to 8 hours (ACG [Rubin 2019]).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Adjust dose depending upon condition being treated and response of patient. The lowest possible dose should be used to control the condition; when dose reduction is possible, the dose should be reduced gradually. In life-threatening situations, parenteral doses larger than the oral dose may be needed.
Adrenal insufficiency; acute (adrenal crisis): Dosage regimens variable: IM, IV (preferred):
Weight-directed: Limited data available: Infants, Children, and Adolescents: Initial: 2 to 3 mg/kg; maximum dose: 100 mg/dose; then for infants: 1 to 5 mg/kg/dose every 6 hours; for children and adolescents, see BSA- or age-directed dosing; may also be administered I.O. if necessary (Cameron 2012; Hegenbarth 2008; Marx 2014)
BSA-directed dosing: Limited data available: Infants, Children, and Adolescents: Initial: 50 to 100 mg/m2 once followed by 50 to 100 mg/m2/day in 4 divided doses (Ahmet 2011; Auron 2015; Hegenbarth 2008; Shulman 2007)
Age-directed dosing (fixed dosing): Limited data available (Cameron 2012; Elder 2015; Kliegman 2016):
Infants: 10 to 25 mg once followed by 10 to 25 mg/day in divided doses every 6 hours for 24 hours then subsequent dose reductions and rate determined by patient response
Children <5 years (eg, young children): 25 to 50 mg once followed by 25 to 50 mg/day in divided doses every 6 hours for 24 hours then subsequent dose reductions and rate determined by patient response
Children ≥5 years (eg, older children): 50 to 100 mg once followed by 50 mg/day in divided doses every 6 hours for 24 hours then subsequent dose reductions and rate determined by patient response
Adolescents: 100 mg once followed by 100 mg/day in divided doses every 6 hours for 24 hours then subsequent dose reduction and rate determined by patient response
Anti-inflammatory or immunosuppressive: Note: Dosing range variable; individualize dose for disease state and patient response.
Infants and Children:
Oral: 2.5 to 10 mg/kg/day or 75 to 300 mg/m2/day divided every 6 to 8 hours (Kliegman 2007)
IM, IV:
Manufacturer's labeling: Initial: 0.56 to 8 mg/kg/day or 20 to 240 mg/m2/day in 3 or 4 divided doses
Alternate dosing: Limited data available: 1 to 5 mg/kg/day or 30 to 150 mg/m2/day divided every 12 to 24 hours (Kliegman 2007)
Adolescents: Oral, IM, IV, SubQ: 15 to 240 mg every 12 hours (Kliegman 2007)
Congenital adrenal hyperplasia: Infants, Children, and Adolescents: AAP Recommendations: Note: Administer morning dose as early as possible. Tablets may result in more reliable serum concentrations than oral liquid formulation; use of oral suspension is not recommended. Individualize dose by monitoring growth, hormone levels, and bone age; mineralocorticoid (eg, fludrocortisone) and sodium supplement may be required in salt losers (AAP 2000; AAP 2010; Endocrine Society 2010)
Initial: Oral (tablets): 10 to 15 mg/m2/day in 3 divided doses; higher initial doses (20 mg/m2/day) may be required to achieve initial target hormone serum concentrations (AAP 2010; Endocrine Society 2010).
Maintenance dose: Oral (tablets): Usual requirement:
Infants: 2.5 to 5 mg/dose 3 times/day
Children: 5 to 10 mg/dose 3 times/day
Adolescents (fully grown): 15 to 25 mg/day divided in 2 to 3 daily doses
Physiologic replacement: Infants and Children: Oral: 8 to 10 mg/m2/day divided every 8 hours; up to 12 mg/m2/day in some patients; to replicate diurnal variation, the highest doses are typically administered in the morning and midday dose with the lower dose in the evening (Ahmet 2011; Elder 2015; Gupta 2008; Maguire 2007; Shulman 2007)
Stress dosing; supplemental: Limited data available; dosage regimens variable: Infants, Children, and Adolescents: Note: Dosing based on the level of physiological stress related to condition, dose should be individualized based on patient and continued until resolution of stressful condition (usually 24 to 48 hours) (Shulman 2007). Typically, supplementation for emotional or minimal physiological stress conditions or prior to exercise is not necessary (Elder 2010; Endocrine Society [Speiser 2010]; Shulman 2007). Dosing is generally 2 to 3 times physiologic replacement level (Elder 2010; Shulman 2007).
BSA-directed dosing (Ahmet 2011; Shulman 2007): Oral, IM, IV:
Mild to moderate stress: 20 to 50 mg/m2/day divided into 3 or 4 doses; doses on the lower end of the range (20 to 30 mg/m2/day) may be divided twice daily
Major stress or surgery: 100 mg/m2/day in divided doses every 6 hours
Planned surgery: Pre-anesthesia of 50 mg/m2 IV or IM administered 30 to 60 minutes prior to surgery followed by second dose of 50 mg/m2 as a continuous IV infusion or in divided doses every 6 hours for at least 24 hours
Age-directed for moderate stress in patients with congenital adrenal hyperplasia (Endocrine Society [Speiser 2010]):
Infants and preschool children: IV: Initial dose: 25 mg once, followed by a daily dose that is 3 to 4 times the patient's standard maintenance dose in divided doses every 6 hours
School-age children: IV: Initial dose: 50 mg once, followed by a daily dose that is 3 to 4 times the patient's standard maintenance dose in divided doses every 6 hours
Adolescents: IV: Initial dose: 100 mg once, followed by a daily dose that is 3 to 4 times the patient's standard maintenance dose in divided doses every 6 hours
Septic shock; catecholamine-refractory with suspected/proved adrenal insufficiency: Limited data available: Infants, Children, and Adolescents: IV: 50 to 100 mg/m2/day (Dellinger 2013; Marx 2014; Shulman 2007); in some cases, doses may be titrated up to 50 mg/kg/day if necessary for shock reversal; however, efficacy data variable with the higher doses (Brierley 2009; Menon 2012)
Reconstitution
IV bolus or IM administration: Reconstitute 100 mg vials with bacteriostatic water or bacteriostatic sodium chloride (not >2 mL).
IV infusion administration: Add reconstituted solutions to an appropriate volume of D5W, NS, or D5NS (100 to 1,000 mL for a 100 mg solution; 250 to 1,000 mL for a 250 mg solution; 500 to 1,000 mL for a 500 mg solution; 1,000 mL for a 1,000 mg solution). In cases where administration of a small volume of fluid is desirable, 100 to 3,000 mg of hydrocortisone may be added to 50 mL of D5W or NS.
Act-O-Vial: Press the activator to force diluent into the powder compartment. Following gentle agitation, solution may be withdrawn via syringe through a needle inserted into the center of the stopper.
Extemporaneously Prepared
2 mg/mL Oral Suspension (ASHP Standard Concentration) (ASHP 2017)
A 2 mg/mL oral suspension may be made with 10 mg tablets and a 1:1 mixture of Ora-Sweet and Ora-Plus. Crush ten 10 mg hydrocortisone tablets in a mortar and reduce to a fine powder. Add a small amount of vehicle and mix to a uniform paste; mix while adding the vehicle in incremental proportions to almost 50 mL; transfer to a calibrated amber bottle, rinse mortar with vehicle, and add sufficient quantity of vehicle to make 50 mL. Label “shake well.” Stable under refrigeration or at room temperature for 90 days.
Chong G, Decarie D, Ensom MHH. Stability of hydrocortisone in extemporaneously compounded suspension. J Inform Pharmacother. 2003;13:100-110.
2.5 mg/mL Oral Suspension
A 2.5 mg/mL oral suspension may be made with either tablets or powder and a vehicle containing sodium carboxymethylcellulose (1 g), syrup BP (10 mL), hydroxybenzoate 0.1% preservatives (0.1 g), polysorbate 80 (0.5 mL), citric acid (0.6 g), and water. To make the vehicle, dissolve the hydroxybenzoate, citric acid, and syrup BP in hot water. Cool solution and add the carboxymethylcellulose; leave overnight. Crush twelve-and-one-half 20 mg hydrocortisone tablets (or use 250 mg of powder) in a mortar and reduce to a fine powder while adding polysorbate 80. Add small portions of vehicle and mix to a uniform paste; mix while adding the vehicle in incremental proportions to almost 100 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add sufficient quantity of vehicle to make 100 mL. Label “shake well” and “refrigerate.” Stable for 90 days.
Fawcett JP, Boulton DW, Jiang R, et al. Stability of hydrocortisone oral Suspensions prepared from tablets and powder. Ann Pharmacother. 1995;29(10):987-990.8845559
Administration
Oral: Administer with food or milk to decrease GI upset.
Parenteral: For IM or IV administration: Dermal and/or subdermal skin depression may occur at injection site.
IM: Avoid injection into deltoid muscle (high incidence of subcutaneous atrophy).
IV bolus: Administer undiluted over at least 30 seconds; for large doses (≥500 mg), administer over 10 minutes.
IV intermittent infusion: Further dilute in a compatible fluid and administer over 20 to 30 minutes.
Dietary Considerations
Systemic use of corticosteroids may require a diet with increased potassium, vitamins A, B6, C, D, folate, calcium, zinc, phosphorus, and decreased sodium. Some products may contain sodium.
Storage
Oral: Store at 20°C to 25°C (68°F to 77°F).
Injection: Store intact vials at 20°C to 25°C (68°F to 77°F); protect from light. Heat sensitive; do not autoclave vial. Reconstituted solutions are stable for 3 days at 20°C to 25°C (68°F to 77°F); protect from light. Solutions prepared for IV infusion are stable for at least 4 hours.
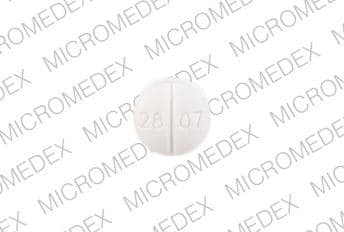
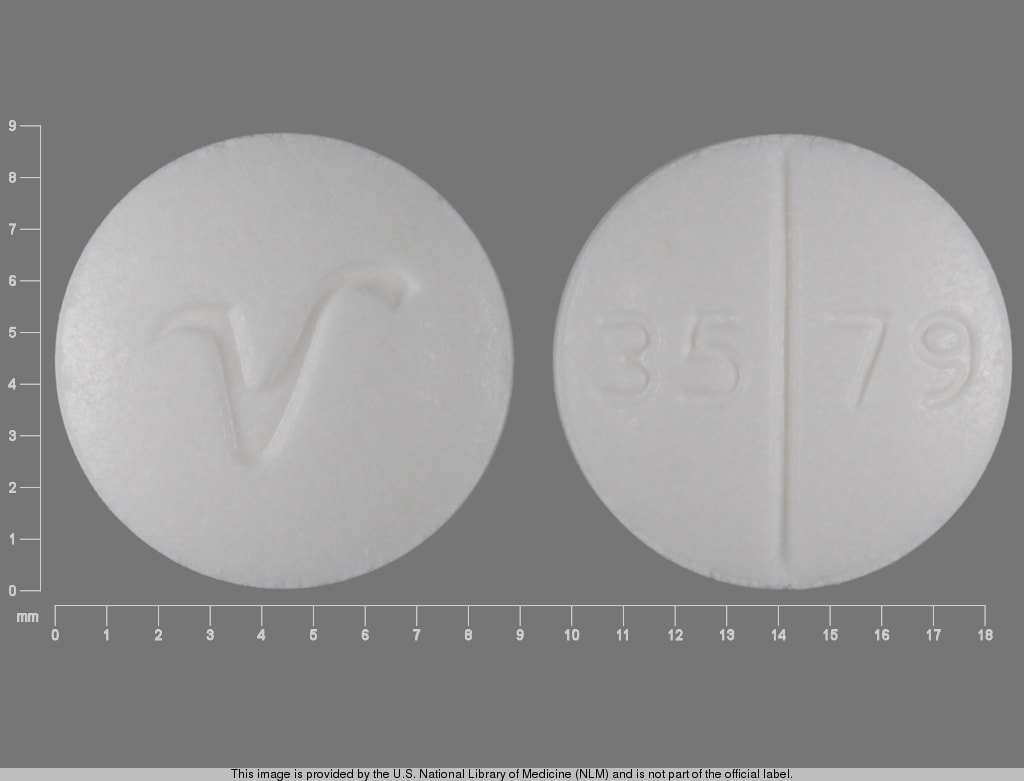
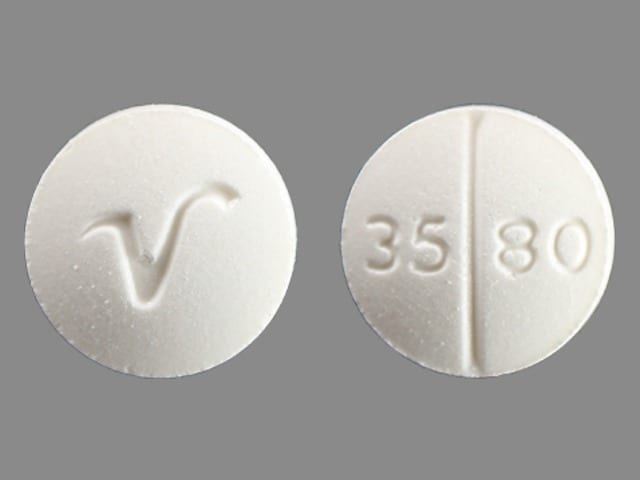
Hydrocortisone (Systemic) Images
Drug Interactions
Acetylcholinesterase Inhibitors: Corticosteroids (Systemic) may enhance the adverse/toxic effect of Acetylcholinesterase Inhibitors. Increased muscular weakness may occur. Monitor therapy
Aldesleukin: Corticosteroids may diminish the antineoplastic effect of Aldesleukin. Avoid combination
Amphotericin B: Corticosteroids (Systemic) may enhance the hypokalemic effect of Amphotericin B. Monitor therapy
Androgens: Corticosteroids (Systemic) may enhance the fluid-retaining effect of Androgens. Monitor therapy
Antacids: May decrease the bioavailability of Corticosteroids (Oral). Management: Consider separating doses by 2 or more hours. Budesonide enteric coated tablets could dissolve prematurely if given with drugs that lower gastric acid, with unknown impact on budesonide therapeutic effects. Consider therapy modification
Antidiabetic Agents: Hyperglycemia-Associated Agents may diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Aprepitant: May increase the serum concentration of Corticosteroids (Systemic). Management: No dose adjustment is needed for single 40 mg aprepitant doses. For other regimens, reduce oral dexamethasone or methylprednisolone doses by 50%, and IV methylprednisolone doses by 25%. Antiemetic regimens containing dexamethasone reflect this adjustment. Consider therapy modification
Axicabtagene Ciloleucel: Corticosteroids (Systemic) may diminish the therapeutic effect of Axicabtagene Ciloleucel. Management: Avoid use of corticosteroids as premedication before axicabtagene ciloleucel. Corticosteroids may, however, be required for treatment of cytokine release syndrome or neurologic toxicity. Consider therapy modification
Baricitinib: Immunosuppressants may enhance the immunosuppressive effect of Baricitinib. Management: Use of baricitinib in combination with potent immunosuppressants such as azathioprine or cyclosporine is not recommended. Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted. Consider therapy modification
BCG (Intravesical): Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Bile Acid Sequestrants: May decrease the absorption of Corticosteroids (Oral). Monitor therapy
Calcitriol (Systemic): Corticosteroids (Systemic) may diminish the therapeutic effect of Calcitriol (Systemic). Monitor therapy
Cladribine: May enhance the immunosuppressive effect of Immunosuppressants. Avoid combination
Coccidioides immitis Skin Test: Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. Monitor therapy
Corticorelin: Corticosteroids may diminish the therapeutic effect of Corticorelin. Specifically, the plasma ACTH response to corticorelin may be blunted by recent or current corticosteroid therapy. Monitor therapy
Cosyntropin: Hydrocortisone (Systemic) may diminish the diagnostic effect of Cosyntropin. Management: Patients receiving hydrocortisone should omit their pre-test dose on the day selected for cosyntropin testing. Consider therapy modification
CYP3A4 Inducers (Strong): May decrease the serum concentration of Hydrocortisone (Systemic). Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Corticosteroids (Systemic). Monitor therapy
Deferasirox: Corticosteroids (Systemic) may enhance the adverse/toxic effect of Deferasirox. Specifically, the risk for GI ulceration/irritation or GI bleeding may be increased. Monitor therapy
Deferasirox: Corticosteroids may enhance the adverse/toxic effect of Deferasirox. Specifically, the risk for GI ulceration/irritation or GI bleeding may be increased. Monitor therapy
Denosumab: May enhance the adverse/toxic effect of Immunosuppressants. Specifically, the risk for serious infections may be increased. Monitor therapy
Desirudin: Corticosteroids (Systemic) may enhance the anticoagulant effect of Desirudin. More specifically, corticosteroids may increase hemorrhagic risk during desirudin treatment. Management: Discontinue treatment with systemic corticosteroids prior to desirudin initiation. If concomitant use cannot be avoided, monitor patients receiving these combinations closely for clinical and laboratory evidence of excessive anticoagulation. Consider therapy modification
Desmopressin: Corticosteroids (Systemic) may enhance the hyponatremic effect of Desmopressin. Avoid combination
DilTIAZem: May increase the serum concentration of Corticosteroids (Systemic). Monitor therapy
Echinacea: May diminish the therapeutic effect of Immunosuppressants. Consider therapy modification
Erdafitinib: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Estrogen Derivatives: May increase the serum concentration of Corticosteroids (Systemic). Monitor therapy
Fexinidazole [INT]: Corticosteroids (Systemic) may enhance the arrhythmogenic effect of Fexinidazole [INT]. Avoid combination
Fingolimod: Immunosuppressants may enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). Consider therapy modification
Fosaprepitant: May increase the serum concentration of Corticosteroids (Systemic). The active metabolite aprepitant is likely responsible for this effect. Consider therapy modification
Hyaluronidase: Corticosteroids may diminish the therapeutic effect of Hyaluronidase. Management: Patients receiving corticosteroids (particularly at larger doses) may not experience the desired clinical response to standard doses of hyaluronidase. Larger doses of hyaluronidase may be required. Consider therapy modification
Indacaterol: May enhance the hypokalemic effect of Corticosteroids (Systemic). Monitor therapy
Indium 111 Capromab Pendetide: Corticosteroids (Systemic) may diminish the diagnostic effect of Indium 111 Capromab Pendetide. Avoid combination
Isoniazid: Corticosteroids (Systemic) may decrease the serum concentration of Isoniazid. Monitor therapy
Lasmiditan: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Avoid combination
Leflunomide: Immunosuppressants may enhance the adverse/toxic effect of Leflunomide. Specifically, the risk for hematologic toxicity such as pancytopenia, agranulocytosis, and/or thrombocytopenia may be increased. Management: Consider not using a leflunomide loading dose in patients receiving other immunosuppressants. Patients receiving both leflunomide and another immunosuppressant should be monitored for bone marrow suppression at least monthly. Consider therapy modification
Loop Diuretics: Corticosteroids (Systemic) may enhance the hypokalemic effect of Loop Diuretics. Monitor therapy
Lumacaftor and Ivacaftor: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. Lumacaftor and Ivacaftor may increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Macimorelin: Corticosteroids (Systemic) may diminish the diagnostic effect of Macimorelin. Avoid combination
Mifamurtide: Corticosteroids (Systemic) may diminish the therapeutic effect of Mifamurtide. Avoid combination
MiFEPRIStone: May diminish the therapeutic effect of Corticosteroids (Systemic). MiFEPRIStone may increase the serum concentration of Corticosteroids (Systemic). Management: Avoid mifepristone in patients who require long-term corticosteroid treatment of serious illnesses or conditions (e.g., for immunosuppression following transplantation). Corticosteroid effects may be reduced by mifepristone treatment. Avoid combination
Mitotane: May decrease the serum concentration of Corticosteroids (Systemic). Consider therapy modification
Natalizumab: Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. Avoid combination
Neuromuscular-Blocking Agents (Nondepolarizing): May enhance the adverse neuromuscular effect of Corticosteroids (Systemic). Increased muscle weakness, possibly progressing to polyneuropathies and myopathies, may occur. Consider therapy modification
Nicorandil: Corticosteroids (Systemic) may enhance the adverse/toxic effect of Nicorandil. Gastrointestinal perforation has been reported in association with this combination. Monitor therapy
Nivolumab: Immunosuppressants may diminish the therapeutic effect of Nivolumab. Consider therapy modification
Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective): Corticosteroids (Systemic) may enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective). Monitor therapy
Nonsteroidal Anti-Inflammatory Agents (Nonselective): Corticosteroids (Systemic) may enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents (Nonselective). Monitor therapy
Ocrelizumab: May enhance the immunosuppressive effect of Immunosuppressants. Monitor therapy
P-glycoprotein/ABCB1 Inducers: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inducers may also further limit the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
P-glycoprotein/ABCB1 Inhibitors: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inhibitors may also enhance the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
Pidotimod: Immunosuppressants may diminish the therapeutic effect of Pidotimod. Monitor therapy
Pimecrolimus: May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Quinolones: Corticosteroids (Systemic) may enhance the adverse/toxic effect of Quinolones. Specifically, the risk of tendonitis and tendon rupture may be increased. Monitor therapy
Ranolazine: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Ritodrine: Corticosteroids may enhance the adverse/toxic effect of Ritodrine. Monitor therapy
Roflumilast: May enhance the immunosuppressive effect of Immunosuppressants. Consider therapy modification
Salicylates: May enhance the adverse/toxic effect of Corticosteroids (Systemic). These specifically include gastrointestinal ulceration and bleeding. Corticosteroids (Systemic) may decrease the serum concentration of Salicylates. Withdrawal of corticosteroids may result in salicylate toxicity. Monitor therapy
Sargramostim: Corticosteroids (Systemic) may enhance the therapeutic effect of Sargramostim. Specifically, corticosteroids may enhance the myeloproliferative effects of sargramostim. Monitor therapy
Siponimod: Immunosuppressants may enhance the immunosuppressive effect of Siponimod. Monitor therapy
Sipuleucel-T: Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. Consider therapy modification
Somatropin: Corticosteroids (Systemic) may diminish the therapeutic effect of Somatropin. Monitor therapy
Tacrolimus (Systemic): Corticosteroids (Systemic) may decrease the serum concentration of Tacrolimus (Systemic). Conversely, when discontinuing corticosteroid therapy, tacrolimus concentrations may increase. Monitor therapy
Tacrolimus (Topical): May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Tertomotide: Immunosuppressants may diminish the therapeutic effect of Tertomotide. Monitor therapy
Thiazide and Thiazide-Like Diuretics: Corticosteroids (Systemic) may enhance the hypokalemic effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Tisagenlecleucel: Corticosteroids (Systemic) may diminish the therapeutic effect of Tisagenlecleucel. Management: Avoid use of corticosteroids as premedication or at any time during treatment with tisagenlecleucel, except in the case of life-threatening emergency (such as resistant cytokine release syndrome). Consider therapy modification
Tofacitinib: Immunosuppressants may enhance the immunosuppressive effect of Tofacitinib. Management: Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted, and this warning seems particularly focused on more potent immunosuppressants. Consider therapy modification
Trastuzumab: May enhance the neutropenic effect of Immunosuppressants. Monitor therapy
Upadacitinib: Immunosuppressants may enhance the immunosuppressive effect of Upadacitinib. Avoid combination
Urea Cycle Disorder Agents: Corticosteroids (Systemic) may diminish the therapeutic effect of Urea Cycle Disorder Agents. More specifically, Corticosteroids (Systemic) may increase protein catabolism and plasma ammonia concentrations, thereby increasing the doses of Urea Cycle Disorder Agents needed to maintain these concentrations in the target range. Monitor therapy
Vaccines (Inactivated): Immunosuppressants may diminish the therapeutic effect of Vaccines (Inactivated). Management: Vaccine efficacy may be reduced. Complete all age-appropriate vaccinations at least 2 weeks prior to starting an immunosuppressant. If vaccinated during immunosuppressant therapy, revaccinate at least 3 months after immunosuppressant discontinuation. Consider therapy modification
Vaccines (Live): Corticosteroids (Systemic) may enhance the adverse/toxic effect of Vaccines (Live). Corticosteroids (Systemic) may diminish the therapeutic effect of Vaccines (Live). Management: Doses equivalent to less than 2 mg/kg or 20 mg per day of prednisone administered for less than 2 weeks are not considered sufficiently immunosuppressive to create vaccine safety concerns. Higher doses and longer durations should be avoided. Consider therapy modification
Warfarin: Corticosteroids (Systemic) may enhance the anticoagulant effect of Warfarin. Monitor therapy
Test Interactions
May decrease response to skin tests
Adverse Reactions
Frequency not defined.
Cardiovascular: Atheromatous embolism, bradycardia, cardiac arrhythmia, cardiac failure (especially in susceptible patients), cardiomegaly, circulatory shock, hypertension, hypertrophic cardiomyopathy (premature infants), myocardial rupture (post-myocardial infarction), syncope, tachycardia, thromboembolism, thrombophlebitis, vasculitis
Central nervous system: Arachnoiditis (intrathecal administration), depression, emotional lability, euphoria, headache, increased intracranial pressure (with pseudotumor cerebri; usually following discontinuation), insomnia, malaise, meningitis (intrathecal administration), myasthenia, neuritis, neuropathy, paraplegia (intrathecal administration), paresthesia, personality changes, psychic disorder, seizure, sensory disturbance (intrathecal administration), tingling of skin (especially in the perineal area after IV injection), vertigo
Dermatologic: Acne vulgaris, allergic dermatitis, alopecia, atrophic striae, burning sensation of skin (especially in the perineal area after IV injection), diaphoresis, ecchymosis, erythema (including facial), exfoliation of skin, hyperpigmentation, hypertrichosis, hypopigmentation, skin atrophy, skin rash, suppression of skin test reaction, urticaria, xeroderma
Endocrine & metabolic: Adrenal suppression, Cushing syndrome, diabetes mellitus (latent), fluid retention, glycosuria, growth suppression, hirsutism, HPA-axis suppression, hypercalcemia (associated with cancers), hyperglycemia (including increased requirements for insulin or oral hypoglycemic agents in diabetes mellitus), hypokalemia, hypokalemic alkalosis, impaired glucose tolerance, lipodystrophy, lipomatosis (epidural), menstrual disease (menstrual irregularities), moon face, negative nitrogen balance, protein catabolism, sodium retention, weight gain
Gastrointestinal: Abdominal distention, carbohydrate intolerance, dyspepsia, gastrointestinal disease (intrathecal administration), gastrointestinal perforation (small and large intestine, particularly in patients with inflammatory bowel disease), hiccups, increased appetite, nausea, pancreatitis, peptic ulcer (with possible perforation and hemorrhage), ulcerative esophagitis, vomiting
Genitourinary: Asthenospermia, bladder dysfunction (intrathecal administration)
Hematologic & oncologic: Leukocytosis, petechia
Hepatic: Hepatomegaly, increased serum transaminases (usually mild elevations and reversible on discontinuation)
Hypersensitivity: Anaphylaxis, angioedema, hypersensitivity reaction
Infection: Increased susceptibility to infection, infection, sterile abscess
Local: Atrophy at injection site (cutaneous and subcutaneous), postinjection flare (intra-articular use), skin edema
Neuromuscular & skeletal: Amyotrophy, Charcot-like arthropathy, lower extremity weakness (intrathecal administration), osteonecrosis (aseptic necrosis of femoral and humoral heads), osteoporosis, pathological fracture (long bones), rupture of tendon (particularly Achilles tendon), steroid myopathy, vertebral compression fracture
Ophthalmic: Cataract (posterior subcapsular), exophthalmos, glaucoma, increased intraocular pressure, retinopathy (central serous chorioretinopathy)
Respiratory: Pulmonary edema
Miscellaneous: Wound healing impairment
<1%, postmarketing, and/or case reports: Anaphylactoid reaction, blindness (periocular injection)
Warnings/Precautions
Concerns related to adverse effects:
- Adrenal suppression: May cause hypercortisolism or suppression of hypothalamic-pituitary-adrenal (HPA) axis, particularly in younger children or in patients receiving high doses for prolonged periods. HPA axis suppression may lead to adrenal crisis. Withdrawal and discontinuation of a corticosteroid should be done slowly and carefully. Particular care is required when patients are transferred from systemic corticosteroids to inhaled products due to possible adrenal insufficiency or withdrawal from steroids, including an increase in allergic symptoms. Patients receiving >20 mg per day of prednisone (or equivalent) may be most susceptible. Fatalities have occurred due to adrenal insufficiency in asthmatic patients during and after transfer from systemic corticosteroids to aerosol steroids; aerosol steroids do not provide the systemic steroid needed to treat patients having trauma, surgery, or infections.
- Anaphylactoid reactions: Rare cases of anaphylactoid reactions have been observed in patients receiving corticosteroids.
- Dermal changes: Avoid injection or leakage into the dermis; dermal and/or subdermal skin depression may occur at the site of injection. Avoid deltoid muscle injection; subcutaneous atrophy may occur.
- Immunosuppression: Prolonged use of corticosteroids may increase the incidence of secondary infection, mask acute infection (including fungal infections), prolong or exacerbate viral infections, or limit response to killed or inactivated vaccines. Exposure to chickenpox or measles should be avoided. Corticosteroids should not be used for cerebral malaria, fungal infections, or viral hepatitis. Close observation is required in patients with latent tuberculosis and/or TB reactivity; restrict use in active TB (only fulminating or disseminated TB in conjunction with antituberculosis treatment). Latent or active amebiasis should be ruled out in any patient with recent travel to tropical climates or unexplained diarrhea prior to corticosteroid initiation. Use with extreme caution in patients with Strongyloides infections; hyperinfection, dissemination and fatalities have occurred.
- Kaposi sarcoma: Prolonged treatment with corticosteroids has been associated with the development of Kaposi sarcoma (case reports); if noted, discontinuation of therapy should be considered (Goedert 2002).
- Myopathy: Acute myopathy has been reported with high dose corticosteroids, usually in patients with neuromuscular transmission disorders; may involve ocular and/or respiratory muscles; monitor creatine kinase; recovery may be delayed.
- Psychiatric disturbances: Corticosteroid use may cause psychiatric disturbances, including euphoria, insomnia, mood swings, personality changes, severe depression, or psychotic manifestations. Pre-existing psychiatric conditions may be exacerbated by corticosteroid use.
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with HF and/or hypertension; use has been associated with fluid retention, electrolyte disturbances, and hypertension. Use with caution following acute MI; corticosteroids have been associated with myocardial rupture.
- Diabetes: Use corticosteroids with caution in patients with diabetes mellitus; may alter glucose production/regulation leading to hyperglycemia.
- Gastrointestinal disease: Use with caution in patients with GI diseases (diverticulitis, fresh intestinal anastomoses, active or latent peptic ulcer, ulcerative colitis, abscess or other pyogenic infection) due to perforation risk.
- Head injury: Increased mortality was observed in patients receiving high-dose IV methylprednisolone; high-dose corticosteroids should not be used for the management of head injury.
- Hepatic impairment: Use with caution in patients with hepatic impairment, including cirrhosis; long-term use has been associated with fluid retention.
- Myasthenia gravis: Use with caution in patients with myasthenia gravis; exacerbation of symptoms has occurred especially during initial treatment with corticosteroids.
- Ocular disease: Use with caution in patients with cataracts and/or glaucoma; increased intraocular pressure, open-angle glaucoma, and cataracts have occurred with prolonged use. Oral steroid treatment is not recommended for the treatment of acute optic neuritis; may increase frequency of new episodes and does not affect short- or long-term visual outcomes. Use with caution in patients with ocular herpes simplex; corneal perforation may occur; do not use in active ocular herpes simplex. Consider routine eye exams in chronic users.
- Osteoporosis: Use with caution in patients with osteoporosis; high doses and/or long-term use of corticosteroids have been associated with increased bone loss and osteoporotic fractures.
- Pheochromocytoma: Pheochromocytoma crisis has been reported with corticosteroids (may be fatal). Consider the risk of pheochromocytoma crisis prior to administering corticosteroids in patients with suspected pheochromocytoma.
- Renal impairment: Use with caution in patients with renal impairment; fluid retention may occur.
- Seizure disorders: Use corticosteroids with caution in patients with a history of seizure disorder; seizures have been reported with adrenal crisis.
- Septic shock or sepsis syndrome: Corticosteroids should not be administered for the treatment of sepsis in the absence of shock (SCCM/ESICM [Annane 2017]).
- Thyroid disease: Changes in thyroid status may necessitate dosage adjustments; metabolic clearance of corticosteroids increases in hyperthyroid patients and decreases in hypothyroid ones.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Use with caution in the elderly with the smallest possible effective dose for the shortest duration.
- Pediatric: May affect growth velocity; growth should be routinely monitored in pediatric patients.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Diluent for injection may contain benzyl alcohol and some dosage forms may contain sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol and/or benzyl alcohol derivative with caution in neonates. See manufacturer’s labeling.
Other warnings/precautions:
- Discontinuation of therapy: Withdraw therapy with gradual tapering of dose.
- Epidural injection: Corticosteroids are not approved for epidural injection. Serious neurologic events (eg, spinal cord infarction, paraplegia, quadriplegia, cortical blindness, stroke), some resulting in death, have been reported with epidural injection of corticosteroids, with and without use of fluoroscopy.
- Stress: Patients may require higher doses when subject to stress (ie, trauma, surgery, severe infection).
Monitoring Parameters
Serum glucose, electrolytes; blood pressure, weight, presence of infection; monitor IOP with therapy >6 weeks; bone mineral density; assess HPA axis suppression (eg, ACTH stimulation test, morning plasma cortisol test, urinary free cortisol test); growth in pediatric patients.
Pregnancy
Pregnancy Considerations
Adverse events have been observed with corticosteroids in animal reproduction studies. Some studies have shown an association between first trimester systemic corticosteroid use and oral clefts or decreased birth weight; however, information is conflicting and may be influenced by maternal dose/indication for use (Lunghi 2010; Park-Wyllie 2000; Pradat 2003). Hypoadrenalism may occur in newborns following maternal use of corticosteroids in pregnancy; monitor.
When treating women with adrenal insufficiency (primary or central or congenital adrenal hyperplasia) during pregnancy, hydrocortisone is the preferred corticosteroid. Doses may need to be adjusted as pregnancy progresses, and stress doses may be required during active labor. Pregnant women with adrenal insufficiency should be monitored at least once each trimester (ES [Bornstein 2016]; ES [Fleseriu 2016]; ES [Speiser 2018]).
Uncontrolled asthma is associated with adverse events on pregnancy (increased risk of perinatal mortality, preeclampsia, preterm birth, low birth weight infants). Poorly controlled asthma or asthma exacerbations may have a greater fetal/maternal risk than what is associated with appropriately used asthma medications (ACOG 2008; GINA 2018). Inhaled corticosteroids are recommended for the treatment of asthma during pregnancy; however, systemic corticosteroids should be used to control acute exacerbations or treat severe persistent asthma (ACOG 2008; GINA 2018; Namazy 2016). Women who require systemic corticosteroids for management of their asthma should be given intravenous corticosteroids, such as hydrocortisone, during labor and for 24 hours after delivery to prevent adrenal crisis (ACOG 2008).
When systemic corticosteroids are needed in pregnancy for rheumatic disorders, it is generally recommended to use the lowest effective dose for the shortest duration of time, avoiding high doses during the first trimester (Götestam Skorpen 2016; Makol 2011; Østensen 2009).
For dermatologic disorders in pregnant women, systemic corticosteroids are generally not preferred for initial therapy; should be avoided during the first trimester; and used during the second or third trimester at the lowest effective dose (Bae 2012; Leachman 2006).
Patient Education
What is this drug used for?
- It is used for many health problems like allergy signs, asthma, adrenal gland problems, blood problems, skin rashes, or swelling problems.
- This is not a list of all health problems that this drug may be used for. Talk with the doctor.
Frequently reported side effects of this drug
- Nausea
- Vomiting
- Trouble sleeping
- Restlessness
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Adrenal gland problems like severe nausea, vomiting, severe dizziness, passing out, muscle weakness, severe fatigue, mood changes, lack of appetite, or weight loss
- Infection
- High blood sugar like confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit
- Low potassium like muscle pain or weakness, muscle cramps, or an abnormal heartbeat
- Pancreatitis like severe abdominal pain, severe back pain, severe nausea, or vomiting
- Cushing syndrome like weight gain in upper back or abdomen; moon face; severe headache; or slow healing
- Severe loss of strength and energy
- Irritability
- Tremors
- Fast heartbeat
- Confusion
- Dizziness
- Sweating a lot
- Shortness of breath
- Excessive weight gain
- Swelling of arms or legs
- Skin changes like acne, stretch marks, slow healing, or hair growth
- Severe headache
- Passing out
- Bone pain
- Joint pain
- Menstrual changes
- Chest pain
- Vision changes
- Eye pain
- Severe eye irritation
- Mood changes
- Behavioral changes
- Depression
- Seizures
- Bruising
- Bleeding
- Severe abdominal pain
- Black, tarry, or bloody stools
- Vomiting blood
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.